Introduction
The association between migraine and alcohol consumption continues to generate mixed and unclear results. In the Head-HUNT study from Norway, an association was found between increased alcohol consumption and migraine while in a Danish population study, the risk of migraine with aura was reduced in patients with weekly alcohol consumption. Reference Aamodt, Stovner, Hagen, Bråthen and Zwart1,Reference Le, Tfelt-Hansen, Skytthe, Kyvik and Olesen2 In a 12-month prevalence of alcohol dependence, rates were similar between patients with migraine and those without. Reference Jette, Pattern and Williams3
The reasons for potentially decreased alcohol consumption stem from widely held beliefs that alcohol can trigger or exacerbate migraine, with one study reporting that 35.6% of its 2197 participants noted alcoholic beverages to be a “trigger” of migraine, with red wine being most commonly implicated. Reference Onderwater, Van Oosterhout, Schoonman, Ferrari and Terwindt4 A 2022 prospective study conversely suggested that there was no significant effect on the likelihood of a migraine attack in the 24 hours after drinking, and a slightly lower chance from 24 to 48 hours after ingestion. Reference Vives-Mestres, Casanova, Puig, Ginebra and Rosen5 A 2020 prospective study showed that in adults with episodic migraine, ingestion of five or more drinks was associated with a twofold increase in headache the next day but there was no increase with one to two drinks. Reference Mostofsky, Bertisch and Vgontzas6 More recently, a 2023 meta-analysis incorporating 22 studies suggested that alcohol consumption and migraine are inversely correlated but such a study utilized a heterogenous group of patients. Reference Błaszczyk, Straburzyński and Więckiewicz7
Within the migraine population, it is also unclear what factors could potentially affect the risk of alcohol consumption for patients with migraine. The National Comorbidity Survey Replication (NCSR) found that the odds ratio for 12-month prevalence of alcohol use disorder was not higher for patients with chronic daily headache relative to those without headache, after demographics were controlled for, suggesting this was possibly due to comorbid post-traumatic stress disorder or depression. Reference Peterlin, Rosso, Sheftell, Libon, Mossey and Merikangas8 Similarly, the previous literature has suggested a strong relationship between depression, anxiety, post-traumatic stress disorder, and alcohol use disorder. Reference Castillo-Carniglia, Keyes, Hasin and Cerdá9
We sought to build on these studies by assessing the association between chronic migraine and alcohol use disorder relative to chronic disease controls and to analyze the impact of comorbid depression, anxiety, and post-traumatic stress disorder on this association.
Methods
All data were obtained through the Stanford Research Repository (STARR) and approved by the Stanford Institutional Review Board. Cohorts for assessment were built on different criteria for each but were drawn from the baseline group of patients seen in the Stanford Headache Clinic of the Department of Neurology, a tertiary headache center, or the Pain Management Clinic in the Department of Anesthesia between January 1, 2017 and December 31, 2019, and were older than 18 at the time of visit. Demographics for each group were determined include sex, race, ethnicity, and average age.
Patient groups were then built based on one of these International Classification of Disease, Tenth Edition (ICD-10) codes that were assigned during the observed time period: G43.7 chronic migraine; M54.5 low back pain; E11 type 2 diabetes mellitus (T2DM). Low Back Pain served as a non-headache chronic pain control. T2DM acted as the chronic non-pain condition control. Subgroups were then built for these disease states based on the presence or absence of: F32 Depressive episode or F33 Major depressive disorder, recurrent; F41 Other anxiety disorders; F43.1 Post-traumatic stress disorder.
Smaller subgroups were then built to include patients meeting these previous criteria and ever receiving a diagnosis of alcohol use disorder stemming from the ICD-10 codes: F10.1 Alcohol Abuse or F10.2 Alcohol Dependence.
The primary outcome was the odds ratio for alcohol use disorder in patients with chronic migraine or with chronic migraine and additional factors relative to controls. Secondary outcomes included differences in demographics between these groups including sex, race, ethnicity, and age. This is the primary analysis of this data.
