A 77-year-old woman presented with a 4-day history of dyspnea and was admitted to our hospital. Her past medical history included hypertension, chronic heart failure, and myasthenia gravis, for which she had been taking furosemide (10 mg/day), carvedilol (5 mg/day), prednisolone (7 mg/day), tacrolimus (3 mg/day), sulfamethoxazole (400 mg, three times a week), and trimethoprim (80 mg, three times a week).
On admission, there was no decreased level of consciousness or headache. Her body temperature was 36.4°C. Saturation of percutaneous oxygen was 98% on room air. Blood tests showed a white blood cell count of 6540/μL and a C-reactive protein level of <0.10 mg/dL. Testing for human immunodeficiency virus was negative. Chest X-ray demonstrated no findings suggestive of interstitial lung disease. After admission, she had episodes of fever above 38.0°C. Serological studies 9 days after admission detected cryptococcal antigens. A lumbar puncture carried out 21 days after admission yielded watery but slightly yellow CSF.
The CSF was evaluated using a hemocytometer (DHC-F01; NanoEnTek Inc., Seoul, Korea) with Samson’s solution (Muto Pure Chemicals Co., Ltd, Tokyo, Japan). This solution is composed of 30 g of acetic acid, 2 g of phenol, and 2 g of 10% alcoholic fuchsin solution, which are brought to a total volume of 100 mL with water. The cell count was 183/μL, comprising mononuclear cells of 165/μL and polymorphonuclear cells of 18/μL. Interestingly, the cryptococcal organisms were visible on hemocytometer (Figure 1). Total protein and glucose levels of the CSF were 264 and 10 mg/dL, respectively. The administration of amphotericin B and flucytosine was initiated based on a diagnosis of cryptococcal meningitis. CSF culture confirmed the presence of cryptococcus neoformans.
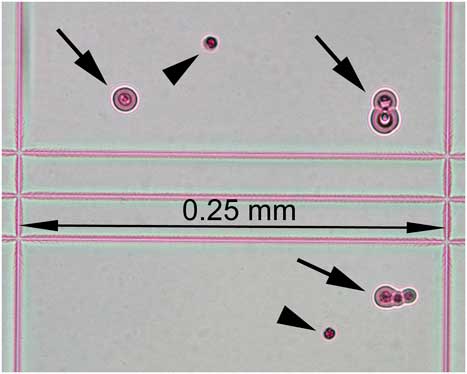
Figure 1 The hemocytometer used has a 0.25 mm grid. The arrows indicate encapsulated cryptococcal organisms, some of which display budding, and the arrowheads indicate mononuclear cells.
Although blood and CSF cultures as well as detection of serum and CSF cryptococcal antigens are standard methods for a diagnosis of cryptococcal meningitis,Reference Tunkel, Glaser and Bloch 1 the demonstration of cryptococcal organisms by hemocytometer can provide a rapid diagnosis of cryptococcal meningitis and accelerate definitive treatment. Others have described cytological methods for detecting cryptococcal organisms,Reference Choi and Kim 2 however, their detection by hemocytometry represents a very rapid, available, and inexpensive opportunity.
Acknowledgments
The authors thank Toshikazu Kohno for medical care of the patient, and Shoichiro Ishihara for helpful comments for this study.
Disclosures
The authors have no conflicts of interest to declare.



