The associations between red and processed meat consumption and heart disease incidence and mortality have been assessed in several studies and meta-analyses(Reference Micha, Michas and Mozaffarian1,Reference Abete, Romaguera and Vieira2) . Two meta-analyses on red meat consumption and risk of CHD or ischaemic heart disease (IHD) found no associations(Reference Micha, Michas and Mozaffarian1,Reference Abete, Romaguera and Vieira2) . However, two prospective studies published after the meta-analyses were performed found an 18–19 % increased risk for every consumption increment of 100 g/d(Reference Bernstein, Sun and Hu3,Reference Pan, Sun and Bernstein4) . A meta-analysis studying heart disease mortality and not just disease found that increments of 100 g/d in red meat consumption were associated with 24 % increased risk of cardiovascular mortality(Reference Abete, Romaguera and Vieira2).
A meta-analysis on processed meat consumption and cardiovascular events found that every 50 g/d increment in consumption was associated with 44 % increased risk of cardiovascular events(Reference Micha, Michas and Mozaffarian1). Another meta-analysis found that increments of 50 g/d in consumption of processed meat were associated with 24 % increased risk of cardiovascular mortality. However, this analysis did not find associations with IHD mortality(Reference Abete, Romaguera and Vieira2).
Confounding factors such as sex, age, smoking, physical activity and disease history are routinely included in analyses on associations between meat consumption and risk of heart disease. However, it has been suggested that other dietary factors including fruit, vegetable and fibre intake may influence these associations(Reference Fogelholm, Kanerva and Mannisto5). Therefore, other dietary factors should be considered when estimating the causal association between meat consumption and heart disease risk. Previous studies have accommodated for this confounding by adjusting analyses for other dietary factors. Yet, in order to understand the influence of other dietary factors on associations between meat consumption and heart disease risk, dietary confounding is better assessed when stratifying the association by other dietary factors. The present study will allow for the identification of different associations between meat consumption and heart disease in participants with a healthy diet compared to participants with an unhealthy diet. A study conducted in Sweden investigated if an association between red meat consumption and cardiovascular mortality differed between those with high and low consumption of fruit and vegetables. In the present study, the associations did not differ between those with high and low consumption of fruit and vegetables(Reference Bellavia, Stilling and Wolk6). Dietary quality is, however, composed of a range of factors beyond fruit and vegetable consumption, and detailed dietary information is required to estimate the dietary quality. In the present study, detailed information on a range of dietary factors was obtained from a cohort of more than 10 000 individuals and information on IHD was obtained from national health registers. Therefore, the aim of the present study was to assess whether meat consumption is associated with IHD, and subsequently assess if the association is modified by dietary quality.
Methods
The Danish National Survey on Diet and Physical Activity
The analyses were based on information from participants in Danish National Survey on Diet and Physical Activity 2000–2002, 2003–2008 and 2011–2013. The study sample was a random sample drawn from the Danish Civil Registration System and comprised of non-institutionalised Danish citizens. The response proportions in Danish National Survey on Diet and Physical Activity 2000–2002, 2003–2008 and 2011–2013 were 53·3, 53·3 and 54·4 %, respectively. Only participants aged 15–75 years at baseline were eligible for inclusion in the study (n 9848). In order to study incident disease, individuals were excluded if they had been diagnosed with IHD any time before baseline. The same strategy was applied for analyses on acute coronary syndrome (ACS). Thus, 8007 participants were included in analyses on IHD, and 8198 were included in analyses on ACS.
Information on food intake was obtained via self-administered, quantitative 7-d pre-coded food diaries. The data collection has previously been described(Reference Biltoft-Jensen, Matthiessen and Rasmussen7). The detailed dietary registration allowed for a subdivision into red and processed meat and for constructing a diet quality index based on the Danish dietary guidelines. Information on meat consumption, dietary quality, energy intake, alcohol energy intake, BMI (<18·5; 18·5–24·9; 25–29·9; ≥30 kg/m2), smoking (never, former, current) and leisure physical activity (none, light, moderate/hard) was extracted or generated from the surveys. Red meat was defined as unprocessed muscle tissue from mammals such as beef, veal, pork and lamb. In this population, red meat mainly consisted of beef, veal and pork. A small intake of unprocessed edible offal, for example, liver and heart, was included. The meat could be minced and/or frozen. Processed meat was defined as red meat or poultry that undergo a transformation and contain approved ingredients and may be subject to some form of preservation including smoking, drying, curing or fermentation.
