The COVID-19 pandemic spread quickly around the world in 2020–2021, resulting in significant setbacks in progress towards the sustainable development goals. Whereas the global prevalence of severe food insecurity steadily declined since the year 2000, it has again risen from 9·3 % in 2019 onwards to 11·7 % in 2021, following multiple global crises including the pandemic(Reference Burki1,2) . Currently, close to 800 million people experience hunger, the majority of whom lives in Asia. Simultaneously, the pandemic has had profound adverse effects on the mental health condition of youth worldwide. According to UNICEF, lockdowns have had a direct impact on mental health of at least one out of seven students worldwide(3). Evidence for this unwanted side effect mostly comes from high-income countries(Reference Pierce, Hope and Ford4–Reference Dietze and Peacock6). The few studies from low- and middle-income countries have mainly relied on convenience samples and Internet-based surveys, which are unlikely to be representative and to reach the rural poor. Food security and mental health are linked through complex pathways of interconnected determinants(Reference Pourmotabbed, Moradi and Babaei7,Reference Maynard, Andrade and Packull-McCormick8) . In a recent systematic evidence gap map including 1895 studies on Food and Nutrition Security (FNS) and mental health, it was concluded that most scientific information on this topic comes from high-income countries, and that there were only few that combined design, contextual factors and analyses to provide the most needed information to develop efficient programmes and policies(Reference Sparling, Deeney and Cheng9).
In Indonesia, a Large-Scale Social Restriction (PSBB) in response to the COVID-19 pandemic was stipulated starting in April 2020. This has disrupted food security in terms of availability and access to food, with 13 % of households reporting food shortages(10). As reported from other countries, reduced household income may also have impacted food availability and household food security(Reference Tran, Nguyen and Le11). This has given rise to increased malnutrition in the country(12,13) . Unfortunately, little is known about the impact of the pandemic on nutritional status of Indonesian adolescents, nor on their mental health condition. One study showed a higher occurrence of social behaviour problems due to increased subjective anxiety during the COVID-19 pandemic, triggered by social media(Reference Wiguna, Anindyajati and Kaligis14). We have previously shown that, against the backdrop of the COVID-19 pandemic, certain typologies of depression predicted the occurrence of anaemia 1 year later among adolescents living in Gunungkidul, Yogyakarta(Reference Asrullah, Maula and Listyadewi15). It has also been demonstrated that unhealthy dietary patterns and diet quality are associated with depression and, in some cases, with severe anxiety(Reference Sparling, Deeney and Cheng9,Reference Li, Lv and Wei16,Reference Lai, Hiles and Bisquera17) . There is only limited evidence of a link between food security and mental health among adolescents(Reference Jung, Kim and Bishop18,Reference O’Keeffe, Kelly and O’Herlihy19) . Addressing these factors is crucial for preventing outbreaks and pandemics, as poor nutrition and mental health can weaken immune responses, making adolescents more susceptible to diseases. Immediate intervention is needed to mitigate severe health outcomes and support long-term well-being. The present study aims to determine the association between food security, nutrition and mental health among Indonesian adolescents during the COVID-19 pandemic. Insights from this research can guide effective policies and interventions, not only for Indonesia but also for other regions facing similar challenges, ultimately contributing to better pandemic preparedness and public health strategies.
Method
Study design and participants
In this study, we collected information from 576 adolescents, including 286 boys and 286 girls, who were between the ages of 10 and 19 years, in Gunungkidul district, Yogyakarta province, Indonesia. In data collection procedure, we first randomly selected nine subdistricts based on probability proportional to size from three areas: north, central and south. Next, in each of the chosen subdistricts, two villages were selected, and we randomly selected eight girls and eight boys from each of these eighteen villages according to age group: 10–14 years and 15–19 years. To enable this, we first conducted a listing survey for which we visited all villages and all households with adolescents. This resulted in a list of 9942 adolescents who could potentially be part of our study. If a selected adolescent refused participation, we applied random replacement with another adolescent from the same village. The selection procedure and data collection only covered rural areas, and therefore this study does not reflect urban areas.
Data collection
In Indonesia, school closures due to the COVID-19 pandemic were implemented from March 2020 until April 2022. The gathering of baseline data occurred from May to August 2021. Subsequent follow-up data collection took place from May to July 2022. Initially, data were collected from a total of 576 adolescents. Among them, 288 were boys and 288 were girls. However, during the follow-up period, only 511 adolescents continued to participate in the study (222 boys and 230 girls; Fig. 1). Loss to follow-up was mostly (71 %) due to relocation. Nevertheless, there were no discernible differences in characteristics between adolescents who remained in the study and those who dropped out (online Supplementary Table 1).
