Women of reproductive age in Lebanon and the Middle East region have biological and social risk factors compromising their dietary intake and physical activity level and enhancing their risk of developing obesity(Reference Jabbour, Khalil and Ronzoni1–Reference Okati-Aliabad, Ansari-Moghaddam and Kargar3). Studying dietary intake in this age group is a public health priority given the impact of obesity on women’s health, productivity and quality of life(Reference Pullar, Wickramasinghe and Demaio4–Reference Chowdhury and Siddik6). Children are also affected by maternal obesity(Reference Shrestha, Prowak and Berlandi-Short7). Offspring of women with excess weight have an increased risk of developing neural tube defects, diabetes as well as cardiovascular and renal diseases among other non-communicable diseases (NCD)(Reference Chowdhury and Siddik6,Reference Elshenawy and Simmons8,Reference Vena, D’Ambrosio and Paladini9) .
Given the modulatory effects of nutrition on disease risk, the association between dietary exposures and NCD remains an important research area(Reference Marmot and Bell10,Reference Iriti, Varoni and Vitalini11) . However, the ability to accurately evaluate dietary exposures through self-reports has been challenging in epidemiological studies. Weighed diet records are relatively reliable and valid in assessing nutrient intake given their precision and the absence of memory and reporting bias(Reference Freedman, Commins and Moler12,Reference Al-Shaar, Yuan and Rosner13) . Yet, the latter method is resource intensive, imposes a heavy burden on research subjects and can be associated with social desirability bias(Reference Bailey14,Reference Thompson and Subar15) . Self-reported methods such as Food Frequency Questionnaire (FFQ) have been more extensively used as they are less invasive, cost efficient and estimate longer-term dietary intake(Reference Willett and Lenart16,Reference Athanasiadou, Kyrkou and Fotiou17) . Yet, despite their widespread utilisation, FFQ may not be practical for routine clinical and research use among participants with limited time given their long administration duration(Reference Bailey14,Reference Thompson and Subar15) . Diet screeners have been proposed as time- and resource-efficient alternatives to FFQ(Reference Thompson, Midthune and Kahle18). Even though diet screeners cannot characterise overall diet like FFQ, they can provide reliable and practical information on dietary patterns, especially when they inquire about portion sizes(Reference Thompson, Midthune and Kahle18). Several FFQs have been culturally validated to assess the Lebanese and Mediterranean diet among adults and women of reproductive age(Reference Papazian, Hout and Sibai19–Reference Harmouche-Karaki, Mahfouz and Obeyd23) . Yet, to our knowledge, no diet screener incorporating portion sizes has been developed and validated in Lebanon and the Mediterranean Region in adults. The purpose of this study was to assess the reproducibility and agreement of the Modified Mediterranean Prime Screen (MMPS) in estimating obesogenic nutrient intake among women of reproductive age compared with a reference FFQ.
Methodology
Study design
This validation study was conducted as part of a larger longitudinal birth cohort at the American University of Beirut Medical Center (AUBMC), Beirut-Lebanon. This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the Institutional Review Board (IRB) of the American University at Beirut (AUB) under study number IMGEHF22, and subjects gave their written consent after being informed of the benefits and risks of joining the study. Data were collected between December 2019 and September 2021 through face-to-face (F2F) and telephone interviews. Originally, questionnaires were administered F2F but shifted to telephone administration in April 2020 during the coronavirus disease 2019 pandemic and lockdowns, as required by the IRB. As per IRB guidance, F2F assessments were resumed in December 2020, and data collection was completed in September 2021.
Participants
Eligible participants were women aged > 18 years, attending routine visits for their infants and toddlers at the private and public paediatric clinics at AUBMC. Participants were excluded if they had diabetes mellitus (type 1 or type 2), history of gestational diabetes, twins/triplets, neonatal physical anomalies, renal stones, diagnosis of cancer in the last 10 years (other than basal cell carcinoma), uncontrolled thyroid dysfunction or were pregnant. These exclusion criteria were set to be in conformity with the exclusion criteria of the parent cohort from which this ancillary study originated(Reference Chakhtoura, Nassar and Arabi24) . The minimum sample size acceptable for calibration of dietary tools has been suggested to be 100–110(Reference Willett and Lenart16,Reference Cade, Thompson and Burley25) . Based on a minimal sample of 110 and accounting for an anticipated dropout rate of 30 %, data were collected on 143 participants.