To assess the dietary quality, the diet of each participant was given a dietary quality score(Reference Tetens, Andersen and Astrup8,Reference Knudsen, Fagt and Trolle9) . This was based on how well their diet complied with five of the official Danish dietary guidelines on fruit and vegetables, fish, whole grain, SFA and added sugars. For each dietary guideline, a score between 0 and 1 was given by dividing the dietary content of the actual component with the recommended dietary content. For example, the recommended intake of fruit and vegetables is 600 g/d. Thus, if a participant ate 200 g of fruit and vegetables per day, the score was 200/600 = 0·33. For SFA and added sugars, the scores were reverse. For example, for a participant with an energy intake of 15E% from SFA where the recommendation is <10E%, the score was 1–(15–9·999)/9·999) = 0·50. Scores >1 were truncated at 1 and scores < 0 were truncated at 0. The scores were added to yield the total score between 0 and 5. For those participants who had answered more than one survey (eighty-nine persons), information from their first survey was included.
Register-based information
Events of IHD and ACS were identified through linkage with information from registers using the unique personal identification number(Reference Pedersen10). The outcome IHD was based on information from the National Patient Register(Reference Lynge, Sandegaard and Rebolj11) on primary and secondary diagnoses and from the Register of Causes of Death(Reference Helweg-Larsen12) on underlying cause of death (ICD-8: 410–414; ICD-10: I20–I25). Information on ACS was also based on information from the National Patient Register on primary and secondary diagnoses and from the Register of Causes of Death on underlying cause of death (ICD-8: 410 and 427.27; ICD-10: I20.0 and I21).
Information on age, sex, ethnicity (Danish, Western non-Danish, non-Western) and emigration was obtained from the Danish Civil Registration System(Reference Pedersen10). Educational attainment was based on information from the Population’s Educational Register(Reference Jensen and Rasmussen13) and classified into short (primary school), medium (high school or vocational school) and long education (higher education). Information on diabetes up to 10 years before baseline was obtained from the National Patient Register (ICD-8: 249–250; ICD-10: E10–E14).
Analyses
The cohort was followed from baseline (date of survey interview) or from age 37 whichever came last. Delayed entry into the analyses was applied because the outcomes were almost absent among participants younger than 37 years. Follow-up ended at first diagnosis or death due to the studied outcome or at emigration, death or end of follow-up (31 December 2017), whichever came first.
Missing information on country of origin (0·01 %) was imputed as Danish origin, missing educational level (1·5 %) was imputed as short education, missing BMI (1·0 %) was imputed as normal BMI (18·5–24·9), missing smoking status (1·1 %) was imputed as never smoker and missing information on physical activity (0·4 %) was imputed as moderate/hard. Apart from educational level, these imputed values were chosen as they were the most prevalent among the non-missing values. For educational level, short education was chosen, because missing information on this is more common among persons with short education(Reference Jensen and Rasmussen13).
Associations between meat consumption and outcomes
The categorisations of meat consumption were based on the observed quartiles. For analyses of IHD, the measures of meat consumption were categorised in three groups (lower quartile, the two middle quartiles, upper quartile). Due to the small number of cases with ACS, the measures of meat consumption were categorised in two groups (below median, median and above) in these analyses. The same methods were applied for categorisation of dietary quality. For the continuous measures of meat consumption, red meat was included as increment of 100 g/d, and processed meat was included as increment of 50 g/d.
The associations between meat consumption and the studied outcomes were estimated using Cox regression analyses with age as the underlying timescale. The different types of meat consumption were included in different regression models. The analyses were adjusted for sex, educational attainment (the year before baseline), ethnicity, smoking, physical activity, alcohol, BMI, total energy intake and history of diabetes. To test if the associations between meat consumption and the outcomes were best represented by non-linear effects, quadratic and cubic terms were included in the models. However, non-linear effects were non-significant, so meat consumption was included linearly.
To evaluate if the assumption of proportional hazards was fulfilled, the Schoenfeld residuals were estimated. A linear regression model tested whether these residuals were correlated with the underlying timescale (age). These analyses indicated that the assumption was fulfilled. Further, the log-negative–log survival curves for each of the exposure and outcome variables were visually inspected and did not indicate serious violation of the assumption.
