CHD is one of the leading causes of death in the world(Reference Lozano, Naghavi and Foreman1). Several dietary factors have been associated with risk of CHD. High intake of saturated fats (SFA), especially when replacing polyunsaturated fat (PUFA), has been associated with higher risk of CHD(Reference Jakobsen, O’Reilly and Heitmann2,Reference Mozaffarian, Micha and Wallace3) , whereas higher intakes of, for example, whole grains, fruits and vegetables and fish(Reference Bechthold, Boeing and Schwedhelm4) have been associated with lower risk of CHD. One of the most effective ways of improving CHD risk factors is through the modulation of diet(Reference Mente, de Koning and Shannon5).
Dietary scores are used to measure the cumulative effects and interactions between several food items and nutrients and estimate the healthiness of the whole diet(Reference Waijers, Feskens and Ocké6). The Mediterranean diet is one example of a diet with beneficial health outcomes but due to different cultural and geographical factors, adherence to it is relatively poor in Nordic countries(Reference Sofi, Abbate and Gensini7). The Baltic Sea Diet Score was developed to characterise a healthy diet based on typical Nordic foods consumed in Finland and is characterised by high consumption of berries and fruits, whole grains, vegetables, rapeseed oil, fish, low-fat dairy and low consumption of processed meat and alcohol(Reference Kanerva, Kaartinen and Schwab8).
In previous studies, higher adherence to Baltic Sea Diet Score has been beneficially associated with cardiometabolic risk factors(Reference Kanerva, Kaartinen and Rissanen9) and other positive health outcomes and risk factors, such as lower risk of abdominal obesity(Reference Kanerva, Kaartinen and Schwab10), better physical capacity in old age(Reference Perälä, von Bonsdorff and Männistö11) and lower risk of elevated serum C-reactive protein (CRP) concentration(Reference Kanerva, Loo and Eriksson12).
There is still a limited number of studies with the Baltic Sea Diet Score, but other comparable healthy Nordic diet scores have also observed beneficial associations between healthy Nordic diet and CHD risk factors, such as hypertension and weight gain(Reference Poulsen, Crone and Astrup13), lower risk of type 2 diabetes(Reference Lacoppidan, Kyrø and Loft14), improved lipid profile in hypercholesterolaemic subjects(Reference Adamsson, Reumark and Fredriksson15) and decreased inflammation risk(Reference Uusitupa, Hermansen and Savolainen16). High adherence to healthy Nordic diet has also been associated with lower total mortality(Reference Olsen, Egeberg and Halkjær17–Reference Warensjö Lemming, Byberg and Wolk19) and lower risk of diseases, such as colorectal cancer(Reference Kyrø, Skeie and Loft20) and stroke(Reference Hansen, Overvad and Kyrø21). Only few studies have investigated associations with incident CHD risk, with mixed findings(Reference Gunge, Andersen and Kyrø22,Reference Galbete, Kröger and Jannasch23) .
Because of the limited number of studies, our aim was to examine the association between healthy Nordic diet, based on a modified Baltic Sea Diet Score, and risk of CHD in the Kuopio Ischaemic Heart Disease Risk Factor Study (KIHD), a population of middle-aged and older men from eastern Finland. We have previously reported that a low adherence to a healthy Nordic diet was associated with a higher risk of CVD death in the present study population(Reference Tertsunen, Hantunen and Tuomainen24). We additionally investigated the associations with risk factors of CHD, including blood pressure, serum lipid profile and serum CRP. We also examined the associations with carotid atherosclerosis in a subgroup for whom common carotid artery (CCA) intima–media thickness (IMT) measurements were available. To our knowledge, the association between healthy Nordic diet and carotid atherosclerosis has not been previously reported.
