Introduction
Out-of-hospital cardiac arrest (OHCA) is a life-threatening condition. Each year more than an estimated 300,000 people suffer an OHCA in North America.Reference Roger, Go and Lloyd-Jones 1 Despite recent advancements in prehospital and emergency care, the prognosis in North America remains poor, with on average less than 10% surviving,Reference Nichol, Thomas and Callaway 2 , Reference Sasson, Rogers and Dahl 3 an unfortunate trend that has remained relatively stable over the past 30 years.Reference Sasson, Rogers and Dahl 3
Although early cardiopulmonary resuscitation (CPR) and rapid successful defibrillation can improve survival rates to almost 40%,Reference Weisfeldt, Sitlani and Ornato 4 it is highly dependent on numerous factors as represented by the links in the cardiac chain of survival, including immediate recognition of the event and activation of emergency medical services (EMS), early CPR, rapid defibrillation, effective advanced life support, and integrated post-cardiac arrest care.Reference Travers, Rea and Bobrow 5 The Utstein variables were formulated as a template for cardiac arrest research and as a way to report the contribution of individual links in the chain.Reference Jacobs, Nadkarni and Bahr 6 This template also highlights core data elements necessary for OHCA studies with the appropriate definitions (e.g., cardiac arrest witness status, EMS response time, bystander CPR, etiology).Reference Jacobs, Nadkarni and Bahr 6 Researchers believed that these variables would account for most, if not all, aspects of survival.
In 2010, Rea et al. demonstrated that the Utstein variables accounted for only 72% of the nontraumatic EMS-treated survival (c-statistic=0.86), which suggests that other unknown factors may influence outcomes.Reference Rea, Cook and Stiell 7 But despite the vast amount of evidence implicating the Utstein variables as the main predictors of survival, few studies to date have investigated non-Utstein variables as predictors of survival and their influence on outcome variability.Reference Sasson, Rogers and Dahl 3 , Reference Rea, Cook and Stiell 7
In OHCA, socioeconomic status (SES)Reference Clarke, Schellenbaum and Rea 8 – Reference Sayegh, Swor and Chu 14 and race/ethnicityReference Sayegh, Swor and Chu 14 – Reference McNally, Robb and Mehta 24 have been studied in relation to survival-to-hospital discharge and bystander CPR. These results are often contradictory and inconclusive, and these studies were limited in scope, only including one or two non-Utstein variables.
More recently, studies investigated the role of multiple factors on OHCA outcomes by expanding research from other disciplines, demonstrating that location can influence health outcomes.Reference Diez Roux 25 Ahn et al. used the Carstairs index as a composite measure to relate neighbourhood deprivation to cardiac arrest outcome in South Korea. They created deprivation indices for each census tract by averaging the z-standardized score across four census-derived indicators (overcrowding, unemployment among economically active men, percent in manual occupations, and lack of car ownership). Districts were then categorized into five quintiles based on level of deprivation. After adjusting for the Utstein variables, survival was significantly lower in the most deprived neighbourhood as compared to the least deprived.Reference Ahn, Shin and Hwang 26 Sasson et al. evaluated collectively the influence of neighbourhood median household income and racial composition on the probability of receiving bystander CPR.Reference Sasson, Magid and Chan 13 They found that when compared to high-income Caucasian neighbourhoods, bystander CPR was less likely to occur in all neighbourhoods except those racially integrated with high median household incomes.Reference Sasson, Magid and Chan 13
Aside from a few prior studies, the majority of the literature has explored SES as a single variable (i.e., median household income or property tax value) with widely differing results. No study has been conducted in a Canadian setting, and none has collectively evaluated geographic, environmental, social, and cultural factors. Despite numerous examples within the social science and epidemiology literature where SES is treated as a complex, multidimensional construct encompassing varied socioeconomic and demographic factors, OHCA studies continue to use single SES descriptors in their analyses. This limitation might lead to inaccurate conclusions or mask potential differences in health-related outcomes.Reference Braveman, Cubbin and Egerter 27 Furthermore, no previous study has investigated whether non-Utstein factors account for the remaining 28% of survival.
Given the previous limitations in the existing knowledge base, this study will investigate nontraditional determinants of OHCA outcomes in Toronto, Canada. In particular, neighbourhood factors will be used to investigate and potentially improve the understanding of what influences cardiac arrest outcomes.
