CLINICIAN'S CAPSULE
What is known about the topic?
In traumatically injured patients, excessive blood loss necessitating the transfusion of red blood cell units is common.
What did this study ask?
What is the association between pre-hospital hypothermia (<36°C) and transfusion risk within 24 hours after hospital arrival for traumatic injury?
What did this study find?
This cohort study highlighted that hypothermia was associated with a 68% increased odds of a red blood cell transfusion.
Why does this study matter to clinicians?
Hypothermia may be an early indication of transfusion risk and may highlight the need for early interventions to mitigate a temperature decrease.
INTRODUCTION
In both Canada and the United States, trauma remains the leading cause of death in individuals aged 1 to 34 years and is among the top five leading causes of death nationwide for patients of all ages.Reference Mack, Clapperton and Macpherson1 Uncontrolled hemorrhage represents the leading cause of preventable death among these patients.Reference Mack, Clapperton and Macpherson1
Traditionally, the management of bleeding patients in the pre-hospital setting has been aggressive resuscitation with isotonic fluid to maintain tissue perfusion. However, this therapy may contribute to worsening coagulopathy, cellular injury, and bleeding.Reference Cheung, To and Chan2 As a result, “damage control resuscitation” has become the standard of care in the management of trauma patients. Damage control resuscitation allows physicians to integrate hemostatic resuscitation, permissive hypotension, and damage control surgery to prevent coagulopathy until definitive treatment is made available.Reference Lamb, MacGoey, Navarro and Brooks3 Implementing components of damage control resuscitation in the pre-hospital setting has shown to have clinical benefit.Reference Morrison, Carrick and Norman4 Nevertheless, pre-hospital providers are limited in the care they can provide. The definitive management of massive hemorrhage in trauma patients is surgical control of the bleeding site,Reference Holcomb5 yet most deaths from bleeding occur on route to the hospital or soon after admission.Reference Sauaia, Moore and Moore6,Reference Heckbert, Vedder and Hoffman7 Therefore, finding solutions to modify the risk of hemorrhagic death, particularly among patients requiring surgical intervention, is critical.
One such solution is the prevention of accidental hypothermia, defined as an unintentional reduction in patient temperature to <36°C that is associated with a higher risk of morbidity and mortality among trauma patients.Reference Jurkovich, Greiser, Luterman and Curreri8,Reference Dirkmann, Hanke, Görlinger and Peters9 Given that hypothermia impairs coagulation enzyme activity and decreases platelet aggregation and the availability of fibrinogen, it can further increase bleeding risk.Reference Beekley10,Reference Holcomb, Jenkins and Rhee11
While hypothermia is conceivable in all pre-hospital patients, it is highly prevalent among those with a traumatic injury.Reference Lapostolle, Couvreur and Koch12 The etiology of hypothermia is multifactorial, including heat loss because of environmental exposure, infusion of cold intravenous fluids, and hemorrhagic shock.Reference Søreide13 Patients requiring emergency surgery in trauma pose additional challenges for the maintenance of normothermia. For example, they may require referral to tertiary centres and, as a result, experience prolonged transportation and environmental heat loss. Similarly, patients having specific surgical procedures such as cavitary surgery may be at an increased risk for hypothermia because of heat loss from the open abdomen. Finally, the induction of anesthesia, in both trauma and surgical patients, directly affects thermoregulation and is an independent risk factor for hypothermia.Reference Matsukawa, Sessler and Sessler14–Reference Rajagopalan, Mascha, Na and Sessler16
In this study, we aimed to evaluate the independent association between pre-hospital hypothermia and transfusion as it has important clinical consequences for the pre-hospital setting. First, hypothermia can have deleterious effects on the cardiac, neurologic, renal, and respiratory systems.Reference Søreide13,Reference Perlman, Callum and Laflamme17 Therefore, evaluating its clinical utility beyond coagulopathy can help alert first responders early to communicate that these are individuals at high risk for transfusion. Second, reducing the severity and duration of hypothermia has been associated with an increased probability of successful resuscitation and reduced mortality in one, albeit small, prospective cohort of injured patients.Reference Gentilello, Jurkovich, Stark, Hassantash and O'Keefe18 Hence, it may inform the need for early rewarming strategies in the pre-hospital setting.
