Over the past few years, the gluten-free diet (GFD) has increased in popularity at a rate greater than may be expected based on the prevalence of gluten-related disorders such as coeliac disease (CD), wheat allergy and non-coeliac gluten sensitivity(Reference Catassi, Anderson and Hill1–Reference Elli, Branchi and Tomba3). Individuals with irritable bowel syndrome may also avoid gluten, though this may be due to co-occurrence of non-coeliac gluten sensitivity(Reference Catassi, Alaedini and Bojarski4). It has been suggested that the rise in adherence to GFD has been driven primarily by those who do not have gluten-related disorders. The GFD has been widely promoted in popular culture, rising in popularity in part, due to mass media and non-scientific reports of health and weight-loss claims(Reference Jones5,Reference Croall, Trott and Rej6) , which are not supported by scientific evidence(Reference Marcason7).
We have previously reported that 1·9 % of Canadians self-report following a GFD(Reference Mudryj, Waugh and Slater8), defined as the complete elimination of foods like wheat, barley, rye and triticale(Reference Bascunan, Vespa and Araya9). While there are no known direct adverse health effects of avoiding gluten unnecessarily or without recommendation, there may be social and nutritional implications. Access to gluten-free (GF) products may be limited, particularly in non-urban centres(Reference Jamieson and Gougeon10), despite the documented improvement in the variety of GF products available to Canadian consumers(11). The economic burden of a GFD has been well-documented in the literature(Reference Jamieson and Gougeon10,Reference Panagiotou and Kontogianni12–Reference Mearns, Taylor and Boulanger15) , with commercially available GF products being significantly more expensive than comparable products(Reference Stevens and Rashid16); this may act as a barrier to dietary compliance, potentially contributing to clinical and nutritional consequences.
Awareness of possible differences in nutrient intakes is important when comparing dietary patterns and their associations with health and disease. Traditionally, nutrition therapy for those avoiding gluten has mostly focused on food items to be excluded from the diet(Reference Thompson, Dennis and Higgins17). However, research suggests concern about the nutritional profile of GF products, as few GF products are enriched with the vitamins and minerals that gluten-containing grains are, so they are usually lower in fibre and B vitamins(Reference Jamieson and Gougeon10,Reference Thompson, Dennis and Higgins17–Reference Pellegrini and Agostoni20) . Subsequently, individuals following a GFD may be susceptible to nutritional inadequacies. Nutrient composition analysis of packaged food products labelled ‘gluten-free’ compared with comparable gluten-containing products found that the fibre, Fe and folate content of GF pasta was significantly lower than regular pasta(Reference Kulai and Rashid21). Therefore, following a GFD may lead to possible nutrient deficiencies due to low intakes.
Evidence also suggests that patients observing a GFD may also be at risk for lowered intakes of Ca and vitamin D, though for some this may be due to secondary lactose intolerance commonly attributed to the loss of lactase in individuals newly diagnosed with CD(Reference Lerner, Wusterhausen and Ajay22,Reference Ojetti, Nucera and Migneco23) . In this way, multiple dietary avoidances among those adhering to a GFD diet may further compromise nutritional status, which may be compounded by impairments to nutrient absorption(Reference Malterre24). Therefore, it is important to examine the occurrence of multiple dietary avoidances among those following a GFD and their nutritional implications. The objectives of the present study were to (1) describe and test for differences in key nutrient intakes, overall diet quality, supplement use and BMI among Canadians who avoid dietary gluten compared to Canadians with no dietary exclusions and (2) describe additional dietary avoidances, such as meat, poultry, fish, shellfish, eggs or dairy products, adhered to by Canadians who avoid gluten.
Materials and methods
Design
The present study utilised a cross-sectional design using data from the 2015 Canadian Community Health Survey (CCHS) Nutrition Survey. The 2015 CCHS used a multistage stratified cluster sample that was nationally representative for age, sex, geography and socio-economic status (n 20 487; response rate 61·6 %)(25). The main objectives of the 2015 CCHS were to gather reliable, detailed and timely information on the dietary intake and nutritional well-being of Canadians and to inform future policies and health guidelines. The CCHS consisted of both a general health survey and 24-h dietary recall. The recall was used to estimate the distribution of usual dietary intake in terms of foods, food groups, nutrients and eating patterns among a representative sample of Canadians. For our analysis, we excluded participants who were pregnant (n 119) and breast-feeding (n 188), as well as participants <2 years old.