Objectives
The objective of this study is to describe the methodology that will be used to investigate the role of neighbourhood factors as determinants of out-of-hospital cardiac arrest outcomes. The specific research questions are the following:
-
1. In OHCA patients, are patient home neighbourhood factors associated with either survival-to-hospital discharge or a return of spontaneous circulation (ROSC) at emergency department (ED) arrival? Does the addition of patient home neighbourhood factors to the Utstein variables improve the overall discrimination of those variables?
-
2. In OHCA patients, are arrest location neighbourhood factors associated with bystander CPR? Does the addition of arrest location neighbourhood factors to the Utstein variables improve the overall discrimination of those variables?
Methods
Study design
A retrospective, observational cohort study design will be used to investigate the relationship between neighbourhood factors and cardiac arrest outcomes.
Setting and study participants
All patients who experience an OHCA within the catchment area of the University of Toronto’s regional coordinating centre are entered into the Resuscitation Outcomes Consortium (ROC) Epistry–Cardiac Arrest registry, whose methodology has been previously described.Reference Morrison, Nichol and Rea 28 Briefly, ROC Epistry–Cardiac Arrest is a prospective population-based epidemiologic web registry of consecutive OHCA patients assessed by prehospital care providers. Prehospital care providers complete standardized documentation after each cardiac arrest, which is entered into ROC Epistry–Cardiac Arrest. Collected data include patient identifiers, call characteristics, prehospital interventions, and outcomes. An extensive quality assurance program is in place to verify the accuracy of the study data.Reference Morrison, Nichol and Rea 28
Primary care paramedics provide prehospital care in all regions and can perform CPR and semiautomated defibrillation. First responders from local fire departments and advanced care paramedics are tiered to all OHCA patients if and when available. Fire services in Ontario are equipped with automated external defibrillators and can perform basic life-support skills, while advanced care paramedics are able to gain intravenous access, provide advanced airway manoeuvres, and administer advanced life support (ALS) medications.
Inclusion and exclusion criteria for this study are in accordance with the Utstein template.Reference Jacobs, Nadkarni and Bahr 6 All adult patients within the city of Toronto, age 20+ years, who sustained a nontraumatic OHCA will be eligible for enrolment. A minimum age of 20 years will be used to be consistent with other literatureReference Rea, Cook and Stiell 7 and the Canadian census age category definitions. 29 Any patient who met the criteria for obvious death (i.e., rigor mortis, lividity, decapitation, hemisection, or decomposition), who had a valid do-not-resuscitate-advanced directive, or whose OHCA was witnessed by paramedics will be excluded. Any patient who is missing adequate information for geocoding will also be excluded.
Geocoding
The patient’s individual postal code will be used to determine his or her neighbourhood. 30 Unfortunately, in health research, the use of the term neighbourhoods (or community or area) is problematic because it has been broadly used to determine health, yet rarely has been consistently defined.Reference Diez Roux 25 Although there is no standard definition of neighbourhood within the ROC Epistry–Cardiac Arrest, census tracts will be used in this project to define neighbourhoods. Census tracts consist of relatively small homogeneous subsets of the population with about 2,500–6,000 people (Figure 1) 31 and have been used previously when studying the role of location in OHCA outcomes.Reference Clarke, Schellenbaum and Rea 8 , Reference Hallstrom, Boutin and Cobb 9 , Reference Mitchell, Stubbs and Eisenberg 11 – Reference Sayegh, Swor and Chu 14 , Reference Galea, Blaney and Nandi 17 , Reference Iwashyna, Christakis and Becker 23 , Reference Nichol, Stiell and Laupacis 32
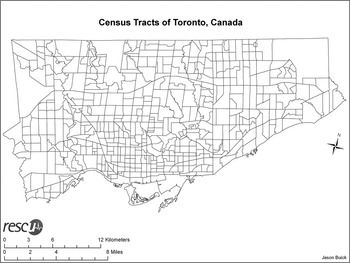
Figure 1 The 531 census tracts within the city of Toronto.