METHODS
Subjects and setting
Sunnybrook Health Sciences Centre (SHSC) is a Level 1 trauma centre that services a population of approximately 6 million. SHSC maintains a trauma registry that meets the standards of the National Trauma Data Standard. We performed an analysis using the trauma registry and identified all adults aged 18 years or older, presenting with admission for traumatic injury and emergent surgery between July 2010 and June 2014. Emergent surgery was defined as any procedure performed in an operating room and occurring within six hours of arrival in the trauma bay or emergency department (ED).Reference Alam, Olarte and Callum19
The following patients were excluded: 1) patients with thermal injuries, as they are treated through a different care pathway; 2) patients pronounced dead on arrival to the trauma bay or with an injury severity score of 75, as these are nonsurvivable injuriesReference Baker, O'Neill, Haddon and Long20; and 3) hyperthermic (>38.3°C) patients, as they may be at an increased risk of morbidity and mortality.Reference Wade, Salinas, Eastridge, McManus and Holcomb21 The research ethics board of SHSC reviewed this quality improvement project and advised that it did not require ethics approval.Reference Alam, Olarte and Callum19
Data collection and variable definitions
Clinical data were abstracted from patient charts by two research assistants independently and in duplicate using an a priori developed data extraction form. Demographic information and patient outcomes were obtained from the trauma registry.
Outcomes
The study outcome was the receipt of one or more units of RBC within 24 hours of admission in the trauma bay, operating room, or intensive care unit (ICU).
Exposure
The primary independent variable of interest was pre-hospital hypothermia, defined as core body temperature <36°C,Reference Peng and Bongard22 measured within 15 minutes of arrival to the trauma bay using a calibrated tympanic membrane temperature measurement.
Covariates
The a priori model developed to evaluate the association between hypothermia and RBC transfusion included covariates known to be associated with transfusion in trauma. First, the injury severity score, which quantifies trauma severity, was included as a continuous variable because of its strong correlation with morbidity in trauma patients. The injury severity score ranges from 1 to 75, for which a score >15 represents a major trauma.Reference Baker, O'Neill, Haddon and Long20 Given that we are a Level 1 trauma centre, our patients are often transferred from district hospitals and may be at an increased risk for transfusion because of the complexity of their injuries. Hence, we included this variable in the multivariable analysis.Reference Sampalis, Denis, Fréchette, Brown, Fleiszer and Mulder23 Vital signs measured within 15 minutes of arrival to the trauma bay, such as systolic blood pressure (mm Hg) and heart rate (beats per minute), used as early indicators of hemodynamic instability, were considered continuous variables.Reference Nunez, Voskresensky and Dossett24,Reference Mutschler, Nienaber and Münzberg25 Clinical markers of bleeding, such as baseline hemoglobin (Hb), coagulopathy (international normalized ratio [INR]), and acidosis (pH), measured within one hour of arrival to the trauma bay, were also considered continuous variables.Reference Lamb, MacGoey, Navarro and Brooks3,Reference Dirkmann, Hanke, Görlinger and Peters9
Missing data
Predictors with >10% missing data were excluded from further analysis. Furthermore, to evaluate the potential systematic exclusion of patients, those with missing temperature measurements in the trauma bay were compared with the cohort with complete data. A standardized difference (SD) between the included and missing cohorts has been reported (see Supplemental Appendix; Table 1), in which imbalance was defined as an absolute value of greater than 0.10. For variables with <10% missing data, contributing observations were excluded.
Statistical analysis
A univariable analysis was performed, stratified by temperature category, comparing predictors of RBC transfusion. Continuous, normally distributed variables were compared with Student's t-test, and for non-normally distributed variables, the Wilcoxon rank-sum test was used. Finally, comparisons of categorical variables were evaluated with the chi-square test.
To assess the relationship between hypothermia and transfusion risks, a multivariable logistic regression model was constructed. Variables were selected a priori and considered for inclusion if they were known to be associated with hypothermia, morbidity, or transfusion in trauma. To further evaluate the association between pre-hospital temperature and transfusion, the pre-hospital temperature was included in the model as a continuous variable in a post hoc sensitivity analysis.
