As many low- and middle-income countries, Colombia currently faces a rapid rise in the prevalence of childhood overweight and obesity, together with relatively high rates of childhood stunting in both urban and rural areas (national average 14·9 %)( Reference Isanaka, Mora-Plazas and Lopez-Arana 1 , Reference Parra, Iannotti and Gomez 2 ). This so-called ‘double burden of malnutrition’( Reference Tzioumis and Adair 3 ) has resulted from a nutrition transition to energy-dense diets that are high in saturated fat, sugar and refined foods, inadequate access to healthy food choices and sedentary lifestyles( Reference Hughes, Sherriff and Ness 4 ). Parallel to these trends, many low- and middle-income countries have introduced cash-transfer programmes (conditional and unconditional), which aim to break the intergenerational transmission of poverty by providing monetary transfers to poor families( Reference Forde, Rasanathan and Krech 5 – Reference Schubert and Slater 9 ). Practically every country in Latin America, including Colombia, has a conditional cash-transfer programme (CCT), whereas in some African and Asian nations both conditional and unconditional cash-transfer programmes have also been implemented and have shown positive effects( Reference Aguero, Carter and Woolard 8 – Reference Robertson, Mushati and Eaton 14 ).
Several studies have shown that CCT programmes have positive effects on child health and nutritional outcomes( Reference Gertler 15 – Reference Handa and Davis 17 ). CCT programmes may do so by increasing family income, raising compliance with growth and preventive-care check-ups( Reference Lagarde, Haines and Palmer 7 , Reference Fernald, Gertler and Neufeld 18 , Reference Black, Victora and Walker 19 ), and improving knowledge and awareness of caregiving practices through workshops( Reference Barber and Gertler 20 , Reference Gaarder, Glassman and Todd 21 ). In Brazil, a reduction in under-5 mortality has been attributed to the large CCT Bolsa Familia programme( Reference Rasella, Aquino and Santos 22 ). Likewise, CCT programmes have been linked to reductions in childhood illness in Mexico and Malawi( Reference Lagarde, Haines and Palmer 7 , Reference Schubert and Slater 9 , Reference Handa and Davis 17 , Reference Gertler and Boyce 23 ). Evidence also suggests that CCT programmes improve the quality of diet by increasing household fruit and vegetable consumption( Reference Attanasio and Mesnard 11 , Reference Leroy, Ruel and Verhofstadt 24 , Reference Bassett 25 ). Yet, some evidence suggests that cash transfers may also increase intake of unhealthy foods associated with chronic diseases( Reference de Bem Lignani, Sichieri and Burlandy 26 ), contributing to rising trends in BMI. For example, a study among adults in Colombia concluded that CCT’s had increased the risk of obesity among mothers( Reference Forde, Chandola and Garcia 27 ); likewise, evidence from Mexico’s Oportunidades (now Prospera) suggests that CCT’s may increase the consumption of fruits and vegetables, but also lead to excess energy consumption( Reference Leroy, Gadsden and Rodriguez-Ramirez 28 ). Concerns have thus been raised that providing cash to poor families may have unintended negative consequences on nutrition, increasing the risk of overweight and obesity( Reference Fernald 10 , Reference Morris, Olinto and Flores 29 ).
In 2002, the Government of Colombia introduced the CCT programme Familias en Acción (FA) targeting poor households with children aged 0–17 years( Reference Attanasio and Mesnard 11 , Reference Forde, Chandola and Garcia 27 ). At present, the FA programme serves 2·8 million households, covering a quarter of the Colombian population and over half of the nation’s poor( 30 ). Early evidence from FA suggests that this programme was associated with a 16·5 % increase on the purchase of protein-rich foods, as well as with increased height for age (0·16 z-score) among the youngest and poorest children( Reference Attanasio and Mesnard 11 , Reference Attanasio, Benavides and Borda 31 , Reference Attanasio, Gómez and Heredia 32 ). Nonetheless, less is known about the potential effects of CCT programmes in Colombia on the double burden of malnutrition among children of pre-school and school age, a sensitive period that may have implications for outcomes later in life( Reference Campbell, Conti and Heckman 33 ). In this study, we evaluated the impact of the FA CCT programme on under- and over-nutrition in children from poor households in Colombia. We hypothesised that cash transfers would reduce rates of stunting and underweight, while also increasing the risk of overweight and obesity.