Ethics approval
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and our secondary analysis was approved by the Social Sciences and Humanities Research Council of Canada (file: CISS-RDC-993902). Informed consent was obtained from all subjects/patients. All analysis for the present study was conducted at the Manitoba Research Data Centre and is consistent with Research Ethics Board requirements. All study output and results were reviewed and vetted by Statistics Canada to ensure disclosure avoidance prior to release.
Measures
The 24-h recall was administered by trained interviewers, asking respondents about the various foods and beverages consumed in the past 24 h, including types and amounts of foods consumed, eating occasion and time of consumption(25). For participants under 6 years of age, the questionnaire was answered by a parent or guardian. For respondents aged 6–11 years old, the survey and 24-h recall were completed by the child, with assistance by a proxy(26). Dietary gluten avoidance was defined using self-reported responses to the question ‘Do you completely exclude any of the following foods from your diet? By completely exclude, we mean you never eat it on its own or as part of a prepared dish’. Responses included meat (beef, pork, lamb, etc.), poultry (chicken, turkey, duck, etc.), fish and shellfish, eggs, dairy products (milk, cheese, etc.) and gluten sources (wheat, barley, triticale, etc.). Adherence to a GFD was defined as an affirmative response to avoidance of gluten sources(26). Participants who did not respond affirmatively to any avoidance were categorised as having ‘no dietary avoidances’.
The Health Eating Index (HEI) is a tool that provides an indication of how well an individual’s diet aligns with recommendations for healthy eating and was estimated using a version adapted to Canada’s Food Guide to Healthy Eating (2007)(Reference Garriguet27). Notably, HEI is based on age group- and sex-specific dietary recommendations and includes a number of component scores for food groups and key nutrients, providing an HEI score out of 100. BMI is based on measured height and weight, calculated as weight (kg) divided by height (m2), and is reported here for adults (≥18 years old) only.
The Nutritional Supplement module as well as the Nutritional Supplement Details module included questions such as: ‘In the past month, that is, from one month ago to yesterday, did you take any vitamins, minerals, fibre supplements, antacids, fish oils or other oils?’(25) Possible answers to the question were yes, no, refusal to answer and do not know. Respondents were also asked to identify the supplements being used. If more than one supplement during the past month was used, the respondent was asked to locate the supplement container from which the Natural Product Number was recorded, if available. If unavailable, the brand name was recorded(25). These questions were used to classify respondents into those who use supplements and those who did not(25).
Canadians following a GFD and those reporting no dietary avoidances were described according to sex, age group, province or region, household education, income adequacy and race/ethnicity. Sex was dichotomised as male and female. Age groups were categorised as 2–17 years old and ≥18 years old. Region was grouped as British Columbia, the Prairies (Alberta, Saskatchewan and Manitoba), Ontario, Quebec and the Maritimes (New Brunswick, Newfoundland, Nova Scotia and Prince Edward Island), as we have done previously(Reference Mudryj, Waugh and Slater8). Highest level of household education was categorised as less than secondary school graduation, some post-secondary and post-secondary graduation or diploma/equivalent. Household income adequacy, as defined by Statistics Canada using total household income and number of individuals in the household, was classified into four categories: lowest to lower-middle income group, middle to upper-middle income group and highest income group. Missing data for income were imputed by Statistics Canada. Race/ethnicity was self-reported and dichotomised as white, and Indigenous or racialised, based on the categorisations collected in the survey(26).
Statistical analyses
First, we estimated proportions, with standard error, for each socio-demographic variable, according to dietary gluten avoidance and no dietary avoidances. We used a χ 2 test to test for differences between the two groups for each of the demographic variables, as well as self-reported use of nutrient supplements in the past 30 d. Second, we estimated the proportion and 95 % CI of the whole sample who avoided each of the exclusion groups (i.e. meat, poultry, fish and shellfish, etc.). We did the same for the sample who reported dietary gluten avoidance. Participants who reported at least one avoidance were further grouped as reporting < three or three or more total dietary avoidances and compared between those reporting dietary gluten avoidance and those not reporting dietary gluten avoidance.
