Organic foods, acclaimed for environmental benefits related to their production(Reference Reganold and Wachter1), are also perceived as having beneficial effects on health(Reference Baudry, Mejean and Peneau2–Reference Pearson, Henryks and Jones5) because they contain fewer pesticide residues as compared with conventionally grown foods(6). European rules imposed a very low common limit for all pesticides on all baby foodstuffs(7), whatever the mode of agricultural production. Studies examining the consumption of organic foods during pregnancy have reported a protective effect on some birth outcomes, such as pre-eclampsia, hypospadias and cryptorchidism(Reference Torjusen, Brantsaeter and Haugen8,Reference Brantsaeter, Torjusen and Meltzer9) , as well as a child’s later health, such as atopic diseases(Reference Kummeling, Thijs and Huber10–Reference Stenius, Swartz and Lilja13). However, the evidence remains sparse and controversial(Reference Batra, Sharma and Gupta14).
Despite the complexity of characterising organic food consumers(Reference Pearson, Henryks and Jones5), their profiles have been reported in numerous studies mainly in adulthood. Such consumers tend to be older and female, have a high education level, have children and follow an overall healthy lifestyle (compliance with dietary recommendations and regular physical activity, no smoking)(Reference Baudry, Mejean and Peneau2,Reference Pearson, Henryks and Jones5) . Except for a previous study of pregnant women(Reference Torjusen, Brantsaeter and Haugen15), little is known about consuming organic foods in the perinatal period and the associated family characteristics. This previous study showed that socio-economic characteristics related to frequent consumption of organic foods during pregnancy were not just those usually related to healthier behaviours: women with both low and high education and in the lowest income group were more likely to eat organic foods than other women.
Infant feeding practices are known to affect numerous aspects of health in later life(Reference Martin, Ling and Blackburn16–Reference Victora, Bahl and Barros20). However, several aspects of feeding practices such as breast-feeding duration, age at complementary feeding introduction and type of foods used in infancy are inter-related(Reference Betoko, Charles and Hankard21) and known to be associated with family characteristics and the health status of the infant(Reference Betoko, Charles and Hankard21–Reference Smithers, Brazionis and Golley23). Organic food consumption is associated with a healthy lifestyle(Reference Mie, Andersen and Gunnarsson11), so we should examine the links between feeding organic foods during the complementary feeding period and other feeding practices.
The aim of the present study was to describe the choice of organic foods for complementary feeding in a large nationwide birth cohort and its association with family characteristics and other infant feeding practices.
Materials and methods
Study population
The present analysis was based on data from the Étude Longitudinale Française depuis l’Enfance (ELFE) study, a nationally representative birth cohort that included 18 329 children born in a random sample of 349 maternity units in France in 2011(Reference Charles, Thierry and Lanoe24). From April 2011, inclusion took place during twenty-five selected recruitment days over four waves of 4–8 d each and covering all four seasons. Inclusion criteria were birth after 33 weeks’ gestation to mothers aged 18 years or older who were not planning to move outside of metropolitan France (i.e. the area of the French Republic, which is geographically in Europe) in the following 3 years. Data were collected in standardised interviews conducted by trained interviewers and self-completed questionnaires.
Mothers were interviewed in the maternity ward for medical information about their pregnancy and their newborn, sociodemographic and lifestyle-related characteristics, and eating habits during pregnancy. Additional information was collected from obstetric and paediatric medical files. At 2, 12 and 24 months post-partum, telephone interviews with mothers and fathers collected data on infant feeding and more details on demographic and socio-economic characteristics. From 3 to 10 months after delivery, families were asked to complete a monthly questionnaire via the Internet (70 %) or by paper that asked about the infant’s diet (feeding methods, food and beverage introduction).
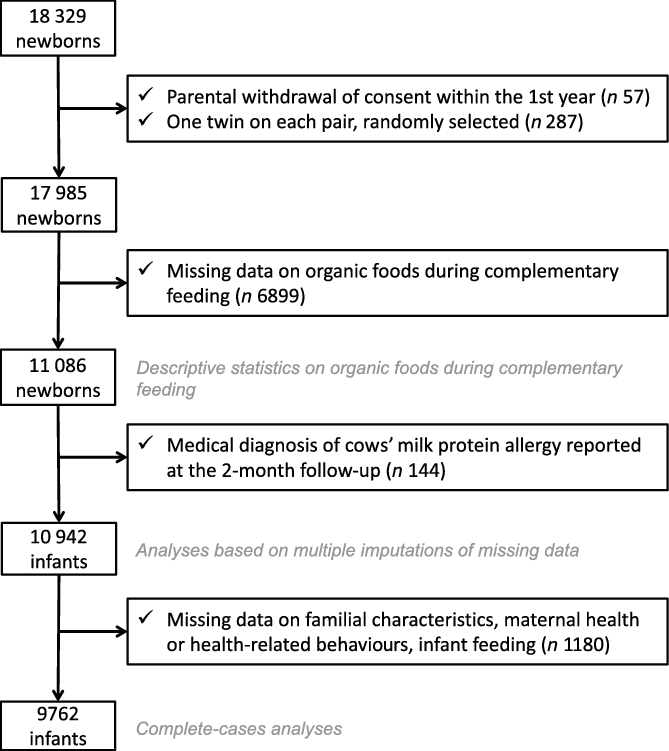
Fig. 1. Flow chart.
