Introduction
Over a period of 100 years, the proportion of people aged 60 and more will triple, from a mere 11 % in 1950 to no less than 33 % in 2050(1–Reference Goulding, Rogers and Smith4). Nutrition is one of the major determinants of successful aging, defined as the ability to maintain three key elements: low risk of disease and disease-related disability, high mental and physical function, and active engagement of life(Reference Knoops, de Groot and Kromhout5–Reference Kozlowska, Szczecinska and Roszkowski6). Food is not only critical to one's physiological well-being but also contributes to one's social, cultural, and psychological quality of life(Reference Schroll, Carbajal, Decarli, Martins, Grunenberger, Blauw and de Groot7). In fact, quality of life is mentioned worldwide as an important issue in future research related to active and healthy “successful” ageing.
Physiological and functional changes that occur with aging can result in changes in nutrient needs(Reference Vincent, Lauque and Lanzmann8–Reference Wakimoto and Block9). Knowledge of nutrient requirements of older adults is growing yet is still inadequately documented(Reference Blanc, Schoeller and Bauer10–Reference Foote, Giuliano and Harris11). Older adults have unique nutrient needs(Reference Dean, Raats, Grunert and Lumbers12). Both cross-sectional and longitudinal studies document that the quantity of food and energy intake usually decreases substantially across the spectrum of aging. Surprisingly, there is a lack of information about fatty acids, mainly long-chain polyunsaturated omega-3. Strategies to prevent and (or) reduce morbidity in the elderly are therefore required as worldwide the population ages. Increasing the intake of omega-3, particularly the long-chain n-3 PUFA may be one such strategy(Reference Buhr and Bales13–Reference Lichtenstein, Rasmussen and Yu15).
Omega-3 fatty acids are now generally recognized as potentially beneficial for optimal function of the cardiovascular system in adults(Reference Riediger, Othman and Miyoung16–Reference Kamphuis, Geerlings and Tijhuis17). As clear examples, because of the increasing risk of deteriorating health of the cardiovascular system and brain with age, is important to establish whether healthy aging is associated with changes in plasma ω3 fatty acid content or response to fortification/supplementation(Reference Whelan18). It is becoming increasingly evident that long chain PUFA from the n-3 family appears to be neuroprotective and may also have unique properties in affecting neurobiology, both of critical interest during the aging process(Reference Bazan19–Reference Lukiw and Bazan27). Intake of n-3 PUFA has also been associated with potential benefits in other age-related morbidities, including rheumatoid arthritis, depression and macular degeneration. In fact, surprisingly, in both plasma and red blood cells, several studies have reported that the content of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) rises significantly from the second to the seventh decade of life(Reference Caprari, Scuteri and Salvati28–Reference Vandal, Freemantle and Tremblay-Mercier33). Normally, higher plasma (and red cell) ω3 fatty acid status in the elderly would seem to be due to higher fish/seafood intake but may also be due to aging-related changes in ω3 metabolism. However, these findings are not universal, since other studies have found that the intake of polyunsaturated fatty acids decrease with age(Reference Garry, Hunt, Koehler, VanderJagt and Vellas34) and most older people eat less that the recommended amounts. In contrast to their proposed actions in childhood, where n-3 long-chain polyunsaturated fatty acids are required for healthy development of brain tissue, in older age are more like to act in a protective and health-maintaining manner. For example, n-3 are known to inhibit hepatic triglyceride synthesis and by modifying eicosanoid function, cause vascular relaxation, a diminished inflammatory process and decrease platelet aggregation(Reference Uauy and Valenzuela35).
Nevertheless, these studies all had important limitations, including a small number of subjects. In addition, although 65 years of age is frequently used as reference, there is no official or widely accepted definition of elderly, so the cut-off used in studies is often as low as 50 years of age. Furthermore, information about the health status, blood chemistry, cognitive function or physical activity of elderly research subjects is rarely given in sufficient detail to establish whether or not the data reported are for the healthy elderly. The main target of the present chapter of the systematic review is based on moderately healthy elderly, based on their active lifestyle, normal cognition and relatively good physical condition.