Data collection
Assessments were conducted in two visits that were 2 weeks–6 months apart. In the first visit (Visit 1), we assessed demographic characteristics, parity, gravida, number of children, marital status, working status, education, current and family medical history, physical activity level (using the Arabic version of the International Physical Activity Questionnaire-Short Form) as well as food security (using the Arab Family Food Security Scale)(Reference Craig, Marshall and Sjöström26–Reference Sahyoun, Nord and Sassine29). In addition, anthropometric measurements of weight, height and BMI were collected. BMI was categorised using the WHO recommendations(30). In the second visit (Visit 2), in addition to performing the dietary assessment, participants were asked to report their physical activity level and food security to evaluate relevant changes.
As for dietary intake, we asked participants to recall their intake of each food item (for the FFQ) or category (for the MMPS) in the preceding 3 months. With regard to the order of administration of the tools, MMPS was administered first since it is shorter and contains a smaller number of food items. The research team did not want to administer the FFQ first as it could artificially improve the agreement validity of the MMPS with the FFQ since participants would be more likely to remember the food items from a detailed FFQ.
Diet screener development
We adapted the MMPS from the Prime Screen (PS), a validated diet screener designed to assess diet quality in relation to NCD, mainly cardiovascular diseases, cancer and osteoporosis(Reference Rifas-Shiman, Willett and Lobb31). The PS, used in the VIVA cohort as a time-efficient tool to evaluate the diet quality of mothers, assesses the frequency of intake of eighteen food categories including fruits, vegetables, dairy products, whole grains, fish, red and processed meats and deep-fried food(Reference Rifas-Shiman, Willett and Lobb31,Reference Oken, Baccarelli and Gold32) . Our expert committee, composed of three experienced dietitians, adapted the PS to include food items that are commonly consumed in the local Mediterranean Lebanese culture and identified local foods associated with chronic diseases, metabolic syndrome and cancer. To ensure that the tool was brief, food items were grouped into categories that were closest in caloric and macronutrient content. We grouped the following nutrients due to their association with obesity when consumed in inadequate amounts: energy, carbohydrates, added sugars, trans-fatty acid (TFA) and unsaturated fatty acids. The final tool was composed of thirty-two food and beverage items (vegetables (raw, cooked and stuffed), fruits, juices, milk products, cheeses, eggs, oils and seeds, butters and creams, grains, pastries, sweets, fish, meats, chicken and processed meat, sugars and jams, diet drinks, sweeteners and alcoholic beverages) with four possible frequency choices (rarely/never, monthly, weekly or daily) (online Supplementary Table 1). The committee members assigned food groups in the MMPS to allow for the calculation of diet quality scores and included portion sizes to improve quantity estimates. We expressed portion sizes in lay terms such as thumbs, cups, spoons and palm sizes instead of weights and volumes.
