More than 175,000 people sustain a concussion annually in Ontario Reference Langer, Levy and Bayley1 and up to 35% continue to experience persistent post-concussion symptoms beyond 3 months. Reference Cancelliere, Verville and Stubbs2 Why some people recover in days and others take months or years is not clear, but this appears to be the result of multiple interacting neuropathological and psychological factors. Reference Marshall, Lithopoulos and Curran3 Effective treatments to prevent persistent symptoms are still to be developed and evaluated. Safe timing for return to activity following concussion remains unclear. Furthermore, there is growing evidence that a single concussive event and even multiple sub-concussive hits can be associated with a more aggressive aging process. Reference Del Bigio, Krawitz and Sinha4 However, who is at risk and why remains unknown.
Seeds Toward a Concussion Network
In 2014, the St. Michael’s Hospital Head Injury Clinic hosted a meeting with health care professionals (physiotherapy, athletic therapists, occupational therapy, nursing, physiatry, psychiatry, emergency physicians) advocacy groups, persons and family members with lived experience of concussion. The Ontario Concussion Care Strategy (OCCS) emerged with a vision to work collaboratively to improve concussion care and reduce the impact of chronic impairment.
By 2015, an environmental scan of selected specialty clinics across Ontario was completed to understand the data being collected during the assessment and follow-up of adults with concussion. It became clear that the common data elements (CDEs) established by the National Institute of Neurological Disorders and Stroke 5 were not being used in Ontario and wide variability existed between clinics. It was recognized that CDEs had the potential to: (a) improve quality of care, (b) reduce specialty clinic wait times, (c) educate health care providers, (d) support multisite research, (e) promote data harmonization, (f) align data for research collaboration and comparison, and (g) provide benchmarks for individual sites 5 to support health policy & planning. The OCCS agreed to establish and implement CDEs to create a minimum data set for concussion care in Ontario.
Implementing CDEs for Concussion Care and Research
After reviewing the literature, OCCS sought consensus among provincial concussion experts Reference Hunt, Michalak and Ouchterlony6 to establish CDEs. With funding from the Ontario Neurotrauma Foundation, data collection using Research Electronic Data Capture (REDCap) by four concussion clinics in Toronto, Ottawa, London and Thunder Bay commenced. The OCCS continued to promote uptake of the CDEs (Figure 1) and identified key elements that would be required to move toward a standardized provincial approach to concussion care and research:
-
• A centralized hub with staff and resources to support the network’s vision
-
• Funding for development, sustainability and research
-
A website to house and share tools
-
• Staff support for ongoing assessment and review of CDEs
-
• Funding for systematic electronic data capture of CDEs
-
• Staff for data management (collection and curation)
-
• Staff for multisite coordination
-
• Funding to expand partnerships for geographical representation across the province

Figure 1: CONNECT CDEs.
NINDS = National Institute of Neurological Disorders and Stroke; CDC = Center for Disease Control; TBI=Traumatic Brain Injury.
Establishing a Diverse and Inclusive Concussion Network
With new funding from the Ontario Brain Institute (OBI), 7 a Program Manager was hired and OCCS rebranded as Concussion Ontario Network: Neuroinformatics to Enhance Clinical care and Translation (CONNECT). Challenges affecting concussion care were identified including: a) non-evidence-based care for symptom management, b) a need to increase the knowledge-base of health care providers, c) concerns about clinics with questionable credentials, d) challenges with guideline implementation in schools, e) inadequate funding support for multidisciplinary care, f) waiting times >1 year for tertiary care in some areas, and g) stigma related to stress and depression post-concussion. The CONNECT network affirmed a ‘CLEAR’ mandate to focus on the value add of CONNECT: a Cooperative network to Link research to practice, Engage with community, and Activate commercialization and Research that matters more to more.
Inspired by Haddon’s injury matrix, Reference Haddon8 CONNECT developed a framework for research based on four themes: (1) Before the Trauma, (2) The Trauma, (3) After the Trauma, and (4) Long Term Consequences (Figure 1). Before the Trauma considers the influence of premorbid biopsychosocial factors on outcomes. The Trauma focuses on developing an improved understanding of the pathophysiology, diagnosis, and early management of concussion (<30 days). Reference Hunt, Dosaj and Ackery9 After the Trauma addresses the management of sequelae 30-89 days post-injury. Whereas, Long Term Consequences is concerned with the potential for deterioration 90 days or more post-concussion. Together, themes 1 and 2 aim to discover innovative tools for the assessment and diagnosis of concussion (Recognize). Whereas, themes 3 and 4 seek to test novel interventions that speed recovery, prevent re-injury, and reduce the risk of long term complications (Maximize). These vertical themes intersect with the transverse discovery platforms set out by OBI. 7 The arrow emphasizes the integrative role of Diversity and Neuroinformtics. Diversity is used to describe the many ways that people who experience a concussion may differ. Examples of diversity include primary characteristics of age, race, birth sex, medical history and differences in injury related elements such as mechanism of injury (ie. transportation, recreation, violence etc.) type and duration of symptoms, and time since injury (acute, subacute or longer term). Neuroinformatics entails collecting and collating all available data in a form that harnesses advanced analytic processes such as machine learning. The data has the potential to optimize patient outcomes by facilitating the provision of the right care at the right time to the right person (Personalize) (Figure 2).
Examining the CONNECT Data
By March 2023, CONNECT enrolled 819 participants (Table 1). The sample has a 2:1 ratio of females to males. This is important as concussion research to date has focused disproportionately on males. Reference Kenzie, Parks, Bigler, Lim, Chesnutt and Wakeland10 Compared to characteristics of the Ontario population the current CONNECT data (see Table 1) is more heavily weighted toward younger adults. Employment status is fairly evenly divided across Ontario, whereas a 3:1 ratio of employed (including those on disability or short/long-term leave) to unemployed is seen in the CONNECTdata. The largest proportion of participants in the CONNECT sample have never been married, whereas in Ontario the majority are married.
Table 1: Comparison of CONNECT data to Ontario 2021 census data

