Experiencing a major disaster such as earthquake can exert lingering impacts on health, directly and indirectly through alteration of health behaviours, including dietary behaviours(Reference Goldmann and Galea1,Reference Rubeis, Lee and Anwer2) . Despite its fundamental role in determining health outcomes, long-term impact of disaster experience on diet(Reference Whitaker, Phillips and Orzol3) has been less studied among older people who are prone to disease and are vulnerable to disaster damages(Reference Jia, Tian and Liu4).
Disasters can potentially lead to changes in dietary behaviours through several hypothetical pathways. First, disaster-related trauma can affect mental health, which in turn affects people’s appetite and dietary habits, e.g. choice of food items(Reference Abbasalizad Farhangi, Dehghan and Jahangiry5). It has been shown that those with depression are more likely to consume high fat and sugar foods while fewer fruits and vegetables(Reference Payne, Steck and George6), and these associations can be different between men and women(Reference Mohamad, Sabbah and Smail7,Reference Zellner, Loaiza and Gonzalez8) . A previous study showed that older people suffering from post-traumatic stress symptoms (PTSS) and/or depression a decade after the Great East Japan Earthquake and Tsunami reported less consumption of Japanese traditional diet high in vegetables, soya products and fruits(Reference Yazawa, Shiba and Hikichi9). Notably, men showed unhealthy dietary pattern when they lived alone or were unmarried and suffered from mental problems, while women did not show such difference according to their marital status. Second, disaster-related loss of a spouse can also affect survivors’ eating habits: older adults who experience widowhood are known to face challenges in maintaining the quality of their diet(Reference Rosenbloom and Whittington10,Reference Shahar, Schultz and Shahar11) . This may be due to various factors, including a lack of motivation to cook for eating alone, as well as changes in daily routines. In addition, increased loneliness due to death of spouse, family or friends can diminish the social reasons for and pleasures associated with, eating(Reference Shifflett and McIntosh12,Reference Walker and Beauchene13) . Third, other disaster-related experiences, such as residential displacement, can produce changes in the diet due to alterations in the home environment (e.g. the inconvenience of cooking meals in temporary housing with cramped kitchen space) or changes in the local food environment(Reference Hikichi, Aida and Kondo14,Reference Shiba, Hanazato and Aida15) .
Disaster-related traumas may increase a specific dietary pattern: pro-inflammatory diet, which is characterised by a high intake of refined grains, sugars, red and processed meat, eggs, high-fat dairy products, artificially sweetened drinks and salt(Reference Stromsnes, Correas and Lehmann16). Pro-inflammatory diet may increase after disasters because emotional distress may make people turn to comfort foods that are typically high in sugars and unhealthy fats, as well as limited access to fresh food and cooking facilities in the aftermath of the disaster can alter their cooking behaviour and lead to an increased reliance on processed and packaged foods. There has been exponential growth in the literature linking dietary inflammation to health. A systematic review of sixteen studies by Chen et al. (Reference Chen, Peng and Lian17) concluded that adults in the highest dietary inflammatory index (DII®) category showed significantly higher odds for depressive symptoms compared with the lowest DII category (OR = 1·28, 95 % CI 1·17, 1·39). There also are longitudinal studies showing that the inflammatory dietary pattern is associated with a higher depression risk(Reference Lucas, Chocano-Bedoya and Shulze18,Reference Sánchez-Villegas, Ruíz-Canela and Fuente-Arrillaga19) . Pro-inflammatory diet has been linked to other health outcomes including functional disability(Reference Tomata, Shivappa and Zhang20), frailty(Reference Tomata, Shivappa and Zhang20,Reference Kim and Park21) , CVD(Reference Ruiz-Canela, Bes-Rastrollo and Martínez-González22–Reference Garcia-Arellano, Ramallal and Ruiz-Canela24), dementia(Reference Hayden, Beavers and Steck25) and mortality(Reference Ruiz-Canela, Bes-Rastrollo and Martínez-González22,Reference Shivappa, Blair and Prizment26) . Despite its importance, there have been limited studies investigating the link between disaster experiences and eating behaviours. Specifically, research considering pre-disaster depression is notably scarce, and the issue of reverse causality remains unresolved.
In this study, we sought to investigate the impact of disaster damages on the dietary inflammatory score conditional on pre-disaster characteristics including depressive symptoms among older survivors 9 years after the Great East Japan Earthquake and Tsunami (GLIDE number: #EQ-2011-000028-JPN). In Japan, women are overwhelming more likely to be involved in household chores including preparing meals compared with men(27). In addition, as individuals advance in age, people tend to rely on other family members to undertake cooking responsibilities on their behalf, particularly as they become more frail. In this study, we investigated the impact of disaster damages on the DII, where higher scores indicate pro-inflammatory (i.e. unhealthy) diet, and how these relationships differed between genders or meal preparation habit. We hypothesised that those who experienced disaster damages would have higher DII.
