Pregnant women must consume enough calories and nutrients to provide sustenance for both themselves and the developing fetus(Reference Watts, Rockett and Baer1). Moreover, adequate nutrition during pregnancy is important for the development of the placenta, for a healthy delivery and for future lactation. A key focus of attention in public health has been micronutrient deficiencies in pregnancy, because of the increased needs and greater vulnerability of pregnant women to the effects of micronutrient deficiency or imbalance(Reference Rondó, Villar and Tomkins2). Deficiency of certain nutrients can lead to anaemia and neural tube defects(Reference Watts, Rockett and Baer1). Dietary surveys of pregnant women in industrialised countries consistently demonstrate Fe intake well below current recommendations(Reference Schofield, Stewart and Wheeler3). As a consequence, Fe deficiency anaemia is common in pregnancy. Beneficial health effects of nutrient supplementation in a well-nourished pregnant population have only been documented for folate in the prevention of neural tube defects(Reference Wilson, Davies and Désilets4), and for Fe in the prevention of anaemia(Reference Melamed, Ben-Haroush and Kaplan5).
Epidemiological studies indicate that fetal nutrition may influence fetal growth, development and the risk of developing various diseases later in life(Reference Harding6). As such, it would also be necessary to monitor the diets of pregnant and lactating women to verify whether they are adequate in long-chain n-3 fatty acids, given the structural role played by DHA in the brain and retina, and the rapid brain development that takes place during the last trimester of pregnancy and infancy(Reference Cetin and Koletzko7, Reference Gibson and Makrides8). There is a growing interest in the mother's diet during pregnancy, and it is becoming increasingly important to develop reliable methods for monitoring maternal consumption of foods and nutrients, including dietary supplements. The FFQ is a tool commonly used in large epidemiological studies in different contexts, groups and populations, owing to their low cost and ease of administration(Reference Katsouyanni, Rimm and Gnardellis9, Reference Shu, Yang and Jin10). In general, the studies have been conducted to evaluate intake of nutrients and foods from the diet, leaving out information on the use of dietary supplements. Assessment of dietary supplement use in pregnant women is necessary, owing to the fact that both the use of dietary supplements and the consumption of fortified foods are on the rise.
Research conducted as part of the European Commission's EURopean micronutrient RECommendations Aligned (EURRECA) Network of Excellence has focused on extensive literature reviews addressing the validation of methods used to assess intake of micronutrients, n-3 fatty acids and of special population groups: pregnant women, infant, children, adolescents and elderly people(Reference Ashwell, Lambert and Alles11). In the present review, the studies on dietary methods used to assess micronutrient intake during pregnancy are presented.
Material and methods
The research question applied to the systematic review was ‘which dietary methods are reliable for the assessment of micronutrient intake during pregnancy?’. The main stages of the review are illustrated in Fig. 1. The review included English, Spanish, French, Italian, Portuguese and German articles, without limits on time frame or country. Stage 1 of the review involved searching for publications using electronic databases (MEDLINE and EMBASE). The MeSH terms used in the general search were: nutritional assessment, diet, nutritional status, dietary intake, food intake, validity, validation study, reproducibility, replication study, correlation coefficient and correlational study in the title and abstract. As a second specific search, the following words were included: pregnancy, pregnant women, ‘dietary assessment’, ‘dietary intake’, ‘nutrition assessment’, ‘diet quality’, reliability, reproducibility, validit* and correlate* as free text in the title and abstract. Additional publications were identified from references published in the original papers. At stage 2 of the review, the title and abstract were analysed by two independent reviewers and the exclusion criteria were applied (Table 1). At stage 3, studies that fulfilled the inclusion criteria were analysed for relevance to the research question.

Fig. 1 Main stages of the systematic review process.
Table 1 Inclusion and exclusion criteria

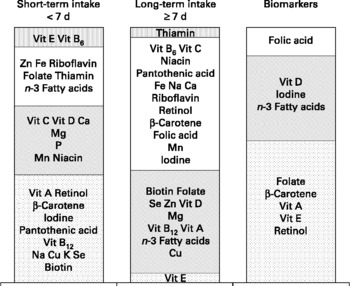
The selected studies were then classified into three different types according to the reference method applied in the validation studies: (1) reference method assessing intake of < 7 d (including 24-h dietary recall, estimated dietary records (EDR) and weighed dietary records (WDR)), classified as reflecting short-term intake; (2) reference method assessing intake of ≥ 7 d, reflecting more long-term intake; (3) reference method that employed the use of a biomarker (BM).