Materials and methods
Study population
The KIHD was designed to investigate risk factors for CVD, atherosclerosis and related outcomes in a prospective, population-based sample of men from eastern Finland(Reference Salonen25). The baseline examinations were carried out in 1984–1989. A total of 2682 men (83 % of those eligible) who were 42, 48, 54 or 60 years old at baseline were recruited. The baseline characteristics of the entire study population have been described elsewhere(Reference Salonen, Salonen and Seppänen26). Subjects with history of CHD (n 677) at baseline or with missing data on dietary intakes (n 24) were excluded, leaving 1981 men for the current analyses. Data on CCA–IMT measurements were available for 1053 participants, and complete data on serum CRP, LDL-cholesterol and HDL-cholesterol and TAG concentrations and systolic and diastolic blood pressure for 1889 participants.
Ethical approval
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Research Ethics Committee of the University of Kuopio. Written informed consent was obtained from all subjects.
Assessment of dietary intakes
Consumption of foods at baseline was assessed with an instructed food recording of 4 d, of which one was a weekend day. Household measures and a picture book of common foods and dishes were used to help in estimation of portion sizes. The picture book contained 126 most common foods and drinks consumed in Finland during the 1980s, and for each food item the participant could choose from 3 to 5 commonly used portion sizes or describe the portion size in relation to those in the book(Reference Haapa, Toponen and Pietinen27). In order to further improve accuracy, instructions were given and completed food records were checked by a nutritionist together with the participant. Dietary intakes were calculated using the NUTRICA® 2.5 software (Social Insurance Institution) that includes nutrient content data for over 1100 foods, drinks and dishes. The databank of the software was mainly based on Finnish values of nutrient composition of foods. The dietary intakes represent total consumption, including foods in mixed dishes and recipes. Whole grain was defined as the whole kernel of grain or cereal, according to the HEALTHGRAIN definition(Reference Van der Kamp, Poutanen and Seal28).
Healthy Nordic diet score
The original Baltic Sea Diet Score consists of nine components, of which six are food groups and three represent nutrients(Reference Kanerva, Kaartinen and Schwab8). The food items have been selected based on the traditional food culture in Finland. However, due to the lack of information on certain food items in our data used for the current analyses, the contents in the score components in our study are not identical to the original Baltic Sea Diet Score. Our data do not include information on the intake of individual fruits, vegetables or grains, so we instead used broader intake categories. For example, one of the components in the original score was ‘Rye, oats and barley’. In our score, the component ‘whole grains’ was used that includes also whole-grain wheat products, in addition to rye, oats and barley. The original Baltic Sea Diet Score components and those used in the current study are presented in online Supplementary Table S1. The score used in our analyses includes all fruits and berries, roots, pulses and vegetables, whole grains excluding rice and pasta, fat-free milk and milk <2 % fat, salmon and freshwater fish, processed and unprocessed red meat, total fat as a percentage of total energy intake, ratio of PUFA to SFA and trans-fatty acids and ethanol. The score was calculated according to quartiles of consumption for each score component(Reference Kanerva, Kaartinen and Schwab8). For the positive score components, the lowest quartile was given 0 points, the second one 1 point, the third one 2 points and the highest quartile of intake 3 points. For the negative score components, points were given in reverse order, except for alcohol, which was given 0–1 point (one point was given if the ethanol intake was < 20 g/d, otherwise zero points were given). The points given for each component were summed up to obtain the overall score. The resulting score ranged from 0 to 25. The higher the score, the higher the adherence to a healthy Nordic diet. In the analysis, the score was categorised into quartiles. The lowest quartile included scores <10, the two middle quartiles included scores 10–12 and 13–14 and the highest quartile included scores >14.
