Introduction
With the first reported COVID-19 (SARS-CoV-2) case in December 2019, the World Health Organization declared a pandemic resulting in varying levels of social distancing and public health measure restrictions across the world. To mitigate the spread of COVID-19, personal practices and community-based measures were set in place, including limits on public health gatherings, non-essential businesses, non-urgent clinical care, and travel. Despite the existing safety precautions in place, COVID-19 has increased the vulnerability for certain populations, specifically the elderly, those with comorbidities, and patients living with a chronic disease such as Parkinson’s disease (PD). Reference Papa, Brundin and Fung1
These measures inadvertently impacted the routines for people with PD and their care partners in compromised neurological clinical care and drastically changed the way of life to minimize the risk of becoming infected playing a negative role in PD patients. Reference Sainz-Amo, Baena-Álvarez and Pareés2 The rapid progression of the pandemic and governments response to the reorganization of the economy has limited health care resources, and placed PD patients at risk in deterioration of motor-worsening and indirect effects including non-motor negative consequences of stress, self-isolation, anxiety, and depression. Reference Zipprich, Teschner, Witte, Schönenberg and Prell3-Reference Helmich and Bloem5 The public health restrictions have further impacted the way PD patients obtain medications for their management of the disease.
Overall, the health care sector has undergone rapid and drastic modifications to cope with current needs, with routine clinic visits consequently being on hold to address acute care. Reference Prasad, Holla and Neeraja6 Alberta reported 315 new COVID-19 cases and 7 more COVID-19-related deaths by April 29, 2020, with a total of 3,590 cases in the Calgary zone. The Movement Disorders Clinic at the Foothills Medical Centre Calgary, Alberta, suspended their clinics on March 13, 2020, cancelling all in-person clinical appointments and transitioning to a new growing field of telemedicine. With the second wave of COVID-19 approaching, continued virtual care becomes increasingly critical to understand. A purely qualitative approach on PD experiences with virtual care and COVID-19 is missing. While there is new emerging quantitative studies Reference Fasano, Cereda and Barichella7,Reference Fasano, Elia and Dallocchio8 on PD and COVID-19, a qualitative approach on perceptions, attitudes, and experiences has been limited, leaving patient-centered outcomes to be overshadowed during this time. Our single-center study provides insight into the direct and indirect associations between COVID-19 and PD clinical care and other daily effects, which may serve as guidance in the current and upcoming times of telemedicine.
The present study aimed to understand the impacts of COVID-19 on patients’ clinical symptoms of PD in both motor and non-motor aspects and learn from the direct experiences of virtual medicine from PD patients that could help guide social and health services virtually moving forward. We conducted a qualitative study with patients who receive community-based care at a specialty Movement Disorders clinic. A qualitative approach with a reflexive thematic approach to context analysis was used to collect rich data and develop in-depth understanding on this population’s lived experience to better inform health care management for patients living with PD during a pandemic and utilizing virtual care. This study utilizes patient engagement to drive understanding and next steps for future virtual care.
Research Design
We completed 22 virtual, in-depth semi-structured interviews with persons diagnosed with PD between April 28 and May 13, 2020, and their care partners if they wished to attend the interviews and were able to provide consent. To provide current and up-to-date data on the pandemic’s impacts, participants were enrolled and provided detail on their experience while the pandemic was occurring, and public health measures were in place.
Recruitment
We purposely recruited participants who are regularly followed up by the Movement Disorders Clinic in Calgary, Alberta, Canada. Participants had a diagnosis of PD verified by a specialty neurologist according to the UK Brain Bank diagnostic criteria, Reference Daniel and Lees9 had agreed to participate in the CaPRI (Calgary Parkinson Research Initiative) registry, and had previously provided written consent to be contacted about additional research. CaPRI registry’s purpose is to increase our understanding and knowledge of PD or other Parkinsonian syndromes to develop better tests to diagnose and improve the management and treatments of the disease. Consecutive patients from the CaPRI registry who had experiences in telemedicine in the last 6 weeks or had an upcoming virtual appointment were included.
Potential participants were contacted by telephone and informed of the project, after which information sheets and consent forms specific to the study were emailed shortly after to interested participants following local IRB consenting procedures. Participants were given a minimum of 24 h to consider the information and discuss it with family members or health providers before consenting to take part. Participants were given the option of telephone or Zoom interviews for their scheduled interviews. 10 Zoom is a web-based video conferencing tool that allows a virtual face-to-face meeting. Zoom provided more intimate interaction for those participants longing for the interpersonal connection. It also provides many participants practice with using video conferencing and technology who hoped to be better able to use Zoom amid COVID-19 with friends and family. Alternatively, some participants opted for the convince and simplicity of the telephone interview.