Methods
Study population and design
Data were obtained from the evaluation of the FA programme up to 2006( Reference Attanasio, Benavides and Borda 31 ). In brief, the FA programme is a large-scale intervention that provides cash to mothers of poor households. The programme has two components: health and education. The health component provides cash to the mothers on the condition that their children younger than 7 years of age regularly attend vaccination programmes as well as growth and development check-ups. The educational component requires that children aged 7–17 years regularly attend school. For example, in 2002, families with children under 7 years received 40 000 Colombian pesos (COP) monthly (13 % of the minimum wage) and this amount has been increased to 63 525–74 100 COP (10–11·5 % of the minimum wage) (about US$32–US$38) for children who attend vaccination, growth and development check-ups, whereas families with children aged 7–17 years received between 14 000 and 28 000 COP in 2002 and are receiving 10 600–58 225 COP currently (about US$13–US$30) for each child that attends at least 80 % of school lessons at the primary and secondary level. Eligibility for the CCT programme is determined based on a scoring system known as the System for Identifying and Selecting Beneficiaries, a survey of low-income households used to derive a poverty score that ranges from 0 to 100 and enables targeting social-welfare programmes( Reference Forde, Chandola and Garcia 27 , Reference Paes-Sousa, Regalia and Stampini 34 ). Implementation of the programme includes operational units at the national, departmental and municipality levels. The programme is managed and implemented by a National Coordinating Unit, but Regional Coordinating Units in each department manage the programme and liaise with the national and municipal governments. Programme monitoring is a joint responsibility of departmental and municipality governments and includes a comprehensive monitoring system that follows families through the various stages of programme implementation, such as (1) beneficiaries’ registration and status, (2) compliance with programme conditions, (3) payment of transfers and (4) complaints and case management( Reference Paes-Sousa, Regalia and Stampini 34 ). Municipal Liaison Offices verify that mothers meet the conditions. If a mother fails to meet the requirements three consecutive times, she could be dismissed from the programme. The money is periodically transferred to the bank account of the beneficiaries( Reference Paes-Sousa, Regalia and Stampini 34 ).
In 2001, 622 municipalities from a total of 1060 Colombian municipalities were selected to implement the programme because they fulfilled the following criteria: (1) a population of <100 000 inhabitants, (2) health and education infrastructure to guarantee programme implementation, (3) a bank to enable cash transfers and (4) up-to-date census, welfare and service infrastructure data. Apart from living in a municipality where the programme was implemented, families were required to (1) hold a Colombian citizen card, (2) have children younger than 18 years of age and (3) be formally classified in the lowest level of the official socio-economic classification in December 1999. At the beginning of the programme, 360 000 households fulfilled the criteria and were included in the programme( Reference Attanasio, Benavides and Borda 31 ). To assess the impact of the programme, an evaluation was carried out by the Institute of Fiscal Studies, an independent research institute in London (UK). Details of the evaluation are available elsewhere( Reference Attanasio, Benavides and Borda 31 ). In brief, fifty-seven treatment municipalities from the 622 municipalities implementing the programme were selected. These were compared with sixty-five matched control municipalities that were not targeted to receive the programme yet. In practice, except for the requirement to have a bank, control municipalities fulfilled all other eligibility criteria, and were thus comparable with treatment municipalities.
Baseline assessments were scheduled to take place in 2002 before the programme started, but owing to political pressure the programme started before baseline assessment in twenty-six out of the fifty-seven treatment municipalities( Reference Attanasio, Benavides and Borda 31 ), and therefore were excluded from the primary analysis in this study (Fig. 1).