Health examination and measurements
Venous blood samples were collected between 08.00 and 10.00 hours at the baseline examinations. Subjects were instructed to abstain from ingesting alcohol for 3 d and from smoking and eating for 12 h prior to giving the sample. Detailed descriptions of the determination of serum lipids and lipoproteins(Reference Salonen, Nyyssönen and Korpela29), assessment of medical history and medications at baseline(Reference Salonen, Nyyssönen and Korpela29), family history of diseases(Reference Salonen, Nyyssönen and Korpela29), smoking(Reference Salonen, Nyyssönen and Korpela29) and physical activity(Reference Lakka, Venäläinen and Rauramaa30) have been published. The main lipoprotein fractions (VLDL, LDL and HDL) were separated weekly from unfrozen serum samples by ultracentrifugation and precipitation. The cholesterol content of all lipoprotein fractions was measured enzymatically by the cholesterol oxidase/peroxidaseamidopyrine method (Boehringer Mannheim). Average alcohol intake over the past 12 months (g/week) was assessed with a structured quantity-frequency method using the Nordic-Alcohol Consumption Inventory for drinking behaviour(Reference Kauhanen, Julkunen and Salonen31). Physical activity was assessed using the KIHD 12-month leisure-time physical activity history, which covers in detail the most common physical activities of middle-aged Finnish men and enables the assessment of all components of physical activity, including energy expenditure, duration, frequency and mean intensity. Hypertension was defined as blood pressure over 140/90 mmHg or medical treatment for hypertension. Resting blood pressure was measured six times with a random-zero mercury sphygmomanometer: three times in a supine position after a rest of 5 min before each measurement, one time in a standing position after a standing rest of 1 min and two times in a sitting position after 5-min rest before both measurements. The mean of each respective six values was used in the present analyses as the systolic and diastolic blood pressure. Serum CRP was measured with an immunometric assay (Immulite High Sensitivity CRP Assay, DPC) using clinical chemistry analyser Kone Specific (KONE Instruments Oy). BMI was computed as the ratio of weight in kilograms to the square of height in metres. Information on the medication use during the follow-up was obtained from the national Drug Prescription Registry at the Social Insurance Institute. Education and income were assessed by self-administered questionnaires.
Assessment of carotid atherosclerosis
The extent and severity of carotid atherosclerosis were assessed by high-resolution B-mode ultrasonographic examination of the right and left CCA in a 1·0–1·5-cm section at the distal end of the CCA, proximal to the carotid bulb, as described earlier(Reference Salonen, Seppänen and Lakka32). Ultrasonographic examinations were conducted by one physician. All examinations were performed with the subject in a supine position. IMT, calculated as the mean distance between the intima–lumen and media–adventitia interfaces, was estimated at approximately 100 points in both the right and left CCA. For the present study, two measures of IMT were used: (1) the mean IMT, calculated as the mean of all IMT estimates from the right and left CCA and considered an overall measure of the atherosclerotic process and (2) the maximal IMT, the average of the points of maximal thickness from the right and left CCA and indicative of the depth of intrusion of IMT into the lumen in this part of the CCA.
Ascertainment of follow-up events
Data on fatal and non-fatal CHD events from the beginning of the study in 27 March 1984 to the end of the follow-up in 31 December 2014 were obtained by computer linkage to the national hospital discharge and death certificate registers. Diagnostic information was collected from hospitals and classified using identical diagnostic criteria. Each suspected coronary event (ICD-9 codes 410–414 and ICD-10 codes I20–I25) was classified into (1) a definite acute myocardial infarction, (2) a probable acute myocardial infarction, (3) a typical acute chest pain episode of more than 20 min indicating CHD, (4) an ischaemic cardiac arrest with successful resuscitation or (5) no acute coronary event by a physician using the original patient records. The first four events were used as a diagnosis of CHD. Acute coronary events that did not lead to death during the following 24 h were considered as a non-fatal event. If a subject had multiple non-fatal CHD events during the follow-up or a non-fatal event followed by a fatal event, the first was considered the end point.