Methods
Data
The data used in this study were obtained from the Iwanuma Study, which is a part of a larger national cohort study of Japanese older adults called the Japan Gerontological Evaluation Study(Reference Kondo and Rosenberg28). The study was conducted in Iwanuma city, which was one of the field sites of the Japan Gerontological Evaluation Study located in Miyagi Prefecture with a population of 44 187 in 2010. The baseline survey was conducted in August 2010, seven months prior to the Great East Japan Earthquake and Tsunami of March 11, 2011 (the Richter scale: 9·0). The the Japan Gerontological Evaluation Study conducted a census of all residents over the age of 65 in Iwanuma city (n 8576) and received valid responses from 4957 residents (response rate = 57·8 %). The study participants were representative of the population of Iwanuma city as a whole(Reference Hikichi, Aida and Tsuboya29).
The earthquake and tsunami resulted in the loss of 180 lives, damage to 5542 homes and the flooding of 48 % of the land area of Iwanuma city. Many survivors were forced to relocate to temporary housing or subsidised apartments on the rental market. The first follow-up survey was conducted in 2013, 2·5 years after the disaster, for all baseline cohort survivors. Of the 4380 eligible survivors who lived in Iwanuma city, 3567 people responded to the mailed survey (follow-up rate: 81·4 %). In January 2020, approximately 9 years after the disaster, dietary data were obtained from a follow-up survey (n 2573, follow-up rate 79·6 %) using the brief-type self-administered diet history questionnaire (BDHQ), which is a validated self-administered food frequency questionnaire based on the consumption frequency of fifty-eight food and beverage items during the preceding month(Reference Sasaki, Yanagibori and Amano30–Reference Kobayashi, Honda and Murakami32). BDHQ is a short version of a comprehensive self-administered diet history questionnaire (DHQ: 150-item semi-quantitative questionnaire) that includes food and beverage items commonly consumed in Japan. The validity of BDHQ was confirmed by comparing nutrient intake against DHQ using semi-weighed 16-day dietary records as reference, and its short-term test-retest reliability of eating habits has also been established(Reference Yatsuya, Ohwaki and Tamakoshi33). A total of 1531 individuals participated in both the 2010 and 2013 surveys and completed the dietary survey in 2020. After excluding individuals who did not provide information on weight and height (n 4), or reported an energy intake less than half of the energy requirement for the lowest physical activity category (< 725 kcal/d; n 7) or more than 1·5 times of the energy requirement for the highest physical activity category (> 3300 kcal/d; n 118) of the recommended amount by the Dietary Reference Intakes for Japanese(34), the analytical sample was reduced to 1375. The sample selection strategy is illustrated in Fig. 1.