Statistical Analysis
All data were analyzed in Microsoft Excel. Descriptive statistics were used to assess for demographics of each cohort. Due to the small number, or absence of patients entirely, in certain disease and demographic combinations, tests for statistical significance were not conducted for race and ethnicity. Odds ratios with 95% confidence intervals were used to assess for differences in rates of alcohol use disorder between groups. A two-sided, students T-test was used to assess for statistically significant differences in ages between groups. Statistical significance was set at p < 0.05.
Results
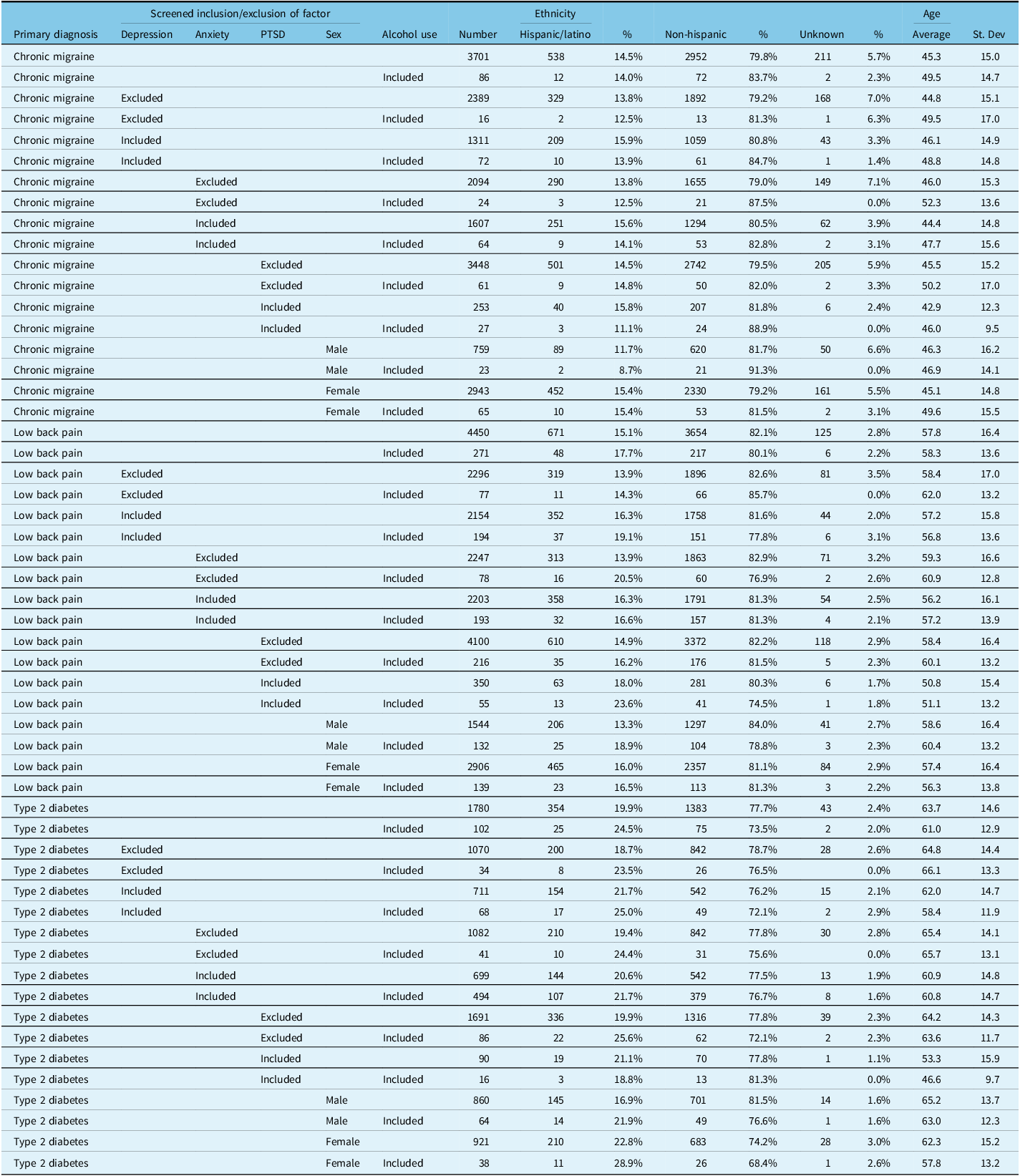
A total of 3701 patients with chronic migraine, 4450 patients with low back pain, and 1780 patients with type 2 diabetes mellitus met inclusion criteria. The full demographics of each cohort are available in Table 1, Table 2, and Table 3. In patients with chronic migraine, male sex was not associated with a higher risk of alcohol use disorder relative to women (OR 1.38; 95% CI: 0.87–2.21, p = 0.173). When looking at men and women with chronic migraine, separately, relative to their controls of male or female patients with LBP or T2DM, respectively, the risk of alcohol use disorder was statistically significantly lower in those with chronic migraine relative to the comparators (Fig. 1a,b). A portion of the subsets of patients with alcohol use disorder and chronic migraine, with or without additional factors, were statistically significantly older than the cohort-at-large (4/9 with an average age difference of + 5.1 ± 0.9 years). Fewer of the subset of patients with alcohol use disorder and LBP, with or without additional factors, had statistically significant age differences (2/9 with an average age difference of + 2.6 ± 1.4 years). This is in contrast to the patients with alcohol use disorder and T2DM, with or without additional factors, in whom the age difference relative to the cohorts-at-large, was younger (3/9 with an average age difference of −2.7 ± 2.3 years).