All analyses were conducted using SAS statistical software (University Edition, Version 9.4, SAS Institute Inc, Care, NC).
RESULTS
Data inspection and review
A total of 1,546 patients admitted between July 01, 2010, and June 30, 2014, met our inclusion criteria (Figure 1). A sample of 1,448 (94%) individuals remained after patients with data absent for these variables were excluded. Variables that had >10% missing values in this cohort (pH and lactate) were excluded from the analysis. The exposure of interest, baseline temperature, was not measured in 745 patients (51%). While these patients were excluded to facilitate analysis of the data, their characteristics were comparable with the included cohort (see Supplemental Table 1).

Figure 1. STROBE patient flow diagram (TB = trauma bay).
Description of cohort
A total of 703 patients (median age [interquartile range, IQR], 40 [27–55]; 77.5% male) who presented to the SHSC trauma bay were included to evaluate the association between hypothermia and transfusion (Table 1). The incidence of hypothermia was 51% (n = 356); 18% (n = 128) were <35°C, 5% (n = 32) were <34°C, and 0.3% (n = 2) were <33°C.
Table 1. Clinical characteristics of the hypothermic and normothermic trauma patients requiring emergency surgery

ISS = injury severity score; INR = international normalized ratio; IQR = interquartile range; RBC = red blood cells; SD = standard deviation; u = units.
*Comparison between hypothermic and normothermic patients.
†Wilcoxon rank-sum test.
‡t-test.
+Chi-square test.
Rates of transfusion of blood products
The incidence of transfusion within 24 hours for the overall cohort was 29% (n = 203), with 37% (n = 131) in the hypothermia group and 21% (n = 72) in the normothermia group (p < 0.001). The proportion of hypothermic patients compared with that of normothermic patients requiring platelets (14.0% v. 4.0%, respectively; p value < 0.001), frozen plasma (18.5% v. 4.0%, respectively; p value < 0.001), and cryoprecipitate (9.5% v. 2.9%, respectively; p value < 0.001) were significantly higher. Moreover, 12% (n = 42) of hypothermic patients required >6 units of RBCs compared with 2% (n = 8) of patients in the normothermic group (p < 0.001).
The median length of stay in the hypothermic and normothermic cohorts was 12 days and 10 days, respectively (p < 0.001). The proportion of patients who died during the hospitalization was higher in the hypothermic than normothermic cohorts (7.5% v. 3.8%, respectively; p = 0.03).
Association between hypothermia and transfusion
Results of the unadjusted analysis are summarized in Table 2. Hypothermia was associated with a 2.22 fold increased odds of transfusion of RBCs (95% confidence interval [CI] 1.58–3.11). After adjusting for available confounders including age, sex, coagulopathy (INR and platelets), referral status, vital signs (blood pressure and heart rate), and injury severity score, we found that hypothermia was associated with a 68% increase in the odds of transfusion within 24 hours (adjusted odds ratio [OR] 1.68; 95% CI 1.06–2.56; Table 3). Furthermore, in a subsequent sensitivity analysis, we found that each 1°C reduction in temperature was associated with a 30% increase in the odds of transfusion within 24 hours (adjusted OR 1.30; 95% CI 1.06–1.60; Appendix Table 2).
Table 2. Univariable predictors of transfusion (≥1 RBC in the first 24 hours) in a cohort of trauma patients requiring emergency surgery
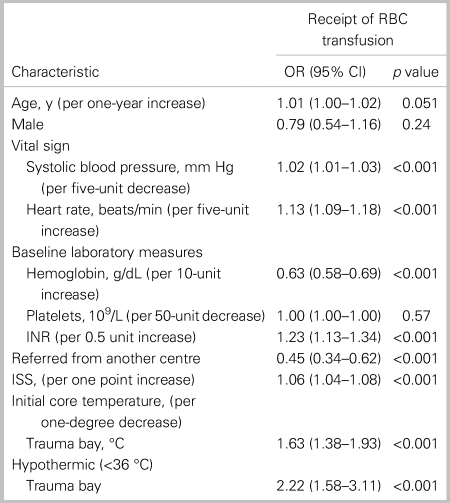
Abbreviations: CI = confidence interval; INR = international normalized ratio; ISS = injury severity score; OR = odds ratio; RBC = red blood cell.