CONNECT participants (Table 2) are largely greater than 12 weeks post-injury, followed by those less than 4 weeks post-injury; although, there was a larger difference in size between these two groups among females. In total, the majority of injuries were attributed to falls and transportation-related incidents, which is important as most current research is focused on sport. Injury mechanism is evenly distributed across falls/flying and falling objects, transportation and sport/exercise related events in males. The majority of females were injured from falls/flying and falling objects. A similar proportion of females and males reported a previous diagnosis of concussion and learning disability. The proportion of females reporting a previous mental health condition was higher than males.
Table 2: CONNECTing injury and medical history by sex
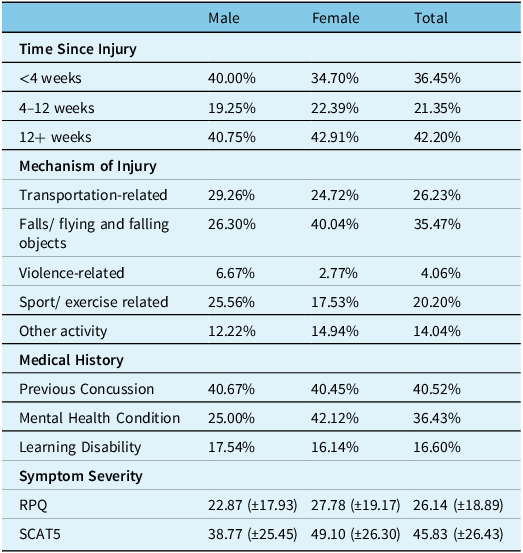
N = 819 with missing values omitted. ‘Mental Health Condition’ includes anxiety, depression and any other mental health illness. ‘Learning Disability’ includes dyslexia and ADD/ADHD. Symptom Severity scores are presented as: mean (standard deviation). SCAT5 = Sport Concussion Assessment Tool 5. The SCAT5 is used by 3/10 sites and is scored out of 132 with higher scores indicating a higher number and severity of symptoms. RPQ = Rivermead Post-Concussion Symptoms Questionnaire. The RPQ is used by 7/10 sites and is scored out of 64 with higher scores indicating a higher number and severity of symptoms.
To date 75% of participants self-identified as White, while the remainder were grouped into Non-White which included Aboriginal, Arab, Black, Chinese, East Asian, Filipino, Japanese, Jewish, Korean, Latin American, South Asian, Southeast Asian and West Asian. Non-White participants had a greater proportion of young patients, while Whites has a greater proportion of older patients (Figure 3). Whites reported a greater proportion of migraine headaches pre-injury compared to Non-White (p = 0.039) (Figure 4) as well, a larger proportion of Whites reported they experienced greater depression, anxiety or any mental health condition pre-injury (p = 0.0002132) (Figure 5). A greater proportion of Non-Whites reported seeking more emergency room visits post-concussion for care (p = 0.002) while Whites reported more post-concussion visits to their family doctor (p = 0.00005793) (Figure 6).
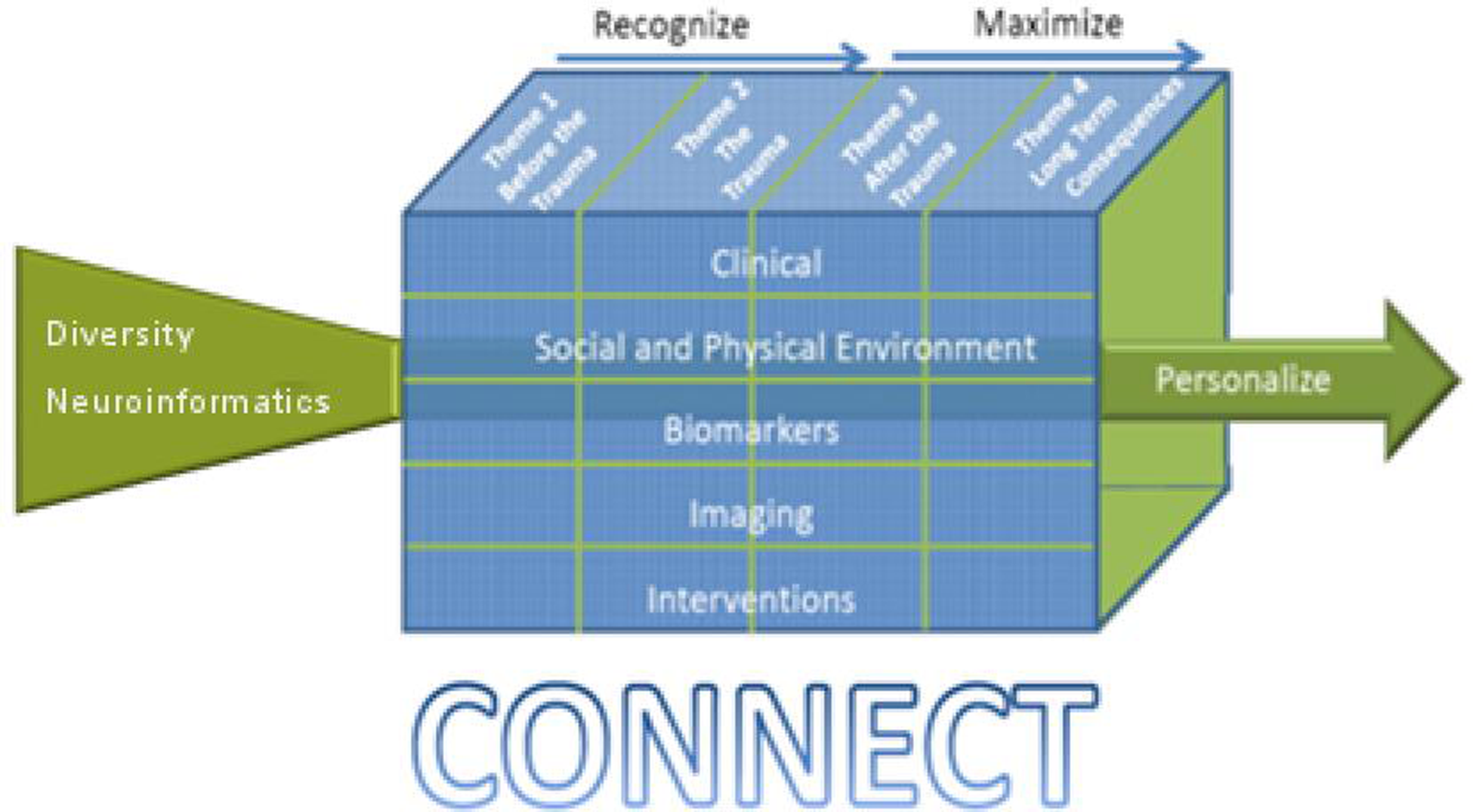
Figure 2: CONNECT’s conceptual model: merging care with research.