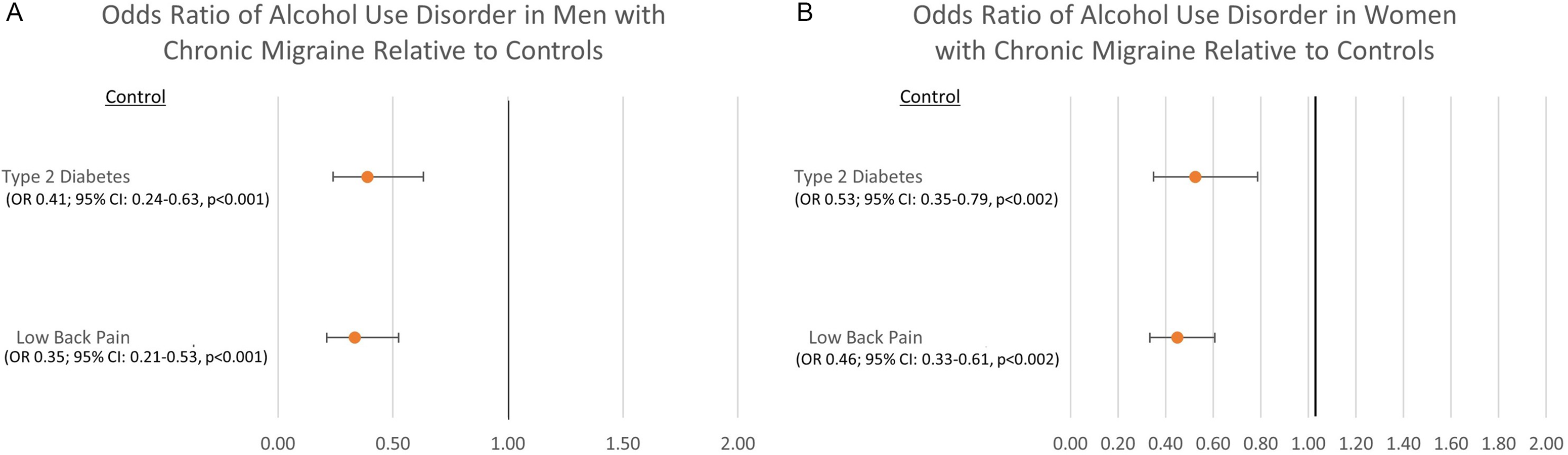
Figure 1: Odds ratio of alcohol use disorder in patients with chronic migraine relative to controls by sex: 1a. Men. 1b. Women.