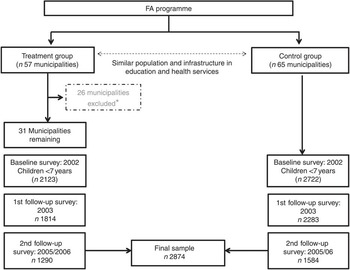
Fig. 1 Participant flowchart, Familias en Acción, conditional cash transfer programme, Colombia. * Twenty-six municipalities were excluded due to the programme having started before baseline assessment.
Complete anthropometric information was available for 5591 children aged 2–6 years (from a total of 6039 of eligible participants). We excluded 746 children with missing covariates at baseline, leaving a baseline sample of 2123 treated and 2722 control children. A first follow-up assessment was carried out in 2003 and included 1814 children in the treatment group and 2283 in the control group who had previously been measured in 2002. Finally, a second follow-up assessment was carried out between 2005 and 2006, and comprised 1290 children in treatment municipalities and 1584 in the control group, with valid data for weight and height in all the observed periods, and is the final sample for this longitudinal analysis. Differences in attrition are reported in the online Supplementary Table S1. Overall, we found that baseline characteristics of children and mothers lost to follow-up were similar to those of mothers and children remaining in follow-up. However, children lost to follow-up were slightly older (5·1 v. 4·4 years, P value<0·0001), less likely to be overweight (14·1 v. 16·5 %, P value 0·02) and had lower BMI-for-age z-scores (BMI z-scores) (0·12 v. 0·22 z-score, P value 0·001). However, missing status was not significantly associated with treatment or control status.
Outcome measures
Height and weight of children were measured by trained fieldworkers using a protocol of the Pan-American Health Organization Manual on Anthropometrics( Reference Lohman, Roche and Martorell 35 ). Weight was measured using electronic scales (Seca 770; Vogel & Halke) with a precision of 0·1 kg. Height was measured using measuring boards with a precision of 0·1 cm (Shorr Productions). BMI was computed as weight in kilograms divided by the square of height in metres. We calculated height-for-age z-scores (HAZ) and BMI z-scores, based on the WHO Child Growth Standards( Reference de Onis, Martorell and Garza 36 , Reference de Onis, Onyango and Borghi 37 ). These references are being used in Colombia since 2010( 38 ). Two different outcome measures were defined: the HAZ and BMI z-score as a continuously distributed variable and a categorical variable with the following categories: stunting (HAZ<–2), thinness (BMI z-score<–2), normal (BMI z-score between −1 and +1), overweight (BMI z-score>+1) and obese (BMI z-score>+2). In this categorisation, overweight includes obesity as well.
Covariates
Covariates at the individual, household and municipality level were used as control variables. Children’s individual characteristics included age, sex and whether the child was participating in Hogares Comunitarios, a home-based childcare supplementary nutrition and psychosocial stimulation programme for children from poor families. We controlled for maternal characteristics including the mother’s educational attainment, marital status, age and BMI. Mothers’ highest level of completed education was categorised into the following groups: (1) no education, (2) incomplete primary, (3) completed primary, (4) incomplete secondary, (5) completed secondary and (6) higher education. Covariates also included household size and household income at baseline, measured by asking respondents their income from all sources in the past month, including wages, salaries, retirement benefits, help from relatives and rent from property. In regression models, household income was log-transformed to account for non-linearities. At the municipality level, models included number of inhabitants, level of urbanisation and geographical region categorised into (1) Central region, (2) Caribbean region, (3) Pacific region and (4) Eastern region.
Ethical considerations
Ethics approval for the evaluation study was granted by a local institutional ethics committee. Adults provided signed informed consent to participate in the study. Data from the evaluation are made publically available by the Planning Department of the Colombian Government with no identifiable information on survey participants (https://www.dnp.gov.co/Paginas/inicio.aspx).