Informed consent was obtained using Qualtrics survey software 11 in all but one participant who could not connect to the internet to access the consent form and provided explicit oral consent. Despite oral consent only being used by one participant, explicit oral consent was incorporated in this study to ethically include a diverse population who may have encountered other difficulties consenting via Qualtrics. Throughout the study, process consent was used, meaning participants consented once via online consent form and consented again verbally at the scheduled time of the interview to ensure that all participants were still comfortable participating in the study at the time of contact. Reference Dewing12 In some instances, participants wished to reschedule, and process consent was sought again at the time of the rescheduled contact between researcher and participant. The Conjoint Human Research Ethics Board approved this study at the University of Calgary (REB20-0559).
Data Collection
In-depth interviews were used in a semi-structured format as they are an appropriate way to gain a rich, full understanding of lived experiences. The semi-structured questionnaire consisted of initial questions relating to the pandemic itself, including normal activities and care before the pandemic. The interview schedule was developed through consultation with clinical experts, academic experts, and patient/family representatives regularly involved in research with the Brain and Mental Health Research Clinics. Further questions captured how daily routines and clinical care have been impacted by adherence to ongoing regulations, exploring physical and mental health strains. Overall attitudes and coping mechanisms were explored, and participants were inquired for their feedback on any improvements in helping them during this social distancing and improving virtual clinical care.
To achieve theoretical saturation the team estimated approximately 15–20 interviews with different participants would likely need to be completed. Reference Braun, Clarke, Weate, Smith and Sparkes13,Reference Clarke, Braun, Terry, Hayfield and Liamputtong14 Therefore, with 22 participants enrolled, the target data quota was reached for allowing diverse and rich coding to be available. Common themes were emerging after approximately 15 completed interviews, with the remaining interviews allowing for member checking to look for confirming or disconfirming experiences, and enhancing rigor. In-depth interviews were recorded with an audio recording device and transcribed immediately after. Field notes were taken during interviews or directly following the interviews and uploaded with the recordings to be reviewed during the analysis. Demographic data obtained were age at the time of participation, gender, and information on whether the participants had been tested or diagnosed for SARS-CoV-2. An initial list of 39 potential participants was obtained from the CaPRI registry list. Twenty-two participants were enrolled; 17 from the original list were contacted but either declined or were unable to be reached. The duration of the interviews ranged from 23m:45s to 1h:05m:44s (mean length = 43m:52s) and were completed either by phone or Zoom depending on participant preference, as previously described. Recruitment and data collection were completed by the main research assistant (BA). The senior investigators oversaw the study process. The interviewer had no previous relationship with any of the participants on the registry list and introduced herself and the reason for work at the initial contact.
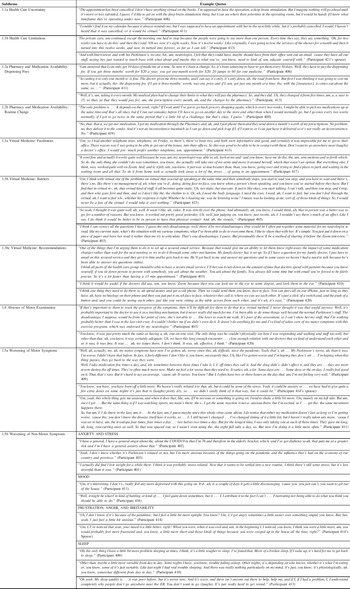
Figure 1 displays a timeline of the provincial measures for social distancing and health system changes. The Movement Disorders Clinic had stopped in-person clinic visits on March 13, 2020, onwards. Study participants were faced with cancellation of their in-person appointments until further notice, while other appointments were able to be adapted to virtual appointments.

Figure 1. Timeline of COVID-19 Public Health Response in Alberta, Canada.
Analysis
Audio recordings were transcribed verbatim using a secure professional transcribing service and anonymized for any identifying information by the interviewer. Transcripts and field notes were uploaded into NVivo 12 software for qualitative analysis and data management. 15 To achieve theoretical saturation and generate themes, interviews were transcribed in parallel while data collection was still occurring. The first step of the analysis was to become immersed in the data analysis by having transcripts read and re-read while the interview recordings were replayed. Reflexive thematic analysis was used, which allowed the researchers to be the core in coding and theme development. Reference Braun, Clarke, Weate, Smith and Sparkes13,Reference Clarke, Braun, Terry, Hayfield and Liamputtong14 This form of analysis is well suited for exploring people’s experiences, views, and perceptions. Patterns, analytical thoughts, and iterative analysis were captured through memos and annotations. Research team meetings were held weekly to touch base on emerging codes and themes from the data analysis.