Ageing physiological process, its association with quality of life and the impact of omega-3 fatty acids intake and/or status is the focus of the present chapter. Undoubtedly, ageing is linked to several pathological conditions (osteoporosis, sarcopenia, neurodegenerative diseases, etc.) that are not targeted. The main question to be discussed in the present review is: How ω3 fatty acids may affect the overall diet and quality of life in the elderly people subjects?
Methods
This report deals with the effects of omega-3 fatty acids on normal aging of older adults ( ≥ 65 years) and on their quality of life.
Study identification
We searched Medline (1966–2011), EMBASE (1980–2011) and LILACS (1982–2011). The terms used and the search strategies were the following:
Fatty Acids, Omega-3/all subheadings
DHA
EPA
Aged
Aged nutrition physiology
Nutritional Status
Diet records
Dietary supplements
Health
Health Status Indicators
Quality of life
Cognition
Cognition disorders
Food, fortified
Bone density
Muscle tonus
Deficiency (subheading)
The search strategies, which were applied in the three databases above mentioned, were as follows:
“Fatty Acids, Omega-3”/all subheadings or “Docosahexaenoic acids (DHA)” or “Eicosapentaenoic acids (EPA)” or “DHA and EPA” and “Aged” or “Aged nutrition physiology” and “Nutritional status” or “Diet records” or “Dietary supplements” or “Health” or “Health Status Indicators” or “Quality of life” or “Cognition” or “Cognition disorders” or “Food, fortified” or “Bone density” or “Muscle tonus” or “Deficiency” (subheading).
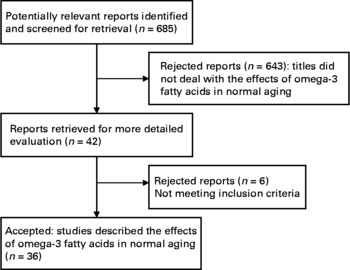
The search was not limited by language of publication or study design, in order to increase specificity. The titles and abstract obtained (a total amount of 685) were screened for relevant articles. The full texts of the relevant articles were checked for inclusion criteria (n = 100). Our purpose at this initial phase of screening was to identify articles that described studies about the effects of omega-3 fatty acids on normal healthy aging in human subjects and on their quality of life. Therefore, the full text of any articles for which it was not possible to determine relevance from the title and/or abstract was also retrieved for further review. At this point, only titles and/or abstracts that clearly did not meet these criteria for inclusion were rejected (n = 643). Two of the investigators (N. U. and M. A.) independently decided which studies met the inclusion criteria. Any differences were resolved by consensus, also by consulting a third reviewer (G. V.) in order to resolve any persisting difference. The flow diagram for screening process is depicted in (Fig. 1). The final number of studies included for the present systematic review was 36.
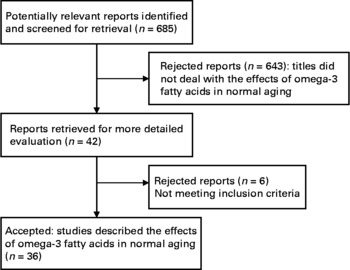
Fig. 1 Flow diagram for screening process.
Study selection criteria
Studies were included if they met the following criteria; otherwise they were excluded:
1 The studies reported research on human subjects including at least a group ≥ 65 years.
2 All participants were healthy elderly people without diagnosis of a pathological condition.
3 The studies were related to the effects derived only from EPA or DHA or EPA plus DHA dietary intakes and/or status, without the presence of other confounding factors such as vitamin or mineral supplements, etc.
4 The studies reported dietary intakes of EPA or DHA or EPA plus DHA from natural food sources and/or fortified foods and/or supplements. The supplements (if applied) could be taken with any dose or duration.
5 All categories of epidemiological studies were included.
6 The dietary assessment included a validated methodology, regardless of the tool.
7 The studies informing of the nutritional status included also the standardized method utilized.
To increase the generalization of the results, no restrictions were established on participants' baseline nutritional status or other study settings (community dwelling, participants on their own …)
Types of outcomes
We focused on the effects of omega-3 fatty acids on the main aspects derived from the impairment in the quality of life that is unavoidably associated to normal and physiological aging, such as nutritional status itself, cognition, bone health, muscle tonus, and general health status.