Ethical approval
Participating mothers provided written consent for themselves and their child. When present at inclusion, fathers signed the consent form for the child’s participation or were informed about their right to oppose it. The ELFE study received approvals from the Advisory Committee for the Treatment of Information on Health Research (Comité Consultatif sur le Traitement des Informations pour la Recherche en Santé), the National Agency Regulating Data Protection (Commission Nationale Informatique et Libertés) and the National Statistics Council.
Family characteristics assessment
Parental sociodemographic characteristics of interest were maternal migration status (migrant, descendant of migrant, majority population), age at delivery (18–25, 25–29, 30–34, ≥35 years), number of older children in the household (ELFE child is the first child, one older child, at least two older children), single parenthood, maternal education level (up to lower secondary, upper secondary, intermediate, 3-year university degree, at least 5-year university degree), monthly family income per consumption unit(25) (≤€750, €751–1111, €1112–1500, €1501–1944, €1945–2500, >€2500), employment status during pregnancy (employed, unemployed, out of the labour force (housewife/student/retired/disabled)) and motives for choice of feeding method (breast or formula milk) at birth: child’s health or well-being/practical reasons/interaction with infant/usual feeding method/other or unknown. Maternal health characteristics included self-reported height and pre-pregnancy weight, maternal smoking during pregnancy (never smoker, smoker only before pregnancy, smoker in early pregnancy and smoker throughout pregnancy).
During the hospital stay, the recruited women (n 18 042) were asked to complete a self-administered FFQ to describe their dietary intake over the last 3 months of their pregnancy(Reference de Gavelle, de Lauzon-Guillain and Charles26). A diet quality score, based on the consumption of the main food groups, was calculated by using seventeen quantitative benchmarks as previously described(Reference Kadawathagedara, Kersuzan and Wagner27).
Infant characteristics
Newborn characteristics were collected from the medical record: sex, twin birth, gestational age and birth weight. Medical diagnosis of the infant’s allergy to cows’ milk protein was also collected from the parents with the 2-month questionnaire.
Infant feeding
Details on milk feeding practices were collected monthly from 2 to 10 months and then at 12 and 24 months. From these data, any breast-feeding duration and age at infant formula introduction were calculated as previously described(Reference Wagner, Kersuzan and Gojard28).
Details on complementary feeding practices were collected monthly from 3 to 10 months. We calculated the age of introduction of thirteen food groups (fruits, vegetables, potatoes, water, fruit juice, infant cereals, meat, fish, eggs, bread and pasta, dairy products, cows’ milk and dessert), along with the age of introduction of unmixed meat and crushed vegetables and fruits, as previously defined(Reference Bournez, Ksiazek and Wagner22). Each month, the parents reported the frequency of use of organic foods to feed their infant during the last month (0 – never; 1 – sometimes; 2 – often; 3 – always or almost always), as well as the frequency of use of commercial complementary foods to feed their infant during the last month. The frequency of feeding with organic foods during complementary feeding was individually summarised as the median frequency of feeding with organic foods reported between the age of introduction to complementary foods and age 10 months. The frequency of feeding with commercial complementary foods was individually summarised as the median frequency of feeding with commercial complementary foods reported between the age of introduction to complementary foods and age 10 months. Among families completing the 3- to 10-month questionnaires, 86 % of children had at least five collection points for organic foods.
Sample selection
Children whose parents withdrew consent (n 57) were excluded from the study (Fig. 1). We randomly selected one twin of two (n 287) to avoid family clusters. We excluded children whose frequency of consumption of organic foods was missing, as they did not complete the 3–10-month questionnaire or did not provide enough information to summarise intake during complementary feeding (n 6899), which left 11 086 children to compute national statistics on feeding with organic foods during complementary feeding.
To analyse the associations between familial/infant characteristics and frequency of feeding with organic foods, we excluded children with a medical diagnosis of allergy to cows’ milk protein reported at the 2-month follow-up (n 144) because it might deeply affect infant feeding. After excluding children with missing data on family or infant characteristics (n 1180), the complete-cases analysis was based on 9762 children. The analyses accounting for maternal diet quality during pregnancy involved 8985 children, and those accounting for other feeding practices involved 8588 children.