Third, the 24-h dietary recall data were coded according to the 2015 Canadian Nutrient File(28), which includes GF foods, and were used to estimate daily average nutrient intakes. We estimated intakes of the following nutrients for both the sample avoiding gluten and those reporting no avoidances: energy (kJ/d), carbohydrate (g/d and percentage energy), saturated fat (percentage energy), folate (μg/d), vitamin B12 (μg/d), vitamin B6 (μg/d), thiamin (mg/d), riboflavin (mg/d), vitamin D (μg/d), Ca (mg/d), Fe (μg/d), fibre (g/d), Na (mg/d) and Zn (mg/d). These results were then calculated as a percentage of the Dietary Reference Intakes (DRI) for each respective nutrient to assess intake levels based on the recommended reference values for healthy populations(29). The DRI, which include RDA, Adequate Intake, and Tolerable Upper Intake Level, are recommended nutrient intakes based on age and sex. In this way, nutrient intakes were standardised according to age and sex. For fibre, this corresponds to an Adequate Intake; for Ca, vitamin D, folate, vitamin B12, Fe and Zn, this corresponds to the RDA and for Na, the Tolerable Upper Intake Level. We also reported nutrient intakes in amounts per 4184 kJ (1000 kcal), given significant differences detected in energy intake between the two groups. The normality of the distributions of nutrient intakes was examined through histograms, means, medians, standard errors, interquartile range and kurtosis. From these results, we were confident that distributions approximated normal distributions. As such, we used t tests to test for differences in percentage DRI for each respective nutrient according to dietary gluten avoidance. We also used t tests to test for differences in mean HEI and BMI (for adults only).
All analyses were performed using PASW SPSS Statistics, IBM, version 14 and STATA Statistical Analysis Software, RTI International, version 15. All analyses applied the survey sampling weights to account for the complex sampling design of the CCHS using the bootstrap method with 500 sets of replication weights supplied by Statistics Canada. Missing data were minimal, aside from income, as previously described, and as such any missing data were ignored.
Results
As we have previously reported, 488 participants, or an estimated 1·9 % of the Canadian population, report dietary gluten avoidance(Reference Mudryj, Waugh and Slater8). A higher proportion of Canadians who avoided dietary gluten were women, at 64·2 %, as compared with Canadians who reported no dietary avoidances, of which 48·9 % were women, respectively. Other than age group, no other demographic or socio-economic variables were significantly different between Canadians avoiding dietary gluten and those reporting no dietary avoidances. BMI did not differ significantly between adult Canadians avoiding gluten and those without avoidances (Table 1).
Table 1. Demographic characteristics of Canadians who avoid dietary gluten and those with no reported dietary avoidances based on results from the Canadian Community Health Survey, 2015
(Percentages and standard errors; mean values with their standard errors)
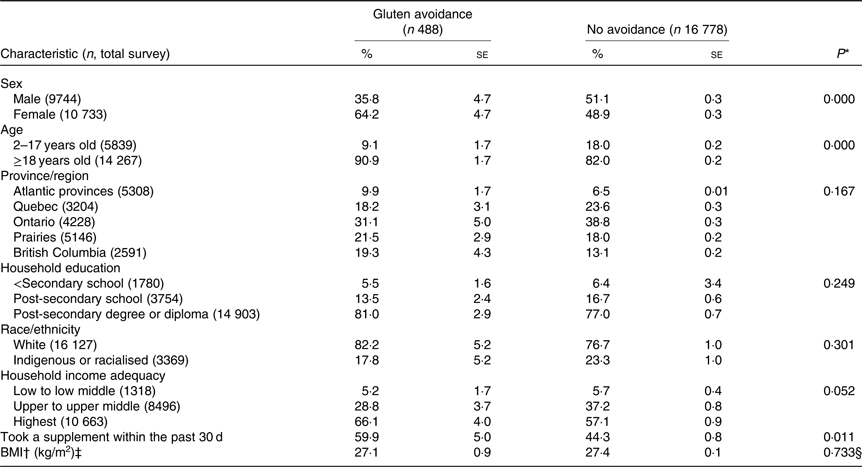
* Results from χ 2 test, unless otherwise noted.