Data Extraction and quality assessment
Data were collected from each article for authors and year of publication, study design, population, age, sex distribution, total sample size, duration, outcomes of interest (Table 1).
Table 1 Characteristics of identified studies on the effects of omega-3 fatty acids on cognitive function in normal aging

MMSE: Mini Mental State Examination; RAVLT: Rey Auditory Verbal Learning Test; RCFT: Rey Complex Figure Test; RSPM: Raven's Standard Progressive Matrices; WAIS: Wechsler Adult Intelligence Scale-revised; IADL 7: Instrumental Activities of Daily Living; DECO: Detérioration Cognitive Observée (observed cognitive deterioration); CVLT: California Verbal Learning Test; CANTAB PAL 6: visuospatial learning and episodic memory test; CANTAB VRM: Verbal Recognition Memory; CANTAB SOC: Stockings of Cambridge; CANTAB SWM: Spatial Working Memory; PMSQ: Pfeiffer's Mental Status Questionnaire; DWRT: Delayed Word Recall Test; DSST/WAIS-R: Digit Symbol Substitution Test of the Wechler Adult Intelligence Scale-revised; WFT: Word Fluency Test
Information about the methodological quality of the studies was also abstracted. One author abstracted the data by using an internal data extraction form, and another one checked the accuracy. A 10-item quality appraisal form, based on the one used by Avenell & Handoll (2005)(Reference Avenell and Handoll36), was used to assess the methodological quality of each included study. The 10 items included the concealment of randomization, intention-to-treat-analysis, blinding of participants, treatment provider and assessor, comparability of groups at entry, identical care programmes, the specification of inclusion and exclusion criteria, definition of the intervention, the overall duration, appropriateness of the follow up, and withdraws.
Data Analysis/Statistics
Due to the heterogeneity among studies, very few studies met the inclusion criteria. Therefore, it was not possible to perform a meta-analysis. The overall effects of omega-3 fatty acids within the studies are described. The point estimates and statistical testing that were described in the original studies are summarized.
Results
The effects of omega-3 fatty acids on normal aging that we summarize as follows are those reported within the 36 studies that were finally included in the present review. According to the quality scale used, all the trials got a score range of 12–20 (20 was the possible maximum score). All the trials were conducted in “developed” countries, and academic institutes or national organizations supported all of them. None reported pharmaceutical company and/or food industry funding.
Effects of omega-3 fatty acid on cognitive function in normal aging
We have retrieved a total of 26 articles that evaluated the effects of omega-3 fatty acids on cognitive function in normal aging and healthy older people. Thirteen were longitudinal studies, ten were cross-sectional (three of them included longitudinal and cross-sectional analysis) and six were randomized, double-blind controlled trials. All of the studies used the Mini Mental State Examination (MMSE) to evaluate global cognitive function which include questions about orientation to time and place, registration, attention and calculation, recall, language, etc and/or other specific test (e.g. verbal fluency, speed, visuospatial skills, etc). Most of them considered cognitive impairment as a MMSE score < 25 and cognitive decline was defined as a drop of more than two points in the MMSE over the period studied; however, cognitive decline is defined uniquely according to each study, and thus comparing outcomes across studies must be interpreted with caution. One analyzed specifically changes in the nerve conduction velocity and compound muscle action potential. The content of omega-3 fatty acid was evaluated through dietary information (intake of fish or DHA/EPA) with appropriate questionnaires or concentration in plasma and/or erythrocyte membrane. The characteristics of the studies that were analyzed are described in Table 1.
Nineteen of all articles showed a positive relationship between an adequate fish consumption or n-3 fatty acids intake (diet or supplements) or total content in erythrocyte membrane and cognitive status or less cognitive decline during aging. These results are promising and encourage further research in order to establish a safe and effective treatment solution for cognitive impairment and subsequently disability in elderly population. Promoting higher intakes of n-3 PUFA in the diet or specifics supplements may have substantial benefits in reducing their risk of cognitive decline. However, authors concluded that further studies are warranted to confirm and evaluate theses potential positive effects.