Table 1: Sex for each group
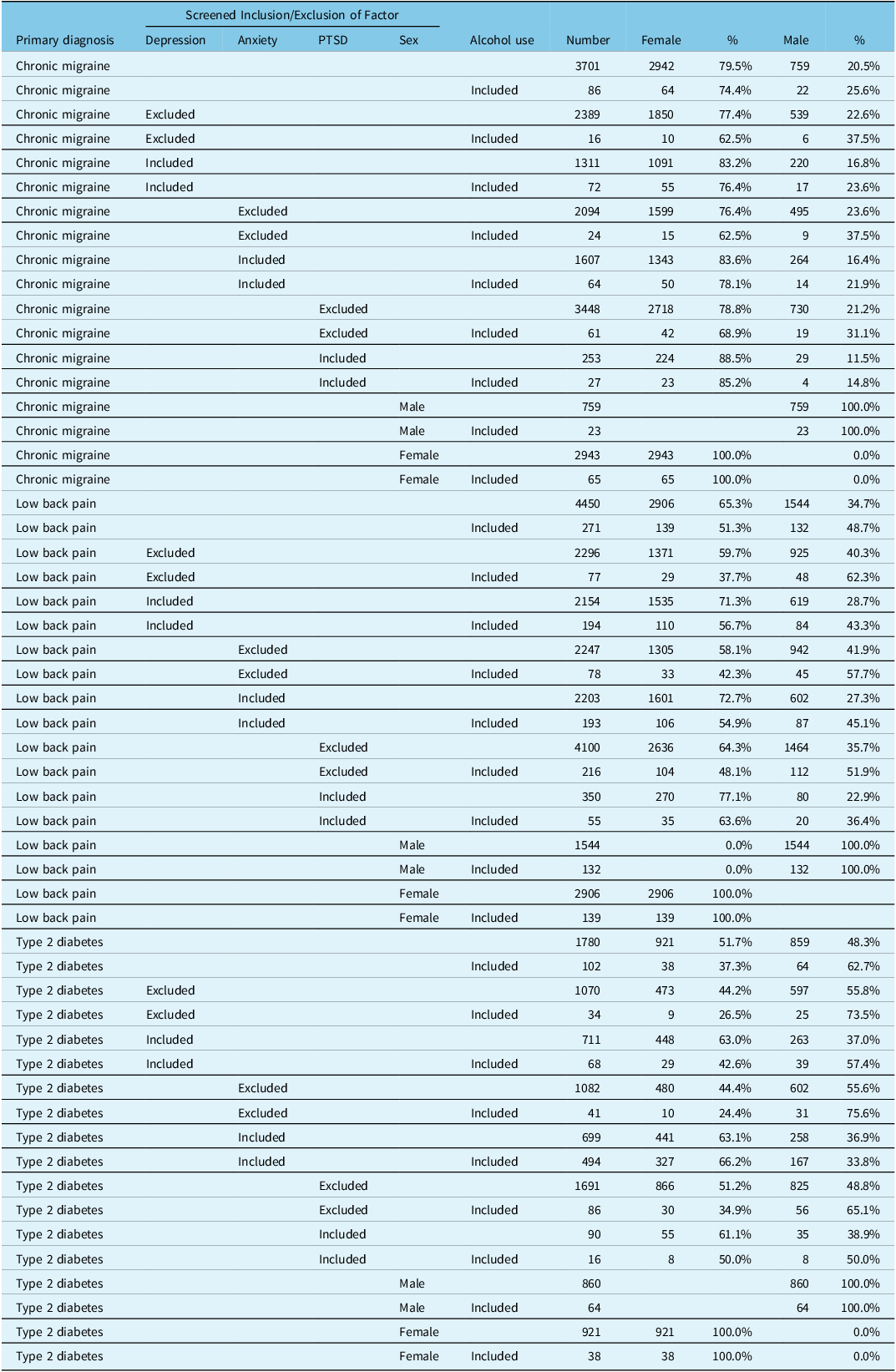
Table 2: Racial demographics for each group
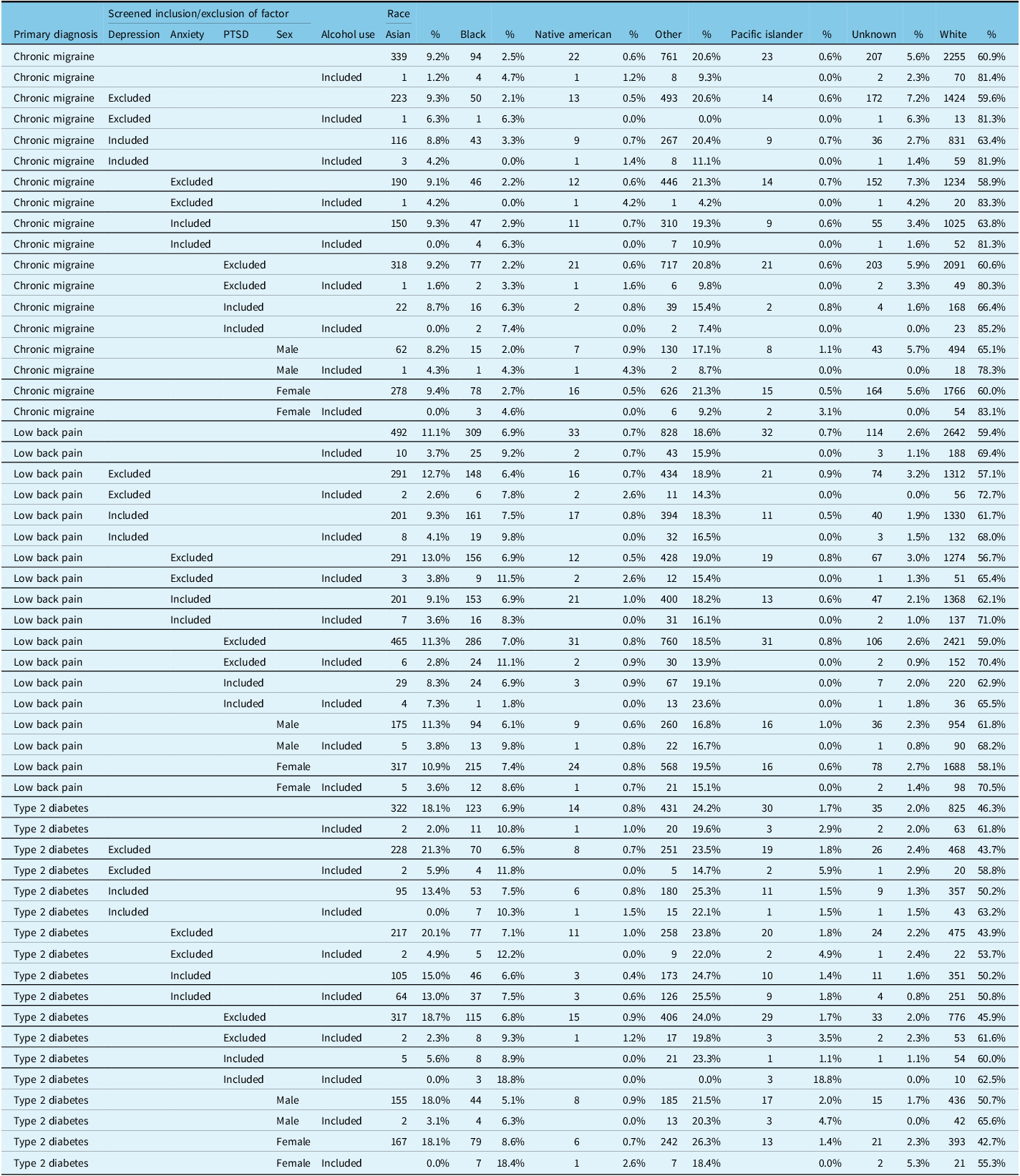
Table 3: Ethnicity demographics and age for each group
Patients with chronic migraine had a lower risk of alcohol use disorder relative to both controls of LBP (OR 0.37; 95% CI: 0.29–0.47, p < 0.001) and T2DM (OR 0.39; 95% CI: 0.29–0.52, p < 0.001) (Fig. 2).