Furthermore, the different studies included in the present review were scored according to a quality score system developed by EURRECA, which has been described in another article in this supplement(Reference Serra-Majem, Frost Andersen and Henriquez-Sánchez12). A total score was calculated according to the mean of the correlation coefficients weighted by the quality score of the validation study. It was considered a poor method for assessing specific nutrient intake when the mean weighted correlation was < 0·30. Methods whose mean weighted correlations were between 0·30 and 0·50 were regarded as acceptable for assessing nutrient intake. Good methods were those whose weighted correlation average was between 0·51 and 0·70, and finally, when the mean weighted correlation was >0·70, the method was considered very good.
Results
A total of seventeen publications(Reference Rondó, Villar and Tomkins2, Reference Brantsaeter, Haugen and Hagve13–Reference Anderson, Hollis and LeVine28) were selected for inclusion, with information on each validation study summarised in Table 2. Six of the publications showed results from European countries (Norway, Denmark, United Kingdom and Finland), ten from American countries (United States of America, Mexico and Brazil) and one study was Australian. The number of participants varied from 16 to 710 in the selected studies.
Table 2 Characteristics of included studies

25(OH)D, 25-hydroxyvitamin D; WDR, weighed dietary records; HSFFQ1, Harvard Service FFQ at 12 gestational week; HSFFQ2, HSFFQ after week 12; HSFFQ3, HSFFQ at 28 gestational week; PFFQ, pregnancy FFQ; SFFQ, semi-quantitative food frequency questionnaire; mWFFQ, modified Willett FFQ.
In five of the studies presented(Reference Rondó, Villar and Tomkins2, Reference Zhou, Schilling and Makrides17, Reference Rifas-Shiman, Fawzi and Rich-Edwards20, Reference Olsen, Hansen and Sandström24, Reference Anderson, Hollis and LeVine28), only one type of micronutrient was analysed, while in the rest of the publications included in the present review, correlations for a wide variety of micronutrients were observed, and a total of twenty-seven micronutrients were analysed. Tables 3–5 show information on the correlation between methods and other statistics in the validation studies in pregnant women for n-3 fatty acids, fifteen vitamins and eleven minerals, respectively. Table 6 presents the classification of the dietary methods utilised for studies in pregnant women according to the mean of the correlation coefficients for each micronutrient weighted by the quality of different validation studies included in the present review. Six studies validated FFQ against 24-h recall(Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Wei, Gardner and Field21, Reference Forsythe and Gage25–Reference Suitor, Gardner and Willett27) analysing a total of twenty-six micronutrients. These assessment methods showed poor correlation for twelve micronutrients and acceptable correlation for eight other micronutrients, while six micronutrients showed a good correlation and therefore a good classification. Two different FFQ were validated against EDR(Reference Erkkola, Karppinen and Javanainen19, Reference Robinson, Godfrey and Osmond23). In these studies applying FFQ v. EDR, twenty-four micronutrients were analysed in which acceptable correlations were observed in twelve micronutrients, whereas another twelve micronutrients presented a good classification. Micronutrients with correlations < 0·3 (poor) were not observed in any study. Additionally, three FFQ were validated against WDR, and a total of fourteen micronutrients were analysed(Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14, Reference Brown, Buzzard and Jacobs22). These assessment methods showed poor correlations only for Na and acceptable correlations for eight micronutrients, while five micronutrients showed a good correlation and therefore a good classification. It should be noted that micronutrients with correlations >0·7 (very good) were not observed in any study. Comparison of different dietary assessment methods in pregnant women by vitamins and minerals is presented in Fig. 2. This figure shows that EDR used as the reference method for evaluating FFQ present better correlations for several micronutrients than other methods in these population groups.
Table 3 Validation studies in pregnant women: n-3 fatty acids

WDR, weighed dietary records; CC, correlation coefficient; BM, biomarker; 24HR, 24-h recall; ALN, α-linolenic acid; HSFFQ2, Harvard Service FFQ after week 12; HSFFQ3, Harvard Service FFQ at 28 gestational week.
Significance: *P < 0·05; **P < 0·01; ***P < 0·001.
† Adjusted for total energy intake.
‡ Adjusted for total energy intake and corrected for random within-person variation.