As compared with the 9762 included children, excluded children often had younger mothers (30·2 (sd 5·6) v. 31·3 (sd 4·6) years, P < 0·0001) with lower education level (14·7 % v. 23·5 % with a Master’s degree, P < 0·0001) and lower income (mean €1423 (sd 1033) v. €1751 (sd 979) per consumption unit, P < 0·0001). They more frequently had two or more siblings (22·7 v. 16·5 %, P < 0·0001), an immigrant mother (15·9 v. 6·5 %, P < 0·0001) and a mother who smoked throughout pregnancy (21·0 v. 12·4 %, P < 0·0001).
Statistical analyses
To provide representative descriptive statistics of births in 2011 in metropolitan France, the data (rates of choosing organic food) were weighted to take into account the inclusion procedure and biases related to non-consent(Reference Juillard29). Weighting also included calibration on margins from the state register’s statistical data and the 2010 French National Perinatal study(Reference Blondel, Lelong and Kermarrec30) on the following variables: age, region, marital status, migration status, level of education and primiparity. This weighting was calculated for the subsample that completed the questionnaire on infant diet at least once from 3 to 10 months.
Bivariate associations between family characteristics and frequency of feeding with organic foods were analysed with χ 2 tests and those between infant feeding practices and frequency of feeding with organic foods with ANOVA. Multivariable associations between familial or infant characteristics and frequency of feeding with organic foods (never, sometimes, often, always or almost always) were assessed by multinomial logistic regression, simultaneously including the family characteristics presented previously and additionally adjusted for variables related to study design (mother’s region of residence, size of maternity unit and wave of recruitment). Not feeding with organic foods during complementary feeding was considered the reference category. Analyses were conducted with a three-step approach. First, only maternal sociodemographic characteristics were considered simultaneously: age, education level, migration status, single motherhood, number of children in the household, employment during pregnancy and household income. In addition to sociodemographic characteristics, analyses included maternal health and health-related behaviours: smoking status during pregnancy, pre-pregnancy BMI, diet quality during pregnancy and motives for choice of initial feeding method. In a final model, infant characteristics and infant feeding practices were considered simultaneously: sex, birth weight-for-gestational age, any breast-feeding duration, age at complementary feeding introduction and frequency of feeding with commercial complementary foods.
To deal with selection and attrition bias, we performed a sensitivity analysis with weighted data according to the weighting described previously on the complete-cases sample. Because the main analyses were based on the complete-cases sample, we also performed a sensitivity analysis using multiple imputation to deal with missing data on family characteristics. We assumed that data were missing at random and generated five independent data sets with the fully conditional specification method (SAS software: MI procedure, FCS statement, NIMPUTE option) and then calculated pooled effect estimates (SAS software: MIANALYSE procedure). In imputation models, we included all variables of interest after ranking them in ascending order of missing data. Categorical variables were imputed with a multinomial model, ordinal or binary variables with logistic regression, and continuous variables with linear regression. These sensitivity analyses involved data for all participants with data on organic foods choice for complementary feeding (n 10 945). To generate significance testing of categorical variables, the median of the P values from the imputed data analyses in each data set was used, as proposed by Eekhout et al. (Reference Eekhout, van de Wiel and Heymans31).
All analyses involved using SAS V9.4 (SAS).
Results
Descriptive statistics
For the 11 086 infants with data on organic foods, the weighted frequencies of feeding with organic foods between complementary food introduction and 10 months were: never 51·3 (95 % CI 50·1, 52·6) %, sometimes 24·0 (95 % CI 22·9, 25·0) %, often 15·2 (95 % CI 14·4, 16·1) % and always or almost always 9·5 (95 % CI 8·8, 10·1) %.
Maternal sociodemographic and socio-economic characteristics
Family and infant characteristics were compared by frequency of feeding with organic foods during complementary feeding (Table 1).