Two of the articles showed some improvements but other measures remained unchanged. Vercambre et al. (Reference Vercambre, Boutron-Ruault and Ritchie37) observed an inverse association between fish consumptions and n-3 fatty acids intake and cognitive decline but not significant for functional impairment. Dullemeijer et al. (Reference Dullemeijer, Durga and Brouwer38) concluded that higher plasma proportions of n-3 fatty acids are associated with less decline cognitive performance in sensorimotor speed and complex speed but not in memory, information-processing speed and word fluency.
Five of the studies showed no positive effects of n-3 fatty acids in cognitive function. Two RCTs(Reference Dangour, Allen and Elbourne24, Reference Van de Rest, Geleijnse and Kok39) used high doses or EPA plus DHA and olive oil or oleic acid as placebo but did not find significant changes in any cognitive domains over 6 and 24 months, respectively. Both of them recommended that further longer trials should be conducted. Three cross-sectional studies(Reference Ortega, Requejo and Andrés40–Reference Van de Rest, Spiro and Krall-Kaye42) showed no significant differences in n-3 PUFA intake between controls and cases of cognitive decline/impairment, and two of them(Reference Laurin, Verreault and Lindsay41, Reference Van de Rest, Spiro and Krall-Kaye42) also did not show any significant associations between fatty fish or n-3 PUFA intake and cognitive change over 5 and 6 years, respectively.
More prospective studies, as well as interventions studies investigating the association between n-3 PUFA and domain-specific measures are needed to clarify the current conflicting results observed in the literature.
Effects of omega-3 fatty acids on immune function in normal aging
A total of five studies (four RCT and one cross sectional and longitudinal) examining the effect of omega-3 fatty acids on immune function (Table 2) were included. All four RCT studies assessed the effect of moderate dietary supplementation with omega-3 fatty acids (EPA or EPA + DHA) on immune biomarkers known to be altered in normal healthy aging. Even very low doses of n-3 fatty acids resulted in significantly decreased proliferative responses of lymphocytes in two of the studies(Reference Thies, Nebe-von-Caron and Powell43–Reference Bechoua, Dubois and Véricel44). In one of them(Reference Bechoua, Dubois and Véricel44), also, this was accompanied by a marked significant (P < 0·05) increase of their particulate PDE activity (+56–57 %) and an increase (P < 0·05) in cyclic nucleotide intracellular levels. At the same time, the glutathione peroxidase activity was markedly depressed (P < 0·01). The cross sectional study, on the contrary(Reference Wardwell, Chapman-Novakofski and Herrel45), reported significant positive correlations (P < 0·05) between PHA-induced proliferation and intake of DHA and EPA. However, these authors state that intakes of DHA plus EPA were inadequate for the studied population when compared to recommended intakes. They also suggest that dietary EPA in vivo might interact differently compared to in vitro studies where EPA is added to cell cultures.
Table 2 Characteristics of identified studies on the effects of omega-3 fatty acids on immune function in normal aging

On the other hand, a moderate amount of extra supplementary EPA (720 mg) resulted in a decrease of NK cell activity in the same elderly population(Reference Thies, Nebe-von-Caron and Powell46). This decline (48 %) was fully reversed by 4 weeks after supplementation had ceased.
The effects of different amounts of EPA on innate immune outcomes in older males compared to young were also evaluated(Reference Rees, Miles and Banerjee31). EPA was incorporated in a linear dose-response fashion into plasma and mononuclear cell (MNC) phospholipids; incorporation was greater in the older men. This increased incorporation was associated with decreased production of prostaglandin E2 by MNCs. Also, EPA treatment caused a dose-dependent decrease in neutrophil respiratory burst only in the older men.
These five above mentioned studies therefore suggest that even very low doses of omega-3 fatty acids may be sufficient to affect the immune responses of elderly subjects.
Effects of omega-3 fatty acids on bone health and muscle tonus in normal non-pathological aging
In total, three studies were identified that described the effects of omega-3 fatty acids on bone health or muscle tonus with normal aging; one was a RCT and two were cohort studies. The characteristics of the studies that were analyzed are described in Table 3. The three of them described positive outcomes derived from both dietary and supplemental omega-3 fatty acid intakes on aging.
