Introduction
Populations are aging. In Canada, 14.1% of the population is aged 65 years or older. This is expected to accelerate over the next 20 years.Reference Milan 1 Population aging is of considerable concern for emergency medical services (EMS), as older adults tend to use emergency services at disproportionately higher rates compared with younger age groups.Reference Aminzadeh and Dalziel 2 - Reference Shah, Bazarian and Lerner 4 In a national sample (United States data), 38% of older adults seen in the emergency department (ED) arrived by EMS.Reference Shah, Bazarian and Lerner 4 The disproportionately higher EMS usage rate among older adults is well documented in other countries, including Australia and Turkey,Reference Shah, Bazarian and Lerner 4 - Reference Keskinoglu, Sofuoglu and Ozmen 6 and is notably highest in the oldest age group (>85 years), a rapidly growing segment of society.Reference Lowthian, Jolley and Curtis 7
EMS utilization rates have been studied in relation to a number of factors, including age, socio-demographic characteristics, and insurance status.Reference McConnell and Wilson 3 , Reference Meisel, Pines and Polsky 8 EMS use for older adults is higher in urban centersReference McConnell and Wilson 3 , Reference Lowthian, Jolley and Curtis 7 and among those with lower socio-economic status (United States data).Reference Svenson 9 The relationship between gender and transport rates is mixed, with women having higher overall rates of transport, whereas repeated transports were higher in men.Reference Svenson 9 , Reference Tangherlini, Pletcher and Covec 10
Non-transports are an important part of EMS demand and the risks associated with no transport are potentially high.Reference Moss, Chan and Buchanan 11 However, in some EMS systems, non-transport rates are often difficult to quantify or understand due to limited data.Reference Shah, Bazarian and Lerner 4
Despite the numerous studies on EMS use by the elderly, there appears to be little research exploring this topic in Canada. Our objective, therefore, was to quantify the rate of EMS use by older adults in a provincial EMS system, including both transport to the ED and non-transports.
Methods
Ethics
The Nova Scotia (NS) Capital District Health Authority research ethics committee approved this study (CDHA-RS/2012-248).
Study design
We analyzed data from the NS provincial EMS administrative database that includes electronic Patient Care Record (ePCR) data for each patient.
Setting
In 2010, the Nova Scotia (NS) population was 942,506 people, of whom 51.5% (485,017) were female and 16% (151,160) were ≥65 years old.Reference Milan 1 , 12 The population of NS is served by Emergency Health Services (EHS), a provincial EMS system and the sole provider of emergency and transfer services in the province. EHS provides single access to the EMS system, centralized computer-aided dispatch, standards for response times, and medical oversight. 13 The ground ambulance service is staffed with primary, intermediate, and advanced care paramedics covering an area of 55,000 square kilometers. 13 EHS receives approximately 120,000 to 130,000 requests for service per year, with close to half of requests being inter-facility transfers, resulting in over 100,000 patient transports per year. During the time frame of interest, a user fee was charged for all emergency responses.
Data collection
EHS requires that paramedics document all responses in an ePCR for which they have been dispatched, including transported and non-transported patients. Personal and clinical characteristics are documented along with operational details, including provider level and response time intervals. Each response is assigned a unique identifier generated from the computer-aided dispatch system. Once the ePCR is finalized, it is uploaded to a central server and stored in the EHS administrative database.
We requested data from EHS on all EMS emergency responses for older people (≥65 years) between January 1, 2010 and December 31, 2010. Data included the dispatch problem and response times. Demographic data included the patient’s age, sex, and location by postal code. We categorized location as urban or rural by using the postal code, where the second digit indicates an urban (1-9) or rural (0) address. We requested clinical information consisting of the paramedic’s clinical impression, the first documented Canadian Triage and Acuity Scale (CTAS) score, co-morbidity count, medication count, and number of interventions. Transport data included call disposition (transport to ED or no transport).
We included both community-dwelling older adults and residents of extended care facilities. We excluded air ambulance responses, inter-facility transfers or other scheduled responses (e.g., return to residence from the hospital).