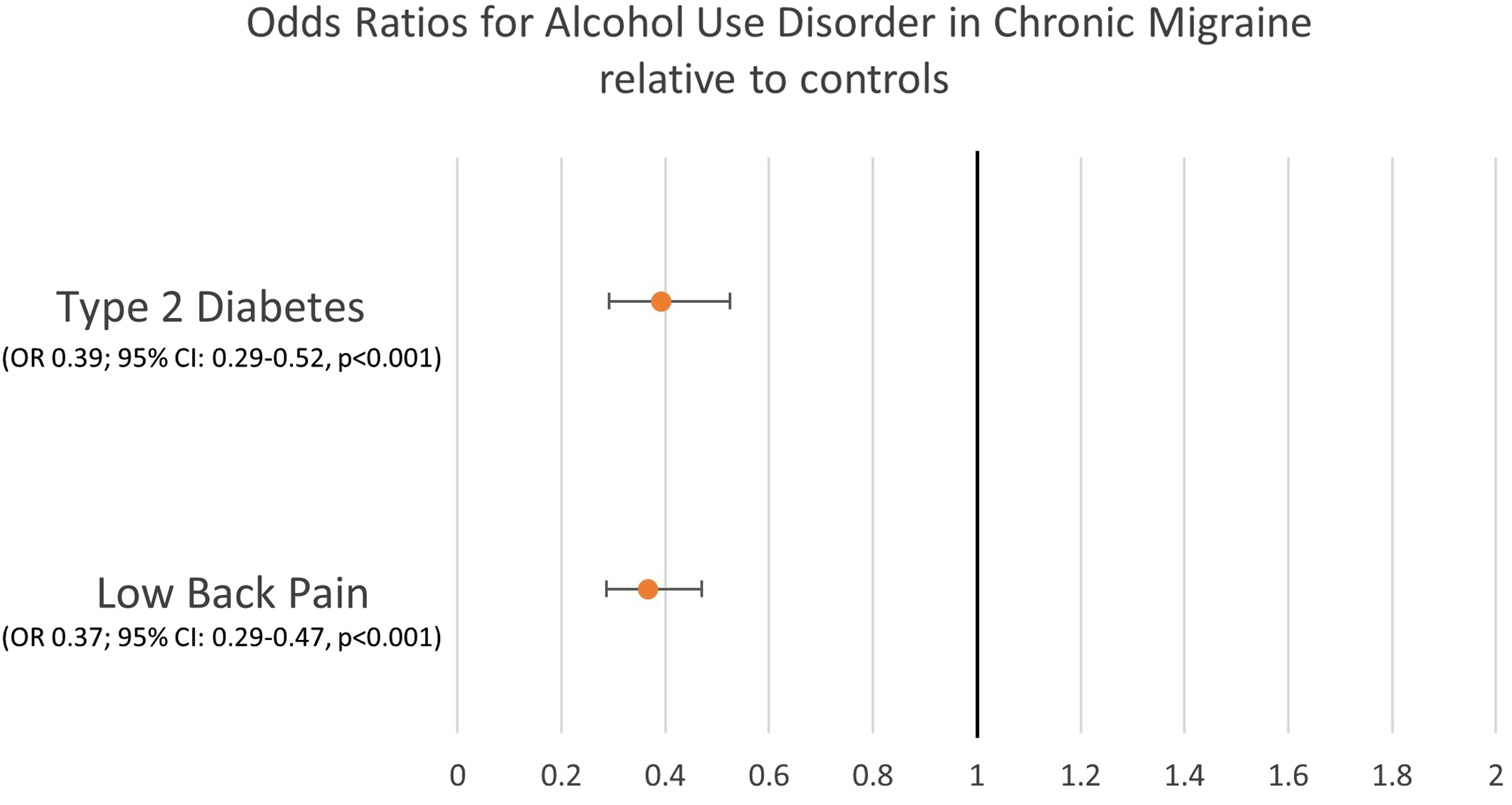
Figure 2: Odds ratios for alcohol use disorder in chronic migraine relative to disease controls.
Given that they are often comorbid with chronic migraine, we assessed the prevalence of receiving a diagnosis of depression, anxiety, or PTSD at any point. Anxiety was most commonly present in 1607/3701 (43.4%) of patients, followed by depression with 1311/3701 (35.4%) of patients, and PTSD with 253/3701 (6.8%) of patients.
Indeed, anxiety, depression, and PTSD were all associated with increased OR of alcohol use disorder for patients with chronic migraine (Fig. 3). Depression was associated with the largest OR for alcohol use disorder in chronic migraine (OR 8.62; 95% CI: 4.99–14.88, p < 0.001), followed by PTSD (OR 6.63; 95% CI: 4.13–10.64, p < 0.001), and anxiety (OR 3.58; 95% CI: 2.23–5.75, p < 0.001). When patients had both depression and anxiety, the OR for alcohol use disorder increased further (OR 13.92; 95% CI: 6.44–30.08, p < 0.001). Patients with depression, anxiety, and PTSD had the highest OR for alcohol use disorder (OR 27.6; 95% CI: 12.58–60.73, p < 0.001).