Figure 3: CONNECT data by age.

Figure 4: CONNECT data by income.

Figure 5: CONNECT data by medical history.

Figure 6: CONNECT data by post-concussion health care utilization.
Sustaining the Network
With an established alliance of clinicians, researchers, consumers and industry partners as well as a robust data management system, CONNECT has the potential to become a global leader in concussion research and evidence-based care. This infrastructure can support large-scale clinical trials and meta-analyses to test novel assessment tools and implement targeted interventions. Differences in patient outcomes can be explored allowing for identification of recommendations for best practices in concussion care. Clinical teams across participating sites shared their perspectives on the strengths of CONNECT (Figure 7). CONNECT is dependent on external funding for support and is pursuing options with academic and industry organizations in order to sustain its ongoing diverse multisite data collection, centralized program coordination, robust data management, and further expansion.

Figure 7: Strengths of CONNECT.
Acknowledgements
We acknowledge support of the 10 clinical site investigators engaged with CONNECT across the province; Dr.’s S Marshall, L Fischer,V Kristman, D Velikonja, S Grenier, as well as authors CT, M Burke, M Bayley, HM and AB. We also appreciate the work of the RAs at each of these sites and we thank the patients for consenting to contribute their data to CONNECT.
Funding
CONNECT acknowledges the support of the Ontario Brain Institute (OBI), an independent nonprofit corporation, funded partially by the Ontario government. Fund to Unity Health from OBI supported salaries to CH and AD.
Statement of authorship
CH, HM and JZ developed the draft manuscript, all authors critically reviewed the paper.