Statistical analysis
We started by comparing characteristics of the treatment and control municipalities using t (for continuous variables) or χ 2 tests (for categorical variables). Although the matched sample design tried to minimise differences between treatment and control municipalities, differences between the two groups may have persisted. These differences would bias the results if variation in post-programme outcomes was due to differences in unmeasured covariates between the treatment and control, rather than due to the programme. Therefore, we used a difference-in-differences (DID) approach to purge estimates of programme impact from pre-existing differences. The DID compares changes between baseline and follow-up between treatment and control, instead of comparing post-treatment outcomes only. The DID estimate is thus defined as the difference in outcome in the treatment group before and after treatment minus the difference in outcome in the control group over the same period. The rationale behind this approach is that the change observed in the control group represents the counterfactual change we would have observed in the treatment group had participants not been treated( Reference Card and Krueger 39 ). This approach has been commonly applied in the evaluation of CCT programmes( Reference Barham and Maluccio 40 , Reference Paes-Sousa, Santos and Miazaki 41 ).
A crucial assumption of the DID approach is that the outcome variable would have evolved in the same way between baseline and follow-up in both treatment and control municipalities had the FA programme not taken place. This is known as the common trend assumption. Although this assumption cannot be tested (we can only observe outcomes for each municipality in either treatment or control state), a common indirect test is to examine trends in the outcome before programme implementation. If trends in relevant outcomes were different before the programme, the common trend assumption would be unlikely to hold during programme implementation. We did not have data on height, weight and BMI across treatment and control municipalities before treatment. However, to assess the potential validity of the common trend assumption, we used data sources provided by the National Statistics Office (DANE: http://www.dane.gov.co/), which collects and harmonises data on all mortality information (under-5 deaths) and birth certificates from all regions at the individual level. We estimated trends in under-5 mortality rates and birth weight in control and treatment municipalities between 1997 and 2001, before the programme started. If trends in these indicators of health and living conditions were similar before the programme, this would provide an indication that the common trend assumption might hold.
We used linear regression (ordinary least squares) models to examine the impact of treatment with CCT on linear HAZ and BMI z-scores, and we implemented logistic regression models to examine the impact of the programme on stunting, thinness, overweight and obesity. The basic model was as follows:
where y is the outcome of interest for individual i in municipality j at time t; Time is a dummy variable with value 0 for baseline assessment and 1 for assessments after the programme started; Treatment is a dummy variable with value 0 for control assignment and 1 for FA treatment assignment; M is a vector of baseline municipality-level covariates; X is a vector of baseline individual-level covariates; and e ijt is the error term. The coefficient for Time represent the change in BMI between baseline and follow-up in the control group. The treatment coefficient reflects differences in BMI between treatment and control at baseline. Time t ×Treatment j , assesses the interaction between treatment assignment and time and corresponds to the DID estimate, as it estimates differences in height and weight trends between the treatment and control groups. In addition, we carried out all the analyses separately for child’s sex and age, maternal education and household income.
To provide a rough estimate of the clinical significance of the effect of the FA programme on BMI z-scores, we estimated a Cohen’s d effect and used common conventions to determine whether effects sizes were small (0·0–0·20), moderate (0·20–0·50) or large (>0·50)( Reference Sullivan and Feinn 42 ).
All the analyses were performed using SAS software 9.3. We incorporated appropriate sample weights and calculated robust standard errors to account for differential selection probabilities and a clustered design.
Results
Table 1 shows that there were no significant differences between treatment and control groups in key baseline characteristics including children’s age and sex, mother’s age and BMI, household size and income, and municipality population size and geographic location. However, children in treatment municipalities were more likely to live in rural areas, less likely to participate in Hogares Comunitarios, a home-based childcare programme, and have mothers with lower educational level. At baseline, the prevalence of stunting was 30·3 % for children in treatment municipalities and 27·9 % for children in control municipalities. At the same time, 17·4 % of children in control municipalities and 15·4 % of children in treatment municipalities were overweight. The prevalence of thinness was relatively low in both treatment (1·9 %) and control (0·9 %) groups. In addition, BMI z-scores were higher in the control group (0·25) than in the treatment group (0·20), and the same pattern was observed for HAZ but there were no significant differences between the two groups.
Table 1 Child, maternal, household and municipality characteristics in control and treatment municipalities in Familias en Acción, Colombia (Numbers and percentages; mean values and standard deviations)Footnote †

* Difference between treatment and control (P<0·05).
† P values for continuous variables are from a t test, whereas those for categorical variables are from a χ 2 test.