† Based on measured height and weight.
‡ Respondents ≥18 years old.
§ Results based on t test.
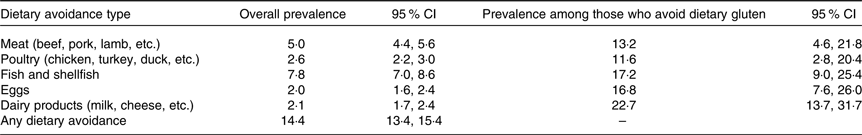
Overall, 14·4 % of Canadians self-reported at least one dietary avoidance. Over 1/5 of Canadians who reported avoiding gluten also reported dairy products avoidance. Canadians who avoid dietary gluten reported other food avoidances at a proportion higher than the general Canadian population. Approximately 17 % of Canadians who avoided gluten also reported excluding fish and shellfish from their diet, with similar numbers for egg avoidance (Table 2). Among Canadians who report at least one dietary avoidance of any kind (estimated at 14·4 % of the population), 10·0 % report two or more other dietary avoidances, or at least three total avoidances. In comparison, 11·1 % of Canadians who avoid gluten report two or more additional food avoidances, other than gluten.
Table 2. Self-reported dietary avoidances in the Canadian population and among those who report dietary gluten avoidance
(Percentages and 95 % confidence intervals)
Compared with Canadians who reported no dietary avoidances, those who avoided gluten had significantly lower intakes of energy content (kJ/d) and carbohydrate (g/d), although carbohydrate intake did not differ between the two groups when expressed relative to total energy intake. When nutrient intakes were expressed as a percentage of their respective DRI, Canadians who avoided gluten had significantly lower intakes of folate, vitamin B12, vitamin D, Fe, Na and Ca compared with those who did not avoid any food groups. Expressed as an amount per 4184 kJ (1000 kcal), only vitamin D intake was significantly lower among those avoiding dietary gluten and only fibre intake per 4184 kJ (1000 kcal) was significantly higher. No significant difference was found between the HEI score of both groups (Table 3). Post hoc analysis was conducted to describe and test for differences in the same nutrient intakes among Canadians avoiding dietary gluten and dairy products, and those avoiding gluten but not dairy products (Table 4). Vitamin D and Ca intakes were not significantly different between the two groups, either as a percentage DRI or per 4184 kJ (1000 kcal).
Table 3. Estimated nutrient intakes from 24-h dietary recall according to self-reported dietary avoidances
(Mean values with their standard errors)
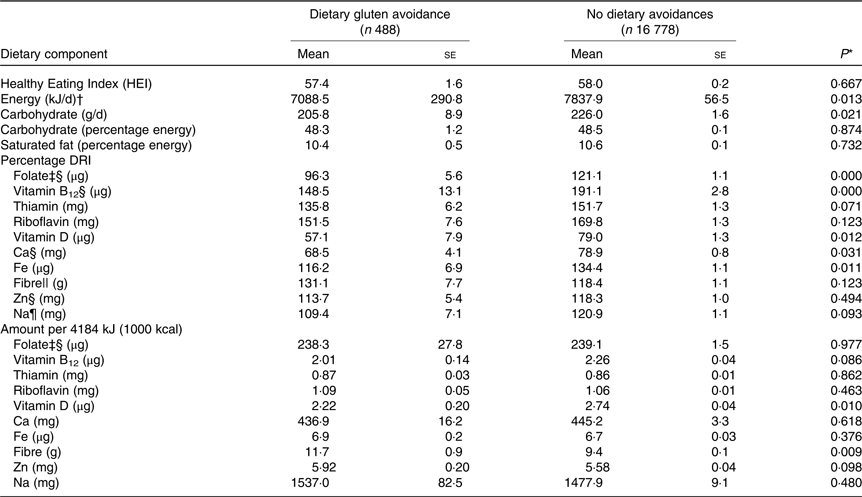
DRI, Dietary Recommended Intake.
* t Test.
† To convert kJ to kcal, divide by 4·184.
‡ Dietary folate equivalent.