Figure 3: Odds ratios for alcohol use disorder in patients with chronic migraine by additional factors.
When depression, anxiety, PTSD, and sex were controlled for individually, the risk of alcohol use disorder in patients with chronic migraine was significantly lower relative to LBP and T2DM, excluding PTSD (Fig. 4); the risk of alcohol use disorder in patients with chronic migraine and PTSD was not statistically significantly different from that of LBP and PTSD (OR 0.64, 95% CI: 0.39–1.05, p = 0.076) and T2DM (OR 0.55, 95% CI: 0.28–1.07, p = 0.077).

Figure 4: Odds ratios for alcohol use disorder in patients with chronic migraine relative to disease controls for 3A: depression. 3B: anxiety. 3C: PTSD.
Discussion
The previous studies have sought to look at alcohol consumption in patients with migraine relative to patients without migraine; however, that may be a suboptimal control as patients with chronic conditions may have different utilization of alcohol relative to healthy controls. Consequently, we elected to use patients with low back pain and T2DM as the controls to represent a control with a pain condition and chronic, non-pain condition, respectively. We found that compared to both of these controls, patients with chronic migraine had a lower OR for alcohol use disorder, consistent with the studies suggesting that alcohol use can exacerbate migraine or is perceived to worsen migraine to the extent that patients avoid it by reputation alone. This comparison held true not only for chronic migraine overall, but for chronic migraine with comorbid depression and anxiety, but not PTSD. This suggests that similar to the NCSR, alcohol use disorder is driven by PTSD to the same extent in these populations. Reference Peterlin, Rosso, Sheftell, Libon, Mossey and Merikangas8
However, for patients with chronic migraine, comorbid depression, anxiety, and PTSD are drivers of increased alcohol use disorder, particularly when in combination with each other, as suggested by the exceptionally high OR of 27.6 for alcohol use disorder in chronic migraine patients with depression, anxiety, and PTSD relative to those with none of these comorbid conditions.
This relationship is especially important given that these comorbidities frequently present with chronic migraine; the observed rates of depression, anxiety, and PTSD in our patients with chronic migraine were consistent with what has been previously reported in literature. Reference Minen, De Dhaem and Van Diest10 The relationship between depression and chronic migraine has been suggested to be bidirectional, and that depression can be a risk factor for being refractory to treatment and medication-overuse headache. Reference Peck, Smitherman and Baskin11 With anxiety and chronic migraine, each is a risk factor for the other; patients with generalized anxiety disorder are at increased risk of migraine and vice versa. Reference Baskin, Lipchik and Smitherman12 PTSD has also been found to have a higher prevalence in patients with migraine than in the general population and a cross sectional study of patients with and without migraine found that PTSD could be a predictor of migraine. Reference Smitherman, Kolivas and Bailey13,Reference Peterlin, Tietjen and Meng14
The association of these psychiatric comorbidities with alcohol use disorder has been well reported. Depression and alcohol use disorder have been shown in a 14-year longitudinal study to be highly comorbid and with those patients at higher risk for downstream sequelae including life dissatisfaction and suicide attempts. Reference Brière, Rohde, Seeley, Klein and Lewinsohn15 Alcohol use disorder has also been shown to be higher in patients with a current anxiety disorder than in those without. Reference Wiener, Moreira and Zago16 Patients with PTSD have also been shown to develop alcohol use disorder at rates of 4.5–6.5 times higher than patients without PTSD. Reference Kessler, Chiu, Demler, Merikangas and Walters17–Reference Creamer, Burgess and McFarlane19
Additionally, the effect of sex on risk of alcohol use disorder in chronic migraine was minimal; there was no increase in OR for alcohol use disorder in men relative to women and both sexes with chronic migraine had a lower risk of alcohol use disorder relative to the LBP and T2DM controls. This is in contrast to the previous studies using NHANES and Swedish data to associate alcohol consumption and female sex and in agreement to the NHANES study suggesting no association between heavy alcohol use and migraine in men. Reference Evans, Lipton and Peterlin20,Reference Molarius, Tegelberg and Ohrvik21