Data analysis
We stored all data in Microsoft Excel 2007 (Redwood, CA) and conducted all statistical analyses using SPSS version 15.0 (Chicago, IL). Baseline characteristics are reported for those ≥65 years old, as this was the focus of our analysis. We reported EMS response and transport rates as per 1,000 population. We calculated the overall rate of EMS use for younger adults (16 to 64 years old) for comparison with no additional analyses performed with this cohort. We conducted chi-square tests to compare categorical variables between transported and non-transported in older adults only. Similarly, we applied independent t-tests to detect differences between continuous variables. We reported the level of significance using a pre-specified cutoff of alpha equal to 0.05 for the first test for each of the two comparison categories.
Results
There were 63,076 emergency responses (excluding inter-facility transfers) for adults in 2010, and 48.6% of these were for the 16% of the population ≥65 years old (Figure 1). The mean age of the older group was 79.9±8.5 years (median 80; IQR 73-86), 57.3% were women and 47.9% were from an urban location. Most (39.7%) were triaged as CTAS 3 and almost half had no intervention (Table 1).
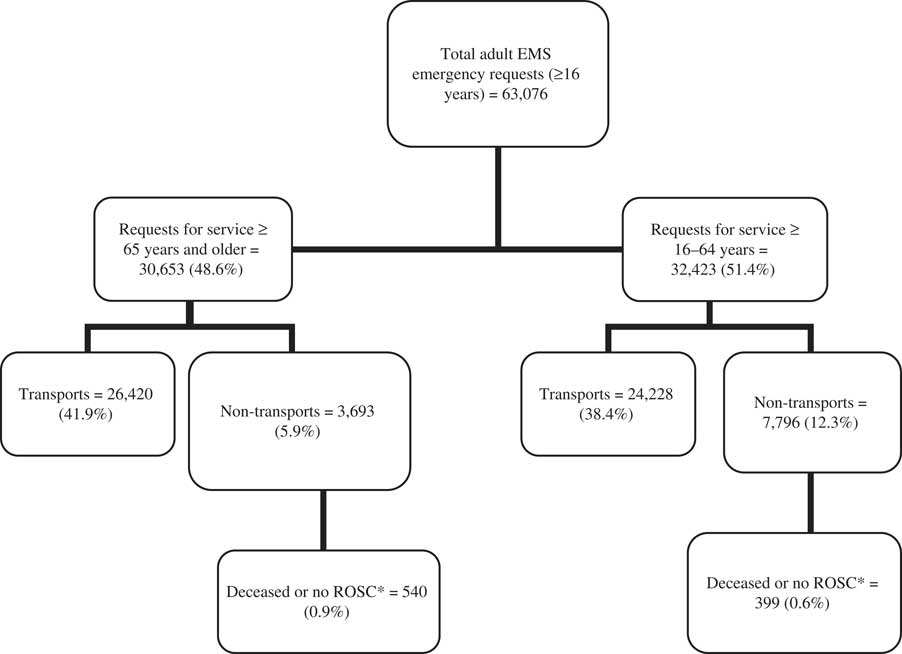
Figure 1 All adult ground ambulance emergency responses in Nova Scotia in 2010. *ROSC = Return of Spontaneous Circulation.
Table 1 Baseline characteristics of older adults (≥65 years)

* MI=myocardial infarction, TIA=transient ischemic attack, CHF=congestive heart failure, COPD=chronic obstructive pulmonary disease.
** CTAS=Canadian Triage and Acuity Score.
Response, transport rates, and non-transport rates per 1,000 were all higher in the older population and again in the oldest of the old (≥85 years) (Table 2).
Table 2 Comparison of response and transport rates by age group

* The denominators were derived from Canada population estimates (2010) 12 : 651,475 (16–64 years), 130,507 (65–84 years), 20,653 (≥85 years).
A comparison of the characteristics of older adults by transport decision shows that those patients not transported were more commonly female and had lower acuity (e.g., CTAS 5). The most common presenting complaint for both transported (n=3,701) and non-transported patients (n=1,177) was fall. Common clinical impressions of transported patients included cardiovascular (n=3,607; 13.7%), respiratory (3,563; 13.5%), trauma (4,197; 15.9%), and gastrointestinal (3,541; 13.4%) complaints. The most common clinical impression identified for non-transported patients was wellness check/no complaint (n=1,534; 41.5%). The average on-scene time for non-transport patients, however, was significantly longer than those who were transported but with significantly fewer interventions performed (Table 3).