We compared the MMPS with a validated culturally specific semi-quantitative FFQ that assesses the intake of 157 Mediterranean and Western food items commonly consumed by the Lebanese population(Reference Papazian, Hout and Sibai19). The reference FFQ had been validated among adults and pregnant subjects living in Lebanon and was shown to have good reproducibility and agreement with 24h recalls(Reference Papazian, Hout and Sibai19,Reference Aoun, Bou Daher and El Osta20) . This tool is designed to assess and evaluate the nutritional intake among different age groups, pregnant women, healthy or suffering from any disease. It is conducted by asking respondents to report their usual consumption frequency of the different food group items over a specific period of time (daily, weekly or monthly). In addition, portion sizes of the common food item components are used in the questionnaire(Reference Papazian, Hout and Sibai19). We referred to nutrients relevant to obesity as obesogenic nutrients in the MMPS and FFQ; these included energy, proteins, carbohydrates, fibre, total sugar, fats (MUFA, PUFA, TFA and SFA) and cholesterol. These nutrients may have a positive or negative association with obesity. Yet, they are worth studying for clinical and research purposes. In order to assess the nutrient composition of each food item and category, we used the food composition databases of the US Department of Agriculture (USDA), the tables of Middle Eastern cuisine as well as other locally relevant food composition tables(Reference Pellet and Shadarevian33–Reference Hoteit, Zoghbi and Rady36). As data in the food composition tables were available in grams rather than in commonly utilised portion sizes (cups, spoons, etc.), items available in the FFQ and MMPS were weighed in the main kitchen of the AUBMC to accurately reflect the composition of the portion sizes specified in the screener. Two experienced research assistants were trained and mentored by licensed dietitians to administer the FFQ and MMPS using relevant food models of Lebanese dishes. To minimise variation in data collection, research assistants were trained on how to estimate food portions in a similar way and followed written guides for portion sizes of local food dishes.
Statistical analysis
Baseline characteristics were described using mean and standard deviation (s d) for continuous variables and counts with percentages for categorical variables. Differences between interview settings were tested using independent samples t test for continuous variables and χ2 test for categorical variables. Total daily intakes of all nutrients were averaged between the two visits for FFQ and MMPS. These values were log transformed and then energy adjusted, using the residual method (regressing nutrient intake on total energy intake) to minimise the influence of extreme nutrient values(Reference Willett and Stampfer37). Normality of these variables was assessed by performing the Shapiro–Wilk test and kurtosis/skewness visual interpretation.
Reproducibility of the questionnaires was assessed using the average measures of the intraclass correlation coefficients (ICC), calculated using random-effect analysis of variance between Visits 1 and 2. To assess the agreement between PS and FFQ mean values, we calculated Pearson correlation coefficients and their 95 % CI. To interpret ICC, values < 0·5, 0·5–0·75, 0·76–0·9 and above 0·9 reflected poor, moderate, good and excellent reliability, respectively(Reference Koo and Li38). Pearson correlation above 0·4 was considered to represent adequate validity(Reference Akoglu39). Subgroup analyses were implemented to evaluate the reproducibility and validity of PS by mode of administration: F2F or telephone administered through assessing the overlap in the ICC and Pearson correlations’ 95 % CI.
Bland–Altman plots were generated to assess the extent of agreement across the range of nutrient intakes between MMPS and FFQ. Differences between the two methods were plotted against the average of the two measures, and the limits of agreements (mean difference (sd 2) were used to reflect the extent of disagreements between the two methods. To generate correction factors to be used for the calculation of corrected intakes in future studies when utilising MMPS, a linear regression model was run where energy-adjusted FFQ measurement was considered a reference against the corresponding MMPS energy-adjusted values, and relevant slopes and intercepts were generated. The significance level was set at 0·05, and all statistical analyses were performed using IBM SPSS Statistics 27.0 (IBM). In addition, the agreement of food security levels between Visit 1 and Visit 2 was assessed by Cohen’s weighted kappa. The values of weighted kappa were interpreted as follows: ≤ 0 no agreement, 0·01–0·20 none to slight, 0·21–0·40 fair, 0·41–0·60 moderate, 0·61–0·80 substantial and 0·81–1·00 as almost perfect agreement(Reference McHugh40).
