Observational data suggest an association between increased whole grain consumption and decreased morbidity and mortality(Reference Jacobs, Slavin and Marquart1–Reference Steffen, Jacobs and Stevens4). While there is an increased drive from health professionals and some cereal-based food manufacturers for increased whole grain consumption at a population level(Reference Mancino, Kuchler and Leibtag5), data show that the vast majority of people in the USA(Reference Good, Holschuh and Albertson6) and Denmark(Reference Kyrø, Skeie and Dragsted7) do not habitually consume the levels of whole-grain foods recommended by the US Department of Agriculture(8) or the Danish National Food Institute Technical University of Denmark(9). Similar, or low, intake levels are reported for the UK population(Reference Thane, Jones and Stephen10), although there are no prescriptive guidelines in the UK currently.
Previous studies(Reference Bradbury, Thomason and Jepson11–Reference Wrieden, Anderson and Longbottom13) have suggested that dietary intervention strategies can result in long-term improvements in dietary intake, in some cases with parallel improvements in health(Reference Esposito, Marfella and Ciotola14–Reference Shai, Schwarzfuchs and Henkin16) or reduced subsequent disease onset(Reference Lindstrom, Ilanne-Parikka and Peltonen17, Reference Cook, Cutler and Obarzanek18). Success of such interventions may be improved by direct or indirect means of increasing exposure of individuals to specific foods/diets and continued counselling or follow-up. There are limited data demonstrating the impact of provision of foods within an intervention period on long-term dietary changes. In one previous report, it has been observed that 14 d exposure to a range of six vegetables significantly increased children's preference and intake of these vegetables 2 weeks post-intervention(Reference Wardle, Cooke and Gibson19), compared with either an information-only intervention or no intervention. Provision of free fruits for a school year to Norwegian children resulted in significant increases in fruit intake up to 3 years post-intervention(Reference Bere, Veierod and Bjelland20). We are not aware of similar data available in the literature related to dietary interventions with whole-grain foods. The WHOLEheart study was a randomised, controlled trial testing the impact of increased consumption of whole-grain foods (wholemeal breads, breakfast cereals, pasta, rice and snacks were made available to participants) on markers of CVD risk in infrequent whole-grain consumers over a 16-week period(Reference Brownlee, Moore and Chatfield21). In brief, participants were recruited to the present study based on age (18+ years), BMI in excess of 25 kg/m2 and low baseline whole grain consumption equivalent to less than 20 g whole grains/d. This intervention provided a unique opportunity to assess habit forming associated with the dietary intake of whole-grain foods by comparing the subsequent intake of whole-grain foods in a group of infrequent whole-grain consumers who had been provided and consumed whole-grain foods over a 16-week period, with a comparator control group (who had made no prior dietary changes).
The aim of the present study was to compare whole-grain food intake in individuals who had previously consumed whole-grain foods as part of a whole-grain food intervention with a control group who made no such dietary change 1 year post-intervention. As a secondary aim, we compared whether there were changes in total dietary intake between the two participant groups over this time period.
Methods
Participants
All participants gave written informed consent. The present study was conducted according to the guidelines laid down in the Declaration of Helsinki. The study was approved by the North Tyneside Local Research Ethics Committee (reference 05/Q0905/75) and by the Newcastle upon Tyne NHS Foundation Trust R&D Department. The study was registered with isrtcn.org (SRCT no. CCT-NAPN-A13175).
The dietary intervention (the WHOLEheart study) from which this sample was drawn recruited 266 overweight, but otherwise healthy, individuals who ate less than one serving of whole grains daily (a serving defined as 20 g whole grains). Participants were randomly allocated into three groups: a control group who were asked to make no dietary changes over the 16-week intervention period; intervention group 1 (provided with whole-grain foods, and asked to consume three servings/d over the 16-week period); intervention group 2 (provided with whole-grain foods, and asked to consume three 20 g servings/d for 8 weeks, followed by six servings of whole grains/d for the subsequent 8 weeks). Full details of participant recruitment and intervention design for the WHOLEheart study have been described elsewhere(Reference Brownlee, Moore and Chatfield21).