Table 3. A multivariable model of the association between hypothermia and transfusion among trauma patients requiring emergency surgery

Abbreviations: CI = confidence interval; ISS = injury severity score; OR = odds ratio.
No variables were found to be collinear.
Omnibus likelihood ratio (chi-square [df], p value) 232.79 (10), p value <0.001; c-statistic: 0.84.
DISCUSSION
This study aimed to evaluate the independent association between pre-hospital hypothermia and transfusion of RBCs among trauma patients. As hypothermic patients had an associated 68% increased odds of an RBC transfusion, we showed that hypothermia is an important early physiologic measure for RBC transfusion in trauma. Hypothermic patients were also noted to have a greater length of stay and mortality.
The incidence of hypothermia in our cohort was 51% which, albeit high, is consistent with other studies where the incidence of hypothermia ranges from 17% to 54%.Reference Bukur, Hadjibashi and Ley26,Reference Klauke, Gräff and Fleischer27 While there is a widespread understanding that hypothermia may be associated with poor outcomes in trauma, it remains a commonly observed phenomenon suggesting potential room for improvement in care.
While hypothermia was associated with an increased transfusion of RBCs, these patients were also more likely to receive other blood products including platelets, frozen plasma, and cryoprecipitate. Approximately one-third of patients in our study required at least one unit of RBCs. Como et al. showed that the transfusion rate among direct from scene trauma patients presenting to the University of Maryland's trauma centre was approximately 10%.Reference Como, Dutton, Scalea, Edelman and Hess28 Our rate was higher as all patients in the cohort required emergency surgery, indicating an increased need for vigilance in this population. Hypothermia was the strongest predictor of transfusion in our study cohort that continues to be seen in a variety of clinical and research settings. In another study of over 15,000 trauma patients presenting to an ED, hypothermia was associated with a two-fold increased risk of transfusion of RBC.Reference Klauke, Gräff and Fleischer27 They identified that an increasing injury severity score was also associated with a transfusion risk. However, injury severity score is often calculated much later as the trauma evolves, requiring diagnostic information from radiography. While it is an important confounder in the relationship between hypothermia and outcome, it may not be a useful clinical indicator of transfusion given the complexity of its calculation.
We also demonstrated that hypothermia was associated with transfusion independent of coagulopathy. Patients may be transfused RBCs in response to the unpredictable hemodynamic, rather than coagulopathic, effects of hypothermia in trauma. The effect of hypothermia on cardiac output and contractility is highly dependent on the severity of hypothermia, volume status, and level of sedation.Reference Polderman29 In normovolemic patients, severe hypothermia reduces cardiac contractility, increases the risk of arrhythmia, and induces hypovolemia because of cold diuresis.Reference Tveita, Ytrehus, Myhre and Hevroy30,Reference Sun, Zhang and Cade31 Therefore, the body's physiologic response to reductions in core temperature contrasts the normal physiologic response to hypovolemia in the polytrauma patient, namely a rise in heart rate with a corresponding initial increase in cardiac output.Reference Vardon, Mrozek, Geeraerts and Fourcade32 For example, in a rat model of trauma and hemorrhage, animals that were maintained hypothermic (32°) during resuscitation had reduced cardiac output relative to those who were restored to normothermia during resuscitation.Reference Mizushima, Wang, Cioffi, Bland and Chaudry33 Similarly, in a porcine model, shock and hypothermia were shown to be additive. A decrease in cardiac output persisted in hypothermic animals, despite controlling bleeding and infusing volume expanders.Reference Krause, Howells and Buhs34 As advanced trauma life support (ATLS) guidelines suggest the treatment of hemorrhagic shock and reduced cardiac output with blood products, it is possible that we are also transfusing in response to the cardiac effects of hypothermia.Reference Subcommittee35 Our study is an important addition to the literature and further suggests the need for research into this area to evaluate the mechanism behind this association and the impact of warming interventions.