Statistical analysis
The univariate relationships of the healthy Nordic diet score with baseline characteristics were assessed by means and linear regression (for continuous variables) or χ 2 tests (for categorical variables). Associations with CHD risk factors and carotid atherosclerosis were analysed with ANCOVA and linear regression. Cox proportional hazards regression models were used to estimate hazard ratios of incident CHD events in quartiles of the score. Due to the low range of values in the score, the number of participants in each quartile is not even. The validity of the proportional hazards assumption was confirmed using Schoenfeld residuals. Possible multicollinearity was checked using variance inflation factors, which all were under 2, indicating no multicollinearity. The analyses were adjusted for relevant covariates, based on established risk factors for CHD and our previous investigation of the association between a healthy Nordic diet score and mortality risk(Reference Tertsunen, Hantunen and Tuomainen24): The model 1 included age (years), examination year and energy intake (kcal/d). The multivariable model 2 included variables in the model 1 and pack-years of smoking, leisure-time physical activity (kcal/d), education (years), marital status (yes/no), income (euros/year) and use of medications (hypercholesterolaemia and hypertension medication and aspirin). The model 3 included possible mediators for the association, BMI (kg/m2) and history of diabetes (yes/no). All quantitative variables were entered in the models as continuous variables. In the analyses of carotid atherosclerosis also the technical covariate focusing depth was included. Cohort mean was used to replace missing values in covariates (<2·7 %). Tests of linear trend were conducted by assigning the median values for each category of exposure variable and treating those as a single continuous variable. All P-values were two-tailed (α = 0·05). Data were analysed using SPSS 25.0 for Windows (IBM Corp.) The post hoc power calculations were done using the Post-hoc Power Calculator at https://clincalc.com/stats/Power.aspx and comparing the extreme quartiles of the healthy Nordic diet score. According to the calculations, we had 46 % power in the analyses with total CHD events and 66 % power in the analyses with fatal CHD events, from 13 (maximal CCA-IMT) to 17 % (mean CCA-IMT) power in the analyses with carotid atherosclerosis and from 14 % (systolic blood pressure) to 93 % (LDL-cholesterol) power in the analyses with the CHD risk factors.
Results
Baseline characteristics of the study population
The baseline characteristics for the 1981 participants are presented in Table 1. Participants who had higher adherence to healthy Nordic diet had higher leisure-time physical activity, education and income and lower total cholesterol levels and alcohol intake and they were less often smokers and were more likely married compared to the participants with lower adherence to healthy Nordic diet.
Table 1 Baseline characteristics of the 1981 participants according to quartiles of the healthy Nordic diet score
(Mean values and standard deviations)
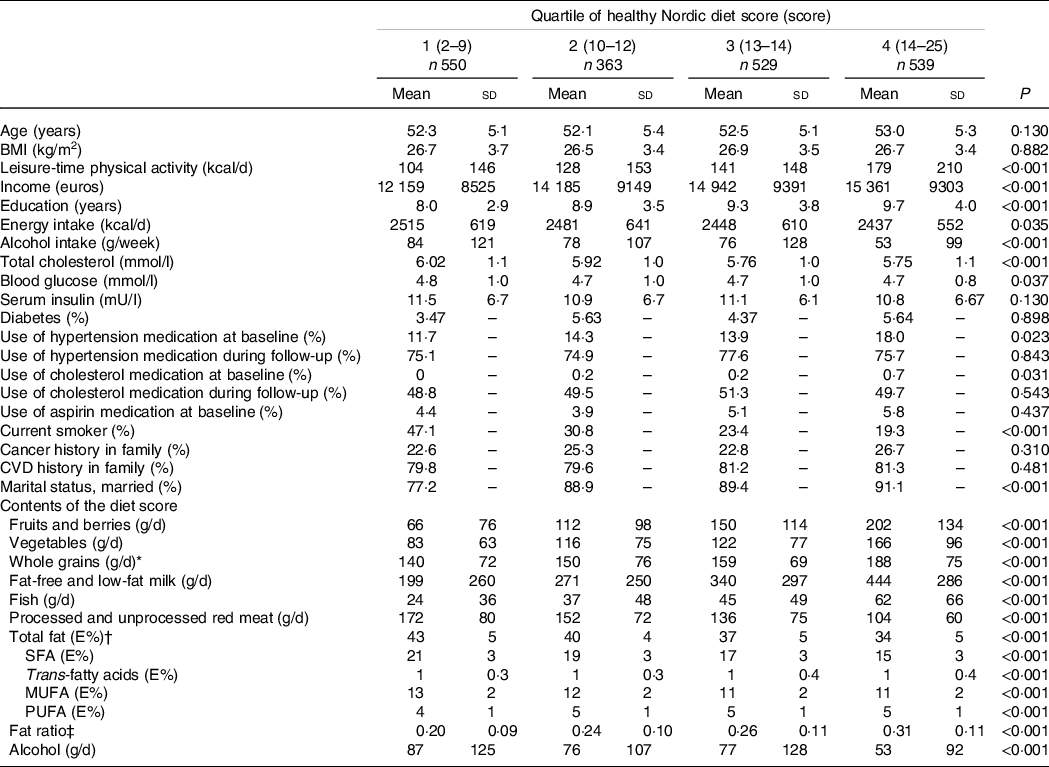
* Excluding rice and pasta.