Upon completion of the intervention, participants were asked whether they would be willing to take part in further research activities. Between 48 and 49 % of control participants and 41 and 52 % of intervention participants provided FFQ data at the post-intervention time points.
Collection of dietary data
Positive respondents were sent FFQ to return by post at 1, 6 and 12 months post-intervention. The FFQ, which recorded food intake only during the previous 7 d, was the same as that used in the WHOLEheart intervention. The 149-item questionnaire was based on the UK European Prospective Investigation into Cancer and Nutrition FFQ, expanded to include inputs for both whole-grain foods provided for the study and other whole-grain foods available in the UK at the time of the study. Within the WHOLEheart intervention, nutrient intake determined from the FFQ was highly correlated with similar estimates from parallel food diaries(22).
Analysis of dietary data
Whole grain consumption was assessed from returned FFQ data, using estimates of portion size based on previously reported average male and female whole-grain food portion sizes(Reference Thane, Jones and Stephen10). Participants' nutrient profile for total dietary intake was estimated using National Diet and Nutrition Survey 2000–1(23) data on portion sizes, and estimates of the nutrient content of a range of food items (McCance & Widdowson(Reference McCance and Widdowson24) data). All data were collated within a custom-made dietary database (Microsoft Access; Microsoft Office).
Statistical analysis
Dietary intake of participants who received whole grains during the intervention (WG group) and those who did not (control group) were compared at each time point, separately and when aggregated across the whole 12 months by the two-sample Wilcoxon rank-sum test using the Stata version 10.1 software package (StataCorp LP). A P value of less than 0·05 was considered as statistically significant. For the purpose of the present analysis, post-intervention food intake data for WG groups 1 and 2 were combined to compare those who were provided with whole-grain foods during the intervention with those who did not.
Results
Return rates for FFQ were 55, 53 and 47 % at 1-, 6- and 12-month post-intervention time points, respectively (compared with >90 % return during the intervention). Data from the responders from each group are highlighted in Table 1. The mean post-intervention whole grain consumption over 12 months for each group is shown in Fig. 1. The demography of the respondents (52 % females, with a median BMI of 29·1 kg/m2 and a median age of 47 years) was very similar to that of all participants in the WHOLEheart intervention (50 % females, with a median BMI of 30·0 kg/m2 and a median age of 46 years).
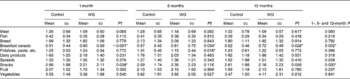
Table 1 Whole grain consumption in WHOLEheart volunteers 1, 6 and 12 months post-intervention* (Mean values and standard deviations; number of subjects and percentages)
WG, whole-grain intervention group.
* Approximately equal numbers of respondents came from the two WG in the original WHOLEheart study at each time point (intervention group 1 v. intervention group 2: 1 month, n 45 v. 42; 6 months, n 41 v. 45; 12 months, n 33 v. 35).

Fig. 1 Mean whole grain (WG) intake at baseline (pre-intervention) and post-intervention time points. □, Control group; ![]() , intervention group 1 (prescribed 60 g WG/d for 16 weeks); ■, intervention group 2 (prescribed 60 g WG/d for first 8 weeks of intervention, followed by 120 g WG/d for the following 8 weeks). n values at baseline are 94 (control), 76 (intervention group 1) and 80 (intervention group 2) at 1 month.
, intervention group 1 (prescribed 60 g WG/d for 16 weeks); ■, intervention group 2 (prescribed 60 g WG/d for first 8 weeks of intervention, followed by 120 g WG/d for the following 8 weeks). n values at baseline are 94 (control), 76 (intervention group 1) and 80 (intervention group 2) at 1 month.
The mean whole grain intake in the control group was between 16 and 19 g across the four measurement periods and did not change from pre-intervention levels (Table 1). In the control group, 14–15 % of the participants consumed no whole-grain foods at 1 and 6 months post-intervention; 25 % consumed no whole-grain foods at 12 months post-intervention. In contrast, only 3, 7 and 6 % of those from the WG group consumed no whole-grain foods at 1, 6 and 12 months post-intervention. Whole grain consumption was significantly higher in intervention group 1 and intervention group 2 participants throughout the post-intervention period compared with both the control group and baseline (P <0·001). However, whole grain consumption was not significantly different between the two intervention groups during the post-intervention period, so the data are combined in Table 1 for ease of comparison. There was a decrease in whole grain consumption for the WG group between 1 month and 12 months post-intervention, but this was not statistically significant, and at the end of the measurement period, this group of subjects was consuming approximately 50 % more whole grains than the control group.