Table 4 Validation studies in pregnant women: vitamins

24HR, 24-h recall; CC, correlation coefficient; HSFFQ2, Harvard Service FFQ after week 12; HSFFQ3, Harvard Service FFQ at 28 gestational week; EDR, estimated dietary records; WDR, weighed dietary records; BM, biomarker; 25(OH)D, 25-hydroxyvitamin D; PFFQ, pregnancy FFQ; mWFFQ, modified Willett FFQ.
Significance: * P < 0·05; **P < 0·01; ***P < 0·001.
† Adjusted for total energy intake.
‡ Adjusted for total energy intake and corrected for random within-person variation.
§ Density refers to nutrients per 4184 kJ (1000 kcal).
∥ Supplement and non-supplement users.
¶ Sum of plasma α-and γ-tocopherols.
Table 5 Validation studies in pregnant women: minerals

24HR, 24-h recall; EDR, estimated dietary records; WDR, weighed dietary records; BM, biomarker; PFFQ, Pregnancy FFQ; HSFFQ2, Harvard Service FFQ after the week 12; HSFFQ3, Harvard Service FFQ at 28 gestational week.
Significance: * P < 0·05; **P < 0·01; ***P < 0·001.
† Density refers to nutrients per 4184 kJ (1000 kcal).
‡ Adjusted for total energy intake.
§ Adjusted for total energy intake and corrected for random within-person variation.
∥ Supplement and non-supplement users.
Table 6 Classification of the dietary assessment methods utilised for studies in pregnant women according to the quality weighted mean of the correlations for each micronutrient

24HR, 24-h recall; EDR, estimated dietary records; WDR, weighed dietary records; BM, biomarker; DH, diet history.

Fig. 2 Comparison of different dietary assessment methods in pregnant women by vitamins and minerals. Vit, Vitamin; EDR, estimated dietary records; WDR, weighed dietary records; 24HR, 24-h recall; BM, biomarker; DH, diet history. (a) ![]() , FFQ v. 24HR;
, FFQ v. 24HR; ![]() , FFQ v. EDR;
, FFQ v. EDR; ![]() , FFQ v. WDR;
, FFQ v. WDR; ![]() , FFQ v. BM;
, FFQ v. BM; ![]() , WDR v. BM;
, WDR v. BM; ![]() , DH v. BM. (b)
, DH v. BM. (b) ![]() , FFQ v. 24HR;
, FFQ v. 24HR; ![]() , FFQ v. EDR;
, FFQ v. EDR; ![]() , FFQ v. WDR;
, FFQ v. WDR; ![]() , FFQ v. BM;
, FFQ v. BM; ![]() , WDR v. BM;
, WDR v. BM; ![]() , checklist v. BM.
, checklist v. BM.
Moreover, these studies were classified according to which reference method was used and categorised into short-term intake, long-term intake or BM. Ten studies were classified into group 1 with a reference method that reflected short-term intake, in which six applied 24-h recalls(Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Wei, Gardner and Field21, Reference Forsythe and Gage25–Reference Suitor, Gardner and Willett27), two used WDR(Reference Brantsaeter, Haugen and Hagve13, Reference Brown, Buzzard and Jacobs22), one applied EDR(Reference Robinson, Godfrey and Osmond23) and one utilised a diet history (DH)(Reference Zhou, Schilling and Makrides17). Likewise, two other studies were classified into group 2 where the reference method reflected long-term intake (one WDR(Reference Mikkelsen, Osler and Olsen14) and one EDR(Reference Erkkola, Karppinen and Javanainen19)). Finally, in group 3, where dietary methods were validated against BM, seven studies were found(Reference Rondó, Villar and Tomkins2, Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14, Reference Parra, Schnaas and Meydani18, Reference Rifas-Shiman, Fawzi and Rich-Edwards20, Reference Olsen, Hansen and Sandström24, Reference Anderson, Hollis and LeVine28). Some articles presented validations of more than one instrument(Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14).