Table 1. Family and infant characteristics by choice of organic foods for complementary feeding*
(Numbers and percentages; mean values and standard deviations, n 9762)
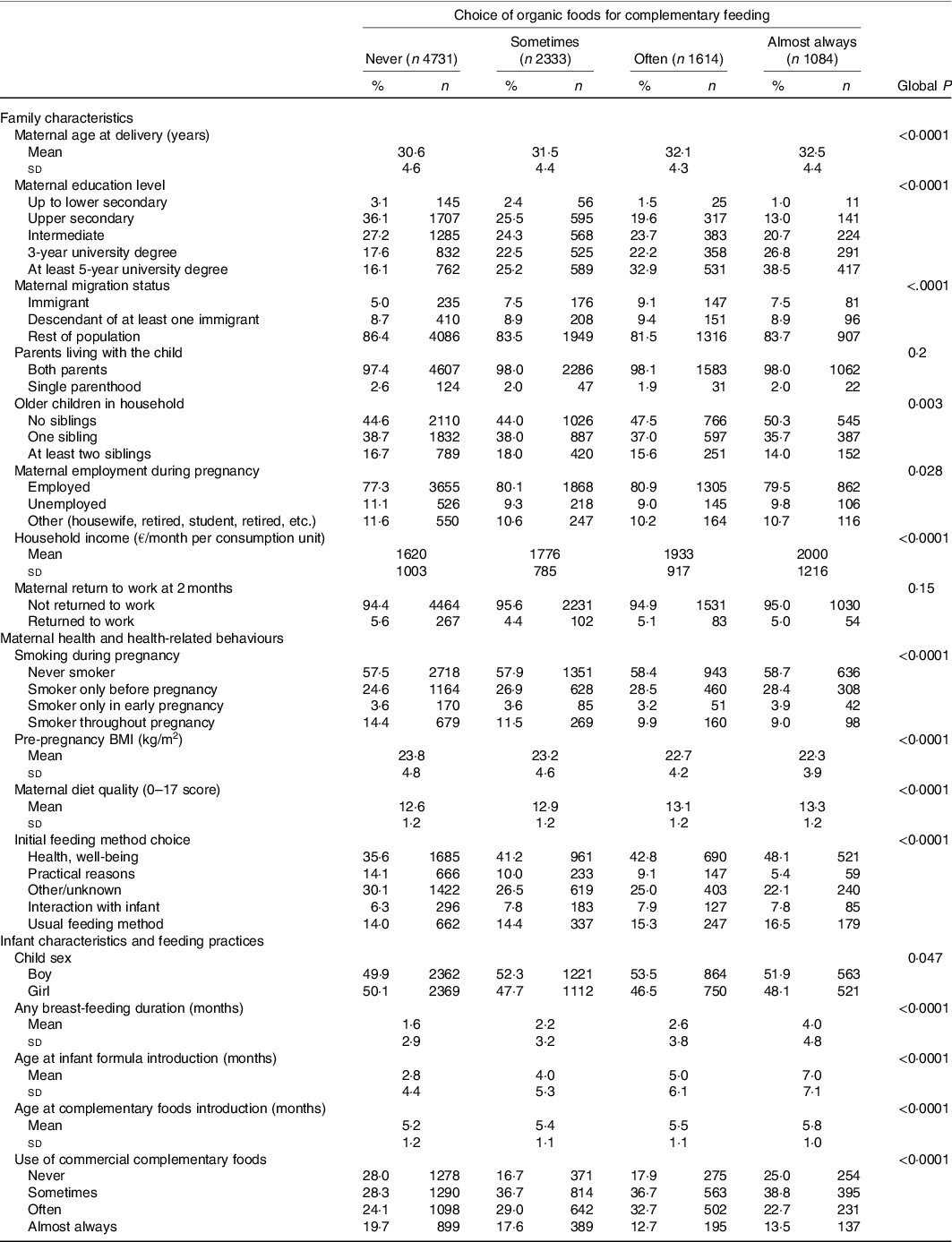
* Associations with frequency of feeding with organic foods were analysed using χ 2 tests for categorical variables and ANOVA for continuous variables.
On multivariable analysis (Table 2), as compared with no feeding with organic foods, the frequency of feeding with organic foods was positively associated with maternal age, education level and household income. Immigrant women were more likely to feed their infant organic foods, but the association was only statistically significant for ‘sometimes’ and ‘often’ categories. Unemployed mothers were more likely to always feed their infant organic foods when adjusted for family income and other characteristics. Single parenthood and maternal return to work at 2 months were not associated with frequency of feeding with organic foods. Finally, families with older siblings were less likely to feed their infant organic foods often or always.