Associations between meat consumption and outcomes stratified by dietary quality
The statistical significance of a modifying effect of dietary quality was tested by including both meat consumption and dietary quality as separate main effects and as an interaction term with each other. These tests were performed both on analyses with meat consumption as a categorical and a continuous variable. The tests on continuous variables were considered the main tests, as they require the least statistical power.
All analyses were performed using SAS 9.4 (SAS Institute Inc.).
Ethics statement
Ethical permission for scientific studies carried out in Denmark is necessary only when they include biological samples, such as blood or tissue, or information from medical records. Therefore, ethical permission was not necessary for the present study.
Results
Among the 8007 participants included in the analyses on IHD, the median follow-up was 9·8 years, during which 439 cases of IHD were recorded. Among the 8198 participants included in the analyses on ACS, the median follow-up was 10 years, during which 242 cases of ACS were recorded.
The baseline characteristics of the study population stratified by red meat consumption and dietary quality are shown in Table 1. The characteristics varied greatly with both red meat consumption and dietary quality. In online Supplementary Table S1, the same characteristics are shown distributed on processed meat consumption. The distribution of meat consumption and dietary quality in the population showed a median consumption of 65 g/d for red meat and of 35 g/d for processed meat (online Supplementary Table S2).
Table 1. Baseline characteristics of study population stratified by consumption of red meat and dietary quality (n 8007)
(Numbers and percentages)
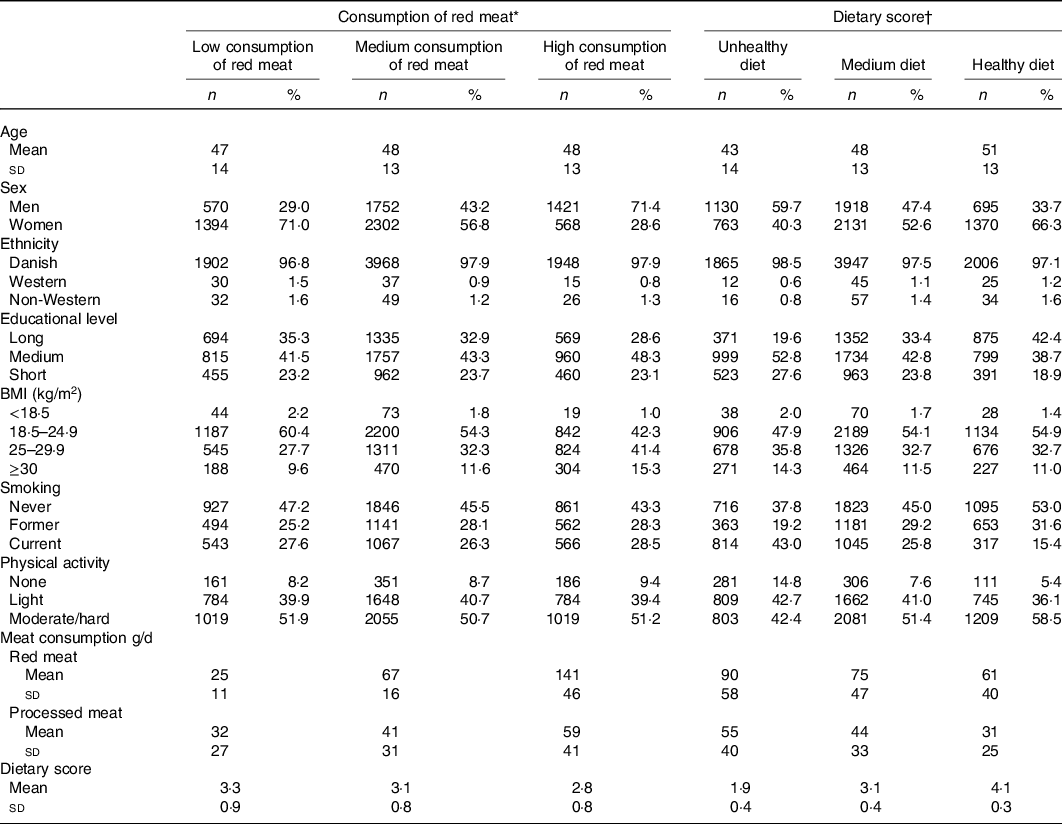
n, number of participants.