Table 2 details the specific differences that occurred in terms of whole-grain food consumption during the intervention and over the 12-month post-intervention period. The WG group participants had a significantly higher intake of whole-grain breads and breakfast cereals compared with the control group at each of the three time points assessed over the 12-month post-intervention period. The consumption of whole-grain pasta and rice, as well as whole-grain snacks was significantly higher in the WG group at some time points post-intervention (1 and 6 months for pasta/rice and 12 months for whole-grain snacks).
Table 2 Daily frequency of consumption of whole-grain and non-whole-grain food products post-intervention (servings/d) (Mean values and standard deviations)

WG, whole-grain intervention group.
* P< 0·05; Wilcoxon rank-sum test.
† P value compares FFQ-reported frequencies of intake between the control and WG groups at each time point post-intervention.
The frequency of consumption of specific food groups by participants at each time point is shown in Table 3. Participation in the intervention arms of the WHOLEheart intervention resulted in a significantly higher daily frequency of breakfast cereal consumption (overall P= 0·002) at 1, 6 and 12 months post-intervention. The average increase in the daily frequency of breakfast cereal consumption was about 0·30 occasions/d compared with the values between 0·43 and 0·57 occasions/d seen during the intervention when whole-grain breakfast cereals were provided to the participants. Overall, across the 12-month follow-up period, the frequency of snack consumption was lower in those participants from the WG group compared with the control group (P= 0·020). Differences in the other food groups were small, with no consistent differences between the control and WG groups. Specifically, the frequency of bread consumption, which had been significantly higher in the WG group at the end of the 16-week intervention period, was not different between the WG and control groups throughout the post-intervention follow-up period. Daily energy intake was not different between the control and intervention group participants throughout the post-intervention period, and was comparable with measures of energy intake recorded at baseline and during the intervention itself (data not shown, P>0·350 at all time points). An increase in estimated dietary fibre intake seen during the intervention in those consuming whole-grain foods continued into the post-intervention period (P< 0·001 overall across 1, 6 and 12 months), although the differences were smaller and only significant at the 12-month time point (mean for control v. intervention groups: 16·5 (sd 5·3) v. 19·8 (sd 7·3) g/d, P= 0·004). Other differences between the control and WG groups seen during the intervention itself (reductions in the proportion of fat and corresponding increase in carbohydrate and increases in some micronutrients) were not consistently different during the follow-up.
Table 3 Reported mean daily frequency of food consumption 1, 6 and 12 months post-intervention (servings/d) (Mean values and standard deviations)
WG, whole-grain intervention group.
* P< 0·05; Wilcoxon rank-sum test.
† P value compares reported food frequency intake between the control and WG groups at each time point post-intervention.
Discussion
This follow-up evaluation suggests that a relatively short, direct dietary intervention with whole-grain foods can have a significant impact on long-term whole grain consumption in individuals who habitually consume low amounts of such foods. The WG group maintained a higher intake of whole grains (>10 g/d compared with the control group) over the 12-month period. It appears as though both an increased percentage of non-consumers of whole grains (at 6 and 12 months post-intervention) and a reduction in elective whole grain consumption cause a gradual reduction in whole grain consumption over time, but this was not statistically significant. This is consistent with evidence that repeated ‘exposure’ to foods that children spontaneously elect not to consume can increase subsequent, long-term dietary inclusion(Reference Birch and Wolfe25). Data from our control group suggest that habitual whole grain consumption is still much lower than that recommended in the USA or Denmark. A number of reasons have been suggested previously as to why individuals in the UK choose refined grain options as opposed to whole grains(Reference Smith, Kuznesof and Richardson26). However, only a small percentage of the participants withdrew from the WHOLEheart intervention period citing unwillingness to consume whole-grain foods as their reason for withdrawal. This suggests that taste acceptability of whole-grain products is possibly higher than the expected taste of these products once the participants had been exposed to them. Qualitative research undertaken with the WHOLEheart volunteers suggests that there are personal, product-related or situational factors that prevent habitual inclusion of whole-grain foods in the diet(Reference Kuznesof, Brownlee and Moore27).