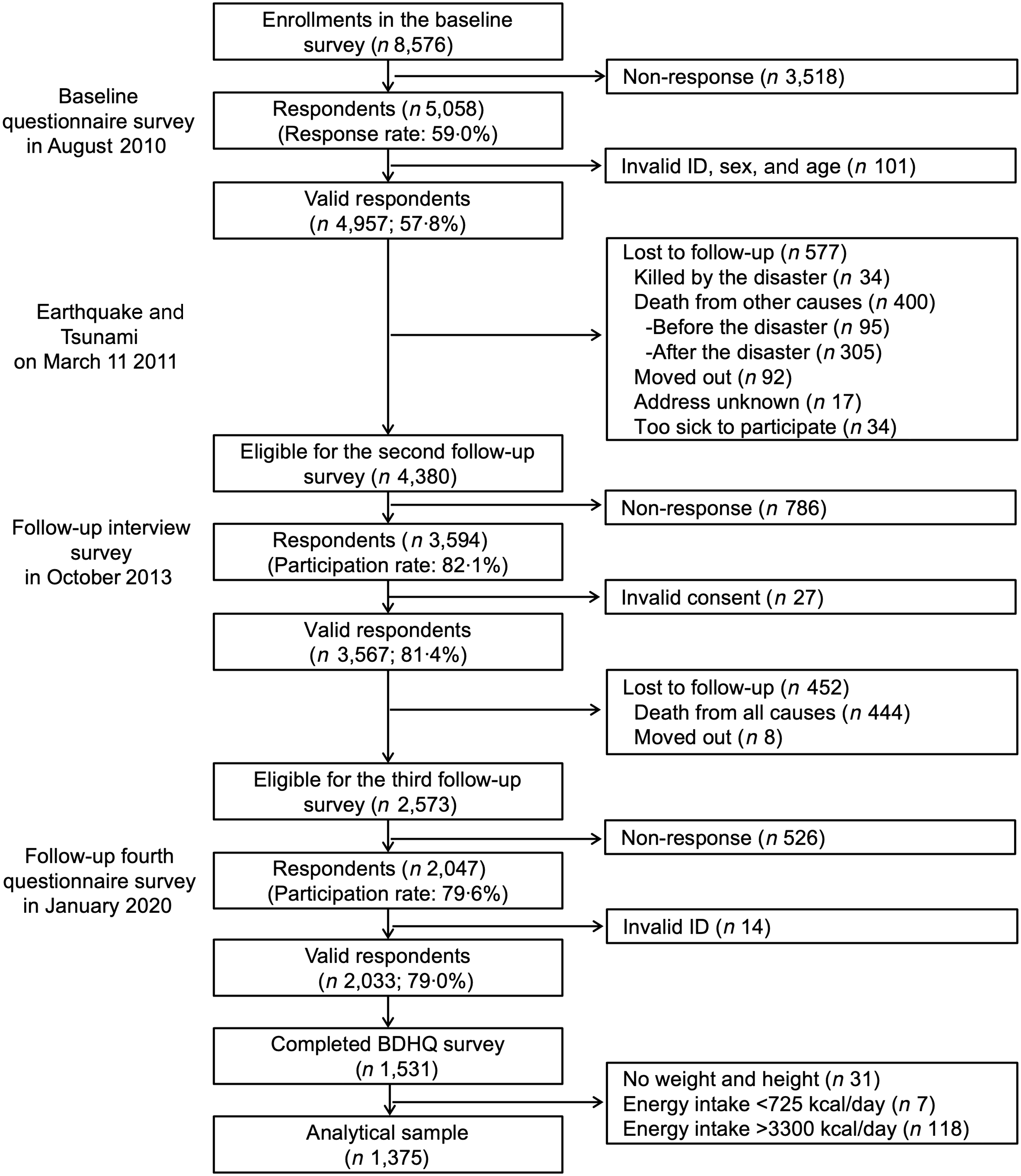
Fig. 1. Flow of the sampling strategy.
Measurements
Pre-disaster variables
The source of our pre-disaster variables is the baseline survey data collected in 2010, which included age (in years), gender (men; women), marital status (married; not married), educational attainment (less than 10 years; 10–12 years; 13 years or more), equivalent household income (less than 200; 200–399; more than 400 million yen), depressive symptoms (no; mild; severe), employment status (currently working; retired; never), BMI, self-rated health (poor; fair; good and excellent), protein consumption (less than once a week; two to three times a week; four to six times a week; once a day and twice or more a day), fruit and vegetable consumption (two to three times a week or less; four to six times a week; once a day and twice or more a day), smoking (never; has stopped > 5 years ago; has stopped within 4 years and current smoker) and alcohol drinking (never; stopped and current drinker). Depressive symptoms were evaluated using the Japanese version of the Geriatric Depression Scale(Reference Sheikh and Yesavage35–Reference Sugishita, Sugishita and Hemmi37). The answers to each of the fifteen binary (yes/no) questions were added together to yield a total score ranging from 0 to 15. A score between 5 and 9 was indicative of mild depressive symptoms, whereas a score of 10 or higher was indicative of severe depressive symptoms. For a post hoc analysis, data on frequency of meeting friends were obtained (almost everyday; two or three times a week; once a week; once or twice a month and a few times a year and never).
Disaster damages and post-disaster stress symptoms
Participants’ experience of five types of disaster damages was retrieved from the follow-up survey in 2013, which includes housing damage (major damage/complete destruction v. less extensive damage), job loss (yes; no), economic loss (yes; no), loss of relatives (yes; no) and loss of friends (yes; no). In addition, whether they relocated after the disaster was obtained (yes; no). PTSS were also assessed in 2013 using the Screening Questionnaire for Disaster Mental Health(Reference Hikichi, Aida and Tsuboya29,Reference Fujii, Kato and Maeda38) . The questionnaire was originally developed to evaluate the PTSS among Japanese older survivors of the Hanshin-Awaji Earthquake in 1995 (Richter scale: 7·3, GLIDE number: #EQ-1995-000003-JPN), which has been validated against the Clinician Administered PTSD Scale and the Impact of Event Scale-Revised(Reference Fujii, Kato and Maeda38). Participants answered nine questions with binary (yes/no) responses, and the total score was calculated (0–9) and categorized into three: no PTSS (0–3), mild (4–5) and severe (6–9) symptoms(Reference Fujii, Kato and Maeda38).