* Low consumption of red meat: <41 g/d; medium consumption of red meat: 41–97 g/d; high consumption of red meat: > 97 g/d.
† Unhealthy diet: < 2·4 on the dietary quality score; medium diet: 2·4–3·7 on the dietary score; healthy diet: > 3·7 on the dietary quality score.
The hazard ratio (HR) for IHD for increments of 100 g/d of red meat was 1·23 (95 % CI 0·99, 1·53). For increments of 50 g/d of processed meat, the HR for IHD was 1·09 (95 % CI 0·93, 1·29) (Table 2). The HR for IHD for high consumption compared with low consumption of red meat was 1·26 (95 % CI 0·93, 1·69). For processed meat, the HR for IHD for high consumption compared with low consumption was 1·10 (95 % CI 0·81, 1·50). The results on ACS were similar, though estimates were lower (online Supplementary Table S3).
Table 2. Association between red meat consumption, processed meat consumption and risk of ischaemic heart disease (n 8007)
(95 % confidence intervals)
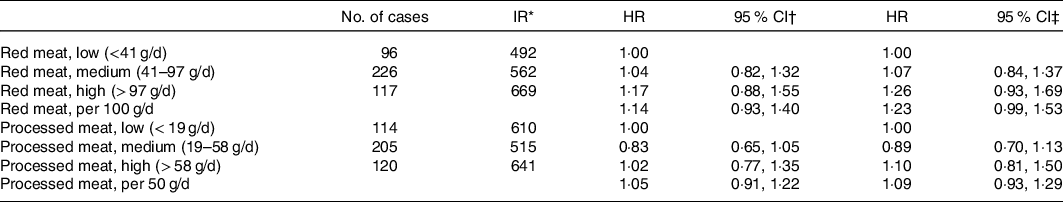
n, number of participants; IR, incidence rates; HR, hazard ratios.
* Per 100 000 person-years.
† Adjusted by sex.
‡ Adjusted by sex, educational attainment (the year before baseline), ethnicity, smoking, physical activity, alcohol, BMI, history of diabetes (10 years before baseline) and total energy intake.
Table 3. Association between red meat consumption, processed meat consumption and risk of ischaemic heart disease. Stratified by dietary quality* (n 8007)
(95 % confidence intervals)
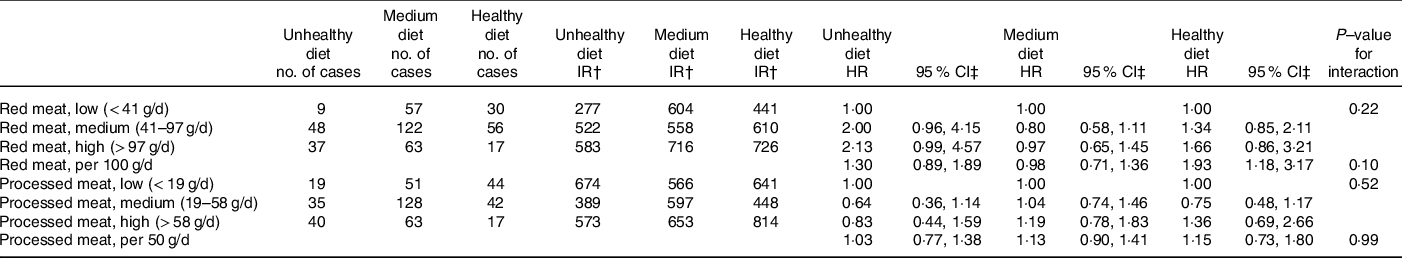
n, number of participants; IR, incidence rates; HR, hazard ratios.
* Unhealthy diet: <2·4 on the dietary quality score; medium diet: 2·4–3·7 on the dietary score; healthy diet: >3·7 on the dietary quality score.
† Per 100 000 person-years.
‡ Adjusted by sex, educational attainment (the year before baseline), ethnicity, smoking, physical activity, alcohol, BMI, history of diabetes (10 years before baseline) and total energy intake.
Associations between meat consumption and risk of IHD stratified by dietary quality are presented in Table 3. For the continuous measure of red meat consumption, the HR was strongest among those with a healthy diet (1·93 (95 % CI 1·18, 3·17)) followed by those with an unhealthy diet (1·30 (95 % CI 0·89, 1·89)), and a medium diet (0·98 (95 % CI 0·71, 1·36)). The test for interaction showed that these estimates were not statistically different (P = 0·10). The same was true for the categorical measure of red meat consumption (P = 0·22). Dietary quality did not modify the associations between processed meat consumption and risk of IHD either.