† Percentage of energy.
‡ The ratio of PUFA to SFA and trans-fatty acids.
Risk factors
When we examined the associations with major CHD risk factors, in the model 1 adjusted for age, examination year and energy intake, lower adherence to healthy Nordic diet was associated with higher serum CRP and LDL-cholesterol concentrations (Table 2). After further adjustment for potential confounders (model 2), only the association with CRP remained statistically significant (extreme-quartile difference 0·66 mg/l, 95 % CI 0·11, 1·21 mg/l), with little change after further adjustment for BMI and diabetes (model 3).
Table 2 Risk factors of CHD in quartiles of the healthy Nordic diet score
(Hazard ratios and 95 % confidence intervals)

* Model 1 is adjusted for age (years), examination year and energy intake (kcal/d).
† Model 2 is adjusted for model 1 plus smoking (never smoker, previous smoker, current smoker <20 cigarettes/d and current smoker ≥ 20 cigarettes/d), leisure-time physical activity (kcal/d), education (years), marital status (married v. other), income (euros/year) and medications (hypercholesterolaemia and hypertension medication and aspirin).
‡ Model 3 is adjusted for model 2 plus BMI (kg/m2) and diabetes (yes/no).
Carotid atherosclerotic and healthy Nordic diet
We did not find evidence for an association between healthy Nordic Diet and carotid atherosclerosis in the basic model (model 1) or after adjustment for potential confounders (model 2) or mediators (model 3) (Table 3).
Table 3 Carotid atherosclerosis in quartiles of the healthy Nordic diet score
(Hazard ratios and 95 % confidence intervals)
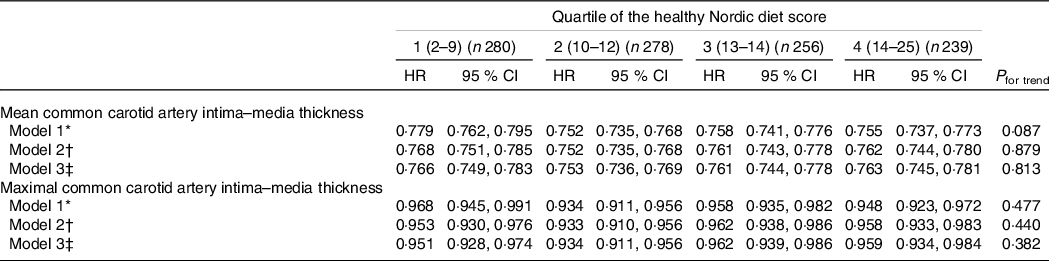
* Model 1 is adjusted for age (years), examination year and energy intake (kcal/d).
† Model 2 is adjusted for model 1 plus smoking (never smoker, previous smoker, current smoker < 20 cigarettes/d and current smoker ≥ 20 cigarettes/d), leisure-time physical activity (kcal/d), education (years), marital status (married v. other), income (euros/year) and medications (hypercholesterolaemia and hypertension medication and aspirin).