Meal preparation status
In the 2020 survey, we asked a question to determine if participants prepare their own meals. The question asked was ‘Can you cook for yourself?’ and respondents had three answer options: ‘Yes, I can and do,’ ‘Yes, I can but usually don’t’ and ‘No, I can’t.’ We created a binary variable to indicate whether participants prepared their own meals by combining the last two answer options into a single category.
Dietary inflammatory index
The DII is a tool used to assess the inflammatory potential of an individual’s diet quantitatively. The DII is calculated based on the intake of several nutrients and foods that have been shown to have either anti-inflammatory or pro-inflammatory effects. In this study, DII was calculated by the twenty-six food parameters obtained in the BDHQ following the methods described previously(Reference Shivappa, Steck and Hurley39,Reference Shivappa, Stubbs and Hébert40) , which includes alcohol, vitamin B12, vitamin B6, β-carotene, carbohydrate, cholesterol, energy, total fat, fibre, folic acid, Fe, Mg, MUFA, niacin, n-3 fatty acids, n-6 fatty acids, protein, PUFA, riboflavin, saturated fat, thiamine, vitamin A, vitamin C, vitamin E, Zn and tea.
First, we determined the relative exposure to each food/nutrient by subtracting the amount of each food/nutrient with the global daily mean intake and dividing it by the standard deviation derived from the world composite database. Second, to minimise the impact of right skewing, we converted the relative exposure values to a centered percentile score. This involved doubling each percentile score and then subtracting by one to create a symmetrical distribution with a range from −1 (maximally anti-inflammatory) to 1 (maximally pro-inflammatory). Third, the value for each parameter was multiplied by the food and nutrient-specific inflammatory effect scores provided by Shivappa et al. (Reference Shivappa, Stubbs and Hébert40) to calculate the DII score for each food and nutrient. These scores are based on an extensive review of the previous scientific literature. Finally, these scores were summed to create the overall DII score (ranged −5·3 to 4·5 in the study participants, where higher scores indicate more pro-inflammatory diet).
Statistical analysis
Least-squares linear regression was conducted to investigate the association between disaster-related trauma and dietary inflammatory index and how these relationships differed by gender and meal preparation status. Model 1 included disaster damages and PTSS, gender and whether the respondent prepared their meals, while Model 2 included the interaction term between disaster damage and gender to investigate potential gender differences in the impact of disaster experiences on diet. Model 3 further incorporated a three-way interaction between gender * disaster damage * whether the respondent prepared their own meals. Covariates included age, marital status, educational attainment, household equivalent income, employment status, BMI, self-rated health, frequency of protein/vegetable intake, smoking, alcohol consumption and depressive symptoms in 2010.