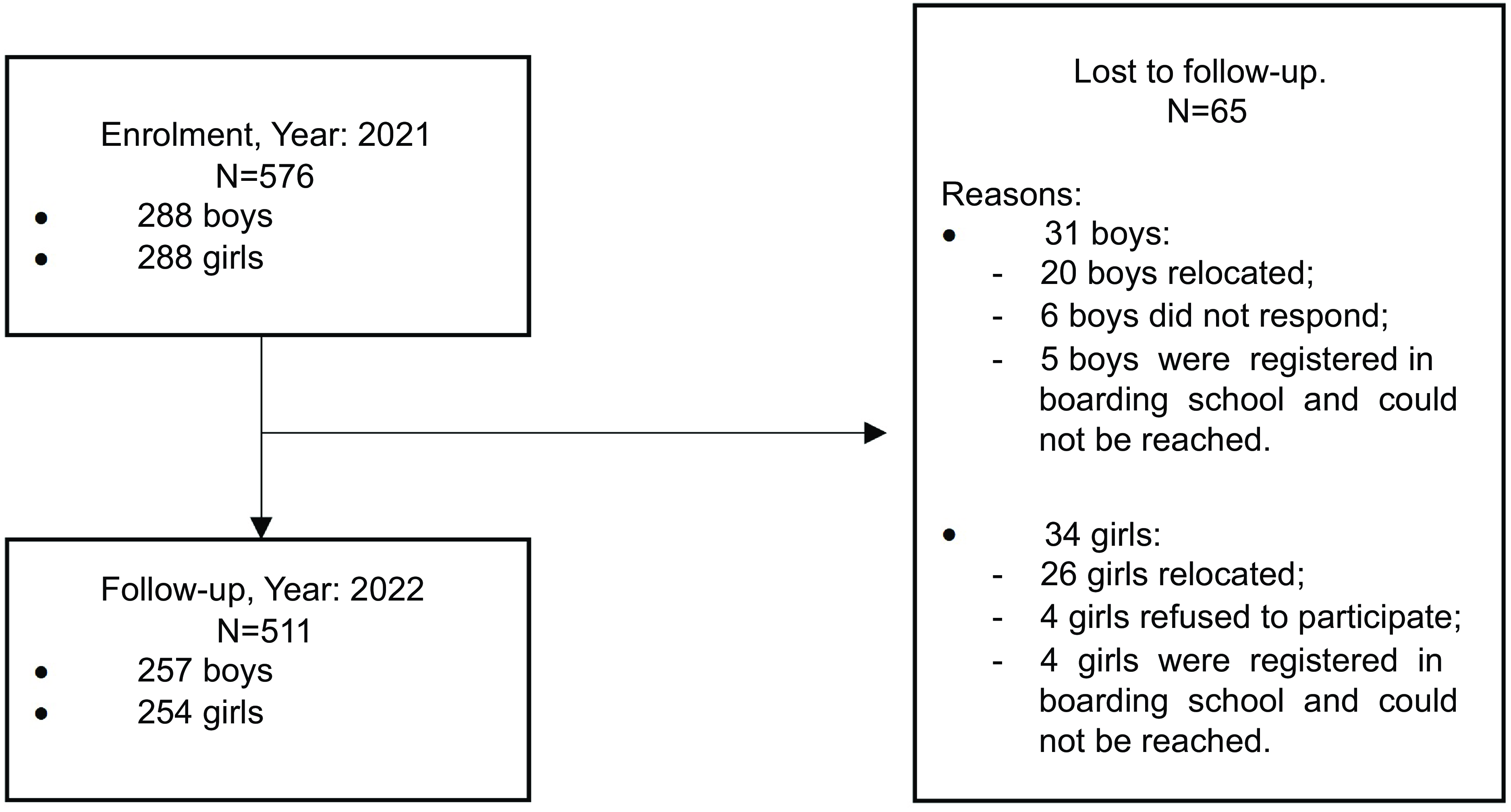
Figure 1. Flow chart of enrolment (year: 2021) and follow-up (year: 2022) of adolescents from Gunungkidul district, Yogyakarta, Indonesia.
All procedures for data collection have been described in a previous publication(Reference Asrullah20). In summary, data collectors visited the selected adolescents, chosen through random sampling, at their residences. Permission letters from authorities, including subdistrict, village and sub-village heads, were carried by the data collectors. Prior to conducting interviews, an information sheet and consent form was signed by the adolescents themselves as well as their parents or guardians.