The FFQ was the main dietary method, which had been validated in fifteen studies. Accordingly, Fig. 3 shows only validation of FFQ studies that assessed n-3 fatty acids and micronutrient intake in pregnant women using a short-term(Reference Brantsaeter, Haugen and Hagve13, Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Wei, Gardner and Field21–Reference Robinson, Godfrey and Osmond23, Reference Forsythe and Gage25–Reference Suitor, Gardner and Willett27) or a long-term(Reference Mikkelsen, Osler and Olsen14, Reference Erkkola, Karppinen and Javanainen19) dietary assessment instrument or BM as a reference method(Reference Rondó, Villar and Tomkins2, Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14, Reference Parra, Schnaas and Meydani18, Reference Rifas-Shiman, Fawzi and Rich-Edwards20, Reference Olsen, Hansen and Sandström24). In regards to the reference method that reflected short-term intake, very good correlations were observed for vitamins E and B6. However, when the reference method used reflected long-term intake, very good correlations were observed only for thiamin. Additionally, BM used as reference methods presented good correlations for folic acid. FFQ validation studies that assessed micronutrient intake in pregnant women, including(Reference Brantsaeter, Haugen and Hagve13, Reference Robinson, Godfrey and Osmond23, Reference Suitor, Gardner and Willett27) or not including(Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Wei, Gardner and Field21, Reference Brown, Buzzard and Jacobs22, Reference Forsythe and Gage25, Reference Greeley, Storbakken and Magel26) dietary supplements, using short-term dietary instruments as the reference method are presented in Fig. 4. When the reference method used reflected short-term intake and the FFQ that were being validated included dietary supplements, poor correlation was observed only for vitamin A.

Fig. 3 Validation of FFQ studies that assess n-3 fatty acids and micronutrient intake in pregnant women using as reference method: short-term or long-term dietary instruments or biomarkers. ![]() , Poor < 0·30; ▨, acceptable 0·30–0·50;
, Poor < 0·30; ▨, acceptable 0·30–0·50; ![]() , good 0·51–0·70;
, good 0·51–0·70; ![]() , very good >0·70. Correlation coefficients weighted by diet quality score.
, very good >0·70. Correlation coefficients weighted by diet quality score.

Fig. 4 Validation of FFQ studies that assess n-3 fatty acids and micronutrient intake in pregnant women, including or not including dietary supplements, using as reference method short-term dietary instruments. ![]() , Poor < 0·30; ▨, acceptable 0·30–0·50;
, Poor < 0·30; ▨, acceptable 0·30–0·50; ![]() , good 0·51–0·70. Correlation coefficients weighted by diet quality score.
, good 0·51–0·70. Correlation coefficients weighted by diet quality score.
Validated dietary methods
Of the seventeen articles included in the present review, fifteen different FFQ had been validated(Reference Rondó, Villar and Tomkins2, Reference Brantsaeter, Haugen and Hagve13–Reference Baer, Blum and Rockett16, Reference Parra, Schnaas and Meydani18–Reference Suitor, Gardner and Willett27). Some articles presented validation of more than one instrument, of which two studies also validated WDR(Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14). A dietary history has been validated in one study(Reference Anderson, Hollis and LeVine28), and a Fe checklist had been validated in another for assessing dietary Fe intake of pregnant women(Reference Zhou, Schilling and Makrides17). Six studies collected information on dietary supplements. All FFQ were designed to capture usual diet; however, the time period covered ranged from habitual diet in the last month (five studies), the last 2 months (one study), the last 3 months (two studies), the last 4 months (one study) or the last 12 months (one study). This information was not specified in five studies. One study developed an Fe checklist for assessing dietary Fe intake of pregnant women, whereas the remaining studies included a wide range of items (55–360 food items) in the questionnaire. The frequency categories reported ranged from three to ten. Six studies developed self-administered FFQ to assess dietary intake during pregnancy and in another five studies, the FFQ were completed by an interviewer.
Reference methods used
Ten studies were classified into group 1 with a reference method that reflected short-term intake, in which six applied 24-h recalls(Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Wei, Gardner and Field21, Reference Forsythe and Gage25–Reference Suitor, Gardner and Willett27), two used WDR(Reference Brantsaeter, Haugen and Hagve13, Reference Brown, Buzzard and Jacobs22), one applied EDR(Reference Robinson, Godfrey and Osmond23) and another a DH(Reference Zhou, Schilling and Makrides17). Likewise, another two studies were classified into group 2 where the reference method reflected long-term intake (one WDR(Reference Mikkelsen, Osler and Olsen14) and one EDR(Reference Erkkola, Karppinen and Javanainen19)). Dietary records (DR) varying in the number of recording days (from 4 to 10 d) were used as the reference method in a total of five studies. The number of repeated 24-h recalls ranged from two to six, which were administered in person or by telephone.