The patient’s home address will be used in the analysis for survival-to-hospital discharge (and a ROSC at ED arrival) under the premise that survival is dependent on both the event and patient characteristics. The patient’s home neighbourhood will be used as a surrogate for patient characteristics, because previous literature shows an association between home neighbourhood and cardiac risk factors, unhealthy behaviours, and overall health.Reference Leal and Chaix 33 – Reference Larson, Story and Nelson 45 The neighbourhood factors of the arrest location (i.e., the pickup address) will be used to study the effects on bystander CPR, because the emergency response (i.e., bystanders and EMS/paramedics) is contingent on the arrest location.Reference Vaillancourt, Lui and De Maio 10 – Reference Sasson, Magid and Chan 13 , Reference Govindarajan and Schull 46 – Reference Grossman, Kim and Macdonald 48
A patient’s home address is recorded as mailing address with street name, street number, and postal code, whereas the pickup address is recorded as a mailing address, with latitude and longitude coordinates and a Universal Transverse Mercator (UTM) value.Reference Morrison, Nichol and Rea 28 Postal codes will be the preferred source for identifying addresses. Missing postal codes will be determined from the street address, 49 the latitude/longitude, or UTM values 50 in a hierarchical fashion.
Postal codes will be linked to one of 531 nine-digit census tracts through a Postal Code Conversion File. 30 Postal code conversion involves assigning each postal code to a census tract based on “best fit” dissemination area provided by Statistics Canada. In this approach, the postal code is assigned to the census tract that best covers the given postal code area. Each cardiac arrest patient will be assigned the characteristics of the associated census tract based on either the patient’s home address or pickup address using geographic information system (GIS) mapping technology.
Neighbourhood variables
Neighbourhood variables to be included in the analysis include 1) the Ontario Marginalization Index (ON-Marg), 2) the crime rate, and 3) the density of family physicians. Each neighbourhood variable is expressed at the census tract level.
The ON-Marg is a geographically derived index used to study marginalization and highlight inequalities in various measures of health and social well being (Table 1).Reference Matheson, Dunn and Smith 51 While previous indices relied heavily on aspects of material deprivation (e.g., income, car and home ownership, education), the ON-Marg reflects the change in society where new inequality measures may better reflect deprivation and health. Its dimensions include 1) residential instability, 2) dependency, 3) material deprivation, and 4) ethnic concentration.Reference Matheson, Dunn and Smith 51 Crime rate is collected by the Centre for Research on Inner City Health at St. Michael’s Hospital and is expressed as a number of violent crimes per 100,000 people at risk. This variable will be used to describe neighbourhood safety. 52 The density of family physicians is collected by the Institute of Clinical and Evaluative Sciences and is expressed as a number of family physicians per 100,000 people. This will be used as a surrogate measure of an individual’s access to health care. 53
Table 1 Dimensions and census variables that make up the Ontario Marginalization Index.
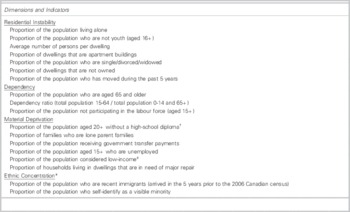
* Aboriginal indicators did not load on any of the factors
† For the 2006 index, the indicator is the proportion of the population ages 25+ without a certificate, diploma or degree. This is due to a change in the Statistics Canada definition
‡ “Low income” is defined as below the low income cutoff (LICO), a Statistics Canada measure that is adjusted for community size, family size, and inflation
Adapted from Matheson (Can J Public Health, 2012)Reference Matheson, Dunn and Smith 51
Each of the six neighbourhood variables will be converted from its continuous form into quintiles, where quintile one will represent a disadvantaged neighbourhood and quintile five will represent an advantaged neighbourhood, to be consistent with previous literature that separates variables of interest by quintiles.Reference Sasson, Keirns and Smith 12 , Reference Ahn, Shin and Hwang 26 , Reference Matheson, Dunn and Smith 51 An analysis of variance (ANOVA) test will be used to ensure that each quintile is significantly different from one another across all variables.
Statistical analysis
Descriptive statistics will be used to assess the distribution of all variables. Continuous variables will be summarized as means and standard deviations, whereas categorical variables will be summarized as counts and percentages. The distribution of each continuous variable will be assessed for normality using graphical interpretation and the Shapiro-Wilk test.
Unadjusted bivariate analyses will be performed to assess for differences between the dependent and independent variables, using either a t-test for all continuous variables or an χ2 test for categorical variables. Model diagnostics will be performed on all models, and multicollinearity will be assessed using either the tolerance statistics or variance inflation factor (VIF). A tolerance of <0.4 or a VIF statistics of >2.5 would indicate multicollinearity.