Results
Characteristics of study subjects
In total, 483 women were approached to participate in this study, 200 provided consent and were enrolled, fifty-seven subjects (29 %) did not continue the study after Visit 1 and 143 completed both questionnaires at two time points. The main reason behind non-participation and withdrawal from the study was limited time/interest in the study. Baseline characteristics did not differ significantly between participants who continued and those who dropped out except for BMI (online Supplementary Table S2). Participants who dropped out after Visit 1 had a higher BMI compared with those who continued the study [BMI of 24·2 (sd 4·0) kg/m2 v. 25·9 (sd 5·5) kg/m2, P value = 0·044). Table 1 shows the baseline characteristics of the 143 study participants who completed the validation study. The questionnaires were administered F2F and over the phone for ninety-five and forty-eight participants, respectively, in Visit 1 and fifty and ninety-three participants, respectively, in Visit 2. The median time between Visit 1 and Visit 2 was 3·2 months, and the range (minimum–maximum) was 5·4 months (0·7–6 months). The baseline characteristics of participants were similar when stratifying by the mode of data collection (F2F v. phone interview), except for the age at enrollment where participants interviewed over the phone were slightly older compared with those interviewed F2F (Table 1). Participants had a mean age of 31·5 (sd 5) years at enrollment, of whom 58 % had a normal BMI (mean 24·2 (sd 4·0) kg/m2). The majority of participants had received higher education, and around half of them were employed on a full-time or part-time basis. Only 22 % reported having ongoing medical problems (Table 1), while a family history of diabetes, hypertension or cancer was prevalent in around 50 % of respondents (data not shown). At Visit 1, 91 % of the sample was food secure, and 38 % did not perform any type of physical activity. The overall weighted kappa for food security levels between the two visits was moderate (kappa = 0·463, P value < 0·01), reflecting no difference between the two assessment points.
Table 1. Baseline characteristics of subjects by interview setting
(Numbers and percentages; mean values and standard deviations)

Reproducibility of FFQ and Prime Screen
The mean ICC for the FFQ was 0·651, ranging from 0·590 for SFA to 0·725 for PUFA, indicating moderate reproducibility. With energy adjustment, the ICC were slightly lower, with a mean of 0·529 and correlations ranging from 0·370 for total fat to 0·648 for cholesterol (Table 2). Subgroup analysis by mode of administration showed comparable correlations for total energy, protein, fibre, MUFA, PUFA, TFA and cholesterol (online Supplementary Tables S3 and S4). Yet, nutrients like carbohydrates, sugar, fat and SFA had non-significant correlations when assessed by different modes of administration (online Supplementary Tables S3 and S4).
Table 2. Intraclass correlation of daily nutrient intake assessed using the Food Frequency Questionnaire (FFQ) and the Modified Mediterranean Prime Screen (MMPS)
(Mean values and standard deviations; 95 % CI)

ICC, intraclass correlation coefficient; PUFA, poly unsaturated fatty acids; SFA, saturated fatty acids; TFA, trans-fatty acids. Average ICC measures are presented.
As for the MMPS’ reproducibility, a moderate ICC of 0·67 was recorded for macronutrients, ranging from 0·622 for MUFA to 0·710 for cholesterol (Table 2). With energy adjustment, the mean ICC was 0·595 (sd 0·08), ranging from 0·428 for SFA to 0·694 for cholesterol. All macronutrients, except for SFA, had moderate reliability (Table 2). Subgroup analysis by administration mode revealed that the MMPS reproducibility was comparable for total energy, protein, carbohydrates, fibre, MUFA, PUFA, TFA and cholesterol (online Supplementary Tables S5 and S6). Fibre, total fat and SFA had non-significant correlations in subgroup analysis (online Supplementary Tables S5 and S6).
Agreements between the Modified Mediterranean Prime Screen and the FFQ
Table 3 presents the Pearson correlations of the nutrient intakes assessed by FFQ and MMPS using the average of the two visits. Total energy intake was highly correlated (0·862 (95 % CI 0·81, 0·91)). The mean energy-adjusted correlation coefficient of macronutrients was 0·645 (sd 0·19), ranging between 0·294 for TFA and 0·831 for cholesterol (Table 3). Correlations were comparable when assessed by mode of administration (online Supplementary Tables S7 and S8). The Bland–Altman plots are presented in Fig. 1 for macronutrients and online Supplementary Fig. S1 for the rest of the nutrients. Visual inspection of the plots revealed an acceptable agreement for the macronutrients where the majority of the data points laid within the limits of agreements (Fig. 1 and online Supplementary Fig. S1). Finally, online Supplementary Table S9 shows the correction factors of the energy-adjusted nutrient intake that can be used to correct for measurement errors when estimating the true intake.