Biomarkers
A total of seven publications analysed BM(Reference Rondó, Villar and Tomkins2, Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14, Reference Parra, Schnaas and Meydani18, Reference Rifas-Shiman, Fawzi and Rich-Edwards20, Reference Olsen, Hansen and Sandström24, Reference Anderson, Hollis and LeVine28), which were used to validate six FFQ and one DH. Some articles presented validation of more than one instrument, of which two studies also validated WDR using BM as reference methods(Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14). The BM analysed were: erythrocyte sum n-3, α-linolenic acid, DHA and EPA in erythrocyte cell membranes; plasma retinol; plasma 25-hydroxyvitamin D concentration (this is a sensitive marker of medium- to long-term vitamin D availability from both dietary and endogenous sources); plasma β-carotene; plasma tocopherol; erythrocyte folic acid; serum folate; erythrocyte folate concentrations (these reflect tissue stores and are a long-term indicator than serum folate); urine iodine excretion.
Discussion
In the present review, seventeen studies(Reference Rondó, Villar and Tomkins2, Reference Brantsaeter, Haugen and Hagve13–Reference Anderson, Hollis and LeVine28) are described. The aim of this analysis was to determine the reliability of methods used to measure the usual intake of vitamins and minerals in pregnant women and how these were validated. The different studies included in the present review were classified according to which reference method was used, those reflecting short-term intake, long-term intake or BM. To rate the different studies, a quality score system was developed by the EURRECA network. A total score was calculated according to the weighted mean of the correlations that had been adjusted by the quality of the different validation studies, and all methods were scored into the categories: poor; acceptable; good; very good. Assessing dietary intake in pregnant women is complicated due to various factors that are dependent on the period of gestation. Poor correlation between instruments may be partly explained by appetite fluctuations and nausea, which may also influence those methods assessing long-term intake(Reference Wirfalt29).
Short-term intake
Ten studies were classified in group 1 with a reference method that reflected short-term intake, in which six applied 24-h recalls(Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Wei, Gardner and Field21, Reference Forsythe and Gage25–Reference Suitor, Gardner and Willett27), two used WDR(Reference Brantsaeter, Haugen and Hagve13, Reference Brown, Buzzard and Jacobs22) and one applied an EDR(Reference Robinson, Godfrey and Osmond23). A DH was used as the reference method in only one study(Reference Zhou, Schilling and Makrides17). Different FFQ were validated for which wide variations in the number of food items were observed (55–360 items). Mouratidou et al. (Reference Mouratidou, Ford and Fraser15) used a sixty-two-item FFQ that yielded higher energy and macronutrients intakes except for alcohol. Highly significant correlations were demonstrated by these authors for most nutrients, from 0·19 for added sugar and Zn to 0·47 for fibre. For most nutrients, positive correlations between the two methods were observed; however, this was not the case for retinol and biotin. In the present study, the percentage of participants classified into the same quintile ranged from 49·6 % for Se and niacin to 66·7 % for Mn. The results of Baer et al. (Reference Baer, Blum and Rockett16) indicated that the Harvard Service FFQ has similar validity during the first and second trimester, as shown by the average deattenuated correlation coefficients of 0·48 and 0·47 for week 12 and week 28 in FFQ compared to the 24-h recalls. These correlations are comparable to those observed among other groups of pregnant women(Reference Erkkola, Karppinen and Javanainen19, Reference Wei, Gardner and Field21, Reference Brown, Buzzard and Jacobs22, Reference Suitor, Gardner and Willett27). Suitor et al. (Reference Suitor, Gardner and Willett27) examined the validity of the Harvard Service FFQ for the assessment of total energies and seven nutrients (protein, Ca, Fe, Zn, vitamins A, B6 and C) among ninety-five low-income pregnant women, comparing intakes estimated from the FFQ to those estimated from three 24-h recalls. With the exception of vitamin A, all of the deattenuated correlation coefficients for nutrient intakes were >0·50. Wei et al. (Reference Wei, Gardner and Field21) extended these results in the same group of women by examining the validity of the Harvard Service FFQ for the assessment of seventeen additional nutrients; they reported a mean deattenuated correlation of 0·47, with correlations ranging from 0·03 for vitamin B12 to 0·90 for Zn. In general, there was good agreement for many nutrients when comparing nutrient intakes assessed in a population of pregnant women by FFQ and 24-h recalls. However, overestimation in the intake of some nutrients was observed when determined by the FFQ than when determined by 24-h recalls. The effects of certain limitations of the 24-h recall method, e.g. reliance on memory and high day-to-day variation, might have been decreased by the collection of more than two dietary recalls(Reference Mouratidou, Ford and Fraser15).