Results
Participant Demographics
A total of 22 participants living with a PD diagnosis were included. Five care partners accompanied the PD participants in the interviews and provided additional data. Out of the 22 participants, 16 males contributed 72.7%, and 6 females accounted for 27.3% of our sample. The age range was 51–79 years old with a mean age of 70.5 years of age. No participants reported a diagnosis of COVID-19 for anyone living in the household; two participants received a negative screening test for COVID-19; five participants reported being told by public health authority that they should self-isolate after returning home from travel.
Thematic Analysis: Experience of the COVID-19 Pandemic
Thematic coding was completed by BA, directed by PR (Principal Investigator and qualitative methods expert) and in collaboration with VB and DM (Movement disorders specialists and researchers).
Impacts of COVID-19 on PD Clinical Care
Healthcare Limitations and Uncertainty
Many patients reported feeling alone and unsupported during the pandemic, expressing limited communication with their physicians and uncertainty around appointments, procedures, and general PD inquiries (Table 1; Subtheme 1.1a Health Care Uncertainty). The public health measures impacted the health services and in turn impacted patients. A few participants stated they had received proper routine care from home care services and reported feeling unsupported when the services stopped (Table 1; Subtheme 1.1b Health Care Uncertainty).
Table 1. Theme: impacts of COVID-19 on PD clinical care
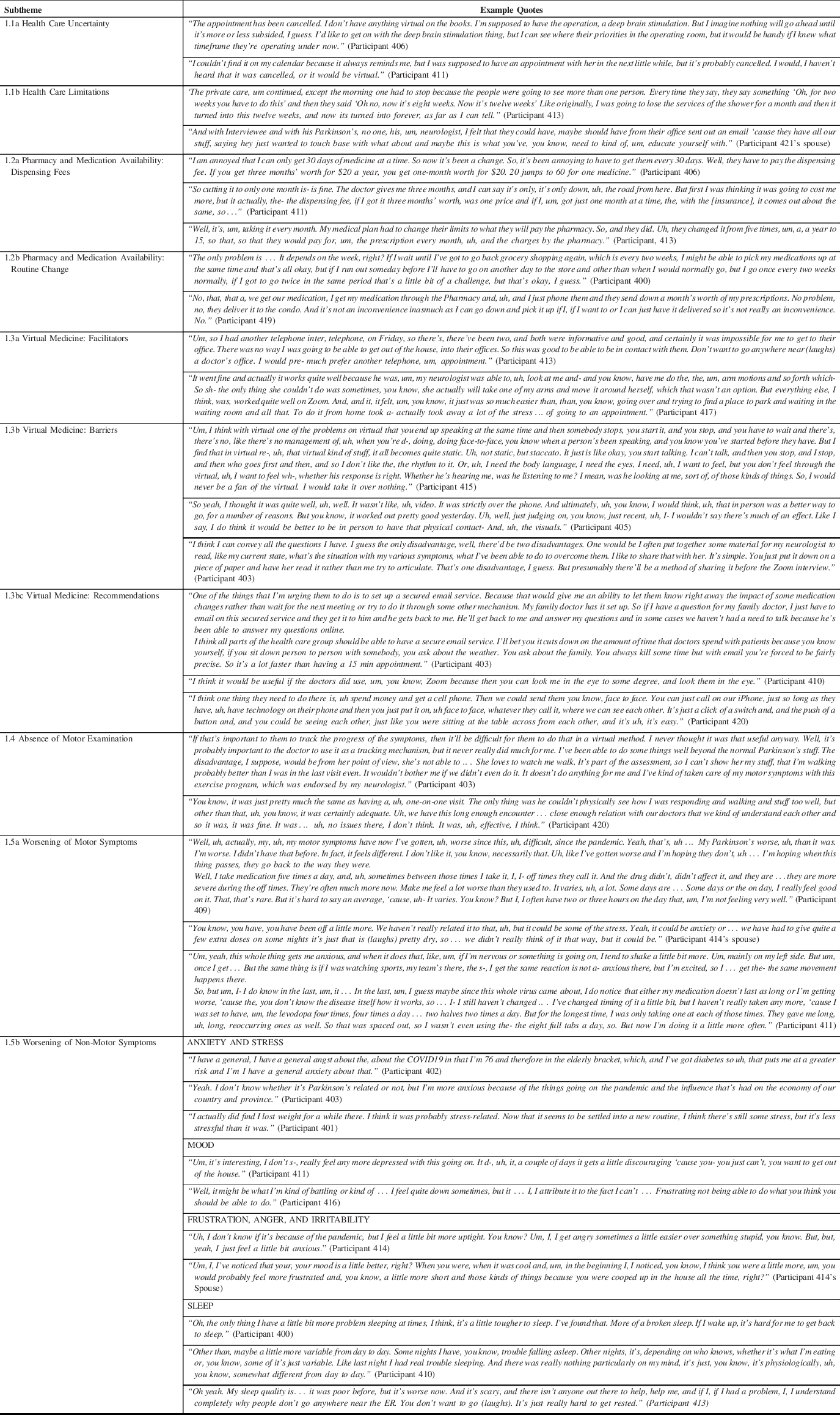
Pharmacy and Medication Availability
Participants reported some uncertainty around the restrictions put in place and expressed concerns about how insurance works with increased dispensing fees (Table 1; Subtheme 1.2a Pharmacy and Medication Availability: Dispensing Fees). Some participants reported a change in routine for obtaining their medication, including the new delivery service provided by pharmacy or shift in routine (Table 1; Subtheme 1.2b Pharmacy and Medication Availability: Routine Changes).