Fig. 2 summarises trends in HAZ, BMI z-scores and the prevalence of stunting, thinness, overweight and obesity for treatment and control municipalities among children aged 2–9 years. The mean HAZ increased and the prevalence of stunting decreased in both groups over time. BMI z-scores decreased in both treatment and control municipalities, but less among children from treatment municipalities. The prevalence of overweight and obesity declined in both groups, but the decline was smaller in the treatment group.
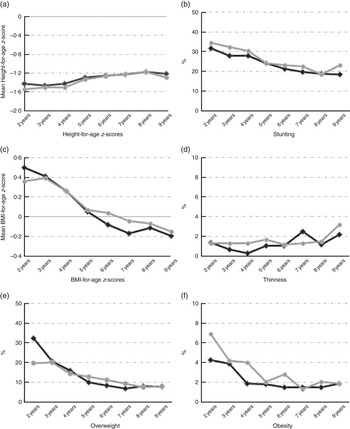
Fig. 2 Trends in (a) height-for-age z-scores, (b) stunting, (c) BMI z-scores, (d) thinness, (e) overweight and (f) obesity by treatment assignment, Familias en Acción, conditional cash transfer programme, Colombia. ![]() , Control;
, Control; ![]() , treatment.
, treatment.
Table 2 shows estimates of the main results examining differential trends in HAZ and BMI z-scores between treatment and control groups, before and after programme enrolment, controlling for all covariates. Columns 1–2 show estimates of the effect of the programme on linear growth (HAZ and stunting). The first row indicates that in control municipalities HAZ increased by 0·14 points (95 % CI 0·10, 0·18) between baseline and follow-up assessments. The last row presents the interaction between treatment and time, the DID estimate of interest, which suggests that assignment to treatment with FA was not associated with an increase in HAZ between baseline and follow-up relative to the control group. Moreover, there was no evidence that the FA programme influenced the odds of stunting (OR 0·92; 95 % CI 0·82, 1·05). Column 3 presents results for BMI z-scores. The FA programme was associated with a larger increase in BMI z-scores between baseline and follow-up relative to the control group (β 0·14; 95 % CI 0·00, 0·27; P<0·05). Columns 4–6 show OR from logistic regression models examining the impact of the FA programme on thinness, overweight and obesity. Although the odds of thinness doubled between baseline and follow-up in the control group (OR 2·27; 95 % CI 0·98, 5·28), children participating in the FA programme were significantly less likely to become thin after the programme (OR 0·25; 95 % CI 0·09, 0·74). In contrast, there was no evidence that the FA programme influenced the odds of overweight (OR 1·24; 95 % CI 0·80, 1·91) or obesity (OR 0·57; 95 % CI 0·21, 1·51). Supplementary analyses of the effects of the programme separately for each follow-up assessment yielded essentially the same results, although CI were somewhat wider (online Supplementary Table S2).
Table 2 Difference-in-differences (DID) estimate of the effect of Familias en Acción (FA) conditional cash-transfer programme on BMI z-scores, thinness, overweight and obesity, ColombiaFootnote * (β-Coefficients, odds ratios and 95 % confidence intervals)
* Variables included in the model are as follows: age, sex, participation in Hogares Comunitarios (home-based health care), mother’s marital status, mother’s age, mother’s education, mother’s BMI, household income, level of urbanisation, inhabitants and region.
Table 3 summarises the DID estimates from models stratified by sex, age, maternal education and household income. There appeared to be a significant effect of the programme on stunting for children from mothers with more than high-school education (OR 0·68; 95 % CI 0·52, 0·91). However, this was a very small group (6 % of all children), whereas there was no evidence of an effect for the majority of children in the sample, whose mothers had less than high-school education.
Table 3 Sub-group analysis: difference-in-differences estimates of the effect Familias en Acción conditional cash-transfer programme on BMI, thinness, overweight and obesity, ColombiaFootnote * (β-Coefficients, odds ratios and 95 % confidence intervals)

* Variables included in all the models are as follows: age, sex, participation in Hogares Comunitarios (home-based health care), mother’s marital status, mother’s age, mother’s education, mother’s BMI, household income, level of urbanisation, inhabitants and region. Coefficients, OR and P values are for a three-way interaction between treatment, time and the demographic variable of interest.