Robinson et al. (Reference Robinson, Godfrey and Osmond23) observed that the FFQ estimates of nutrient intake were higher when compared with the 4-d EDR. This may be the result of the standard portion sizes used in the FFQ being too large, of over-reporting of the frequency of consumption of foods in the FFQ, or of under-reporting of foods consumed in records, both in amount and in frequency. Good agreement between the FFQ and 4-d WDR regarding dietary supplement use and total intake estimates was found by Brantsaeter et al. (Reference Brantsaeter, Haugen and Hagve13). In Brown et al. (Reference Brown, Buzzard and Jacobs22), 4-d WDR were also used to estimate dietary intake, but 4 d for each period were likely to be insufficient to capture a representative estimate of nutrient intake that has large day-to-day variability. Repeated measures of dietary intake would have allowed for greater control of within-person variability and improved comparative correlations(Reference Brown, Buzzard and Jacobs22).
Zhou et al. (Reference Zhou, Schilling and Makrides17) represents the only validation study of a single nutrient checklist designed to assess Fe intake in pregnant women. There was no difference in mean Fe intake reported in the DH and the Fe checklist, and there were good correlations between Fe intakes estimated from both methods. The correlation was strengthened when the contribution of Fe from supplements was included. Other validation studies of FFQ in pregnant women were designed for multiple nutrient assessments(Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Erkkola, Karppinen and Javanainen19, Reference Robinson, Godfrey and Osmond23, Reference Greeley, Storbakken and Magel26, Reference Suitor, Gardner and Willett27), and they reported low correlations for Fe (r 0·39–0·60) between FFQ and DR(Reference Erkkola, Karppinen and Javanainen19, Reference Robinson, Godfrey and Osmond23) or between FFQ and 24-h recall (r 0·32–0·56)(Reference Mouratidou, Ford and Fraser15, Reference Baer, Blum and Rockett16, Reference Greeley, Storbakken and Magel26, Reference Suitor, Gardner and Willett27). Other studies reported comparable correlations for Fe (r 0·67) between FFQ and DR(Reference Brown, Buzzard and Jacobs22), or between FFQ and 24-h recall (r 0·68)(Reference Wei, Gardner and Field21). A simple assessment tool, such as an Fe checklist to identify pregnant women with low-Fe intake that need further assessment and appropriate intervention, could be useful for clinical practice and in research for assessing Fe intake of groups in large-scale studies.
Long-term intake
Likewise, another two studies were classified into group 2, where the reference method reflected long-term intake (one EDR(Reference Mikkelsen, Osler and Olsen14) and one WDR(Reference Erkkola, Karppinen and Javanainen19)). Mikkelsen et al. (Reference Mikkelsen, Osler and Olsen14) analysed FFQ against 7-d WDR and showed that correlation between the two dietary methods was r 0·39 for protein intake, whereas other studies had found higher correlations(Reference Erkkola, Karppinen and Javanainen19, Reference Brown, Buzzard and Jacobs22, Reference Robinson, Godfrey and Osmond23). In Mikkelsen's study, when the women were classified into quintiles of protein intake estimated from the FFQ, a significant increasing trend in intake estimated from 7-d WDR was observed. Significant correlations ranging from 0·35 to 0·56 were found by these authors when comparing the two dietary methods, and the highest correlations were found for folic acid from dietary supplements. In a study of 113 Finnish women in their third trimester of pregnancy, Erkkola et al. (Reference Erkkola, Karppinen and Javanainen19) obtained an average deattenuated correlation coefficient of 0·53 for forty-five nutrients assessed by a 181-item FFQ and two 5-d EDR. These authors observed that the intake of food and nutrients was higher as determined by FFQ than intake assessed using two 5-d EDR. Earlier validation studies conducted in pregnant women have reported similar overestimates using FFQ compared with DR or 24-h recalls(Reference Robinson, Godfrey and Osmond23, Reference Forsythe and Gage25–Reference Suitor, Gardner and Willett27). Overestimation may reflect difficulties in comparing the standard portion size offered with the portion that is actually consumed. The use of a DR is likely to have the least correlated errors as this method does not depend on memory (recorded after each meal). In contrast, the major sources of error with FFQ are due to restrictions imposed by memory and perception of portion sizes.