For data collection, two mobile data collection software programs were utilised: ODK Collect by Get ODK Inc. and Offline Surveys by LimeSurvey GmbH. This mobile data collection set-up was designed to minimise errors during data entry and management. To ensure practicality and reliability, these software programs were continuously tested during a pilot phase and their performance was further assessed during the initial week of data collection. Automated checks of completed answers were implemented for data quality control, and advanced settings were incorporated in the answer boxes to prevent improper data entry during interviews. Interviews were recorded to ensure adherence to established protocols and to aid data managers in the verification processes. In instances of power supply issues or software challenges, data collectors swiftly transitioned to a paper-based questionnaire. Data collectors entered the manual data into the online database on the same day under supervision of the field coordinator and data managers. Subsequently, paper-based questionnaires were uploaded to the ODK software tool for further data verification, if necessary. Each data manager was tasked with verifying the work of four data collectors. Additionally, to uphold data validity, several respondents in each village were randomly revisited. Feedback from respondents and village leaders was sought to validate the interview process, survey listing and mapping methods executed by data collectors. To minimise interview bias, the same data collectors conducted interviews during both the baseline and follow-up phases. Interviews were conducted away from adolescents’ homes and without the presence of parents to maintain objectivity. On average, each interview lasted up to 90 min, adhering to a consistent and objective approach throughout the study.
Study variables
Food security and food consumption
Household food security before and during the pandemic was measured using an adapted version of the Household Food Insecurity Access Scale (HFIAS). The HFIAS comprises ten questions of occurrence and severity food insecurity. Occurrence questions (nine questions), inquire about specific food insecurity conditions in the past 4 weeks, with response options of 0 for no and 1 for yes. The HFIAS score quantifies household food insecurity over the past 4 weeks. Total score (scores range from 0 to 27) can be calculated by summing frequency-of-occurrence question codes, treating instances where occurrence questions were answered ‘no’ as 0, ‘rarely’ as 1, ‘sometimes’ as 2 and ‘often’ as 3. The Household Food Insecurity Access Prevalence (HFIAP) status indicator, used to report household food insecurity, categorises households into four levels of food insecurity: food-secure, mildly, moderately and severely food-insecure(Reference Coates, Swindale and Bilinsky21). In addition, dietary diversity score was assessed by total count of the following ten food groups when being consumed in the previous 24 h: starchy staples, dark-green leafy vegetables, vitamin A-rich fruits and vegetables, other vegetables, other fruits, flesh and organ meat, eggs, fish, legumes/nuts/seeds and milk products. We also assessed the consumption of risk foods, referring to the consumption of salty food, high-fat food and soft drinks, which was classified as low if adolescents consumed such foods only 1–2 times a week, moderate if they consumed them 3–6 times a week and high if they consumed them every day.
Anthropometric measurements
Weight and height were measured to assess nutritional status. Anthropometric measurements were mostly taken in the respondents’ home straight after the interviews, to minimise response bias. Adolescent height was measured to the nearest 0·1 cm using a stadiometer (Kenko Stadiometer 250). Weight was measured without shoes and other accessories and recorded to the nearest 0·1 kg using a flat digital weighing scale (GEA EB1622), placed on a flat surface. Height and weight were measured and recorded twice, with an acceptable difference of 0·2 cm and 0·1 kg. All equipment was calibrated by the Certified Health Laboratory and Calibration Unit, Yogyakarta.
Hb data were collected from all adolescents who were willing to have their finger-prick blood taken, using HemoCue 201+ (HemoCue AB). After correction of Hb concentrations for altitude and smoking(22), anaemia was classified as Hb < 11·5 g/dl for adolescents aged 10–11 years, < 12 g/dl for those aged 12–14 years and for girls aged 15 years and older, and < 13 g/dl for boys aged 15 years and older. All adolescents included at baseline (n 576) underwent the finger-prick test, whereas at follow-up the response rate was lower (n 452).
Assessment of mental health
The Kessler-10 Psychological Distress Scale (K10) was used to measure non-specific psychological distress in the anxiety-depression spectrum, that is, levels of nervousness, agitation, psychological fatigue and depression in the past 4 weeks. The K10 has been translated and validated in Bahasa Indonesia (all the scales had Cronbach’s α > 0·8, with sensitivity of 85·7 % and specificity of 74·7 %). The K10 comprises of ten questions that have strong psychometric properties by which psychiatric cases and non-psychiatric cases can be discriminated (online Supplementary Table 1). A cut-off ≥ 18 points was used to determine the prevalence of depression among adolescent boys and girls(Reference Tran, Kaligis and Wiguna23).