§ RDA, average daily level of intake sufficient to meet the nutrient requirements of nearly all (97–98 %) healthy people.
‖ Adequate Intake, the recommended average daily intake level assumed to ensure nutritional adequacy, established when evidence is insufficient to develop an RDA.
¶ Tolerable Upper Intake Level (UL), highest level of daily intake that is likely to pose no risk of adverse health effects to almost all individuals in the general population.
Table 4. Estimated nutrient intakes from 24-h dietary recall among Canadians self-reporting dietary gluten avoidance according to self-reported dairy product avoidance
(Mean values with their standard errors)
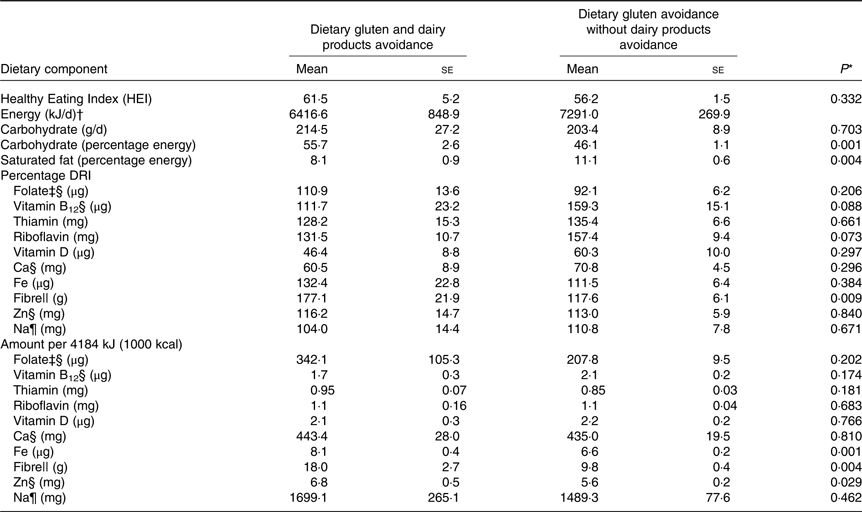
DRI, Dietary Recommended Intake.
* t Test.
† To convert kJ to kcal, divide by 4·184.
‡ Dietary folate equivalent.
§ RDA, average daily level of intake sufficient to meet the nutrient requirements of nearly all (97–98 %) healthy people.
‖ Adequate Intake, the recommended average daily intake level assumed to ensure nutritional adequacy, established when evidence is insufficient to develop an RDA.
¶ Tolerable Upper Intake Level (UL), highest level of daily intake that is likely to pose no risk of adverse health effects to almost all individuals in the general population.
Canadians who reported following a GFD were significantly more likely to use vitamin or mineral supplements in the past 30 d (Table 1), with nearly 60 % of those who avoid gluten reporting supplement use. Among those who reported any supplement use, 83·9 % of dietary gluten avoiders reported taking a supplement containing vitamin D in the last 30 d, compared with 74·0 % of those who report no avoidances (data not shown in table). Furthermore, 63·7 % of those avoiding dietary gluten reported taking a supplement containing vitamin B12 in the last 30 d, compared with 55·4 % of non-avoiders. Post hoc analysis was conducted to describe and test for difference in nutrient intake among Canadians avoiding gluten and reporting supplement use compared with gluten avoiders who do not report supplement use (Table 5). Notably, supplements were not considered in the estimation of nutrient intakes. HEI, or diet quality, was significantly higher among those avoiding gluten and reporting supplement use compared with those not reporting supplement use.