Logistic regression analysis will determine relationships between the neighbourhood factors (in addition to the traditional Utstein variables) and the outcome measures. The regression model will adopt a hierarchical modelling approach using generalized estimating equations to capture variation within neighbourhoods as a random effect. Patients will be clustered based on census tract. This hierarchical approach also accounts for the lack of independence between variables, an assumption that would be violated if a single level modelling approach was used. Eight models will be analysed. One model (#1) will contain only the Utstein (or individual variables). Six models (#2–7) will include the Utstein variables and one neighbourhood factor. The final model (#8) will include the Utstein variables and all neighbourhood factors (Table 2). Odds ratios (ORs) (with 95% confidence intervals) will be used to display the effect size of each independent variable. All statistical analyses will be carried out using SAS 9.3 (SAS Institute, Cary, NC). A two-sided p-value of <0.05 will be considered statistically significant.
Table 2 The variables that will be included in the model.

✓ indicates variables included in logistic regression model
The Utstein variables include: age, gender, location of arrest, bystander witness status, bystander CPR, bystander AED, EMS response time interval, initial rhythm, advanced life support skill, and ROSC at ED arrival.
Receiver operating characteristics curves will be used to measure the model’s ability to discriminate between those with and without the outcome of interest (either survival-to-hospital discharge, a ROSC at ED arrival, or bystander CPR).Reference Cook 54 The area under the curve (AUC) will be used to determine the probability that a patient will be correctly classified based on the outcome. Discrimination will be calculated as ([AUC – 0.5]/0.5).
Choropleth maps
Visual maps will be created using ArcGIS 10 (ESRI Canada Limited, Toronto, ON) to illustrate spatial patterns in the data and assist in disseminating the study findings to the general public who may not be familiar with statistical methodology. These visual maps also serve to drive further analysis and help generate hypotheses for additional studies. Data will be exported from SAS into a Microsoft Excel (Redmond, WA) spreadsheet and subsequently imported into ArcGIS 10. Unadjusted choropleth maps will be created using census tract frequency counts for the outcome measures and by quintiles for neighbourhood factors. Each map will be set in the North American 1983 datum UTM zone 17N coordinate projection system.
Sample size
Because ROC Epistry–Cardiac Arrest is a prospective database, a power calculation will guide sample size calculations to define the smallest significant OR that could be detected, given the fixed sample size and outcome demographics. A 4-year period between April 2006 and March 2010 was used to derive an approximate sample size. An estimated 4,600 eligible patients have a home address in Toronto, of which approximately 18% had a ROSC at ED arrival, and 4.5% survived to hospital discharge. An estimated 5,100 eligible patients have a pickup address in Toronto, where approximately 40% received bystander CPR. Given these sample sizes, this study is powered to detect a significant OR of 1.48 or greater for survival-to-hospital discharge, an OR of 1.23 or greater for a ROSC at ED arrival, and an OR of 1.18 or greater for bystander CPR. All power calculations were carried out using PASS (Power Analysis and Sample Size [version 08.0.8], NCSS Statistical Software, Kaysville, UT).
Research ethics
Individual research ethics boards (REB) at all 37 destination hospitals within the catchment area approved the design and implementation of ROC Epistry–Cardiac Arrest.Reference Morrison, Nichol and Rea 28 An institutional REB at St. Michael’s Hospital provided approval for all retrospective studies using the ROC Epistry–Cardiac Arrest database. This study was also approved by the University of Toronto REB, which governs research performed by graduate students at academic hospitals associated with the University of Toronto.
Discussion
To our knowledge, this will be the first Canadian study to investigate both traditional and nontraditional factors for OHCA outcomes. Although this study will not directly change clinical practice, it will help advance the understanding of a public health concern that kills over 90% of Canadians who experience an OHCA. Provided that differences are observed, this study will also highlight the role of neighbourhood inequalities in explaining differences in survival. The results of this study will be of interest to resuscitation researchers, physicians, city planners, and policymakers because it may lead to the implementation of policy and procedures to optimize the delivery of care for specific neighbourhoods. It will also help decision makers plan future bystander CPR education programs and community-based intervention programs for areas with low rates of bystander CPR. Knowledge of neighbourhood risk factors for cardiac arrests and their association with population demographics could be helpful for treating and counseling individual patients, but also for planning EMS system response and community-wide health programs that will aid the largest number of citizens. It will also contribute to the existing health care system by identifying neighbourhoods that could potentially benefit from targeted policy and public health interventions. With collaboration between scientists, clinicians, policymakers, and elected city and health officials, there is the potential for improving individual and population health.