Table 2. Multivariable associations between family characteristics and feeding with organic foods during complementary feeding*
(Odds ratios and 95 % confidence intervals, n 9762)
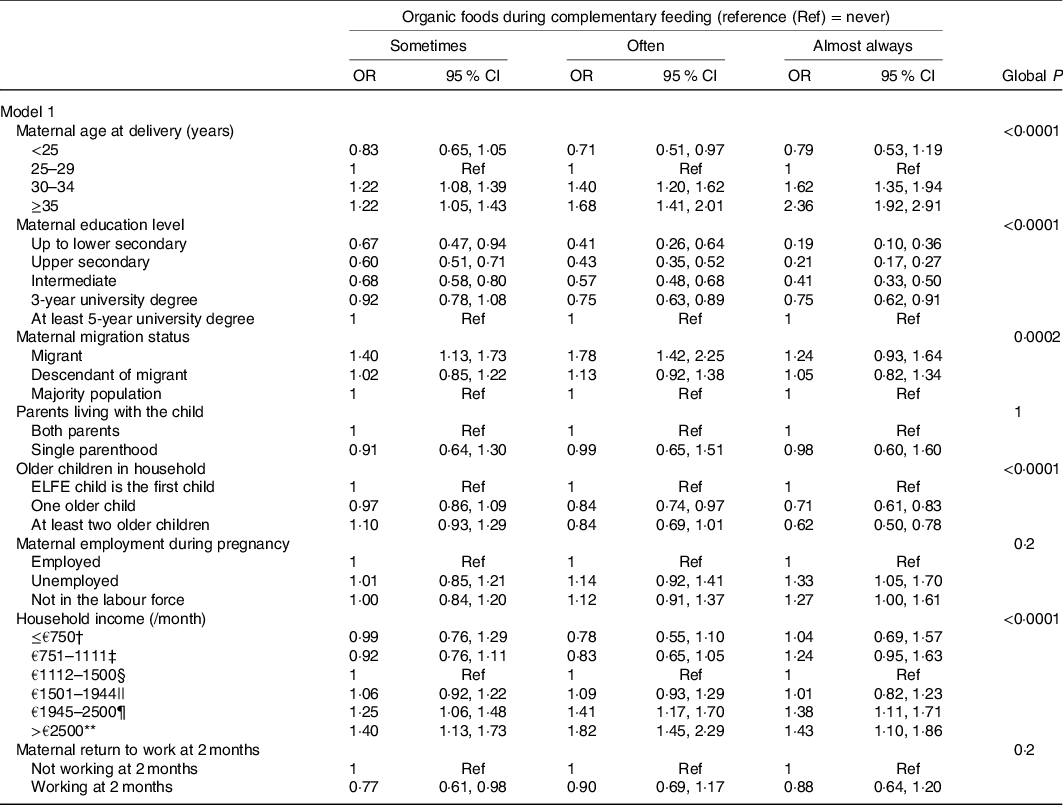
ELFE, Étude Longitudinale Française depuis l’Enfance.
* Multinomial logistic regression including all variables indicated in the table simultaneously and also adjusted for variables related to study design (region, maternity unit size and wave of recruitment).
† Corresponding to (in US$) ≤$815/month.
‡ Corresponding to $816–1207/month.
§ Corresponding to $1208–1630/month.
|| Corresponding to $1631–2113/month.
¶ Corresponding to $2114–2717/month.
** Corresponding to >$2717/month.
Health, motives and health-related behaviours
As compared with women who never smoked, those who stopped smoking before pregnancy or in early pregnancy were more likely to always feed their infant organic foods (Table 3, model 2). Children born to mothers with overweight or obesity were less likely to be fed organic foods than those born to women with normal weight. Likelihood of feeding with organic foods was associated with maternal diet quality during pregnancy. Finally, likelihood of feeding with organic foods was reduced for children of women who initially chose their infant feeding method (breast- or formula feeding) for practical or ‘other reasons’ rather than for their child’s health or well-being.