Table 3 Characteristics of identified studies on the effects of omega-3 fatty acids on bone health and muscle tonus in normal aging

A single cohort study(Reference Farina, Kiel and Roubenoff47) that evaluated the effects of omega-3 fatty acids on bone health in aging was identified. This study investigated the associations between dietary polyunsaturated fatty acid and fish intakes and hip bone mineral density (BMD) at baseline (1988–1989, n = 854) and changes 4 year later in individuals (n = 623) with a mean age of 75 years in the Framingham Osteoporosis. High intakes (> 3 servings/wk) of fish relative to lower intakes were associated with maintenance of femoral neck BMD (FN-BMD) in men (dark fish + tuna, dark fish, and tuna) and in women (dark fish) (P < 0·05), thus suggesting that fish consumption may protect against bone loss. This study was adjusted for confounders, used valid methods to measure outcomes, and described withdrawals and dropouts.
Two studies that assessed the effect of omega-3 fatty acids on muscle tonus in normal aging were identified. The cohort study(Reference Robinson, Jameson and Batelaan48) examined the relationships between diet (fatty fish consumption) and grip strength in older men and women living in their own homes. Of the dietary factors considered in relation to grip strength, the most important was fatty fish consumption. An increase in grip strength of 0·43 kg (95 % confidence interval CI = 0·13–0·74) in men (P = 0·005) and 0·48 kg (95 % CI = 0·24–0·72) in women (P < 0·001) was observed for each additional portion of fatty fish consumed per week. Only one RCT study evaluating the effect of omega-3 fatty acids in muscle tonus in normal aging was retrieved(Reference Smith, Atherton and Reeds49). The objective was to evaluate the effect of omega-3 fatty acid supplementation for 8 weeks on the rate of muscle protein synthesis in elderly population (69- 73 years). Omega-3 fatty acid supplementation (1·86 g EPA and 1·50 g DHA) augmented the hyperaminoacidemia-hyperinsulinemia-induced increase in the rate of muscle protein synthesis (from 0·009 ± 0·005 %/h above basal values to 0·031 ± 0·003 %/h above basal values; P < 0·01), which was accompanied by greater increases in muscle mTORSer2448 (P = 0·08) and p70s6kThr389 (P < 0·01) phosphorylation, two elements of intramuscular signal transduction proteins involved in the regulation of muscle protein synthesis. The authors of these two studies suggest that these important influences on muscle function in older men and women raise the possibility that omega-3 fatty acids may be useful for the prevention and treatment of sarcopenia.
Effects of omega-3 fatty acids on quality of life and mortality in normal aging
Two single studies (both of them RCT) assessed the influence of omega-3 fatty acids in the quality of life of normal aging (Table 4). Moreover, the baseline characteristics of the population of the two studies were the same, 302 independently living older individuals. The studies differed in the outcomes measured(Reference Van de Rest, Geleijnse and Kok50, Reference Van de Rest, Geleijnse and Kok51). The first one investigated the effect of EPA and DHA (1800 mg/d EPA+DHA, 400 mg/d EPA or placebo, for 26 wk) on mental well-being. The second one evaluated the effect on physical health, psychological health, social relationships and satisfaction with environment through the World Health Organization Quality of Life questionnaire (WHOQOL).
Table 4 Characteristics of identified studies on the effects of omega-3 fatty acids on quality of life and mortality in normal aging

Plasma concentrations of EPA+DHA increased by 238 % in the high-dose and 51 % in the low dose fish-oil group, compared with the placebo group, reflecting excellent compliance. However, treatment with neither 1800 mg nor 400 mg differentially affected any of the measures and geriatric scales of mental well being. Following the same pattern, median baseline total WHOQOL scores ranged from 107 to 110 in the three groups and were not significantly different from each other. Treatment with 1800 mg o 400 mg EPA-DHA did not affect total Quality of Life questionnaire (QOL) or any of its separate domains after 26 weeks of intervention. For the interpretation of these results, however, it is quite interesting to note that the placebo capsules contained mainly oleic acid.