Missing values were imputed by the Markov chain Monte Carlo methods to generate twenty datasets(Reference Sterne, White and Carlin41) for those who provided dietary data. The level of statistical significance was set at P < 0·05 (two-tailed). All statistical analyses were conducted using Stata 16.1 or 17.1 (StataCorp).
Results
Table 1 presents the characteristics of study participants. The mean age was 70·9 years (standard deviation of 4·5) in 2010 and 44·6 % were men. In terms of disaster damages, 6·8 % experienced major housing damage, 6·4 % experienced job loss, 22·1 % experienced economic loss, 28·1 % lost their relatives, 17·5 % lost friends in the earthquake and tsunami, and 27 % experienced mild to severe PTSS. In 2020, 68·5 % reported that they prepared their own meals.
Table 1. Characteristics of the study participants (n 1375)
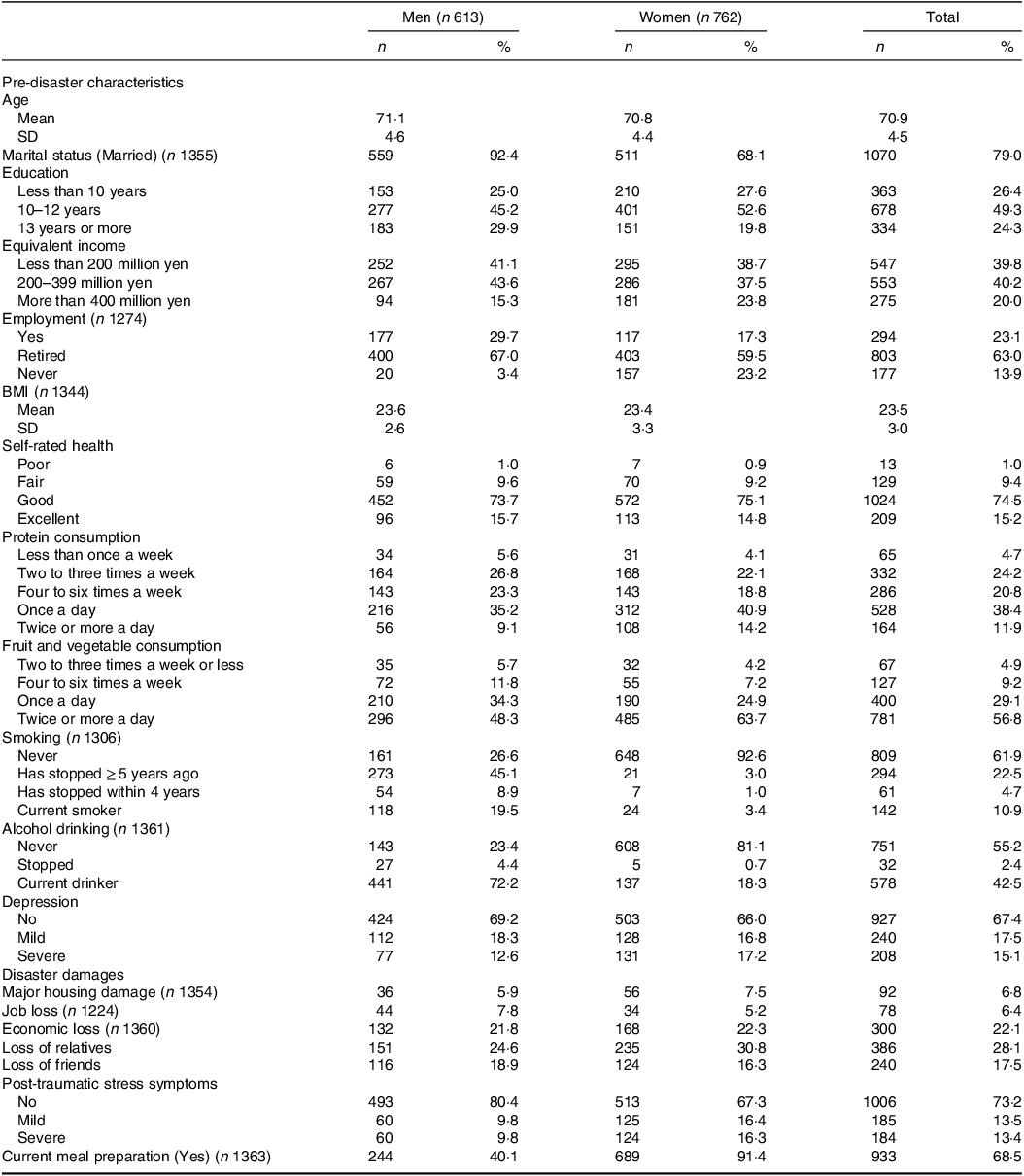
Mean (standard deviation)/n (%) are shown.
Table 2 shows the results regressing DII scores on types of disaster damage. Model 1 revealed that major housing damage was associated with a slightly higher DII score (coef. = 0·38, 95 % CI –0·05, 0·81), which was not statistically significant, while loss of friends was associated with a lower DII score (coef. = −0·28, 95 % CI –0·54, −0·01). Participants who prepared their own meals showed higher DII scores (coef. = 0·31, 95 % CI 0·05, 0·57). Subsequent analyses with interaction terms were conducted only for major housing damage. Model 2 found an interaction between gender and housing damage (P = 0·056); women who experienced housing damage were more likely to show a higher DII score. Three-way interaction (Model 3) indicated that women who prepared their own meals tended to show higher DII scores when they experienced housing damage, although the interaction was not statistically significant (Fig. 2). Online Supplementary Table 1 displays the results of Model 1, encompassing all the estimates including those for covariates for additional information.
Table 2. Disaster damages and post-traumatic-stress symptoms after the disaster and dietary inflammatory index among older survivors of 2011 great east Japan earthquake and Tsunami in 2020 (n 1375)

* P < 0·05.
† P < 0·1.
PTSS, post-traumatic stress symptoms.
Least-squares linear regression analyses were conducted separately for three models. Coefficients (95 % CI) are shown. Covariates included age, marital status, educational attainment, household equivalent income, employment status, BMI, self-rated health, frequency of protein/vegetable intake, smoking, alcohol consumption and depression in 2010. Sample sizes for interaction terms: housing damage (yes) × women (n 56), housing damage (no) × women (n 691), housing damage (yes) × men (n 36), housing damage (no) × men (n 571); housing damage (yes) × women × meal preparation (yes) (n 46), housing damage (no) × women × meal preparation (yes) (n 630), housing damage (yes) × women × meal preparation (no) (n 9), housing damage (no) × women × meal preparation (no) (n 54), housing damage (yes) × men × meal preparation (yes) (n 12), housing damage (no) × men × meal preparation (yes) (n 229), housing damage (yes) × men × meal preparation (no) (n 23), housing damage (no) × men × meal preparation (no) (n 339).