Table 5. Estimated nutrient intakes from 24-h dietary recall among Canadians self-reporting dietary gluten avoidance according to whether or not participants self-report supplementation
(Mean values with their standard errors)
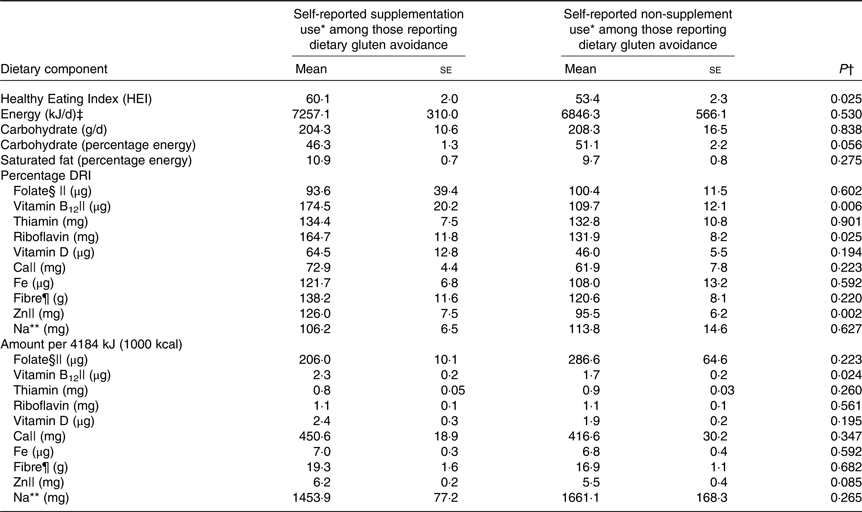
DRI, Dietary Recommended Intake.
* Nutrients from supplements were not included in estimations of nutrient intakes. Nutrient intakes reported reflect amounts consumed from foods.
† t Test.
‡ To convert kJ to kcal, divide by 4·184.
§ Dietary folate equivalent.
‖ RDA, average daily level of intake sufficient to meet the nutrient requirements of nearly all (97–98 %) healthy people.
¶ Adequate Intake, the recommended average daily intake level assumed to ensure nutritional adequacy, established when evidence is insufficient to develop an RDA.
** Tolerable Upper Intake Level (UL), highest level of daily intake that is likely to pose no risk of adverse health effects to almost all individuals in the general population.
Discussion
Dietary patterns and nutritional intakes, as measured in the present study, differed significantly between respondents adhering to a GFD compared with those who reported no dietary avoidances. Most notably, folate, Ca and vitamin D intakes were significantly lower among those following a GFD and were the only nutrients whose mean fell below their respective DRI for those adhering to a GFD. As clinical data were not collected as part of the present study, we are unable to comment on the clinical relevance of these significantly lower intakes; further research would be required.
We also report many co-existing dietary avoidances, which occurred more frequently among those reporting a GFD compared with the overall Canadian population. However, individuals who avoid gluten are not any more likely to avoid multiple other foods (i.e. three or more co-occurring avoidances) as compared with Canadians who report any other dietary avoidance, for example, people who avoid fish or eggs. As expected, the most reported intersection occurred between gluten and dairy products, consistent with previous findings. For example, in newly diagnosed CD patients, secondary lactose intolerance is common due to the loss of the enzyme lactase, caused by the damage to intestinal mucosa inflicted by gluten ingestion(Reference Lerner, Wusterhausen and Ajay22,Reference Ojetti, Nucera and Migneco23) . However this may be temporary, as following a strict GFD, the gut is able to heal, making lactose intolerance temporary in many individuals(Reference Canania30). An observational study of patients with non-coeliac gluten sensitivity also found that milk was more often avoided by this group, compared with the control(Reference Zingone, Bartalini and Siniscalchi31), though reasons were not reported. Notably, gluten avoidance is also a component of many elimination-based diets, including the popular FODMAP diet (which assists in managing irritable bowel syndrome symptoms), the Six Food Elimination Diet (used to manage eosinophilic gastrointestinal disorders)(Reference Kliewer, Venter and Cassin32,Reference Herrick, Murray and Halland33) and elimination of the top allergenic foods (wheat, cows’ milk, soya, egg, tree nuts/peanuts and fish/shellfish). These diets may partially account for the number of Canadians who follow a GFD with additional dairy products, egg or fish/shellfish avoidance. Finally, psychological factors also influence individual food choices and avoidances, including food neophobia, which is common among those with alternative diets. Food neophobia, or the fear of new foods, has been found to be relevant for gluten avoiders, and specifically CD was a determinant contributing to higher food neophobia levels in those who follow GFD(Reference Henriques, King and Meiselman34,Reference Zysk, Gląbska and Guzek35) .