This study has many strengths. First, data will be extracted from a reputable, research quality registry of OHCA patients assessed by prehospital care providers.Reference Morrison, Nichol and Rea 28 This registry has been used to answer OHCA-related questions, which have been incorporated into the current American Heart Association guidelines.Reference Travers, Rea and Bobrow 5 The large sample size provides adequate power to detect small differences in outcomes. Second, the rigorous proposed analytic approach uses hierarchical modelling to account for patient and neighbourhood variables, and for patient clustering within neighbourhoods. Without the risk of multicollinearity, selecting a composite score will take into account the complex and multidimensional aspect of neighbourhood variables.Reference Braveman, Cubbin and Egerter 27 Third, previous research almost exclusively reported ORs, which is useful for highlighting associations between predictor variables and outcomes, but is limited for identifying the discriminative ability of the independent variables. Although identifying causal relationships are not possible with this current design, this study will be the first to use receiver operating characteristics curves as a quantitative measure of a variable’s discriminative ability for cardiac arrest outcomes. Furthermore, this study will demonstrate how GIS mapping technology could be adapted to explore a life-threatening public health concern. Its detailed methods section provides a step-by-step approach for using and adapting GIS technology to prehospital care. Combining cardiac arrest data with this technology provides a unique perspective about the association between locations and OHCA.
This study has some limitations. It relies on postal codes, UTM, or latitude/longitude to link patients with the neighbourhood factors. Location errors could result in misclassification, and then the patient would be linked to the incorrect census tract, which could introduce selection bias. An estimated 5% of cases will be excluded due to incomplete geographic information, which is consistent with previous literature that has excluded between 3% and 15% of eligible cases.Reference Vaillancourt, Lui and De Maio 10 – Reference Sasson, Keirns and Smith 12 , Reference Ahn, Shin and Hwang 26 There are limitations associated with using census data. Neighbourhood characteristics may not be generalizable to individuals within a given census tract. Missing or incorrect data and low frequency counts could also alter conclusions. Although census data have their own limitations, they are one of the only population level datasets available to researchers. To prevent bias, Census Canada does follow up with any incomplete or unanswered questionnaires and adjusts the data for households who do not return a questionnaire. 55
Conclusions
This paper highlights the methodology that will be used to evaluate the role of the neighbourhood as determinants of cardiac arrest outcomes, and whether those factors improve the discriminative ability of the Utstein variables.
Acknowledgements
The ROC is supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077865-University of Iowa, HL077866-Medical College of Wisconsin, HL077867University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael’s Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Hospital Research Institute, HL077887-University of Texas SW Medical Center/Dallas, HL077908-University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR)—Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, and the American Heart Association. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health.
Competing interests: JEB holds a Jumpstart Resuscitation Master’s Studentship from the Canadian Heart and Stroke Foundation. LJM is a U.S. National Institute of Health, Canadian Institute of Health Research, and Heart and Stroke Canada funded investigator within the Resuscitation Outcomes Consortium. She is a past chair and current member of the Science Subcommittee of Emergency Cardiac Care Committee of the American Heart Association and on the editorial board of the 2010 guidelines in resuscitation as the co-chair of the International Liaison Committee of Resuscitation Advance Life Support Taskforce in 2010 and current past chair of the ALS Taskforce for ILCOR 2015. She is the past chair of the Research and Policy Planning Advisory Committee and past board of directors member for Heart and Stroke Canada. The remaining authors have no competing interests relevant to this topic.
Authors’ contributions: JEB conceived and designed the study under guidance from KSA, JGR, AK, PG, PD, and LJM. LJM oversaw data collection. JEB and LJM obtained ethics approval. JEB will be responsible for analysis and interpretation of the data under guidance from JGR, AK, and LJM. JEB and KSA drafted the manuscript, and all authors revised it for critically important intellectual content and approved the final version.