The most striking effects on dietary habits were the significant increase in the frequency of breakfast cereal consumption at all post-intervention time points (see Table 3), and the significant increase in NSP intake in the WG group v. the control group when all time points were considered. Increased frequency of breakfast consumption has been linked to health benefits in population-based studies(Reference Keski-Rahkonen, Kaprio and Rissanen28, Reference Mota, Fidalgo and Silva29), emphasising the additional benefit of this change in dietary pattern. Otherwise, there was little impact on the frequency of consumption of other foods when compared with the intake of the control group.
The ‘gold standard’ for the estimation of dietary intake is through the use of food diaries(Reference Bingham, Cassidy and Cole30, Reference Bingham, Gill and Welch31). However, participants are often less compliant when filling out diaries due to the increased time burden and inconvenience involved(Reference Bingham, Cassidy and Cole30). As a result, the FFQ was the method of choice in the present study for dietary data collection, in order to improve return rate from as many participants as possible. As this was the methodology for collection used during the WHOLEheart intervention period, its use was familiar to participants and provided data directly comparable with previously collected data.
The average consumption of whole-grain foods across the 12-month post-intervention follow-up period, although not statistically significant, appeared to decline, suggesting a gradual removal of whole-grain foods from the diets of those from the WG group. The mean intakes observed fell short of intakes recommended in the USA of 48 g whole grains/d(8), and the more recent Danish recommendations of 75 g whole grains/d(9). However, the mean levels of whole grain consumption measured after 12 months post-intervention (over 36 g/d) are considerably higher than the most recent estimates of whole grain intake in adults both in the UK (median of 14 g/d from 2000–1 data(Reference Thane, Jones and Stephen10)) and the USA (mean values of approximately 11 g/d from 1999–2004 data(Reference O'Neil, Zanovec and Cho32)).
The length of the whole-grain food intervention within the present study was longer than any previous whole-grain intervention (4 months). As such, there is no indication from the present data whether a shorter intervention with whole-grain foods would also result in longer-term, elective whole grain consumption. Specific strategies within this intervention period, and perhaps the method of dietary intervention(Reference Rosen, Schmitz and Cohen33), may also increase the time and amplitude of post-intervention elective whole-grain food consumption. A range of further consumer studies are required to optimise the time, length, magnitude and mode of such interventions. Such studies in long-term, post-intervention dietary changes are not only important to the development of public health messages aimed at increasing the intake of whole grains or other foods, but may also allow for more effective food marketing strategies to further increase the chances of measurable public health benefits.
The participants in the present study were specifically chosen because of their low consumption of whole-grain foods at recruitment. They were provided with a range of whole-grain foods to include in their diet during the intervention period. However, subsequent increases in whole grain consumption (compared with baseline or the control group) represent an increase in the elective consumption of whole-grain foods by these participants. This increased intake was maintained over the course of a 12-month period. As such, dietary intervention with whole-grain foods may represent a strategy through which health professionals (e.g. through provision of sample whole-grain food packs to target groups) or food industry professionals (e.g. through promotions or free samples) could increase the intake of whole-grain food products in the general population. As suggested above, the increased whole grain consumption noted here would not result in the lowest whole-grain consumers reaching dietary guideline levels. However, it would bring such individuals closer to these goals, and aid them in maintaining a higher whole grain intake over a number of months.
Acknowledgements
The present study was supported by the UK Food Standards Agency (project N02036). The authors designed the study; I. A. B. and S. A. K. managed the participant data collection; I. A. B. analysed the dietary intake data. All authors were involved in the data interpretation and manuscript preparation. The authors report no conflicts of interest arising from the present research or its publication.