Concerns over the nutritional implications associated with following a GFD have been established(Reference Miranda, Lasa and Bustamante19,Reference Kulai and Rashid21,Reference Vici, Belli and Biondi36–Reference Dennis, Lee and McCarthy38) . Our results confirm that Canadians following a GFD may be at risk for inadequate intakes of Ca and vitamin D, two nutrients integral to bone health and development. Several surveys have previously reported lower intakes of Ca and vitamin D among patients with CD(Reference Thompson, Dennis and Higgins17,Reference Grace-Farfaglia39) , increasing the risk of metabolic bone disease, osteoporosis and bone fractures(Reference Kemppainen, Kröger and Janatuinen40–Reference Carroccio, Soresi and D’Alcamo42). While individuals avoiding gluten are more likely to also avoid dairy products compared with the general Canadian population, our results do not indicate significantly different Ca or vitamin D intake according to whether or not people also avoid dairy products. This suggests that lower intakes of vitamin D and Ca among those avoiding gluten are not necessarily attributable to dairy products avoidance. Furthermore, Canadians who report no dietary avoidances also report mean intakes of both Ca and vitamins D below their respective DRI.
Those avoiding gluten also reported significantly lower percentage recommended intake for Fe and vitamin B12 compared with those with no avoidances. However, the coexistence of gluten and meat avoidance may partially account for significantly lower Fe and vitamin B12 intakes among Canadians who follow a GFD. Further research examining dietary sources of Fe and vitamin B12 would be required to examine if additional avoidances may be contributing; this analysis is beyond the scope of the present study. Importantly though, both mean Fe and vitamin B12 intakes were above 100 % of the DRI for those avoiding gluten. Therefore, while Fe and vitamin B12 intake is significantly lower among those avoiding gluten, intakes are not in a range suggestive of high vulnerability to deficiency among most Canadians avoiding dietary gluten. Clinical biomarkers necessary to provide insight regarding deficiencies were not collected by the CCHS and therefore not available for secondary analysis.
Given evidence of lower intakes of some nutrients, encouragingly, 59·9 % of Canadians who follow a GFD reported taking a dietary supplement in the past month, with the majority taking a supplement containing vitamin D. This suggests that the majority of Canadians avoiding dietary gluten are aware of the potential risk of vitamin D deficiency and are trying to mitigate this. Unfortunately, our post hoc results suggest those using supplements are consuming a healthier diet to begin with and those potentially in most need of dietary supplements were not using them. This finding is in line with previous research from Germany indicating that supplement users tend to be more health conscious(Reference Frey, Hoffman and Heuer43), and that among those using supplements, fewer people use supplements to treat deficiencies than for prevention or general wellness(Reference Frey, Hoffman and Heuer43).
The lower intake of folate among Canadians avoiding gluten may be related to the nutrient profile of GF cereal products. Federal law requires manufacturers to add folic acid to wheat-based breads, flours and cereals to prevent neural tube defects. However, GF foods, which do not contain wheat, are not required to be fortified with folic acid(Reference Yazynina, Johansson and Jägerstad44). Indeed, studies demonstrate that these products contain lower amounts of folate compared with their gluten-containing counterparts(Reference Thompson18,Reference Yazynina, Johansson and Jägerstad44) . Given the purpose of folic acid fortification of wheat-based products, women of child-bearing age, as well as during pregnancy, may be especially vulnerable to inadequate intakes of folate secondary to dietary gluten avoidance(Reference Bar-Oz, Koren and Nguyen45,Reference Hancock and Koren46) .
Although GF diets may be lacking in fibre, due to the necessary avoidance of many foods that are good sources of fibre (i.e. whole grains), and low content of fibre in GF products(Reference Vici, Belli and Biondi36), we did not observe a significant difference in fibre intake between groups according to percentage of recommended intake. In fact, according to amount of fibre consumed per 4184 kJ (1000 kcal), Canadians avoiding gluten consumed significantly more fibre compared with Canadians reporting no dietary avoidances. One explanation may be that Canadians are finding other fibre-rich GF alternatives to increase their fibre intakes, such as quinoa, amaranth or flours made with legumes or pulses to supplement their diet(Reference Theethira and Dennis47). This suggests that Canadians may be aware of the nutritional shortcomings of following a GFD and/or the food industry may be increasing the fibre content of food products advertised as GF accordingly. High consumer demand has driven food manufacturers to expand and improve the formulations and processing techniques used in their GF products(Reference Bender and Schönlechner48,Reference Hüttner and Arendt49) . Given the changing foodscape and research on the nutritional shortcomings of the GFD, it seems pertinent to monitor the GF food supply, as well as determine what food choices and dietary patterns other than gluten avoidance are contributing to these intakes. In particular, voluntary or mandatory fortification of GF products with folic acid warrants consideration.