Virtual Medicine: Facilitators and Recommendations
Mixed responses were provided regarding the transition from in-person to virtual clinical appointments, with an overall preference for participants’ in-person visits. While some enjoyed the benefits of virtual appointments, most viewed it as a temporary solution acknowledging some form of care was better than a complete halt of clinical care. Those who preferred virtual appointments reported the benefits of over-the-phone appointments’ convenience and efficiency, saving them the hassle of driving and parking (Table 1; Subtheme 1.3a Virtual Medicine Facilitators). Most PD patients reported a preference of seeing their physician due to various barriers they viewed in virtual appointments including simultaneous speaking making it difficult to converse, less connection without being physically present viewed as invaluable and increased difficulty conveying notes or updates virtually (Table 1; Subtheme 1.3b Virtual Medicine Barriers). When asked what could be improved in health care during this pandemic to provide the optimal quality of care during these circumstances, some patients provided insightful recommendations including secure email and video methods to efficiently and remotely connect with physicians (Table 1; Subtheme 1.3b Virtual Medicine: Recommendations).
Absence of Motor Examination
Many patients reported that the appointment’s motor examination was less useful to them and emphasized its importance for their neurologist. Some patients reported a virtual appointment with video could be useful to assess walking, but no significant concerns were expressed with the inability to fully perform a physical examination of motor symptoms during virtual telephone appointments (Table 1; Subtheme 1.4 Absence of Motor Examination).
Worsening of Motor Symptoms
Participants described the worsening of motor symptoms of PD since the pandemic started. Some participants had difficulty differentiating if the worsening of their symptoms was attributed to the disease progression or the pandemic. Others explicitly stated noticing an increase in OFF-times, tremors/shaking, and stuttering (Table 1; Subtheme 1.5a Worsening of Motor Symptoms).
Worsening of Non-Motor Symptoms
During the pandemic, PD patients expressed an increase in anxiety and stress, leaving some participants noticing more substantial changes as a result (Table 1; Subtheme 1.5b Worsening of Non-Motor Symptoms: Anxiety and Stress). Surprisingly, when asked about any mood changes or changes to mental well-being since COVID-19, most participants expressed little to no observed changes in their mood (Table 1; Subtheme 1.5b Worsening of Non-Motor Symptoms: Mood). Some participants expressed an increase in more negative moods, including frustration, anger, and irritability since the pandemic (Table 1; Subtheme 1.5b Worsening of Non-Motor Symptoms: Frustration, Anger, and Irritability). Lastly, many participants reported worsening of sleep during the pandemic, expressing increased difficulty falling asleep and a broken sleep during the nighttime, and increased frequency of daytime naps (Table 1; Subtheme 1.5b Worsening of Non-Motor Symptoms: Sleep).
Impacts on Personal Life
Behavioral Changes to Exercise
Many participants reported abrupt changes in their lives with both cancellation and alteration of multiple routine social and physical activities they were engaged in. Specifically, physical activities have been predominantly impacted by PD participants. Many participants found ways to continue a modified exercise routine despite the closure of many in-person physical activity classes and facilities. Many participants reported their modified exercise routine during the pandemic now includes more walking outside during pleasant weather and adapting to virtual exercise classes either on their own via YouTube or following the Parkinson Association of Alberta exercise classes. PD patients reported adjusting to exercising following these virtual exercises classes including yoga, gentle PD exercises, seated exercises, and stretching. PD patients continue to find a modified exercise routine as many have found improvement in their PD symptoms from exercise (Table 2; Subtheme 2.1 Exercise Changes).
Table 2. Theme: impacts on personal life

Isolation
While some people live together with family and others alone, most of the participants have expressed missing their usual daily activities outside the home and visiting with friends and family taking a toll on their well-being (Table 2; Subtheme 2.2 Isolation).
Managing Boredom
While some participants have expressed feelings of isolation, others are searching or have found new activities to manage the boredom that comes from being isolated in their homes (Table 2; Subtheme 2.3 Managing Boredom).