‡ Model 3 is adjusted for model 2 plus BMI (kg/m2) and diabetes (yes/no).
Risk of incident CHD
During the average follow-up of 21·6 years (sd 8·3 years), 407 men (20·5 %) experienced a CHD event. Of these, 277 were fatal events. In the model 1, those in the lowest v. the highest quartile of the healthy Nordic diet score had 38 % (95 % CI = 7%, 79 %) higher risk of fatal or non-fatal CHD event (P trend across quartiles 0·014) and 73 % (95 % CI = 22%, 147 %, P trend = 0·004) higher risk of CHD death (Table 4). Further adjustment for potential confounders (model 2) significantly weakened the associations and they were not statistically significant anymore (model 2, Table 4). Adjustment for potential mediators slightly attenuated the association further (model 3).
Table 4 Risk of CHD in quartiles of the healthy Nordic diet score
(Hazard ratios and 95 % confidence intervals)
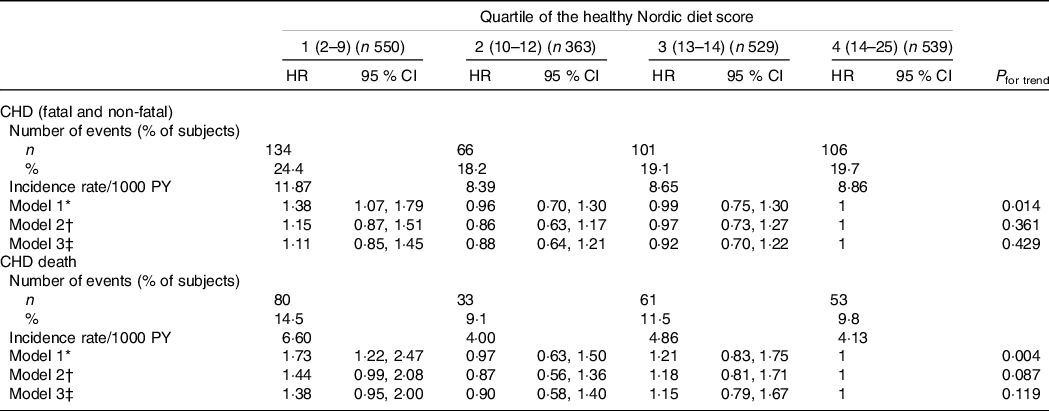
PY, person-years.
* Model 1 is adjusted for age (years), examination year and energy intake (kcal/d).
† Model 2 is adjusted for model 1 plus smoking (never smoker, previous smoker, current smoker < 20 cigarettes/d and current smoker ≥ 20 cigarettes/d), leisure-time physical activity (kcal/d), education (years), marital status (married v. other), income (euros/year) and medications (hypercholesterolaemia and hypertension medication and aspirin).
‡ Model 3 is adjusted for model 2 plus BMI (kg/m2) and diabetes (yes/no).
To evaluate if the long follow-up time attenuated the associations, we examined the associations with shorter follow-up time (mean follow-up 11 years, 191 any CHD events and seventy fatal CHD events). There was no statistically significant association with the risk in these analyses, either. The hazard ratio for the lowest v. the highest quartile was 0·96 (95 % CI 0·63, 1·45, P trend = 0·845) for any CHD and 1·15 (95 % CI 0·58, 2·28, P trend = 0·502) for CHD death (model 2).
Sensitivity analyses
In the analyses with participants with complete data on all covariates (1895 participants, 396 total CHD events and 222 fatal CHD events), the associations were not appreciable different. For example, for total CHD in the lowest v. the highest healthy Nordic diet quartile the hazard ratio was 1·09 (95 % CI 0·83, 1·44, P trend = 0·539, model 2) and for fatal CHD 1·41 (95 % CI 0·97, 2·05, P trend = 0·113). There were no appreciable differences in the analyses with the CHD risk factors or with carotid atherosclerosis, either (data not shown). Finally, because the participants filled the food records throughout the year, differences in the seasonal availability of certain food items, such as fruits and berries, could affect reporting. However, adjusting for the month of diet recording had no appreciable impact on the associations (data not shown).