Table 3. Energy-adjusted and unadjusted Pearson correlation coefficients of the mean intake of macronutrients assessed using the Food Frequency Questionnaire and the Modified Mediterranean Prime Screen
(Mean values and standard deviations; 95 % CI)
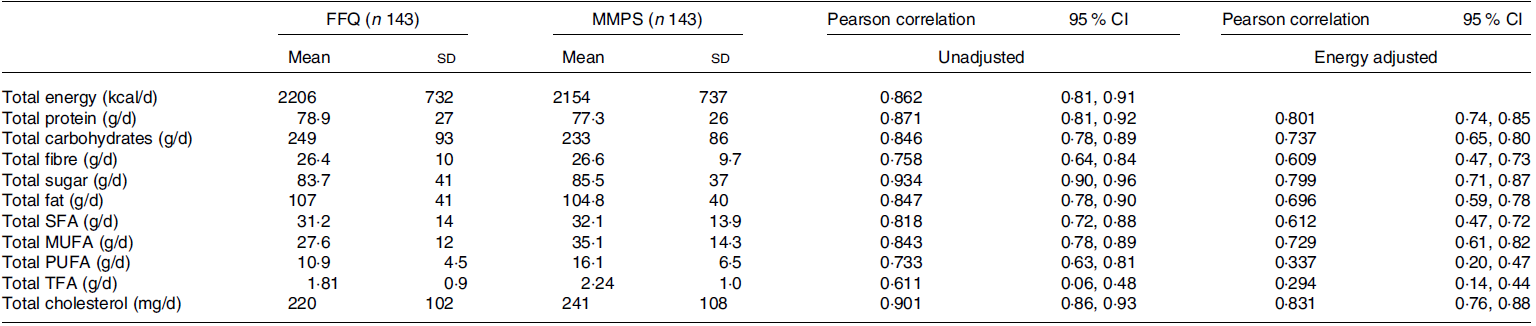
PUFA, poly unsaturated fatty acids; SFA, saturated fatty acids; TFA, trans-fatty acids.
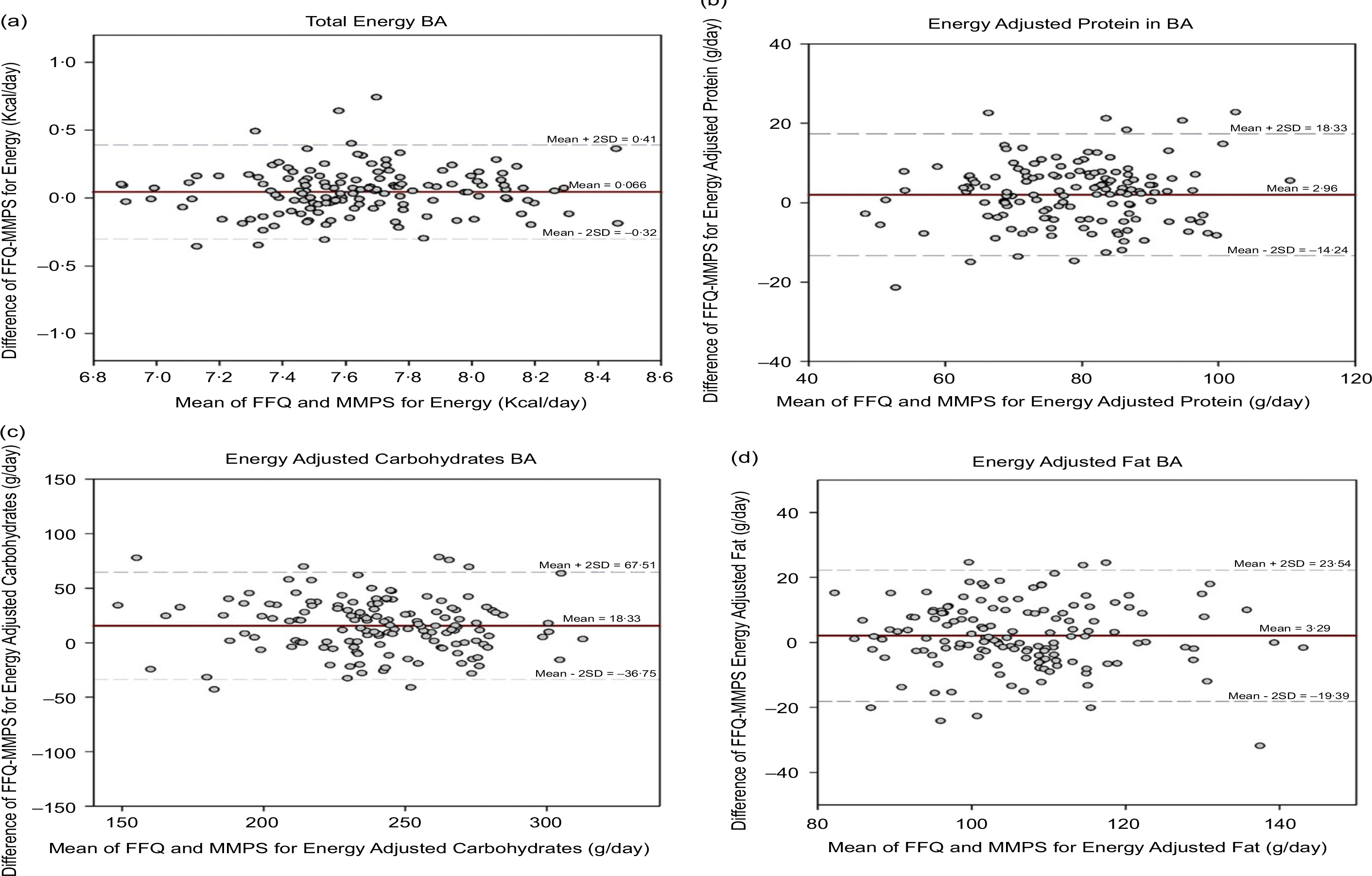
Fig. 1. Bland–Altman plots of energy and energy-adjusted protein, carbohydrates and fat intake. (a) Bland–Altman plots showing the difference between FFQ and MMPS v. the mean of FFQ and MMPS for total energy. (b) Bland–Altman plots showing the difference between FFQ and MMPS v. the mean of FFQ and MMPS for energy-adjusted protein. (c) Bland–Altman plots showing the difference between FFQ and MMPS v. the mean of FFQ and MMPS for energy-adjusted carbohydrates. (d) Bland–Altman plots showing the difference between FFQ and MMPS v. the mean of FFQ and MMPS for energy-adjusted fat. The dashed lines show the limits of agreements (sd 2); solid line shows the mean difference in intake between FFQ and MMPS. FFQ, Food Frequency Questionnaire; MMPS, Modified Mediterranean Prime Screen.
Discussion
This study presents the validation of the MMPS against a reference FFQ on a sample of women of reproductive age residing in Lebanon, a Middle Eastern country. Although the age of our study sample is slightly high, it is consistent with studies assessing women of reproductive age in Lebanon(Reference Nabulsi, Smaili and Abou Khalil41,Reference Hammoud, Saleh and Halawani42) . The reliability of the MMPS was moderate for energy and all obesogenic nutrients except for SFA. The agreement of the MMPS with the reference FFQ was adequate for energy and obesogenic nutrients, with the exception of TFA and PUFA.