Table 3. Multivariable associations between maternal health and health-related behaviours (model 2) or infant characteristics and feeding practices (model 3) and feeding with organic foods during complementary feeding*
(Odds ratios and 95 % confidence intervals)
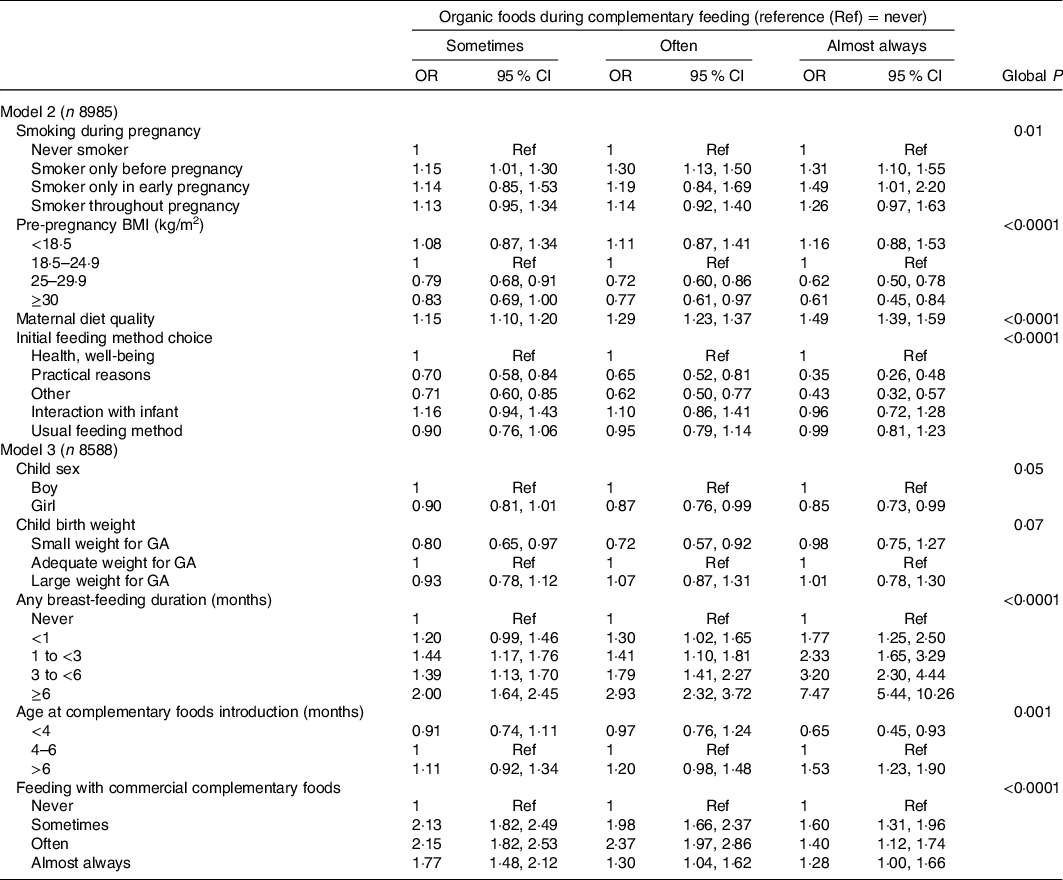
GA, gestational age.
* From multinomial logistic regressions including all variables indicated in the table simultaneously and also adjusted in models 2 and 3 for family characteristics (maternal age, education level, migration status, employment during pregnancy, return to work at 2 months, single parenthood, number of children in the household, household income) and variables related to study design (region, maternity size and wave of recruitment), and in model 3 for maternal health and health-related behaviours (smoking during pregnancy, pre-pregnancy BMI, diet quality during pregnancy, motives for feeding method).
Infant characteristics and infant feeding practices
The model further accounting for infant characteristics is shown in Table 3 (model 3). Girls were less likely to almost always be fed organic foods than boys but not significantly (P = 0·08, Table 3). Infants born small-for-gestational-age were less likely to be fed ‘sometimes’ or ‘often’ with organic foods than their adequate-for-gestational-age counterparts. The frequency of feeding with organic foods was strongly and positively related to any breast-feeding duration and was positively related to age at complementary foods introduction, especially introduction to complementary foods after age 6 months. Infant fed with commercial complementary foods was more likely to be fed with organic foods than infant never fed with commercial complementary foods, but the association between commercial complementary foods and organic foods was quite complex. In fact, the association was stronger for infants consuming commercial complementary food ‘sometimes’ or ‘often’ than ‘almost always’. Moreover, within each frequency of feeding with commercial complementary foods, the association was stronger for intermediate frequency of feeding with organic foods than for high frequency.
Discussion
To our knowledge, this study is the first to characterise feeding with organic foods during complementary feeding and the associated family characteristics or feeding practices during the first year of life. Beyond its positive association with several indicators of socio-economic position, the frequency of feeding with organic foods was strongly related to other infant feeding practices such as long breast-feeding duration and introduction to complementary foods after age 6 months. Furthermore, feeding the infant organic foods was related to maternal health concerns such as smoking cessation before pregnancy.
Frequency of feeding with organic foods during complementary feeding
Published data on the consumption of organic foods in the perinatal period are sparse. The prevalence of organic food consumption by infants born in 2011 in the ELFE study is consistent with that found in literature (although the data collection methods are different), with half of infants never fed organic foods and 25 % often or always fed organic foods. Only one study provided statistics on organic food consumption in the first years of life: in the KOALA Birth Cohort study (beginning in 2000), 16 % of infants consumed a diet with at least 50 % organic foods in their first 2 years of life(Reference Kummeling, Thijs and Huber10). More data are available on organic food consumption during pregnancy. In the KOALA Birth Cohort study, many pregnant women (86 %) consumed a diet based on conventional foods and 14 % a diet with at least 50 % organic foods(Reference Kummeling, Thijs and Huber10). In the Norwegian Mother and Child Cohort Study (MoBa, recruitment from 1999 through 2008), about half of women never/seldom ate organic foods during pregnancy as compared with 16 % who often ate organic foods(Reference Brantsaeter, Torjusen and Meltzer9). In the Danish National Birth Cohort (recruitment between 1996 and 2002), an estimated 56 % of pregnant women were non- or low organic food consumers and 7 % frequent consumers(Reference Petersen, Rasmussen and Strom32).