Interpersonal Relationships
Participants frequently reported adhering to the physical distancing measures by eliminating friends and family regular indoor visitations. Many participants expressed being grandparents and found it very difficult to be stripped of visiting their grandchildren during this time. Furthermore, participants expressed ways to keep socializing amid the pandemic by adapting to use technology, phone or video calls, or visiting outdoors with physical distancing measures. However, most of the perceptions around socialization, despite the attempts to connect via technology, were longing to give and receive hugs of family members and be present physically. In terms of spousal relationships, participants shared a mix of reports, with some expressing increased appreciation for their spouse during the pandemic, while others felt the strain of living in close proximity (Table 2; Subtheme 2.4 Interpersonal Relationships).
Attitudes and Perceptions
Silver Linings of COVID-19
While the pandemic has affected many individuals in negative ways, some of the participants expressed the contrary. They saw some positive changes emerge from the new way of life, including thoughts on their PD being more comfortable managing from home and a slower-paced life, more consistency in meals and medications, and saving time and money on driving (Table 3; Subtheme 3.1 Silver Linings of COVID-19).
Table 3. Theme: attitudes and perceptions

Adhering to Health Experts Attitudes and Awareness
Many participants reported abiding to public health measures in place and minimizing risks for getting infected. Few patients reported having comorbidities and felt at even greater risk. Besides, when asked about travel and socialization restrictions, most participants understood where the priority lies with the health experts in safety precautions even if they miss their usual activities. Participants’ attitudes were negative around those who do not adhere to public health measures (Table 3; Subtheme 3.2 Attitudes Around Health Experts Recommendations).
Personal and Societal Concerns
While many participants expressed minimal fears or concerns about COVID-19 because of the inability to do anything about the situation, others felt different and skeptical of the current situation and what the future will hold, including health, finances, and government decisions (Table 3; Subtheme 3.3 Personal and Societal Concerns).
Discussion
In this single-center study, initial evidence is provided into the clinical and personal impacts of COVID-19 pandemic on persons living with PD through a qualitative approach. Researchers have highlighted the importance of qualitative research during the COVID-19 pandemic, reporting the value in gaining insights into aspects of behavior and perceptions that is often missed in epidemiological and clinical research. Reference Vindrola-Padros, Chisnall and Cooper16 This study allowed building the interview guide accordingly to ask questions on PD patients lived experiences during COVID-19, clinical care and epidemic response efforts to complement epidemiological data. While these interviews did identify PD patients coping reasonably well with the pandemic changes, adverse consequences arose impacting their quality of life, including lack of access to necessary health care, worsening symptoms, and social isolation for others that were explored in depth. These domains provide insight into modifications and restructuring of treatment planning for the subsequent waves of COVID-19 (at the time of writing Calgary, Alberta is currently experiencing a second wave). A benefit of the study was the in-depth data collection that allowed a rich understanding of the experiences of PD patients in an urban, ambulatory care clinic context that is transferable to other outpatient, community-based clinical settings providing virtual care.
Medications
The takeaway from our PD participants was more associated with the uncertainty of pharmacy procedures around PD medications more so than the direct impacts. PD patients of our study coped well with adapting their routines with minimal difficulty. Several provinces in Canada, including Alberta, imposed limits on the supply of prescription drugs that pharmacies can dispense. These restrictions took place in March 2020 and placed a 30-day limit of medication instead of the usual 90 or 100 d creating further impacts for PD patients. While PD patients in our study faced slight disturbances in their ordinary routine regarding obtaining their medication and payments, many had questions around increased dispensing fees. In particular, since they normally would receive 90-days’ worth of prescription medication, they were now paying the dispensing fee three times instead of one. As of June 15, 2020, Alberta’s pharmacies have resumed dispensing up to a 100-day supply for most medications. In one study by Cheong and colleagues, Reference Cheong, Goh and Marras17 out of 346 participants, 45.4% answered ‘yes’ to difficulty obtaining regular PD medication due to COVID-19, while 54.6% answered ‘no’. These findings support our participant’s experiences as those who did express some effect was minimal. The takeaway from our PD participants was more associated with the uncertainty of pharmacy procedure around PD medications more so than the direct impacts. PD patients of our study coped well with adapting their routines and would have no patients reported difficulty receiving their PD medications.
Next steps
Increased communication around pharmacy and medication availability would help in future restrictions of PD medications for individuals. Parkinson Canada, a main information source for PD news, recommends individuals with PD to check their medications and contact pharmacists to refill prescriptions that are running low ahead of time to ensure sufficient time for processing and delivery. 18 Further, Parkinson Canada recommends taking advantage of delivery service if available to limit exposure in the pharmacy. 18 Similarly, the Michael J. Fox Foundation for PD research provided recommendations on their website in regard to PD medications during the pandemic with the guidance of a movement disorders specialist. 19 Some insurance companies are lifting restrictions that typically only allow a one-month supply. PD individuals are encouraged to maintain a 3-month supply of medication and contact their doctor and pharmacist about options if needed. Michael J. Fox Foundation reemphasized taking advantage of delivery service or an insurance mail-order service during these times. 19 It is important to adhere to these recommendations, as limiting supplies to 30 d can increase the risk of contracting COVID-19 by creating the need to go to public places, including pharmacies, more frequently. We encourage PD individuals to stay informed on updates. Future research and policies should encourage pharmacies to facilitate more open communication about PD medications and insurance plans during changes in medication procedures.