Biomarkers
Anderson et al. (Reference Anderson, Hollis and LeVine28) showed the correlation between maternal dietary history of vitamin D intake and maternal serum 25-hydroxyvitamin D levels. These results presented poor classification and weak correlation between the two assessment methods (r 0·072). Other validation studies in pregnant women reported better correlations for vitamin D (r 0·45)(Reference Brantsaeter, Haugen and Hagve13) between FFQ and BM or between WDR and BM (r 0·51)(Reference Brantsaeter, Haugen and Hagve13).
On the other hand, six FFQ(Reference Rondó, Villar and Tomkins2, Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14, Reference Parra, Schnaas and Meydani18, Reference Rifas-Shiman, Fawzi and Rich-Edwards20, Reference Olsen, Hansen and Sandström24) were validated against BM. These assessment methods presented poor correlations for five nutrients, acceptable correlations for three nutrients and only one nutrient presented a good correlation (folic acid, r 0·55 for total folic acid). Rondó et al. (Reference Rondó, Villar and Tomkins2) compared plasma concentrations of vitamin A in 710 women after delivery with a simplified FFQ that included fifty-five food items and observed poor correlations between methods (r 0·11). There were very few studies comparing vitamin A intake, as reported on a FFQ with the corresponding biochemical indicator of vitamin A status. In countries where vitamin A deficiency is not a public-health problem, plasma carotenoids showed a higher statistically significant correlation with dietary questionnaires (although weak) than plasma levels of retinol(Reference Jarvinen, Knekt and Seppanen30–Reference Scott, Thurnham and Hart32). Dietary intake of n-3 PUFA estimated from five different FFQ(Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14, Reference Parra, Schnaas and Meydani18, Reference Rifas-Shiman, Fawzi and Rich-Edwards20, Reference Olsen, Hansen and Sandström24) was validated against fatty acids in serum, plasma or erythrocytes. The best correlation was observed in the study by Rifas-Shiman et al. (Reference Rifas-Shiman, Fawzi and Rich-Edwards20) comparing the dietary intake of fatty acids from a modified version of the Willett semi-quantitative food frequency questionnaire with blood levels of fatty acids (r 0·98). The Pearson correlation coefficients observed in Parra et al. (Reference Parra, Schnaas and Meydani18) among α-linolenic acid, DHA and EPA in erythrocytes against crude dietary concentration were 0·32, 0·35 and 0·36, respectively. After adjustment for total energy intake, these correlations remained similar. The present study showed that the FFQ is adequate to identify the highest and lowest quartiles of n-3 fatty acid intake among pregnant women. A correlation coefficient of 0·32 for α-linolenic acid is relatively high compared with findings from other observational studies correlating biochemical markers to estimated dietary intake. In a similar analysis, Olsen et al. (Reference Olsen, Hansen and Sandström24) reported a correlation coefficient of 0·02 for α-linolenic acid. Mikkelsen et al. (Reference Mikkelsen, Osler and Olsen14) observed that the estimated intake of n-3 fatty acids from the FFQ (r 0·37, P < 0·001) was significantly correlated with erythrocyte EPA. Moreover, there was no correlation between total intake and plasma retinal, and the intake estimated from the FFQ did not correlate with protein excretion (however, one 24-h urine sample is a short-term BM of intake), whereas total folic acid intake was significantly correlated with erythrocyte folic acid level. Brantsaeter et al. (Reference Brantsaeter, Haugen and Hagve13) demonstrated a strong association between BM concentration/excretion and self-reported intake of those nutrients as calculated from the FFQ. A major strength of the present study was that it included BM that reflected long-term as well as short-term intakes. Poor correlations were found between 4-d WDR and plasma concentrations of retinol and tocopherol, and plasma concentrations did not differ between supplement and non-supplement users for tocopherol. This is in agreement with studies in pregnant as well as non-pregnant populations(Reference Scaife, McNeill and Campbell33). Seasonal differences in the correlations between vitamin D intake and BM concentration found in Brantsaeter's study(Reference Brantsaeter, Haugen and Hagve13) were similar to those described in non-pregnant populations(Reference Jacques, Sulsky and Sadowski31, Reference Salamone, Dallal and Zantos34). Likewise, the calculated folate intake was more strongly correlated with serum folate than with erythrocyte folate. In other population studies, serum folate has also been found to be strongly correlated with intake(Reference Jacques, Sulsky and Sadowski31).