Two studies estimating the effect of omega-3 fatty acid on mortality in healthy aging were retrieved (Table 4). Folsom and Demissie(Reference Folsom and Demissie52) investigated the diet of a group of 720 postmenopausal women with low cancer and coronary heart disease risk. There was an inverse age- and energy-adjusted association between total mortality and fish intake, with a relative risk of 0·82 (95 % confidence interval: 0·74, 0·91) for the highest versus lowest quintile. Estimated marine omega-3 fatty acid intake was not associated with total or cause-specific mortality. A recent intervention study(Reference Einvik, Klemsdal and Sandvik53) showed results similar to those above mentioned. A group of elderly men (n = 282) received a total of 2·4 g n-3 PUFA in two capsules twice daily (49 % EPA and 35 % DHA) for 36 months. The authors observed in this supplemented population a tendency toward reduction in all-cause mortality that, despite the low number of participants, reached almost statistical significance (P = 0·063).
Discussion
In the present review we examined the effect of omega-3 fatty acids on different aspects which modulates the quality of life and the abilities to manage for a better life in aging. We finally included thirty-six articles that analyzed parameters related to cognitive decline, bone health and muscle tonus, immune function and general quality of life and mortality.
Results of the present systematic review suggest that the omega-3 fatty acids may have substantial benefits in reducing the risk of cognitive decline in older people, although there were five studies with no positive effects. The variability in outcomes between human studies which are confounded by methodological differences (type of food frequency questionnaire, test to measure cognitive decline, design of the study, etc), make it difficult for conclusions to be made at this time.
Two RCTs of the five negative studies used as placebo olive oil or oleic acid. Recently, Rosales(Reference Rosales54) has published a letter in which explained the possible weakness in these studies. For example, as indicated by the authors, the study population might already consume a sufficient amount of PUFA in their diets and thus not be sensitive to the dose of DHA/EPA provided, but they have also rejected that control group might result in maintaining cognitive function in later life, comparable to the effects of DHA/EPA, because they consumed an extra amount of oleic acid (olive oil) which could provided benefits, albeit by different mechanisms. Actually, prospective studies have shown that the Mediterranean diet is associated with slower cognitive decline and a reduced risk of progression(Reference Panza, Frisardi and Seripa55). Oleic acid, the major component of olive oil, has recently shown to provide a satiety factor, oleylethanolamide, which enhances memory consolidation without crossing the blood-brain barrier(Reference Campolongo, Roozedndaal and Trezza56). This is important in verbal learning, organization, and memory. Oleoythanolamide is a mediator in maintaining cognitive function that it is not related to vascular or other nonvascular biological mechanisms (ie, metabolic, oxidative, and inflammatory). Thus, this evidence suggest that these RCTs should consider the benefits of oleic acid as well as omega-3 PUFA in protecting against age-associated cognitive decline and maintaining cognitve function in later life.
More prospective studies, as well as intervention studies investigating the association between n-3 PUFA and domain-specific measures are needed to clarify the current conflicting results observed in the literature, although these results are promising and encourage promotion higher intakes of n-3 PUFA in the diet or specifics supplements since it seems to have substantial benefits in reducing their risk of cognitive decline(Reference Buhr and Bales13). Earlier intervention is a key factor in potentially treating age-related memory disorders and the maintenance of healthy brain during aging.
The elderly are particularly susceptible to infections due to a decline in immune function with age(Reference Rees, Miles and Banerjee31). The infections also tend to have more severe consequences. Aging results in declines in lymphocyte functioning and proliferation, reductions in antibody formation, and declines on hormones necessary for thymus gland functioning. Environmental factors leading to declines in immune function include certain drug use, and deficiencies in nutrients required for immune function(Reference Everitt, Hilmer, Brand-Miller, Jamieson, Truswell, Sharma, Mason, Morris and Le Couteur14). These deficiencies can be due to a reduction in food intake, as well as a reduced absorption and metabolism of nutrients. Active infections can increase the requirements for certain nutrients, and concomitant diseases can increase the morbidity of infections. Normal aging is accompanied by diverse changes in the immune system. Altered function of both T- and B-cells can be shown by losses in proliferative ability and interleukin-2 and interferon synthesis. This discusses the changes in immune function in the elderly that may be mediated by the intake/status of n-3 fatty acids, and the potential clinical implications of these changes in their metabolism. Only five studies related to this issue were included. The most stimulating global observation is that even low doses of omega-3 fatty acids may be sufficient to affect the immune response in elderly people under moderate dietary supplementation(Reference Thies, Nebe-von-Caron and Powell43–Reference Wardwell, Chapman-Novakofski and Herrel45). However, an important pitfall of all these studies is that those have not been evaluation long-term effects but also the impact on immunological biomarkers after supplementation is ceased.