Other variables
At the household level, parental education was ascertained as the highest educational attainment achieved by the parents. Additionally, parental occupation was evaluated, denoting the nature of the income-generating activities in which the parents were engaged. Household size was determined by number of all occupants residing within the same domicile, irrespective of their formal household registration. Notably, this enumeration accounted for instances where multiple households cohabited within the same physical structure, a phenomenon prevalent in the Indonesian context. Household total income was defined as the aggregate income derived from all family members, encompassing both sustenance and non-sustenance expenditures. This income was stratified into distinct categories, specifically: less than IDR 3.000.000 (categorised as low), ranging between IDR 3.000.000 and IDR 5.000.000 (categorised as moderate) and exceeding IDR 5.000.000 (categorised as high).
Statistical analysis
Frequency distribution and percentages were calculated for all variables both at baseline (2021) and at follow-up (2022). χ 2 tests were utilised to investigate the differences in characteristics between years. Additionally, a paired t test was used to compare the means of the continuous variable at baseline and follow-up. Directed acyclic graph was constructed to determine the confounders and the causal inference of the variables to food security, nutritional status and depression score (online Supplementary Fig. 1). All variables outlined in the directed acyclic graph were included in the analysis. Assumptions and multicollinearity were checked, and all values were found to be within the moderate to low range.
Furthermore, stepwise regression was performed using forward and backward elimination techniques to identify the most appropriate variables for predicting depression scores. Lastly, to analyse the relationships between food security and nutritional status with depression longitudinally among this cohort of adolescents, a linear mixed-effects regression model was employed. All statistical analyses were conducted using STATA-17 packages, with a significance level of P < 0·05.
Result