Clinical Care
Many PD patients routinely visit with their neurologists at the Movement Disorders Clinic for physical motor assessments and medication adjustments. However, only a limited number of patients, such as PD patients receiving Botulinum injections, have returned to in-person visits. Many non-surgical procedures have been postponed preventing patients from potential exposure to the virus. Some elective surgical procedures like deep brain stimulation (DBS) have been delayed, leaving some PD patients facing barriers in achieving optimal care until further notice. Reference Elbeddini, To, Tayefehchamani and Wen20 Only one participant in this study was waiting for his DBS appointment, which has been cancelled for the time being, while many other participants expressed a short-term understanding of the delay in clinical care but foresee progressive PD problems if the clinical visitations do not resume soon.
Hospital visits should still be avoided to those who do not have an urgent need to be in person for their clinical appointments whenever possible during this period. Ample research has come forth with telemedicine’s validity to assess PD patients virtually, including visualization of physical examinations by videotaping or video consultations. Reference Papa, Brundin and Fung1 While many participants in this study seemed indifferent to the motor examination, assessing rigidity and postural reflex impairment can be more complex for the neurologist to assess. The MDS-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) used to evaluate various aspects of PD, including motor and non-motor experiences of daily living and motor complications, has been compromised to the lack of physical examination. Reference Fasano, Antonini and Katzenschlager21,Reference Goetz, Stebbins and Luo22 Due to the inability to perform muscle rigidity and retropulsion pull testing as part of the MDS-UPDRS via videoconference, a modified version has been created that is still reliable and valid, omitting the last pieces. Reference Abdolahi, Scoglio, Killoran, Dorsey and Biglan23 Other than these two described “hands-on” maneuvers, the remaining examination of the MDS-UPDRS, including gait assessment, can be completed if patients are not at high risk of falls. Other routine testing in PD clinical appointments include the Montreal Cognitive Assessment (MoCA), diagnosis of PD, and atypical parkinsonian syndromes that all seem to be promising to be conducted over virtual means rather than in person. Reference Abdolahi, Bull and Darwin24-Reference Tarolli, Zimmerman and Goldenthal27 Many participants’ comments regarding virtual medicine align with the results from a recent online survey of 781 PD patients who expressed their main concerns with telemedicine: the lack of hands-on care, lack of intimate and personal interaction with physicians and difficulties in navigating technology. Reference Spear, Auinger, Simone, Dorsey and Francis28
To continue to support patients and professionals within the PD community regarding ongoing health care, the International Parkinson and Movement Disorder Society 29 has developed a practical step-by-step guide for implementing telemedicine. Despite some barriers, telemedicine for PD care is feasible. It can even be advantageous in terms of access to physicians, convenience, saved time, and cost reductions. Reference Adams, Myers, Waddell, Spear and Schneider30 Telemedicine can be a valuable tool for PD patients who have difficulty travelling to the specialty clinics for their appointments due to distance, mobility, or cognitive impairments. Reference Adams, Myers, Waddell, Spear and Schneider30 One study by Qiang and Marras Reference Qiang and Marras31 found virtual appointments saved PD patients an average of 209 min in travel time, 160-km travel distance and $200 (CAN).