Sociodemographic characteristics and feeding with organic foods during complementary feeding
The frequency of feeding with organic foods during complementary feeding has never been described. Therefore, we compared our findings with correlates and motives reported in adult populations (including pregnant women). Consistent with the literature, feeding with organic foods was related to increased maternal age(Reference Petersen, Rasmussen and Strom32–Reference Kesse-Guyot, Peneau and Mejean34) and education level(Reference Dimitri and Dettmann35,Reference Simoes-Wust, Molto-Puigmarti and van Dongen36) and related to increased household income, even if the association with income and organic foods could be stronger for some food groups (e.g. vegetables) than others (e.g. milk)(Reference Dimitri and Dettmann35). However, in the MoBa study, the consumption of organic foods during pregnancy was related to both younger and older age as well as low education level and low household income(Reference Petersen, Rasmussen and Strom32). In the ELFE study, after adjustment for education level and family income, maternal employment was negatively related to feeding with organic foods.
Households with children seemed more likely to purchase organic foods than those without children(Reference Hughner, McDonagh and Prothero33), but in the ELFE study, parents with older children less likely fed their infant organic foods as compared with those without older children. In the MoBa study, pregnant women with an older child were more likely to consume organic foods than primiparous women, whereas those with at least two previous children were less likely to consume organic foods(Reference Petersen, Rasmussen and Strom32), which suggests that the association between parity and choice of organic foods is complex and depends on the population.
The accessibility and availability of organic foods is strongly associated with organic food consumption(Reference Hughner, McDonagh and Prothero33,Reference Bartels and Reinders37–Reference Lockie, Lyons and Lawrence40) , but unfortunately such an information was not available in the ELFE study.
Maternal health and health-related behaviours and feeding with organic foods during complementary feeding
In the ELFE study, frequent feeding with organic foods during complementary feeding was related to maternal health and health-related behaviours, assessed by maternal weight status, smoking cessation and health concerns such as motives for choice of initial infant feeding method. In the literature, the inverse association between BMI and consumption of organic foods was consistent across studies(Reference Torjusen, Brantsaeter and Haugen15,Reference Petersen, Rasmussen and Strom32,Reference Kesse-Guyot, Peneau and Mejean34,Reference Simoes-Wust, Molto-Puigmarti and van Dongen36,Reference Simoes-Wust, Molto-Puigmarti and Jansen41) . The association with smoking seems complex: some studies highlighted higher consumption of organic foods among former or present smokers than non-smokers(Reference Torjusen, Brantsaeter and Haugen15,Reference Kesse-Guyot, Peneau and Mejean34) but not all(Reference Simoes-Wust, Molto-Puigmarti and Jansen41). In the last study, with about 5 % women smoking during pregnancy, no association was found with active smoking, but women consuming organic foods were less likely to be exposed to passive smoking than women consuming conventional foods(Reference Simoes-Wust, Molto-Puigmarti and Jansen41). In the MoBa study, occasional smokers were more likely to consume organic foods during pregnancy than were non-smokers, but the reverse was found for regular smokers(Reference Petersen, Rasmussen and Strom32). Stronger health concerns were often observed among organic food consumers than others(Reference Kushwah, Dhir and Sagar4,Reference Pearson, Henryks and Jones5,Reference Hughner, McDonagh and Prothero33,Reference Bartels and Reinders37,Reference Lockie, Lyons and Lawrence40,Reference Baudry, Peneau and Alles42–Reference Nie and Zepeda44) . High diet quality was also related to increased likelihood of organic food consumption(Reference Baudry, Mejean and Peneau2,Reference Petersen, Rasmussen and Strom32,Reference Kesse-Guyot, Peneau and Mejean34,Reference Simoes-Wust, Molto-Puigmarti and van Dongen36,Reference Baudry, Alles and Peneau45–Reference Torjusen, Lieblein and Naes50) . Overall, these aspects suggested a cluster of healthy behaviours.