Results on associations between red and processed meat consumption and risk of ACS stratified by dietary quality showed the same trends indicating that dietary quality did not modify the associations (online Supplementary Table S4). Analyses on poultry consumption are shown in online Supplementary Tables S5–S9. The results showed no significant associations between poultry consumption and risk of IHD or ACS.
Separate analyses on the three cohorts from Danish National Survey on Diet and Physical Activity 2000–2002, 2003–2008 and 2011–2013, respectively, were also performed. These showed some differences in effect estimates, but none of the results was statistically significant, and we do not interpret these as different effects dependent on survey year.
Discussion
The results suggested a trend with higher consumption of red or processed meat being associated with higher risk of IHD. The effect estimate was highest for consumption of red meat. However, neither of these trends were statistically significant. Stratification by dietary quality did not indicate that associations between meat consumption and risk of IHD were modified by dietary quality.
The trend for red meat consumption is similar to those found in some previous studies(Reference Abete, Romaguera and Vieira2–Reference Pan, Sun and Bernstein4,Reference Etemadi, Sinha and Ward14) , though these studied cardiovascular mortality. Further, a meta-analysis did not find an association with IHD mortality(Reference Abete, Romaguera and Vieira2) and another meta-analysis did not find an association with risk of CHD(Reference Micha, Michas and Mozaffarian1). The trend for processed meat is somewhat weaker than the associations previously reported in systematic reviews(Reference Micha, Michas and Mozaffarian1,Reference Abete, Romaguera and Vieira2) though one of them only found an association with the broader cardiovascular mortality and not with IHD mortality(Reference Abete, Romaguera and Vieira2). A cohort study conducted in America(Reference Etemadi, Sinha and Ward14) on heart mortality with detailed dietary information found associations closer in magnitude to the trends observed in our study.
Meat consumption, especially red and processed meat consumption, has been heavily debated in relation to possible health effects. Associations between meat consumption and heart disease have mainly been attributed to saturated fat and cholesterol content, but in regard to processed meat also to ingredients such as Na or other preservatives(Reference Bronzato and Durante15). No agreement has been reached on recommended daily intake. However, the World Cancer Research Fund recommends that consumption of red meat should be limited to no more than 350–500 g/week, and that consumption of processed meat should be as low as possible(16). This recommendation is however based on possible carcinogenic effects of meat.
Identified associations and differences between study findings are influenced by differences in study populations and exposure and outcome definitions. For example, associations may differ between regions or even countries. In a meta-analysis on cardiovascular mortality, an association was found for processed meat consumption, but this association could only be observed in studies conducted in US populations and not in studies conducted in European or Asian population(Reference Wang, Lin and Ouyang17). Also, both red meat and processed meat are broader categories of meat that include different types of meat. What characterises dietary red meat or processed meat may therefore differ between countries. For example, pork may be a bigger contributor to red meat consumption in some countries compared with others, where beef could be a bigger contributor to red meat consumption. Previous analyses on the data included in the present study showed that red meat consumption is equally represented by beef/veal and pork and that processed meat consumption is mainly represented by ‘other processed meat’, some salamis and sausages and very little bacon(Reference Mejborn, Møller and Thygesen18). As few cohort studies have the power to analyse meat consumption in this level of detail, it is often not known what characterises red meat or processed meat in the diet of the particular study population. Other differences between countries could be in cooking methods. Examples include differences not only in how much salt is used or how hard the meat is fried but also in the meat’s fat contents, which is believed to be part of the biological pathway between meat consumption and risk of heart disease.
Other factors that will influence the estimates are the abilities to include influential confounders in the analyses. In the present study, both behavioural factors, socio-economic factors, BMI and disease history were included as confounders. BMI is commonly included in nutritional epidemiology. Yet, BMI is also influenced by diet and could be viewed as a mediator instead of a confounder in the associations between meat consumption and the outcomes. However, information on meat consumption, dietary quality and BMI is collected cross-sectionally, and it is not possible to deduce the temporality between these measures. No adjustment was undertaken for other meat types, but consumption of different types of meat is correlated. It is therefore possible that such adjustments would have been appropriate to disentangle the effects of the different types of meat from each other. For example, other published analyses on the same data showed that high consumption of red meat was associated with low consumption of poultry(Reference Mejborn, Møller and Thygesen18).