Our preliminary assessment of the agreement of the MMPS with the reference FFQ in estimating obesogenic nutrient intake revealed promising results. Correlations between the MMPS and FFQ were moderate for all obesogenic nutrients except TFA and PUFA. MMPS tended to overestimate the intake of TFA and PUFA compared with FFQ, possibly due to the categorisation of the MMPS that required many food items to be combined under one category (thirty-two food groups in the MMPS v. 157 food items in the FFQ). A reduction in information is one of the anticipated drawbacks of the screeners compared with longer methods such as FFQ and 24 h recall, with the benefit of reducing administration time(Reference Thompson, Kirkpatrick and Subar43). Moreover, the estimation of TFA and PUFA could have been compromised by the incomplete data on TFA and PUFA in the culturally specific food composition tables(Reference Pellet and Shadarevian33,Reference Batal, Ghattas and El-Aily34) . When comparing and contrasting the MMPS validation with other local FFQ, one notices that the ICC were higher than those of several culturally specific FFQ(Reference El Sayed Ahmad, Baroudi and Shatila21) and comparable or slightly inferior to two other local FFQ(Reference Aoun, Bou Daher and El Osta20,Reference Zalaket, Matta and Hanna-Wakim22) , all administered to Lebanese adults.
With regard to reproducibility, the MMPS had ICC that were moderate for all obesogenic nutrients except SFA. FFQ had an acceptable reproducibility, yet the ICC were lower than those observed in the original validation studies of the reference FFQ (ICC were above 0·9 among adults and pregnant women)(Reference Papazian, Hout and Sibai19,Reference Aoun, Bou Daher and El Osta20) . These latter differences can be partially explained by the shorter time frame between the assessments reported by Aoun et al. and Papazian et al. whereby they had a maximum time frame of 3 weeks and the minimum time between assessments was not specified(Reference Papazian, Hout and Sibai19,Reference Aoun, Bou Daher and El Osta20) . To assess the reproducibility of dietary questionnaires, it is usually best to repeat the administration in an interval that is not very close to the initial administration as this might introduce bias where participants might recall their dietary intake in the second visit based on what they have initially reported and not too far as changes in the habitual diet could occur over time. However, for many subjects, we were challenged by the coronavirus disease 2019 pandemic and the repeated incurred total and partial lockdowns that ensured throughout the study duration. A recent meta-analysis evaluating the reproducibility of FFQ around the world revealed that the time between the administration of FFQ spanned between 1 week and 2·7 years and FFQ administered within 6 months had enhanced reliability compared with those that were performed more than 6 months apart(Reference Cui, Xia and Wu44). The median time interval between the administrations of the questionnaires was 5·2 months in our study, within the recommended time frame. Yet, changes in administration mode (F2F and phone) and in dietary intake that may occur postpartum may have influenced the assessment and underestimated its reproducibility.
Several diet screeners have been validated in different populations and focused on selected dietary components, the majority of which do not incorporate portion sizes. The Mediterranean Diet Adherence Screener (MEDAS) is a fourteen-item screener, derived from the PREvención con DIeta MEDiterránea (PREDIMED) trial, which assesses the adherence to the Mediterranean diet without inquiring about portion sizes(Reference Schröder, Fitó and Estruch45). Given the practicality of administering dietary screeners over the phone, a telephone-based version of MEDAS was also validated(Reference Gregório, Rodrigues and Salvador46). Compared with the MMPS, the MEDAS can be more easily incorporated into research designs as it does not require individuals to recall portion sizes in all of the questions; it contains fewer food groups and can be self-administered. Yet, MEDAS does not provide data on energy and macronutrient intake, consumption of alternative sweeteners and sugar-sweetened beverages as the MMPS does and is therefore less useful in clinical and research applications related to obesity and NCD(Reference Schröder, Fitó and Estruch45). The Dietary Screener Questionnaire (DSQ) is a nineteen-item screener employed by the National Health and Nutrition Examination Survey (NHANES) to estimate intake of selected food groups such as fruits, vegetables, dairy, whole grains and sugar-sweetened beverages. The DSQ is useful in identifying dietary patterns and studying their changes over time(Reference Thompson, Midthune and Kahle18). Compared with the MMPS, DSQ can be self-administered in less time but neither analyses the participants’ nutrient intake (as it does not include questions on portion sizes) nor provides a quantitative assessment of alcohol, alternative sweeteners and olive oil intake, which are important for the evaluation of several dietary indices. Fruit and vegetable screeners in the Eating at America’s Table Study (EATS) do take into consideration portion sizes and allow for evaluation over a meal or over a whole day. These screeners are focused on fruits and vegetables and do not provide an estimation of the rest of the dietary variables. They are useful when the research question is centred around fruits and vegetables only as they provide a thorough and time-efficient assessment of these groups(Reference Thompson, Subar and Smith47).