The characteristics of the adolescents who participated in the study are detailed in Table 1. The majority were students, of normal weight and in early puberty. Notably, there was a high prevalence of smoking (18·3 % in 2021 and 16·8 % in 2022) and overweight-obesity (20·7 % in 2021 and 19·3 % in 2022). Additionally, most parents had only elementary school education, unsecured jobs and low incomes.
Table 1. Individual and household characteristics of adolescents (10–19 years) living in Gunungkidul, Yogyakarta, Indonesia, during COVID-19 pandemic year 2021 (n 576) and 2022 (n 511) (Numbers and percentages; median and minimum and maximum values; mean values and standard deviations)
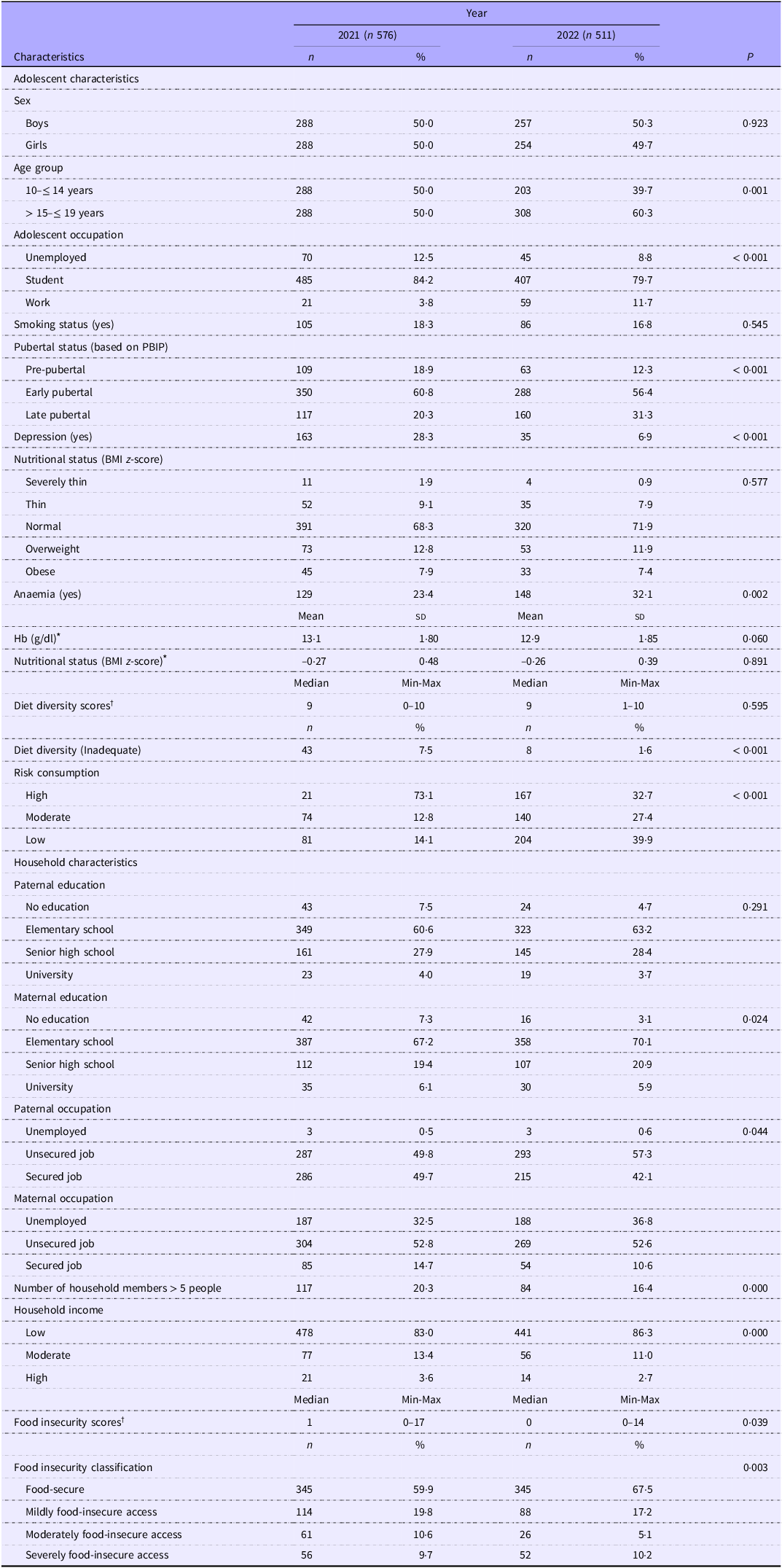
* Data are presented as Mean (sd).
† Data are presented as Median (Min-Max).
There was a large reduction in depression from year 2021 (28·3 %) to follow-up (6·9 %). Reversely, anaemia was more prevalent at follow-up (32·1 %) compared with baseline (23·4 %) and was more prevalent among girls compared with boys (year 2021:33·5 v. 12·7 and year 2022:45·5 v. 18·7, respectively). Notably, there was an improvement in the prevalence of inadequate diet diversity (7·5 % v. 1·6 %), a reduction in the consumption of high-risk foods (73·1 % v. 32·7 %) and an increase in food security (59·9 % v. 67·5 %) after 1 year of follow-up.
Bivariate associations between adolescent and household factors and depression scores at both time points are shown in Table 2. In 2021, being a girl, older age and higher household income were associated with higher depression scores; however, only sex and age remained associated with mental health in 2022 in bivariate analysis. Regarding access to food during the COVID-19 pandemic, there were marked reductions in access to all means of food sourcing during both years of study, including access to wet markets, groceries, warung (small food stores), vegetable warung, mobile stalls, own gardens and barter systems (Fig. 2). The association between moderate and severe food-insecure access with depression scores became stronger from baseline to follow-up (moderate: β: 1·36 (95 % CI −0·10, 2·83) to 4·63 (95 % CI 2·17, 7·09); severe: 1·89 (95 % CI 0·36, 3·41) to 3·30 (95 % CI 1·50, 5·10)). Additionally, inadequate diet diversity and lower Hb concentration were found to be associated with higher scores of adolescent depression (Table 3).