While there are no previous studies identifying specific treatments for patients with chronic migraine and alcohol use disorder, many of the typical preventive medications can be applied for either this use directly, or towards the depression, anxiety, or PTSD which may be comorbid. For example, topiramate, which is commonly used for the prevention of chronic migraine, has also been shown to be effective for reducing alcohol consumption, including greater abstinence and decreased heavy drinking. Reference Blodgett, Del Re, Maisel and Finney22 Gabapentin has also been proposed as a treatment for alcohol use disorder but with mixed evidence. Reference Kranzler, Feinn, Morris and Hartwell23 Beyond these medications, anti-depressants such as venlafaxine or amitriptyline may be helpful in treating patients with chronic migraine, depression, and alcohol use disorder, with the aim of indirectly treating the alcohol use by directly treating the comorbid depression. Reference Torrens, Fonseca, Mateu and Farré24
Taken together, when patients establish care, it is the opportune time to not only assess for alcohol use disorder itself but also the comorbid factors that can impact not only their headache burden but also increases the risk for alcohol use disorder. To achieve this, validated alcohol screening tools, such as the Cut down, Annoyed, Guilty, and Eye-opener screener (CAGE) can be integrated into the patient intake paperwork to assess for alcohol use disorder. Reference Mulvaney-Day, Marshall and Downey Piscopo25 Alternatively, screening patients with the 11 questions asked in the DSM-5 criteria for alcohol use disorder could allow for longitudinal and quantitative monitoring. 26 Similarly, validated questionnaires for anxiety, depression, and PTSD can help alert the clinician to these comorbidities. Reference Mulvaney-Day, Marshall and Downey Piscopo25 However, simply assessing for alcohol use disorder, anxiety, depression, and PTSD alone are insufficient if not then treated; comprehensive headache management requires treating not only the primary headache disorder but also underlying contributing conditions and factors, often best performed with a team approach including physicians, psychologists, physical therapists, and social workers.
Our study is limited by the size of the data and nature of using large retrospective data. While the groups of patients are generally in the hundreds or thousands of patients, with the introduction of multiple additional factors, the size of the groups frequently dropped to fewer than 100 or 50 patients such that demographic analysis was limited. Given that alcohol consumption can be driven by cultural norms, determining the impact of these factors could not be performed due to the often singular or absent representation of a specific racial or ethnic group in many of the subgroups. Reference Dueland27 Additionally, due to the data abstraction system, it was necessary to use International Classification of Disease, Tenth Edition, codes to define these groups and not exact criteria; consequently, though we derived our chronic migraine group from patients seen exclusively by board-certified headache specialists, it is possible that a subset do not meet International Classification of Headache Disorders, Third Edition criteria for chronic migraine; with similar caveats for depression, anxiety, and PTSD and their Diagnostic and Statistical Manual of Mental Disorders criteria. Indeed, the prior studies assessing alcohol and migraine looked at either patient reported and quantified consumption of alcohol or DSM-5 diagnoses of alcohol use disorder and not ICD-10 codes, but the previous literature supports that there is acceptable agreement between DSM-5 diagnoses of alcohol use disorder and ICD-10 code diagnoses of alcohol abuse and alcohol dependence such that this could be an appropriate proxy. Reference Hoffmann and Kopak28
Future prospective trials for chronic migraine and alcohol use disorder could use ICHD-3 and DSM-5 criteria to more appropriately define study populations and then longitudinally track patients to determine if treating a patient’s alcohol use disorder can positively impact their headache burden.
Conclusion
Patients with chronic migraine had a lower odds ratio of AUD relative to controls. But in patients with chronic migraine, those with comorbid depression, anxiety, or PTSD are at higher risk of AUD. When patients establish care, comorbid factors should be assessed and for those at higher risk, AUD should be screened for at every visit.
Acknowledgements
None.
Funding
None.
Competing interests
None.
Statement of authorship
Study concept and design: LSM, NZ. Acquisition of Data: LSM. Analysis and interpretation of data: LSM. Drafting of the manuscript: LSM. Revising it for intellectual content: LSM, NZ. Final approval of the completed manuscript: LSM, NZ.