This approach aligns with the perceptions of participants of this study who mentioned preference over the quick virtual appointments and avoiding the driving, gas, and time usually spent. In the previously mentioned online survey study, overall satisfaction rates were high, with 97% of patients and 86% of physicians reported being satisfied or very satisfied with the virtual visits. Reference Qiang and Marras31
Despite personal preferences, evidence in the field shows no significant changes in outcome between telemedicine and in-person care. Reference Beck, Beran and Biglan32-Reference Sekimoto, Oyama and Hatano34 One study comparing virtual clinical care visits via an iPad mini to regular in-person visits every two months reported no significant differences in quality of life measures including Parkinson’s Disease Questionnaire-39, UPDRS parts I and II, motor scores (UPDRS parts III and IV, Modified Hoehn and Yahr stage), mental health measures (Beck Depression Inventory), number of phone calls, or number of hospital visits. Reference Sekimoto, Oyama and Hatano34
Next Steps
To better address both motor and non-motor symptoms of PD a virtual care policy in Ontario Canada provides useful recommendations for remote clinical care. Reference Shaw, Jamieson, Agarwal, Griffin, Wong and Bhatia35 There has been a lack of long-term policy developments for virtual care. This study asked patients recommendations and opinions on future clinical care and results reported that prospective studies continue to promote patient centered outcomes and acknowledged the focus on patient’s needs during virtual care. Meaningful engagement and discussions could help understand how and why patients would use virtual care technologies. Adopting a similar approach would target a more system-wide investment in Canadian virtual care implementation strategies. Reference Shaw, Jamieson, Agarwal, Griffin, Wong and Bhatia35 Specifically, findings of the consensus policy dialogue indicated that patients recommended communication with their primary health care providers to be reciprocated within 24 h regardless of virtual method. This finding suggests that patients may not provide indicators directly about technology methods of practice but rather meaningful patient engagement in health care policy planning of virtual care could be promising future direction for research. Reference Shaw, Jamieson, Agarwal, Griffin, Wong and Bhatia35 This study aligns with patient-centered primary and community care needed to show importance for two key implications for more implementation of virtual care in clinical care. Qualitative work presented here provides the base for building up the understanding of the best way to measure the effectiveness and quality of virtual care after such a rapid shift to this modality of care provision.
Motor Symptoms
Some participants noticed worsening of their PD symptoms, including increased OFF-times, tremors/shaking, and stuttering (see Table 1; Subtheme 1.5a Worsening of Motor Symptoms). The increased psychological stress during the COVID-19 pandemic can temporarily worsen various motor symptoms, including tremor, freezing of gait, or dyskinesias. Reference Zach, Dirkx, Pasman, Bloem and Helmich36,Reference Macht, Kaussner and Möller37 Psychological stress may reduce the efficacy of dopaminergic medication, which we hypothesize may explain the reported prolongation of OFF-period duration. Reference Zach, Dirkx, Pasman, Bloem and Helmich36 Existing evidence supports that the pandemic induced a significant worsening of motor performance and motor-related disability. Further, the levodopa medication response worsened, and patients saw an increased daily OFF-time, caused by either acute systemic inflammatory response or changes in pharmacokinetics. Reference Macht, Kaussner and Möller37-Reference Umemura, Oeda and Tomita41 A study by Song et al. Reference Song, Ahn, Choi, Mun, Cho and Youn42 collected data on prescribed medications for both motor and non-motor symptoms of PD and found no significant changes of symptoms causing medication adjustment between two clinic visits during the pandemic.
We also discussed changes in patients’ exercise routines. We believe that a decrease in patients’ mobility from their usual physical activities has worsened their PD, including other therapies such as physiotherapy. A significant association between reduced exercise amount and subjective worsening or both motor and non-motor symptoms of PD was reported despite no significant change in the UPDRS part 3 scores. Reference Song, Ahn, Choi, Mun, Cho and Youn42 In a study by Zipprich et al., Reference Zipprich, Teschner, Witte, Schönenberg and Prell3 31.3% of PD patients complained about decreased mobility supporting our findings. Despite the decrease in activities, many participants in this study noted the following virtual exercise programs or spending a lot more time walking outdoors. This aligns with the findings in Zipprich et al.’s study in which 34.3% of the participants with PD had to refrain from sports activities. Reference Zipprich, Teschner, Witte, Schönenberg and Prell3 Of the total, 82.4% found alternative means to continue exercises at home or to go outside. Reference Zipprich, Teschner, Witte, Schönenberg and Prell3 It is important to note that participants’ comments occurred as the weather transitioned into the spring season. We anticipate a decrease in outdoor activities and walking during the upcoming winter months if restrictions are still in place for PD patients and anticipate an increase in feelings of isolation and confinement.
Nonmotor Symptoms
We discussed the worsening of non-motor symptoms for PD patients during the pandemic. Previous studies also reported that experiencing anxiety and worrying about the current situation were reported by 58.6% of patients. Reference Zipprich, Teschner, Witte, Schönenberg and Prell3 Worries and fears revolved around contracting the virus and being at risk due to their PD or other comorbidities, or fears of loved ones contracting it. Two of the apparent non-motor symptoms in this study were decreased sleep quality and an increase in fatigue. A recent study by Xia et al. investigated how the pandemic has affected sleep and mental health of patients with PD in comparison to healthy controls. Reference Xia, Kou and Zhang43 Results of their study showed that 68.9% of the PD patients suffered from sleep disturbance, a much higher rate than that of the general population. Further evidence shows that scores from the Hamilton Anxiety and Depression Scale on PD patients with sleep disturbances were significantly higher than PD patients who did not experience sleep disturbances, indicating that anxiety and depression are important factors affecting PD patients’ sleep quality during the pandemic. Reference Xia, Kou and Zhang43
Next Steps
For monitoring both motor and non-motor symptoms of the disease during the pandemic have been explored in a recent study by Miele et al. who investigated teleconsultations for overcoming outpatient clinic restrictions. Reference Miele, Straccia and Moccia44 They recommend an easy to fill electronic diary may be useful to track daily activities, symptoms of motor and non-motor, feelings and general health. The electronic diary is available for both iOS and Android platforms and is called “The Parkinson’s diary” on the app store. Reference Miele, Straccia and Moccia44 This new strategy is based on similar smartphone application research with a strong correlation in the MDS-UPDRS-III score that shows promising results for evaluating clinical signs that otherwise could not be collected virtually. As our results show that PD patients with both motor and non-motor symptoms have been impacted during the pandemic in varying ways therefore, we would support the recommendation by Miele and colleagues for PD patients to monitor physical and mental status during the pandemic.