Table 2. Bivariate associations between individual and household factors with mental health outcome of adolescents (10–19 years) living in Gunungkidul, Yogyakarta, Indonesia during COVID-19 pandemic year 2021 (n 576) and 2022 (n 511) (Beta and 95 % confidence intervals)
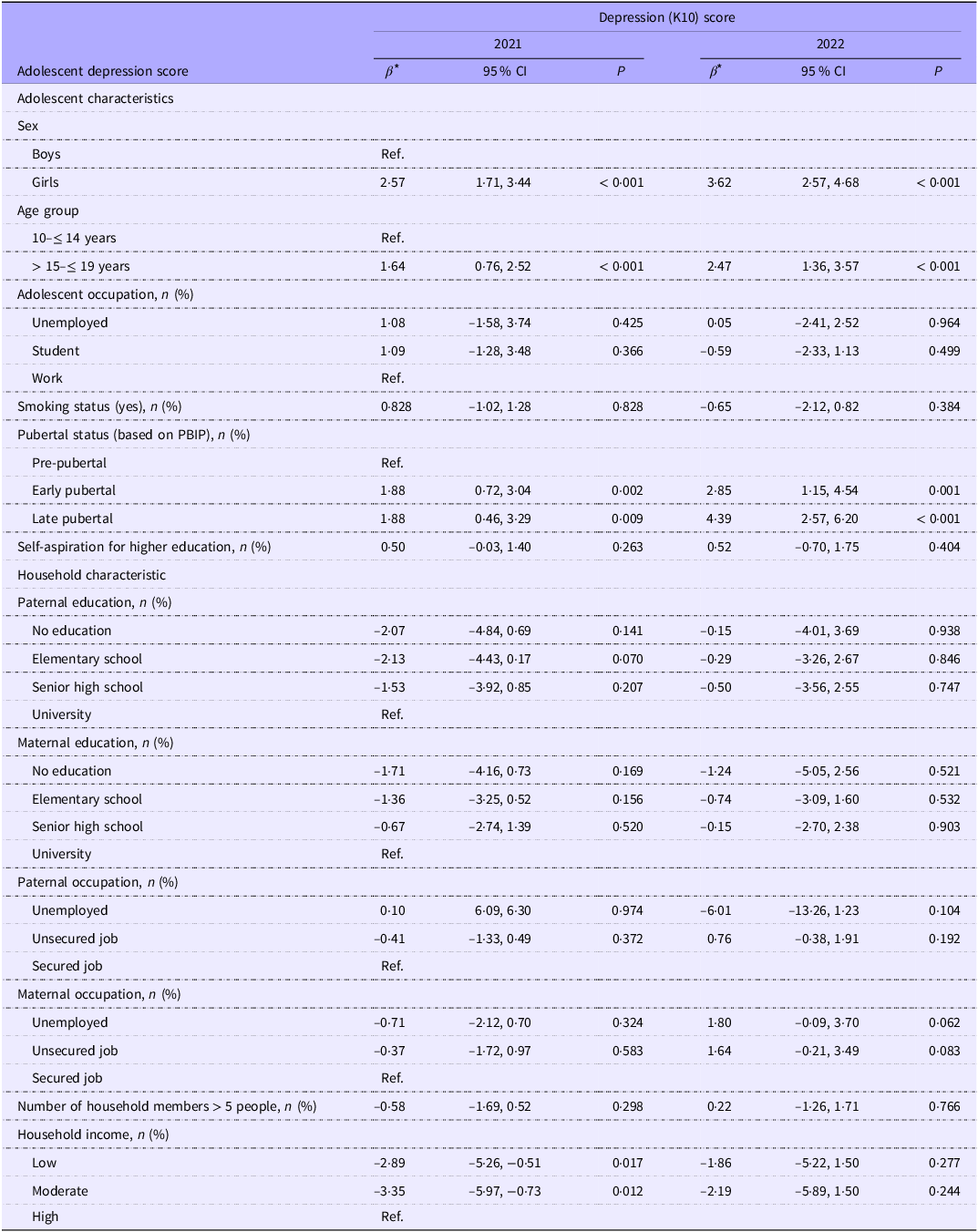
* Unadjusted β from regression analysis.

Figure 2. Household food sourcing in COVID-19 year 2021 and 2022. The percentage indicates respondents who replied ‘yes’, and multiple answers are allowed.
Table 3. Association between food security and nutrition to mental health of the adolescents in year 2021 (n 576) and 2022 (n 511) (Beta and 95 % confidence intervals)

* Unadjusted effect from regression analysis.
In the longitudinal analysis (Table 4), it was observed that a higher food insecurity score was associated with higher scores of depression in adolescents (β: 0·72, 95 % CI 0·52, 0·92)), while BMI z-score was inversely associated with depression score (β: −0·31, 95 % CI 0·68, −0·03)). Diet diversity scores and Hb concentrations were negatively associated with depression scores, but a null-effect could not be ruled out. Although the interaction was not statistically significant, we observed an interaction effect between age and sex in the relationship between Hb and depression. Specifically, we noted a trend where older boys exhibited a stronger association between higher Hb and depression, whereas the opposite trend was observed in girls, with older age associated with lower effect of Hb on depression.