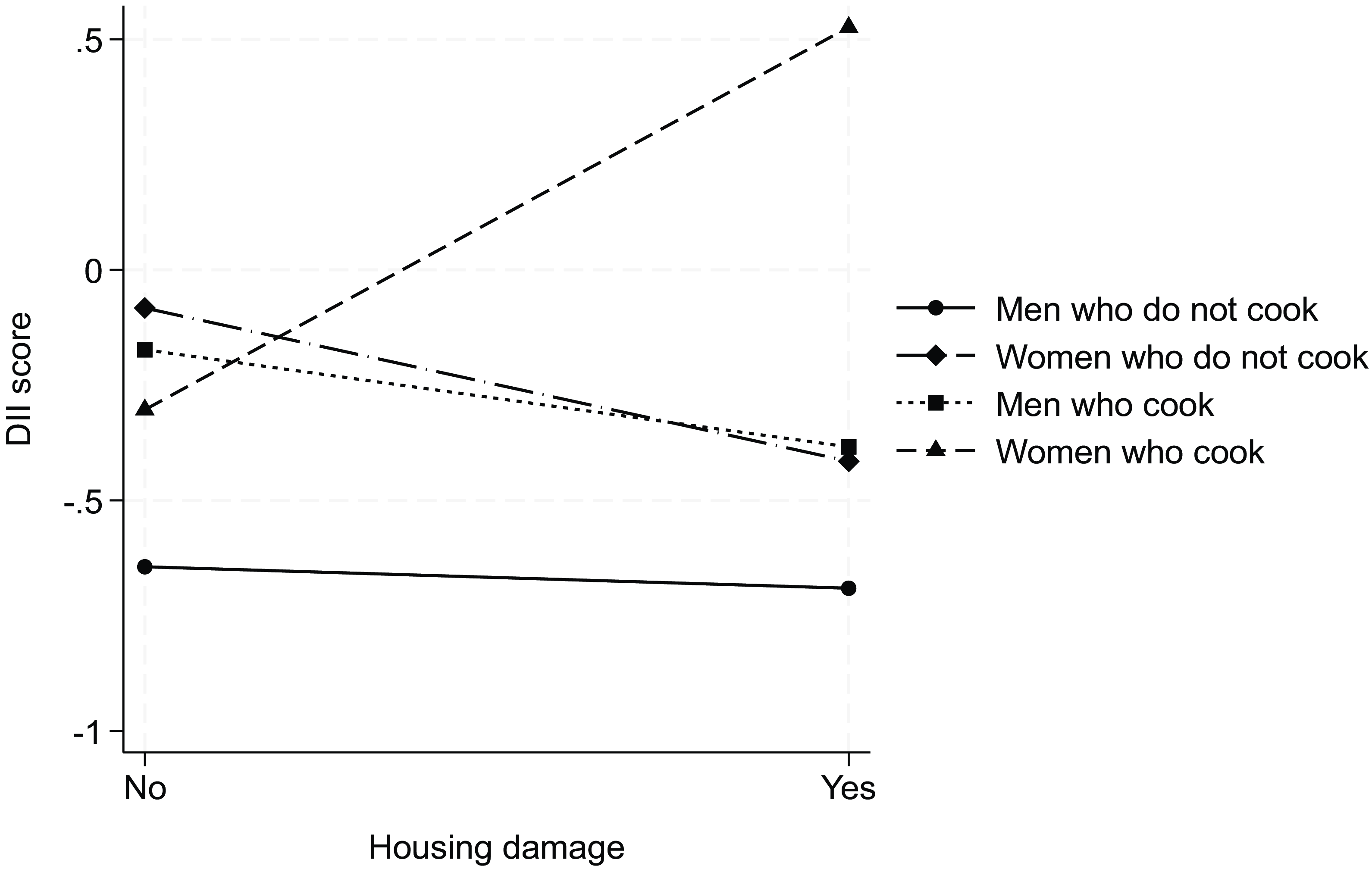
Fig. 2. Interaction between gender, housing damage and meal preparation on the Dietary Inflammatory Index score.
Discussion
Summary of the findings
This study used a long-term follow-up data of the Great East Japan Earthquake and Tsunami to evaluate the impact of the disaster on the inflammatory profile of the diet conditional on pre-disaster characteristics among older disaster survivors. Among the types of disaster damages, housing damage was associated with slightly higher pro-inflammatory dietary scores 9 years after the disaster. Specifically, women had higher DII if they experienced housing damage. On the other hand, loss of friends was associated with a lower DII score.