We found a statistically significant association between red meat consumption measured continuously and IHD risk among participants with a healthy diet. Yet, we consider this a chance finding, which should be interpreted with caution. However, if this association is in fact true, a possible explanation could be if some of those with a healthy diet have made healthy dietary choices because of being diagnosed with high cholesterol or high blood pressure, which are risk factors for IHD. The results did not support that dietary quality modified associations between meat consumption and risk of heart disease. This may be surprising as it could be expected that an overall healthy diet could counterbalance some of the potential harmful health effects of meat consumption. In particular, previous studies have shown that dietary quality is inversely associated with outcomes such as myocardial infarction(Reference Hansen, Overvad and Tetens19) and cardiovascular events(Reference Hlebowicz, Drake and Gullberg20). The results are however also influenced by the applied measure of dietary quality, which does not include all possible aspects of a healthy diet. A study conducted in Sweden found a statistically significant association between consumption of red meat and cardiovascular mortality. This association did not differ between those with high and low consumption of fruit and vegetables(Reference Bellavia, Stilling and Wolk6). Though only one aspect of a healthy diet was included in the Swedish analyses, the findings, in line with the findings from the present analyses, do not support the hypothesis that other dietary factors heavily influence the associations between meat consumption and disease development. It is however possible that more detailed information on dietary quality assessed in a larger dataset would suggest different conclusions.
Even though the results indicate trends in the association between meat consumption and risk of IHD, neither of the results were statistically significant. This highlights that studies on dietary factors’ association with disease outcomes require large cohorts with long follow-up and a sufficient number of disease outcomes in the population. The study population was followed for 5–18 years, but a major limitation of the study is that the population could be as young as 15 years at baseline. Hence, only a limited number of disease outcomes were observed in the population. This has deteriorated the power of the study and therefore limited the ability to reach statistical significance for observed associations. This is especially true for analyses on interactions between meat consumption and dietary quality.
Other limitations include that even though the Danish National Survey on Diet and Physical Activity surveys are representative regarding sex and age, in the latest surveys, participants with short education were underrepresented(Reference Pedersen, Christensen and Matthiessen21), which may limit the generalisability of the findings. In addition, the study only included a baseline dietary registration for each individual. Therefore, it is assumed that the dietary quality does not change during follow-up, but if the population has large variations in dietary quality during follow-up, this would influence the estimated associations. A study has previously shown that study participants’ diet does change substantially over time(Reference Dekker, Boer and Stricker22). This limitation is however very common in nutritional epidemiology, as repeated information on detailed dietary intake is rarely obtained. Another common limitation in nutritional epidemiology is misreporting of dietary intake, which could influence the associations if misreporting is biased by meat consumption, dietary quality or other factors that influence the risk of IHD.
Our study also has several strengths. It was possible to ensure complete follow-up of the study cohort, since identification of IHD was based on linking national registers with high validity and completeness and we included complete information on migration and death. This linkage also enabled us to include only incident cases of IHD, thereby minimising the risk of reverse causality as we excluded those with disease before baseline. The study also included information on a range of dietary components, which made it possible to evaluate if associations were modified by the overall dietary quality. This included registration of the total diet for 7 d, including weekend days, and the data collection process covering all seasons to allow for seasonal variations in dietary quality.
In conclusion, we found trends that higher consumption of red or processed meat was associated with higher risk of IHD, but neither of the trends were statistically significant. Associations between meat consumption and risk of IHD were not modified by dietary quality. Further studies that are able to explore modifying effects of dietary on associations between meat consumption and risk of IHD are needed.
Acknowledgements
The study was financially supported by Promilleafgiftsfonden for Landbrug, Denmark. Promilleafgiftsfonden for Landbrug had no influence on the study design, presentation and interpretation of results nor preparation of the manuscript.
All authors planned and designed the study. S. P. M. was responsible for data management and analyses and drafted the manuscript. All authors contributed to interpretation of study results, critical revision of the paper and approval of final version.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary materials referred to in this article, please visit https://doi.org/10.1017/S0007114521000623