Table 4. Longitudinal associations (unadjusted and adjusted) between food security, diet diversity, Hb concentration and BMI z-score with depression among adolescents 10–19 years living in Gunungkidul, Yogyakarta, Indonesia, during the COVID-19 pandemic using a mixed-effects linear model (n 511) (Beta and 95 % confidence intervals)
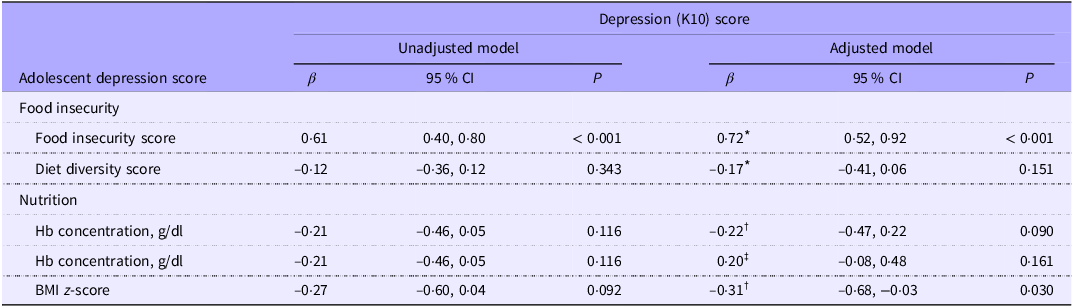
* Adjusted for sex, age, pubertal status and household income.
† Adjusted for age.
‡ Adjusted for age and sex.
Discussion
We investigated the relationship between household food security and nutritional factors with mental health of adolescents living in Gunungkidul, Yogyakarta, Indonesia, during the COVID-19 pandemic. We found that, overall, there was a striking decline in depression from the first to the second year of the pandemic. Food security improved from baseline to follow-up as well as diet diversity, whereas the prevalence of anaemia increased especially among girls. Our data indicate that household food insecurity was associated with higher depression scores, whereas higher BMI z-scores were associated with lower depression scores among adolescents in Gunungkidul district.
The improvement in food security and diet diversity during the COVID-19 pandemic may be attributed to government assistance, which included the provision of cash or food items (typically rice, noodles and oil). This assistance has helped protect households from food insecurity, especially during the pandemic(24). However, this information was not collected in the present study. Furthermore, we found the improvement of food security is linked with better dietary diversity, consistent with previous research showing that greater dietary diversity can be a reliable measure of food security and reflects higher household consumption and energetic availability from non-staples(Reference Antwi, Quaidoo and Ohemeng25). Improvement of food security was also associated with a reduction in high-risk food consumption, likely due to more consistent access to a variety of foods, which supports better dietary choices(Reference Hoddinott and Yohannes26).
Our findings align with a previous longitudinal study in 2601 Singaporean children which showed that food insecurity during the COVID-19 pandemic was associated with children’s well-being(Reference Chen and Yeung27). A study among adolescents living in an urban slum area in Bangladesh found that, during the pandemic, moderate and severe food insecurity was related to harmful coping strategies that are likely to have negative implications for health and well-being(Reference Yasmin, Yasmin and Sultan28). Our results are also consistent with earlier studies that were conducted before the COVID-19 pandemic era. A study in the USA among parents who had at least one child < 18 years of age highlighted the detrimental impact of food insecurity on the mental well-being of adolescents(Reference Patrick, Henkhaus and Zickafoose29). Furthermore, a systematic review of 108 studies including 203 822 children aged 2–17 years showed significant correlations between food insecurity and depression, including externalising and internalising behaviours as well as hyperactivity(Reference Cain, Meyer and Cummer30). Also, a large study involving 132 618 individuals aged 15 years or older from 138 countries found a significant association between food insecurity and subjective well-being(Reference Frongillo, Nguyen and Smith31). Similarly, a study in Ethiopia discovered that facing food insecurity and dealing with stressful life events were both linked to increased symptoms of depression, anxiety and post-traumatic stress(Reference Hadley, Tegegn and Tessema32). In addition, a longitudinal study among 2120 children conducted in Canada reported that family food insecurity predicted children’s adverse mental health symptoms, particularly hyperactivity and inattention(Reference Melchior, Chastang and Falissard33). Taken together, these findings suggest a universal impact of food insecurity on mental health and well-being of adolescents.
A potential mechanism to explain the connection between food insecurity and depression could be that adolescents who face food insecurity experience higher levels of stress and anxiety(Reference Essadek, Shadili and Bergami Goulart Barbosa34), which may be further exacerbated by inadequate dietary intake and poorer nutritional status(Reference Elgar, Sen and Gariépy35). Parents in food-insecure households also experience more emotional distress(Reference Ling, Duren and Robbins36,Reference Fang, Thomsen and Nayga37) , which may affect their parenting style by resorting to harsher disciplinary methods, all of which contribute to their children’s behaviour issues(Reference McIntyre, Williams and Lavorato38,Reference Whitaker, Phillips and Orzol39) . Another possible pathway could be that food insecurity and consequent malnutrition may impact brain health via alterations in neurotransmitter release, either directly or via alterations in the gut microbiota(Reference Owen and Corfe40,Reference Shankar, Chung and Frank41) .