Housing damage and pro-inflammatory diet
As hypothesised, we found that the experience of housing damage was marginally associated with higher inflammatory diet scores. Shiba et al. (Reference Shiba, Hikichi and Aida42) reported that survivors who experienced home loss exhibited increased BMI and waist circumference, as well as decreased high-density lipoprotein cholesterol than those with less housing damage 2·5 years after the Great East Japan Earthquake and Tsunami. A long-term follow-up study of the survivors of the 1988 Spitak earthquake in Armenia similarly found that total home destruction was linked to the increased risk of diabetes after 23 years(Reference Khachadourian43). The present study suggests that post-disaster diet may be one of the pathways linking housing damage and worsened cardiometabolic profiles.
In this study, the positive association between housing damage and DII was more pronounced among women, especially for those who cooked by themselves. It has been shown that women are more susceptible to changes in the neighbourhood environment compared with men(Reference Stafford, Cummins and Macintyre44,Reference Wang, Kim and Gonzalez45) . Shiba et al. (Reference Shiba, Hanazato and Aida15) examined changes in neighbourhood environment after the Great East Japan Earthquake and Tsunami in relation to changes in cardiometabolic markers. In stratified analysis, women who moved to more dense areas (e.g. more food facilities, convenience stores) showed an increase in BMI, but the association was less pronounced among men. Changes in neighbourhood environments in the aftermath of the earthquake may have caused the dietary change especially among women.
Women are also psychologically more vulnerable in the aftermath of disasters(Reference Tolin and Foa46). After the Great East Japan Earthquake and Tsunami, women were 1·6 times more likely to experience PTSS(Reference Yazawa, Aida and Kondo47). According to the current study’s data, women were also 1·1 times more likely to experience the new onset of depressive symptoms compared with male survivors (seventy out of 424 men (16·5 %) v. 93 out of 503 women (18·5 %)). Depression and PTSS are strong predictors of emotional eating, and studies have shown that emotional eating is more frequently observed among women than men and contribute to weight gain(Reference Péneau, Ménard and Méjean48,Reference Camilleri, Méjean and Kesse-Guyot49) . Emotional eating is usually characterised by a decrease in the consumption of fruits and vegetables(Reference Konttinen, Männistö and Sarlio-Lähteenkorva50), which are generally known for their anti-inflammatory properties, and an increase in the intake of energy-dense fast foods, sweets and confectionery(Reference Crawford, Khedkar and Flaws51,Reference Jeffery, Linde and Simon52) , which tend to be more pro-inflammatory(Reference Phillips, Shivappa and Hébert53). Even in the absence of depression/PTSS, individuals who have experienced housing damages are likely to face persistent daily stressors, which are known to be associated with increased consumption of high fat/sugar snacks and with a reduction in main meals and vegetable consumption, indicating a pro-inflammatory diet, which is particularly prominent among women(Reference O’Connor, Jones and Conner54). While we have controlled for pre- and post-disaster mental status, psychological impact of disaster and behavioural changes due to it may be more pronounced among women, resulting in higher consumption of pro-inflammatory diet. Another important factor to consider is that, generally, women are significantly more prone to participating in meal preparation compared with men in Japan(27). The fact that the association between housing damage and inflammatory diet was observed mainly among women who cooked by themselves may suggest that women who do not cook probably have their family members cook for them. This is a hypothetical scenario derived from the results, which should be validated in future studies.
It is also anticipated that the experience of living in a temporary housing may have had a greater impact on the cooking habits of women compared with men. Many people who suffered housing damage relocated to temporary housing called kasetsu jutaku, which have very small kitchens. Such condition may have shifted dietary behaviour towards consumption of more fast foods or simple meals(Reference Zhang, Ohira and Abe55). While there was only twenty-one people who moved to kasetsu jutaku in this study sample, they showed the higher DII score (mean 0·13 sd 1·9, not shown in Tables) compared with those who did not move (mean –0·35 sd 2·0) or those who bought a new house (mean –0·66 sd 1·8). There is also ethnographic research indicating dietary behaviour change after 4 years after the disaster (e.g. the presentation of dishes has shifted from individual servings to large shared plates due to limited space and people stopped making preserved foods, such as miso and pickled vegetables)(Reference Noda, Ogawa and Kuji56). It is possible that one of the pathways linking housing damage and pro-inflammatory diet is the experience of kasetsu jutaku. This is a hypothesis that requires empirical testing. Future studies are warranted to assess the long-term impact of relocation to temporary housing on dietary habits.