A total of three studies were identified that described the effects of omega-3 fatty acids on bone health or muscles tonus with normal aging. Although clear scientific evidence seems to be still insufficient, the three of them described positive outcomes from dietary and supplemental omega-3 fatty acids. The most relevant observation in relation to bone health is the very recent cohort study by Farina et al. (Reference Farina, Kiel and Roubenoff47) in which a long-term (four years changes) effect of consuming fatty fish has been assessed: maintenance of femoral neck bone mineral density either in men or women were well kept. Unfortunately, this is the only powerful study that we considered able to be included in the systematic review. As for the muscle tonus, supplementation with omega-3 fatty acids seems to be very useful and promising to stimulate the complicated protein synthesis during healthy aging(Reference Amarantos, Martinez and Dwyer57). In fact, these nutrients may be considered of critical importance to prevent sarcopenia. Finally, undoubtedly clinical trials are urgent to test the effectiveness of these interventions with omega 3 in reducing the loss of bone health and muscle mass and function associated to normal aging(Reference Farina, Kiel and Roubenoff47).
Public health efforts to promote health and functional independence are critical strategies in helping older adults stay healthy(Reference Armstrong, Doyle and Lamb58). Research has shown that poor health does not have to be an inevitable consequence of aging(1, Reference Gillette, Abellan and Andrieu59). Older adults who practice healthy behaviors, take advantage of clinical preventive services, and continue to engage with family and friends are more likely to remain healthy, live independently, and incur fewer health-related costs(Reference Blacklow2). An essential component to keeping older adults healthy is preventing chronic diseases and reducing associated complications. About 80 % of older adults have one chronic condition, and 50 % have at least two. Infectious diseases (such as influenza and pneumococcal disease) and injuries also take a disproportionate toll on older adults.
In the present systematic review, only two RCT studies reached the criteria for inclusion and discussion. The outcomes to be evaluated after supplementation with EPA and DHA were mental well-being, physical health, psychological health and social relationship with no differences observed reagardless of high vs. moderate dose(Reference Van de Rest, Geleijnse and Kok39, Reference Laurin, Verreault and Lindsay41–Reference Van de Rest, Spiro and Krall-Kaye42, Reference Van de Rest, Geleijnse and Kok50, Reference Van de Rest, Geleijnse and Kok51).
As for mortality an inverse age-and energy-adjusted association between total mortality and fish intake was found. In general, a tendency toward reduction in all-cause mortality is observed after EPA and DHA supplementation although the positive effect seems to be within a better dietary and quality of life patterns(Reference Einvik, Klemsdal and Sandvik53).
Acknowledgements
There are no conflicts of interest for the authors.
Natalia Úbeda (NU) was mainly involved in the design of the search strategies, the inclusion criteria, abstracted the data and quality assessment and the preparation of the methods, results and discussion sections of the manuscript. Finally, NU reviewed carefully the whole manuscript.
María Achón (MA) was mainly involved in the design of the search strategies, the inclusion criteria, abstracted the data and checked the accuracy once NU abstracted the data. MA was also involved in the preparation of the methods, results and discussion sections of the manuscript. Finally, MA reviewed carefully the whole manuscript.
Gregorio Varela-Moreiras (GVM) had the overall the responsibility of the systematic review. He was mainly involved in the design of the search strategies, and was also involved in the introduction and discussion sections of the manuscript but also the final preparation of the systematic review.
No funding was provided for the present work.