Common trend assumption
A crucial assumption of the DID approach is that trends in anthropometric outcomes would have been similar in both treatment and control municipalities had the FA programme not been implemented. Although this assumption cannot be tested because we cannot observe trends in the treatment group in the absence of treatment, a common approach is to assess pre-treatment trends. Data on BMI from children in our study were not available for the pre-treatment period, but we examined pre-treatment trends in two outcomes associated with childhood under-nutrition and overweight – namely, under-5 mortality rates and birth weight. The online Supplementary Fig. S1 shows trends in these outcomes in control and treatment municipalities between 1997 and 2001, before the programme started. Despite some fluctuations across years, there was no evidence for differential trends in infant mortality rate and birth weight between treatment and control municipalities. This was confirmed in models that suggested no interaction between municipality treatment status and time (P>0·05). Although not a definitive test, this provides some reassurance that trends did not differ systematically between treatment and control groups. Evidence from the original evaluation also suggests that there were no pre-treatment differences in income trends between treatment and control municipalities( Reference Attanasio, Benavides and Borda 31 ).
Discussion
Our results suggest that participation in FA reduced the odds of thinness, a relatively rare outcome among children in Colombia, but it had no impact on HAZ, stunting, overweight or obesity. FA programme participation was associated with significant BMI z-scores among children. In order to provide a sense of the magnitude of this effect, we estimated Cohen’s d effect sizes (online Supplementary Table S4) and found that the effects were small in magnitude for both. Overall, these results raise the possibility of an increase of small clinical significance on BMI among children of pre-school and school age.
To our knowledge, few studies have assessed the effect of CCT programmes on children’s BMI. Fernald et al.( Reference Fernald, Gertler and Neufeld 18 ) showed that children participating in the Mexican Oportunidades programme were less likely to be overweight after the treatment (β −0·08; 95 % CI −0·13, −0·03; P 0·001). However, this study only evaluated changes among children enrolled in the programme early in life and it did not include a comparison with children in control areas( Reference Fernald, Gertler and Neufeld 18 ). Likewise, in the Peruvian Juntos programme, BMI z-scores and the prevalence of overweight declined only among girls( Reference Andersen, Reynolds and Behrman 43 ). This may be misleading as changes most likely reflect the natural progression of BMI among children. In particular, a decline in BMI is often linked to the ‘adiposity rebound’ in pre-school age children, whereby BMI declines to a nadir and then begins to increase( Reference Lumeng, Kaciroti and Frisvold 44 ). Some studies suggest that BMI should decline up to age 4 years, after which it starts to increase gradually( Reference Hughes, Sherriff and Ness 4 , Reference Lumeng, Kaciroti and Frisvold 44 ). We also observed a decline in BMI z-scores, overweight and obesity over time, but by using a control group we were able to show that this decline was not due to the CCT programme, as children in treatment municipalities experienced a weaker decline in BMI than children in control municipalities.
Our results show that participation in the FA programme was associated with a reduction in the odds of thinness. Several potential explanations could account for this effect of the FA programme on thinness. First, conditional transfers may have improved the quality of home diet, thus reducing the risk of under-nutrition. Early reports of FA impact suggested that families participating in the programme spent on average 15 % more of their household income on food than families in the control group. Most children participating in the FA programme increased the intakes of vegetables, milk and protein sources of high biological value( Reference Forde, Chandola and Garcia 27 ). Our findings may also be linked to better access and use of healthcare services, which might have reduced the frequency and severity of infectious diseases. This hypothesis is substantiated by early reports of the programme, suggesting that children in the treatment group reported less symptoms of diarrhoea than those in the control group( Reference Attanasio, Gómez and Heredia 32 ). Project reports have also shown that families participating in the FA programme use healthcare services more often than families in the control group and in the general Colombian population( Reference Attanasio and Mesnard 11 , Reference Attanasio, Benavides and Borda 31 , Reference Attanasio, Gómez and Heredia 32 ). The FA programme has been shown to increase compliance with the growth and development check-ups among children under 48 months, and it has increased the rates of DPT vaccination among children under 24 months( Reference Attanasio and Mesnard 11 , Reference Attanasio, Benavides and Borda 31 , Reference Attanasio, Gómez and Heredia 32 ).