This study has several limitations and strengths. One of the main limitations of this validation project is related to the variability in the administration mode of the questionnaires. Switching between F2F and phone was imposed on the researchers during the coronavirus disease 2019 pandemic. This fact may have limited the ability to adequately assess the performance of the screener and reduced the sample size in each subgroup to below 100 participants. The fact that similar trends were observed in the F2F and phone assessments reassured us that the data could be combined and the results remained meaningful. The use of two administration modes can be also considered a strength since the MMPS was tested and deemed feasible in both F2F and telephone settings. Another limitation of this study is related to the reference method employed. Choosing an FFQ as a reference method is involved with inherent biases such as the recall, interviewer and social desirability bias since it relies on self-reporting to a researcher. Complementing the results with recovery biomarkers and using weighed diet records would have enhanced the validity of the findings. Yet, this was not deemed feasible given the limited resources and logistic constraints. A final limitation relates to the lower rate of obesity in the study sample compared with the one documented among adult women in Lebanon (11 % v 31 %)(48). Given that the aim of the study was to assess the reproducibility and agreement in a diverse sample and 35 % of the sample had a BMI of 25 kg/m2 or above, we do not anticipate that this difference has affected the results observed. Strengths of this study included the robust methodology employed to develop the MMPS interface and backend by an experienced multidisciplinary team of researchers, dietitians and public health practitioners. In addition, we have targeted populations from both public and outpatient clinics to have a diverse profile of patients.
Conclusion
The time the FFQ takes to be administered may pose a heavy burden on researchers and hinder participants’ enrollment in research studies. The development of diet screeners is vital to allow for the analysis of associations between dietary intake and health outcomes in a region battling with NCD across the lifespan and struggling with resources to perform health research. This manuscript presented the validation of the MMPS, a diet screener administered in half the time of a full-length FFQ while providing a reliable assessment of many obesogenic nutrients such as energy, proteins, carbohydrates, fibres, sodium and sugar but a poor estimation of TFA and SFA intake. The MMPS has the potential to predict dietary indices, and future studies should assess the ability of the MMPS to evaluate diet quality indices in comparison with the FFQ. Further research should also confirm the findings of this study in different sociodemographic subgroups of the population, which will allow for a wider utilisation of the MMPS in research and clinical applications.
Acknowledgements
The research team would like to acknowledge:
-The participants for the time and efforts dedicated to this study.
-The Clinical Nutrition Department at AUBMC for allowing the research team to use the food services facility for the weighing of local dishes during the development of the MMPS.
This trial was supported by grants from the AUB and by Bernard Lown Scholars in Cardiovascular Health Award, Harvard School of Public Health.
S. A., L. A., M. A., G. E. H. F., H. G., J. J., M. R. and M. S. contributed to the manuscript conception and design of the work; S. A., M. A. and M. R. contributed to the data acquisition; S. A., L. A., M.A., and M. R. performed the data analysis; and S. A., L. A., M. A., G. E. H. F, H. G., J. J. and M. R. contributed to the data interpretation; S. A., M. A. and J. J. had drafted the work; and all of the authors have substantively revised the manuscript and have agreed to the submitted manuscript.
The authors declare they have no relevant conflicts of interest.
The study protocol was approved by the Institutional Review Board of the American University at Beirut.
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524000977