Our study has several limitations. The CCHS only included data from the ten provinces, excluding people from the territories, living on First Nation reserves, settlements, full-time members of the Canadian forces and individuals who are institutionalised. This survey is also cross-sectional; thus, causal inferences cannot be drawn. However, the very large and representative sample size provides a benchmark for future analysis of further CCHS nutrition surveys. Another limitation is that the GFD was self-reported, and we cannot determine the proportion of the sample that follows a GFD due to CD, non-coeliac gluten sensitivity, wheat allergy or other reasons. Similarly, we cannot determine the frequency of supplement use and therefore their impact on nutritional adequacy. The small sample size of Canadians who reported multiple dietary avoidances precluded us from taking into account other differences between Canadians following a GFD and those reporting no avoidances. Further, the CCHS survey did not ask about other food avoidances such as nuts or beans/pulses, for example, and people avoiding these may have been included in the group reporting no avoidances. Although calculating nutrient intakes as a percentage DRI allowed us to assess intakes in a way that standardised nutrient requirements according to sex and age, we were not able to complete models adjusting for other factors, such as energy intake, sex, age or income adequacy, as analyses resulted in unstable estimates. Lastly, we did not apply the National Cancer Institute method to estimate usual intakes, as compared with average intakes, which requires the inclusion of the second dietary recall, due to the small sample who reported dietary gluten avoidance(50).
Conclusions
Individuals avoiding dietary gluten are at risk for nutritional deficiencies, which may be exacerbated by additional dietary avoidances. Patients should be advised on the nutritional quality of GF foods, particularly folic acid content and especially for women of child-bearing age. Knowledge of the risk for nutritional deficits associated with this dietary restriction is important for individuals and their healthcare providers to inform their dietary decisions, as well as for nutritional supplement use. Registered Dietitians should evaluate the nutritional adequacy of GF diets and determine whether there are additional dietary avoidances among clients avoiding gluten, and the potential impact on diet quality. Individuals with CD who have demonstrated evidence of recovery should be advised to retrial consumption of dairy products. Healthcare providers, including Registered Dietitians, gastroenterologists and primary care physicians, should provide guidance to ensure individuals avoiding gluten meet their nutritional goals.
Acknowledgements
We gratefully acknowledge the Manitoba Research Data Centre data analyst Dr Ian Clara for his support in data vetting. Although the research and analysis are based on data from Statistics Canada, the opinions expressed do not represent the views of Statistics Canada. We would also like to acknowledge Melissa Secord of the Canadian Celiac Association, as well as the Manitoba Chapter of the Canadian Celiac Association for their input. We have received permission from each person who has been named in this section.
The present study was supported by the Canadian Celiac Association’s J. A. Campbell Research Award (2018) to N. D. R. and the J. A. Campbell Young Investigator Award (2019) to A. N. M. N. D. R. is also supported by a Canadian Institutes of Health Research Early Career Investigator Award (155435). The present study was also partially supported through start-up funds from the University of Manitoba to N. D. R. This research was also supported by funds to the Canadian Research Data Centre Network (CRDCN) from the Social Science and Humanities research Council (SSHRC), the Canadian Institute for Health Research (CIHR), the Canadian Foundation for Innovation (CFI) and Statistics Canada.
N. D. R. and A. N. M. were involved in the design, conceptualisation and analysis/interpretation of the data. A. K. W., J. J. S., D. R. D. and C. N. B. were involved in the interpretation of the data. A. N. M., A. K. W. and N. D. R. were involved in drafting the manuscript. All authors were involved in reading/revising the manuscript and agreed with the material in the manuscript. We, the authors, take full responsibility for the content of the manuscript.
No potential conflict of interest was reported by the authors.