Yet, an important consideration in interpreting these findings is the fact that the prevalence of thinness at baseline was very low in our sample (1·6 %), and also the effect size estimates at group level were small (Cohen’s d effect between 0·0 and 0·20), and thus the large relative effect we observed was very small in absolute terms. In contrast, the prevalence of stunting (30·3 %) was very high in our sample. Previous studies across different countries have reported positive effects of CCT programmes on height in the youngest and poorest children( Reference Morris, Olinto and Flores 29 , Reference Leroy, Gadsden and Gutierrez 45 – Reference Thomas 47 ). In our study, the FA programme had no effect on HAZ and stunting among pre-school and school-aged children. This finding suggests that other factors that are not amenable to intervention through cash transfers may be more important determinants of linear growth. Stunting is often believed to be determined in the first 1000 d of life, because it is the result of multiple contributing factors early in life, including intra-uterine and antenatal influences, suboptimal breast-feeding and frequent infectious diseases in the first 24 months of life, which can slow down growth, with little apparent catch-up growth before puberty( Reference Prendergast and Humphrey 48 ).
Limitations
Our study has several strengths including a longitudinal design with a 4-year follow-up, a robust DID approach and the use of both direct and standardised weight and height measurements for children. However, some limitations should be considered. First, the baseline response was about 80 % and there was a 30 % loss-to-follow-up due to the high mobility of participants. The impossibility to contact some participants partly reflects the unstable living conditions of a migrating workforce. Nevertheless, children contacted at follow-up did not differ from those who were not contacted at follow-up with respect to several key baseline individual, household and municipality characteristics, and we did not find a differential loss to follow-up between the treatment and control groups.
A second limitation refers to the fact that because of political reasons some treatment municipalities started receiving the cash transfers from the FA programme before the baseline assessment. For these municipalities, therefore, we did not have pre-treatment assessments, and we therefore excluded them from the main analysis. In sensitivity analyses, we examined the impact of the programme incorporating these municipalities as part of the treatment group (online Supplementary Table S3). Although CI were wide, we found similar effects on BMI and stunting outcomes as for our original analysis. Our estimates, therefore, are unlikely to be driven by the exclusion of these municipalities from the treatment group.
Conclusion
Our results suggest that FA, a CCT programme in Colombia, was associated with decreased odds of thinness, whereas there was no evidence of programme effects on stunting, overweight or obesity; the FA programme was associated with a clinically small but statistically significant increase in BMI z-scores. This raises concerns about early small negative effects on BMI among children of pre-school and school age. Although these effects were small, this requires further monitoring to ensure that CCT programmes adequately address the double burden of malnutrition experienced by many low- and middle-income countries around the world.
Acknowledgements
S. L.-A. was supported by the European Union Erasmus Mundus Partnerships programme Erasmus-Columbus (ERACOL) and Fundación para el Futuro de Colombia (COLFUTURO) at Erasmus MC in the Netherlands. M. A. was supported by the European Research Council (ERC) (grant no. 263684), the National Institute on Ageing (award numbers R01AG040248 and R01AG037398), and the LIFEPATH project funded by the European Union’s Horizon2020 research and innovation programme under grant agreement 633666. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Design (S. L.-A., M. A.), data analysis (S. L.-A., M. A.), interpretation of the results (S. L.-A., M. A., A. B., F. J. v. L., I. F.), manuscript preparation (S. L.-A., M. A.), manuscript review (S. L.-A., M. A., A. B., F. J. v. L., I. F.).
The authors declare that no conflicts of interest exist.
Supplementary Material
For supplementary material/s referred to in this article, please visit http://dx.doi.org/doi:10.1017/S0007114516000714