Organic foods and infant feeding during the first year of life
Organic food consumers appeared to have a diet more in line with nutritional guidelines(Reference Kesse-Guyot, Peneau and Mejean34) and high awareness for some nutritional guidelines(Reference Baudry, Mejean and Peneau2). Moreover, consumers of organic foods are more likely to have a healthy lifestyle(Reference Baudry, Mejean and Peneau2,Reference Petersen, Rasmussen and Strom32,Reference Kesse-Guyot, Peneau and Mejean34,Reference Eisinger-Watzl, Wittig and Heuer48–Reference Goetzke, Nitzko and Spiller51) . These findings in adults appeared consistent with the associations between extended breast-feeding (recommended by international societies(Reference Agostoni, Braegger and Decsi52,53) ) or low likelihood of early complementary food introduction (<4 months) and feeding with organic foods. In this cohort, breast-feeding duration was not independent from age at complementary feeding(Reference Bournez, Ksiazek and Wagner22), but the association between organic foods and breast-feeding duration denotes specific attitudes regarding child feeding. However, feeding with organic foods was also related to late complementary food introduction (>6 months), which is not recommended by international societies.
Strengths and limitations
The ELFE cohort is a nationwide study of birth in 2011 in metropolitan France (excluding very premature babies). The main analyses were conducted on a complete-cases sample. However, when missing data on family characteristics were addressed by the multiple imputation method, results remained consistent. Moreover, the sample considered for the present analysis was based on more advantaged families than the initial ELFE sample, which limits the generalisability of our results. However, sensitivity analysis based on weighted data, which deals with part of the selection and attrition biases, provided similar findings, which suggests that these biases had limited impact on our results. The main strengths of the ELFE study include the large sample size and the wide range of sociodemographic and socio-economic variables and profiles. Moreover, data collection was repeated and prospective throughout infancy, thus limiting the memory bias regarding infant diet. Consumption of organic foods during complementary feeding was assessed with only one item (not making possible to identify whether organic foods were commercial or home-made complementary foods), repeated each month from 3 to 10 months, and based only on feeding at home, which allowed for only a quantitative assessment of infant exposure. However, this is the first study with data on organic food consumption during complementary feeding, and the frequency of consumption of organic foods was consistent with previous studies in the perinatal period(Reference Kummeling, Thijs and Huber10,Reference Petersen, Rasmussen and Strom32,Reference Brantsaeter, Ydersbond and Hoppin54) .
Conclusion
About a quarter of infants were fed organic foods (often or always) during the complementary feeding period in France in 2011–2012, as assessed by the ELFE data. Beyond the positive association of organic food feeding and several indicators of the family socio-economic position, organic food feeding was strongly associated with infant feeding practices, in particular long breast-feeding duration and introduction to complementary foods beyond 6 months. All these characteristics need to be carefully considered when studying the potential role of organic food consumption on children’s subsequent health and development.
Acknowledgements
We thank the scientific coordinators (B. Geay, H. Léridon, C. Bois, J. L. Lanoé, X. Thierry, C. Zaros), IT and data managers, statisticians (M. Cheminat, C. Ricourt, A. Candea, S. de Visme), administrative and family communication staff, and study technicians (C. Guevel, M. Zoubiri, L. G. L. Gravier, I. Milan, R. Popa) of the ELFE coordination team as well as the families that gave their time for the study.
The ELFE survey is a joint project between the French Institute for Demographic Studies (INED) and the French National Institute of Health and Medical Research (INSERM), in partnership with the French blood transfusion service (Etablissement français du sang, EFS), Santé publique France, the National Institute for Statistics and Economic Studies (INSEE), the Direction générale de la santé (DGS, part of the Ministry of Health and Social Affairs), the Direction générale de la prévention des risques (DGPR, Ministry for the Environment), the Direction de la recherche, des études, de l’évaluation et des statistiques (DREES, Ministry of Health and Social Affairs), the Département des études, de la prospective et des statistiques (DEPS, Ministry of Culture) and the Caisse nationale des allocations familiales (CNAF), with the support of the Ministry of Higher Education and Research and the Institut national de la jeunesse et de l’éducation populaire (INJEP). Via the RECONAI platform, it receives a government grant managed by the National Research Agency under the ‘Investissements d’avenir’ programme (ANR-11-EQPX-0038).
This study is funded by an ANR grant (InfaDiet project, no ANR-19-CE36-0008).
The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
B. L. G. and F. G. conceptualised and designed the work, conducted the statistical analyses, drafted the initial manuscript and approved the final manuscript as submitted. A. C. and C. D. P. conducted part of the statistical analyses, critically reviewed the manuscript and approved the final manuscript as submitted. B. L. G., S. L., S. N. and M. A. C. designed nutritional data collection instruments, supervised their data collection and data management, critically reviewed the manuscript and approved the final manuscript as submitted. M. A. C. coordinated the ELFE cohort management team. E. K. G. conceptualised and designed the work, contributed to the interpretation of the study, reviewed and revised the manuscript and approved the final manuscript as submitted.
The authors had no conflicts of interest relevant to this article to disclose.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114520005097