Table 3 Characteristics of older patients by transport decision.

* Values indicate mean and standard deviation unless indicated otherwise.
Discussion
To our knowledge, this is the first Canadian EMS study to quantify the rate of EMS use by older adults, including both transport to the ED and non-transports. In this Canadian provincial EMS system, the EMS utilization rate for older adults was found to be comparable to other developed countries: 202.8 responses per 1,000 population versus 167 per 1,000 (United States data)Reference Shah, Bazarian and Lerner 4 and 211.2 per 1,000 (Australia data) Reference Lowthian, Jolley and Curtis 7 . Also, age has been noted to be the major determinant of EMS useReference Svenson 9 and EMS use is the highest in the oldest of the old with transport rates greater than 470 per 1,000Reference Clark and FitzGerald 5 , Reference Lowthian, Jolley and Curtis 7 , which we also confirmed in our study, with a transport rate 4.5 times higher for older adults compared to younger adults.
Given that the aging population will place a greater demand on EMS systems and that it is unlikely that EMS budgets will increase at the same rate to meet those demands, there is a growing need to improve EMS system efficiency and effectiveness, or to better define alternatives to EMS transport. To that end, our study extends the knowledge of previous work by quantifying the non-transport rate, a measure often missed in other analyses.Reference Shah, Bazarian and Lerner 4 We showed that non-transports accounted for 12% of the older adult call volume. This represents a significant utilization of EMS resources, as these calls had a 30% longer on-scene time than transport, during which EMS availability is reduced to the service area without any obvious benefit to the patient. We also found that 23% of our study population were triaged by EMS as CTAS 4 or 5, i.e., seemingly minor complaints, and that EMS provided no interventions for 38.4% of transported patients. While we did not follow these lower acuity CTAS 4 and 5 patients to determine if they needed ED management, all three groups (lower acuity CTAS 4, 5 and the no intervention group) might be more effectively managed by modified or even non-EMS systems.
In NS, provincial emergency care is aiming to provide better care for older adults through improved assessment and efficient care that is congruent with the patient’s care goalsReference Ross 14 , Reference Jensen, Travers and Bardua 15 and also to align EMS with integrated networks of emergency care to improve care continuity.Reference Martinez and Carr 16 There is a movement towards expanded-scope EMS, where increased emergency or primary care is delivered onsite, thereby avoiding transport to the ED.Reference Mason, Knowles and Colwell 17 - Reference Arendts and Sim Johnston 19 Other innovative ideas of managing low-priority EMS calls include secondary telephone triageReference Eastwood, Morgans and Smith 20 , paramedic referral servicesReference Newton, Tunn and Moses 21 , and community paramedic modelsReference Mason, Knowles and Colwell 17 . Either individually or in combinations, the implementation of such innovative programs can allow for EMS services to adapt to the changing health care needs of the population.
Limitations
There are limitations associated with the use of administrative data. Even so, there were no missing data for age (it is a mandatory field for paramedics to complete). There were a few cases where sex (n=25, <0.1%) or the transport decision (n=106 cases, <0.1%) were missing. The accuracy of the paramedic-documented CTAS was not validated, so it is possible that severity was under-estimated. Whether CTAS is a valid measure of illness severity in the non-transported patient should be evaluated further. Unfortunately, postal codes were missing for 6,903 cases (22.5%), precluding analysis. The ePCR data are not linked to hospital records, so patient outcomes were not known. This analysis looked at one calendar year of EMS use, so it is possible that the results may have been affected by conditions that were unique to that year, but to our knowledge this was not the case.
Conclusions
We confirmed that older adults use EMS services at higher rates than younger populations, and that this increases with age and is consistent with other industrialized populations. We also found that the low-priority and non-transport calls by older adults consumed considerable resources in this provincial system. Hence, these might be the areas most malleable to the innovative changes that are needed to meet the challenges facing EMS systems.
Acknowledgments
We would like to express our gratitude to the EHS Operations Management IT services for data query.
Competing Interests: J. Goldstein was supported by a student research award from the Nova Scotia Health Research Foundation and funding from the Atlantic Regional Training Center. No other competing interests were reported.