Discussion
In this population-based cohort study among middle-aged and older men from eastern Finland, we did not find evidence that higher adherence to healthy Nordic diet would associate with risk of CHD, carotid atherosclerosis or with CHD risk factors, except for an inverse association with serum CRP concentration.
To our knowledge, there are only few studies that have reported on the association between healthy Nordic diet and risk of developing CHD. In EPIC-POTSDAM from Germany that included participants aged 35–65 years, there was an inverse but statistically non-significant association with incidence of myocardial infarction with higher adherence to healthy Nordic diet(Reference Galbete, Kröger and Jannasch23). In the Danish Diet, Cancer and Health cohort study with participants aged 50–64 years, higher adherence to healthy Nordic diet was associated with lower risk of myocardial infarction(Reference Gunge, Andersen and Kyrø22). The partial explanation for the lack of association in our study may be differences in the diet scores and research settings. Both of these studies had a much larger number of participants and events that increases the power to find associations. Both studies also included women, although neither study found evidence that sex would modify the associations with risk of myocardial infarction. These studies also used self-administered semiquantitative FFQ to collect information about diet, instead of the 4-d food recording used in our study. Food recording is considered a gold standard in epidemiological studies to assess dietary intakes because it does not rely on memory, and the other assessment methods are often validated against dietary intakes assessed with food recording. Validated FFQ or repeated 24-h diet recalls can therefore provide useful information on long-term diet patterns and composition of diet, and they are more common in epidemiological studies than food records due to, for example, lower costs and lower burden for participants. The single 4-d food recording used in our study may be too short a time to assess habitual long-term dietary intakes. Four days may also not be enough to accurately capture intakes of foods that are commonly consumed only 1–2 times per week, such as fish, which potentially attenuates the associations. This has been observed in our previous study in the KIHD cohort, where higher serum long-chain n-3 PUFA concentration, an objective biomarker for fish intake, was associated with a lower risk of disease, but fish intake was not(Reference Virtanen, Mursu and Voutilainen33). In 1990, the average per capita fish intake in Finland was 18·9 kg/year(34). In men in the KIHD cohort, the average daily fish intake is about 46 g, or about 16·8 kg/year. Because the national average includes both men and women, this indeed suggests that the average fish intake estimated with the 4-d food recording in the KIHD cohort may be underestimated.
In our study, we also examined the associations of healthy Nordic diet with risk factors of CHD. Our finding of an inverse association with serum CRP concentration agrees with a meta-analysis of observational studies, which found that Baltic Sea Diet Score was associated with lower high-sensitive CRP concentration in both men and women(Reference Kanerva, Kaartinen and Rissanen9). A similar association has been observed in some(Reference Kanerva, Loo and Eriksson12) but not all observational studies that have investigated the association with inflammation markers(Reference Sakhaei, Ramezani-Jolfaie and Mohammadi35) using other healthy Nordic diet scores. The meta-analysis also found that adherence to Baltic Sea Diet Score was associated with higher risk of lowered HDL-cholesterol among women(Reference Kanerva, Kaartinen and Rissanen9). In experimental studies, higher adherence to healthy Nordic diet has had a beneficial effect on cardiometabolic risk factors, such as hypertension and weight gain(Reference Poulsen, Crone and Astrup13), blood pressure(Reference Ndanuko, Tapsell and Charlton36), inflammation profile(Reference Uusitupa, Hermansen and Savolainen16) and serum lipids in hypercholesterolaemic subjects(Reference Adamsson, Reumark and Fredriksson15).