Additionally, two WDR were validated against BM(Reference Brantsaeter, Haugen and Hagve13, Reference Mikkelsen, Osler and Olsen14), and these assessment methods showed poor correlation for two nutrients (retinol and vitamin E) and acceptable correlation for five nutrients, whereas protein and vitamin D presented a good classification. Blood sampling and 24-h urine collections were done close to when DR were conducted, so a stronger association between the DR and BM than between FFQ and BM could be expected, at least for BM with a relatively short elimination time. In this manner, Brantsaeter et al. (Reference Brantsaeter, Haugen and Hagve13) observed a stronger association between erythrocyte n-6:n-3 fatty acid ratio and dietary intake n-6:n-3 fatty acid ratio for the FFQ than for the 4-d WDR, indicating that the FFQ reflects true long-term intake better than 4-d WDR.
Conclusion
The aim of the present review was to determine the reliability of methods used to measure the usual intake of vitamins and minerals in pregnant women and to evaluate how these were validated. When comparing different validation methods, the FFQ presents better correlations when EDR are used as the reference method. The FFQ administered to pregnant women showed a wide variety of included food items, ranging from 55 to 360. The frequency categories reported were from three to ten. Further research is needed to clarify the optimal number of food items and frequency categories to be included in questionnaires targeting this population group. FFQ appeared to be the most reliable for measuring short-term intakes of vitamins E and B6 and short- and long-term intakes of thiamin. They were also good for measuring short-term intakes of Zn, Fe, riboflavin and folate, and long-term intakes of vitamins B6, C, niacin, pantothenic acid, Fe, Na, Ca, riboflavin, retinol, β-carotene, folic acid, Mn and iodine. For n-3 fatty acids, the best ranking was observed when analysing FFQ applying short-term reference methods (r 0·51) than when BM (r 0·41) were used as reference methods. When frequency methods were used for assessing micronutrient intake, the inclusion of dietary supplements improved their reliability for most nutrients, except for vitamin A (r < 0·3). When FFQ methods were used for assessing folic acid intake, similar correlations were observed when both long-term intake (r 0·53) and BM (r 0·55) were used as reference methods. Both long-term intake and BM reference methods showed stronger correlations in folic acid intake (r 0·53 and 0·55, respectively) than in folate intake (r 0·48 and 0·26, respectively). The information on folic acid in dietary supplements is better defined than the folate content of the diet. Thus, it is crucial to take into account the use of dietary supplements. These are very popular, especially among pregnant women. Apart from folic acid, BM do not add any more certainty as to the reliability of intake methods. On comparing FFQ methods used for assessing micronutrient intake with long-term reference methods, acceptable or good correlations except for vitamin E were obtained. Intake of this vitamin correlated better with short-term daily intake (r>7) rather than with long-term daily intake. Nelson et al. (Reference Nelson, Black and Morris35) estimated that the number of days required to rank vitamin E intake with desired precision was sixteen. In studies where the reference method reflected long-term intake, 7-d WDR or two 5-d EDR were applied. Repeated measures of dietary intake would have allowed for greater control of within-person variability and improved comparative correlations. The DR should cover at least four weekdays and one weekend day including information on the use of dietary supplements. The use of a booklet with pictures of common foods and mixed dishes is recommended to facilitate the estimation of portion sizes.
Acknowledgements
The studies reported herein have been carried out within the EURRECA Network of Excellence (www.eurreca.org), financially supported by the Commission of the European Communities, specific Research, Technology and Development Programme Quality of Life and Management of Living Resources, within the Sixth Framework Programme, contract no. 036196. This report does not necessarily reflect the Commission's views or its future policy in this area. A. O.-A. wrote the first manuscript; A. O.-A., J. D.-A. and P. H.-S. contributed to the planning of the search and analysed the articles included in the present review; I. C. revised and discussed previous drafts; L. S.-M. contributed to the planning of the search, decided the analysis and presentation of results and created the quality assessment tool of the articles, and revised and discussed previous drafts. There are no conflicts of interest to report. The authors of the present paper would like to thank Drs Margaret Ashwell, Janet Lambert, Adriënne Cavelaars, Olga Souverein and Mrs Sandra Crispim for their technical contribution to this publication. The authors also thank the Health Sciences Library of the University of Las Palmas de Gran Canaria, Lourdes Ribas and Nuria Melián for their contribution in the collection of articles analysed in the present review. Special thanks to Joy Ngo, RD for her help in editing the English version of the manuscript.