Loss of friends and pro-inflammatory diet
Contrary to our hypothesis, other disaster damages were not linked to an increased DII. Instead, the loss of friends was associated with a lower DII. The loss of friends might be linked to a reduced frequency of enjoying meals high in sugar and fat (e.g. snacks), but it is improbable that the influence of such occasional meals has been substantial enough to persist for a decade. One potential explanation for this association is that individuals who lost their friends in the disaster were more likely to be socially active and had a better diet before the disaster, which in turn contributed to their maintenance of a healthier diet after the disaster. We conducted a post hoc analysis using data from 2010 regarding the frequency of consuming protein, fruits and vegetables, as well as social interactions with friends. As shown in the online Supplementary Table 2, individuals who lost their friends in the disaster tended to have a slightly higher frequency of consuming protein, fruits and vegetables, as well as meeting with friends more often before the disaster. Since we did not conduct a pre-disaster dietary survey, it was impossible to observe dietary changes before and after the disaster. A future study is warranted to assess the impact of different types of disaster damages on dietary habits.
Limitations
Several limitations should be acknowledged within this study. First, the absence of pre-disaster dietary data is a notable limitation, although we did account for protein and vegetable intakes as well as alcohol consumption assessed in 2010. Second, the DII score was derived from self-reported food intake, which introduces the potential for recall bias, particularly among individuals with cognitive decline. It is also impossible to distinguish how the meals were prepared (e.g. homemade meals, meals purchased at grocery stores or meals at restaurants). Moreover, the use of complex dietary questionnaire and/or non-participation in the follow-up survey may have resulted in selection bias(Reference Shiba, Kawahara and Aida57). Third, while we considered PTSS as an exposure, it is plausible that it functions as a mediator between disaster damages (e.g. housing damage) and dietary habits. Given the potential existence of both direct and indirect pathways, future research should focus on comprehending the intricate relationship among disasters, mental dysfunction and health behaviours. Lastly, the generalisability of the findings may be limited to other age groups. Older people generally face challenges such as loss of appetite, change or loss in taste, tooth loss and reduced mobility(Reference Pilgrim, Robinson and Sayer58–Reference Kotronia, Brown and Papacosta60), which can further exacerbate the impact of prolonged burden from disaster damages.
Conclusion
Our study shows that nearly a decade after the Great East Japan Earthquake and Tsunami, the experience of housing damage leaves a lingering impact on the quality of individuals’ diets. This sustained impact on dietary habits may have contributed to the deterioration of overall health in various aspects. Notably, this effect was particularly evident among women, who often take on more household responsibilities and are known to be more vulnerable to the environmental and psychological repercussions of disasters compared with men. These findings highlight the importance of providing support to groups who are at increased risk of deterioration in dietary quality in the aftermath of disasters.
Acknowledgements
This study used data from the Japan Gerontological Evaluation Study (the Japan Gerontological Evaluation Study). This study was supported by a grant from the National Institutes of Health (R01 AG042463), Japan Society for the Promotion of Science (JSPS) (KAKENHI Grant Numbers JP22390400, JP22592327, JP24390469, JP15H04781, JP15H01972, JP16H05556, JP19H03860, JP21J01171), Health Labour Sciences Research Grant (H28-Choju-Ippan-002), Japan Agency for Medical Research and Development (AMED) (JP18dk0110027, JP18ls0110002, JP18le0110009, JP20dk0110034, JP21lk0310073, JP21dk0110037), Open Innovation Platform with Enterprises, Research Institute and Academia (OPERA, JPMJOP1831) from the Japan Science and Technology (JST), a grant from Innovative Research Program on Suicide Countermeasures (1–4), a grant from Sasakawa Sports Foundation, a grant from Japan Health Promotion & Fitness Foundation, a grant from Chiba Foundation for Health Promotion & Disease Prevention, the 8020 Research Grant for fiscal 2019 from the 8020 Promotion Foundation (adopted number: 19-2-06), grants from Welfare and the Research Funding for Longevity Sciences from National Center for Geriatrics and Gerontology (29–42, 30–22, 20–19, 21–20), a grant from Meiji, Obirin University and Niimi University (1915010). A.Y. is financially supported by JSPS Research Fellowship for Young Scientists. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the respective funding organisations.
A.Y. and I.K.: Conceptualisation; H.H. and K.K.: data curation; A.Y.: formal analysis; K.K., I.K. and A.Y.: funding acquisition; K.K. and I.K.: investigation; A.Y., I.K. and S.S.: methodology; K.K. and I.K.: project administration; K.K. and I.K.: resources; A.Y.: software; I.K.: supervision; H.H. and K.S.: validation; A.Y.: visualisation; A.Y. and I.K.: roles/writing – original draft; K.S., S.S.O., H.H., S.S. and K.K.: writing – review and editing.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and the study involving human subjects/patients were approved by the Human Subjects Committee of the Harvard T.H. Chan School of Public Health (CR-23143-09), the Institutional Review Boards of Chiba University (protocol #3442), and Tokyo Medical & Dental University (D2021-025). Written informed consent was obtained from all subjects.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524000217