The composition of the different scores that are used to describe healthy Nordic diet may have an impact on the findings. Ideally, the score would include only dietary factors that have an impact on disease risk. Such a score would potentially produce larger and more easily detectable effects on disease risk than its individual components alone. There are several different healthy Nordic diet scores based on the typical foods consumed in the Nordic countries. We modelled the healthy Nordic diet score according to the original Baltic Sea Diet Score from Finland(Reference Kanerva, Kaartinen and Schwab8) but due to lack of information on some individual food items we included some differences (online Supplemental Table S1). The creation of the Baltic Sea Diet Score was based on typical Nordic foods, such as Nordic fruits and berries, rapeseed oil, rye, salmon and dairy products that were considered health promoting and therefore could potentially reduce disease(Reference Bere and Brug37,Reference Adamsson, Reumark and Cederholm38) . Randomised trials had also found evidence that diets containing these foods had improved cardiovascular risk factors(Reference Adamsson, Reumark and Fredriksson15,Reference Uusitupa, Hermansen and Savolainen16) , providing support for their inclusion in the score. However, some scores also include food items that do not exist in other scores, such as shellfish in the Danish Healthy Nordic Food Index(Reference Olsen, Egeberg and Halkjær17) or meal frequency and water consumption in the Norwegian New Nordic Diet Score(Reference Hillesund, Bere and Haugen39) or dietary fat quality in the original Baltic Sea Diet Score(Reference Kanerva, Kaartinen and Schwab8) and in our modified score (online Supplementary Table S2). Therefore, the findings from different studies may not be comparable. The subjective decisions and reasoning regarding the potential score components, availability of data on different dietary components, and balance and weight of the components that are chosen to be part of the score have an impact on how well the score describes a healthy Nordic diet and its impact on disease risk. One explanation for our mostly null findings may be that the score may include components that do not have an association with disease risk in a certain study population, which then attenuates the associations observed with the composite score. For example, higher PUFA intake has been associated with a lower risk of CHD death in the KIHD cohort, whereas total fat intake was not associated with the risk(Reference Virtanen, Mursu and Tuomainen40). The score would also not be useful if there is only little variation in the intakes of the components within the population. However, in the present study there were marked differences in the intakes of the score components (Table 1).
The strengths of the present study include the prospective population-based cohort setting, no loss to follow-up and extensive information about possible confounding factors. The most notable limitation of our study is that the dietary intakes were assessed only once at the baseline in 1984–1989, which may not accurately describe the dietary intakes during the long follow-up. This is a potential source of random error, which would attenuate the true associations. However, we did not find evidence that adherence to healthy Nordic diet would be associated with most CHD risk factors or with carotid atherosclerosis in the cross-sectional analyses at baseline or with incident CHD events during the shorter follow-up time, which supports the lack of an association with the risk of incident events during the long follow-up. It has also been argued that self-reported dietary assessment methods would provide physiologically implausible data (e.g.(Reference Archer, Marlow and Lavie41)). However, although self-reported methods, such as diet records, may not provide accurate information on absolute intakes of foods and nutrients, they are validated and established tools for assessing diet quality and composition, which are the main interests in nutritional epidemiological research(Reference Martín-Calvo and Martínez-González42,Reference Subar, Freedman and Tooze43) . Finally, because our study population included only men, the results of the present study cannot necessarily be generalised to women.
In conclusion, we did not find evidence for statistically significant associations between adherence to a Healthy Nordic diet and risk of CHD, or with carotid atherosclerosis, serum lipids or blood pressure. Better adherence to healthy Nordic diet was associated only with lower serum CRP concentration. More studies are needed to examine the impact of healthy Nordic diet on cardiovascular health.
Acknowledgements
The present study was funded by a personal grant from Juho Vainio Foundation to H.-M. Tertsunen. Juho Vainio Foundation had no role in the design, analysis or writing of this article.
The authors’ responsibilities were as follows – H.-M. T.: analysed the data and drafted the manuscript; J. K. V.: analysed the data and had primary responsibility for final content; S. H., J. T. S., T.-P. T. and J. K. V.: acquired data, designed and conducted research; S. H., J. T. S., T. P. T. and J. K. V.: critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
There are no conflicts of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521001227