In relation to nutritional status, we found a higher BMI z-score to be associated with lower depression scores among our Indonesian study population. A previous study among 39 542 French adolescents aged 17 years found that the effect of BMI on mental health differs between the sexes: boys exhibited a U-shaped association, indicating elevated depression levels for those who were either too thin or too fat, while girls, conversely, showed an initial U shape followed by an inverse convex curve. The latter suggests that underweight girls experienced higher depression levels than normal-weight girls, whereas level of depression was higher in overweight compared with obese girls(Reference Revah-Levy, Speranza and Barry42,Reference Wardle, Williamson and Johnson43) . In line with this, our findings, as BMI changes in our study were more prominently associated with alterations in severely thin, thin and normal-weight adolescents compared with those with overweight and obese individuals (online Supplementary Fig. 2).
Based on the present study, the prevalence of anaemia has increased, especially among girls. This could be due to the fact that the Weekly Iron-Folic Acid Supplementation (WIFS) programme is still in its early stages and has reported poor coverage and compliance(Reference Shyam, Roshita and Rah44). Additionally, during the pandemic, the WIFS programme in Indonesia was replaced with online education about anaemia(Reference Soewondo, Sakti and Irawati45), which may not have been as effective. Whereas our analysis showed that Hb concentration was inversely related to depression scores in bivariate analysis, this association is found for boys but not for girls in longitudinal analysis. This is consistent with findings from a cohort study of 2920 Dutch individuals aged 18–65 years, which also found no independent link between Hb concentration and depressive or anxiety disorders(Reference Lever-van Milligen, Vogelzangs and Smit46). However, past research has demonstrated that lower Hb levels can be associated with increased depressive symptoms(Reference Den Elzen, Willems and Westendorp47–Reference Zarate-Ortiz, Verhoef and Melse-Boonstra49). Studies conducted among high-risk populations, such as elderly(Reference Onder, Penninx and Cesari50) and individuals with CVD(Reference Steptoe, Wikman and Molloy48), have reported inverse relationships. This may be attributed to underlying factors such as poorer physical health, low Fe or vitamin B12 status, decreased brain oxygen levels or inflammation(Reference Vogelzangs, Beekman and De Jonge51–Reference Weiskopf, Feiner and Hopf53). Discrepancies in findings may arise from differences between study populations, such as age, sex and overall health status, and differences in contextual drivers of anaemia and depression.
This study represents the first longitudinal study into the relationship between food security, nutritional factors and mental health among a representative sample of adolescents from Gunungkidul district, Yogyakarta, Indonesia, during the COVID-19 pandemic. The longitudinal design of this study not only reveals changes over time but also uncovers cause-and-effect relationships. However, limitations include potential challenges in generalising findings due to the dynamic nature of the pandemic’s impact on socio-economic factors, as well as the reliance on self-reported data and the lack of some variables such iron folic supplementation and heme-iron consumption, which may introduce bias and limit causal inference. Furthermore, it is important to note that differences in study populations and methodologies, including sampling techniques, measurement tools, data collection and data analysis, may contribute to discrepancies in results with other studies.
In conclusion, we found that food insecurity is associated with depression, whereas better nutritional status is inversely associated with depression among Indonesian adolescents during the COVID-19 pandemic. While our findings align with several previous studies, disparities exist, emphasising the need for continued research to explore the interactions between food security, nutritional factors and mental health among adolescents.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524003027
Acknowledgements
The authors would like to thank Yoga Prajanta from the Centre for Health Policy and Management, Universitas Gadjah Mada, for his support in the data collection, as well as all data collectors, adolescents and parents who participated in the study.
This work is funded through the Innovative Methods and Metrics for Agriculture and Nutrition Action (IMMANA) programme, led by the London School of Hygiene & Tropical Medicine (LSHTM). IMMANA is co-funded with UK Aid from the UK government and by the Bill & Melinda Gates Foundation INV-002962/OPP1211308.
All authors had an essential role in formulation of the research questions; M. A. wrote the first draft of the paper and analysed the data; all authors were involved in interpretation of the data and revision of the manuscript. All authors have read and approved the final paper.
All authors stated no conflict of interest.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the ethical committee of the Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada. The first ethical approval was granted in 2020 (Letter number: KE/FK/0039/EC/2020), but due to COVID-19 pandemic the study was postponed to 2021 with granted ethical approval in 2021 (Letter number: KE/FK/0009/EC/2021). The study also received written permission to be conducted from the local District Level Office (Letter number: 070/00189) and the District Health Office. Before conducting the interviews, all participants and their parents/guardians were given an information sheet and consent form to be signed.