These findings are significant for the pre-hospital setting for two reasons. First, information regarding coagulopathy is often unavailable in the pre-hospital setting or is gathered late while managing severe hemorrhage. For example, in our institution, blood is drawn within 15 minutes, transported to the laboratory in 5 minutes, and analyzed within 20 minutes; hence, actionable lab results take at least 40 minutes to become available after patient arrival. Hypothermia represents a potentially useful early indicator of transfusion requirements. Second, and more importantly, clinicians tend to rely on platelets and INR as clinical endpoints for the management of coagulopathy. However, our work indicates that despite correction of coagulopathy, hypothermia is likely still a clinical indicator of transfusion requirements and may need to be “resuscitated.”
Resuscitating hypothermia in the pre-hospital setting
Our study did not assess the impact of hypothermia management on RBC transfusion, and there are no other randomized patient studies that evaluate the effect the pre-hospital temperature management on transfusion. However, we propose that resuscitating hypothermia represents an opportunity to improve the quality of care in the pre-hospital setting. A recent review highlights the considerable laboratory evidence for the management of hypothermia,Reference Haverkamp, Giesbrecht and Tan36 and a second review has proposed an early goal-directed approach to hypothermia, stressing the importance of “prevention first and treatment second.”Reference Perlman, Callum and Laflamme17 While pre-hospital providers should prioritize the management of life-threatening injuries, a variety of interventions can be performed to resuscitate a temperature less than 36°C aggressively. These patients should be passively warmed by removing any cold or wet clothing and placing them in a wrap that should include insulation, vapour protection, and, ideally, a heat source.Reference Henriksson, Lundgren and Kuklane37 In patients with moderate to severe hypothermia, namely a temperature less than 32°C, active rewarming is necessary, particularly if patients cannot generate endogenous heat from shivering.Reference Oliver, Brierley, Raymond-Barker, Dolci and Walsh38 Effective rewarming modalities include chemical heat packs, hot water bags, electrical heating blankets, or forced warm air.Reference Haverkamp, Giesbrecht and Tan36 Furthermore, while only limited fluids are usually provided in the pre-hospital setting, providers should ensure that infused fluids are warmed, with the avoidance of overzealous use of crystalloid. Finally, emergency medical services (EMS) should notify the receiving hospital to plan for active warming and the increased likelihood of transfusion in these patients.
Limitations
As this was an analysis of a trauma registry, data were limited to only specific risk factors that were measured at the time of collection. Therefore, it was difficult to incorporate other potential confounders such as lactate or acidosis into our models. Similarly, this study was unable to measure diagnoses or interventions that may alter temperature regulation. Furthermore, as this data were representative of only one trauma centre, the results may not apply to another trauma centre. We also concede that over 50% of our patients had missing values for temperature. While we demonstrated that these groups were largely similar on measured characteristics, it is still possible that the excluded patients were systematically different than those who were included in our study. The lack of consistent temperature monitoring is an important finding and calls for innovation in temperature monitoring to overcome the measurement challenges. Nevertheless, we find that both the missing and included patients were similar on measured variables. Finally, it is unclear whether hypothermia may directly increase transfusion requirements or whether it is merely a sign of a more severely injured trauma patient who requires transfusion.
Conclusion
In summary, this single-centre cohort study suggests that pre-hospital hypothermia is independently associated with RBC transfusion in the first 24 hours of arrival in trauma. This work highlights an opportunity to manage and resuscitate hypothermia actively in the trauma setting. Future research should focus on effective monitoring technologies, warming prevention, and management both in the pre-hospital and hospital settings. Prospective randomized controlled trials evaluating whether these warming strategies improve patient morbidity, mortality, and transfusion risk are warranted and will be critical for any health care practitioner involved in trauma care.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.412.
Acknowledgements
Naheed Jivraj: literature search, study design, data analysis, data interpretation, and writing. Lilia Kaustov, PhD: literature search, data interpretation, and critical revision. Kennedy Ning Hao, BHSc: data analysis, data interpretation, and writing. Rachel Strauss, BSc: data collection. Jeannie Callum, MD: study design, data interpretation, writing, and critical revision. Homer Tien, MD: study design. Asim Alam, MD: study design, data collection, data interpretation, writing, and critical revision.
Competing interests
AA receives consulting fees from Medtronic and Zoll. The remaining authors declare that they have no competing interests.