Challenges and Future
We identified some challenges reported by PD participants, including struggles with changes in an exercise routine, feelings of isolation and boredom, and personal concerns about what the new normal will be moving forward. In the study by Zipprich et al., Reference Zipprich, Teschner, Witte, Schönenberg and Prell3 72.7% of participants reported changes in behaviors since COVID-19 emerged. Their results are aligned with our findings that participants’ fears and concerns are that the virus is dangerous in general or to them personally and see themselves as patients of risk. Reference Zipprich, Teschner, Witte, Schönenberg and Prell3 Isolation and limited visitation with family and friends have been common responses expressed by participants. Other challenges include uncertainty about economic and social developments for the future and what clinical care will look like if this continues. On the other hand, we found a handful of participants who took a positive stance on the impacts of COVID-19, including statements on enjoying a slower-paced life. Future research should be conducted to examine if there are positive impacts on the pandemic’s behavioral changes as most of the existing evidence has focused on the concerning impact and effects. Prospective research should also consider more patient engagement in virtual care policy and implementation.
Limitations
The present study has several limitations. This study used a pre-selected sample of patients who have shown interest in research or have had possibly more research exposure than the general PD population of the clinic. Another limitation of the study is selection bias favoring this pre-selected sample that perhaps were relatively healthier and had readily accessible technology including phone, internet, email. We aimed at accommodating for less accessible technology by incorporating oral consent via phone for those patients who were unable to access internet and computer. Due to the restrictions and suspension of in-person clinical visits, we were not able to perform any clinical assessments such as MDS-UPDRS at the time; however, it is worth looking into the use of the virtual adaptations to assessments as noted in the study for future studies where in-person assessment is not possible. Future work should aim to incorporate both the perspectives of patients with PD exploring more symptoms and managing the disease. While our study was inclusive of caregivers/spouses of participants if they wished to join, our main interest was at the lived experiences of those with the PD diagnosis therefore we did not have enough caregivers attend or data to generate unique themes across caregivers for this study. A prospective study could be useful in exploring the caregivers lived experiences during the pandemic.
Conclusion
In conclusion, this study provided an overview of PD participants’ experiences during COVID-19 with an emphasis on clinical aspects and remote care. Three major themes PD patients reported as a result of the pandemic were impacts on clinical care including, personal life, and changes in attitudes and perceptions. The most significant theme was how the pandemic affected PD clinical care including health care and medication limitations, how the transition to virtual care affected PD patients and what is needed moving forward to improve telehealth and symptom management. Suggestions from our participants include increased communication with specialists around clinical care and recommendations for continued clinical management of symptoms amid the pandemic. Overall, this study provides a unique opportunity for researchers to better understand the lived experiences of PD patients in all aspects of their life suggesting innovative means are needed for facilitating virtual health care medicine and increased social interaction to help mitigate future pandemics or anticipated futures waves of COVID-19, extreme weather phenomena or other similar emergencies.
Acknowledgments
This research is supported by the Movement Disorders Program, part of the Cumming School of Medicine at the University of Calgary, and Calgary Parkinson Research Initiative (CaPRI), also supported in-kind the Brain and Mental Health Research Clinics, Hotchkiss Brain Institute, University of Calgary.
Funding
This work is supported by an award from the University of Calgary Cumming School of Medicine COVID Rapid Response Clinical Research Fund (Grant number: CRF-COVID-202003). Direct and in-kind funding was also provided by the Brain and Mental Health Research Clinics, a part of Hotchkiss Brain Institute (https://brainandmentalhealthclinics.ca/).
Conflict of Interest
None of the authors have any conflict of interest or information to disclose in relation to this study.
Statement of Authorship
PR is the principle investigator, who designed and led the research, oversaw qualitative analysis, and manuscript writing. BA conducted interviews, completed qualitative analysis, and is first author on the manuscript. VB and DM are members of the project team, provided input into the study design, contributed to the manuscript writing and review.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2021.70.