Introduction
Parkinson’s disease (PD) is the most common movement disorder, and it is chronic and progressive in nature. Reference DeMaagd and Philip1 The prevalence of PD in the general population is approximately 0.3% of the entire population and 1% of those over 60 years old. Reference Rizek, Kumar and Jog2 Furthermore, the crude prevalence rate in Asian countries specifically ranges from 15 to 328 per 100,000 individuals. Reference Chen and Tsai3,Reference de Lau and Breteler4
Upper extremity disorders are frequently reported in PD as well, especially the hand dysfunction, is a common presentation of PD. Reference Proud, Miller, Martin and Morris5 It affects the functionality of the hand, which results in impaired manual dexterity, fine motor skills deficits, poor grip force control and inability to perform coordinated movements in early stages due to unilateral tremor, mild hypokinesia and rigidity. Some common issues encountered include reduced movement speed and amplitude, poor sequential task performance, disordered fine manipulation of hand involving reach-to-grasp movements, and gripping and manipulating objects using assistive devices, such as crutches and wheelchairs. Furthermore, dexterity difficulties are the second contributor to PD’s impairment following ambulation, making it a burden to the disease. Reference Proud, Miller, Martin and Morris5–Reference Corrêa, de Vieira and de Souza6 Additionally, during their middle stages, participants encountered heightened challenges in self-care activities due to bilateral bradykinesia, axial and distal rigidity, poor synchronisation and torque modulation, rendering their activity limitations more complex. These impairments make them highly dependent on assistive devices and caregiver assistance. In the late stage of PD, limited functional activities and poor structural abilities have been observed due to severe rigidity and joint stiffness, eventually leading to difficulties in daily and self-care activities, in addition to the loss of independence and reduced quality of life (QoL) throughout the illness. Reference Franciotta, Maestri, Ortelli, Ferrazzoli, Mastalli and Frazzitta7,Reference Quinn, Busse and Dal Bello-Haas20
As dexterity performance is slowly deteriorating, several management protocols and interventions have been considered for use in PD rehabilitation programmes that focus on improving hand functionality. However, based on the evidence, majority of the treatment protocols are aimed to improve the gait and lower limb functions.
To date, no evidence on which intervention could best enhance hand dexterity in PD individuals has been investigated. Therefore, this research aimed to determine the best treatment available to improve hand dexterity in patients with PD, by comparing different types of interventions needed to enhance their QoL and well-being, while allowing them to perform functional tasks as independently as possible. This systematic review also aimed to provide better hand dexterity improvement options in individuals with PD in the near future. All in all, the primary objective of this systematic review was to identify the best physiotherapy intervention to improve hand dexterity in PD patients. The secondary objectives were to identify the hand dexterity interventions available for PD patients and determine the quality of these interventions.
Research methodology
Search protocol and registration
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. Following the PRISMA guideline ensures that a systematic review or a meta-analysis is better documented in the way of transparency and accuracy. This systematic review was registered with PROSPERO (CRD42020219788).
Search strategy
The development of the search strategy, which was in accordance with the Problem/Population, Intervention, Comparison, Outcome (PICO) format, was discussed among three reviewers (LMH, CPK and FWH). The developed search strategies were adapted for use in all the selected databases, summarises in Table 1. The relevant keywords and search terms were decided, summarises in Table 2, which are (1) Parkinson*; (2) “hand dexterity” OR “manual dexterity”; (3) physiotherapy; (4) physiotherapy intervention OR technique OR management OR rehabilitation. Formal searching of the databases was started once the consistency within the search process was achieved. The most relevant articles were identified by searching through the following databases: Clinical Key; Cochrane Library; Ovid; Physiotherapy Evidence Database (PEDro); PubMed; PubMed Central; Science Direct; Scopus. These databases were selected because they are related to healthcare services and rehabilitation provisions, and contain predominantly peer-reviewed journal articles, where studies relevant to the objectives of this systematic review could be easily identified. Grey literature search (Google Scholar) was undertaken with the first ten pages of the results reviewed. Hand searching through the reference list of all identified and relevant articles were also performed. All searches were performed between July 2020 and November 6, 2020.
Table 1. Boolean operators SEARCH STRATEGY

Table 2. PICO table

Study design
Only randomised controlled trials (RCTs) were included in this review.
Population
Studies were included if the subjects fulfilled the following criteria: (1) adults aged 18 and over; (2) clinically diagnosed with PD with no exclusion based on type. Studies including a mixed sample of participants, such as patients with conditions other than PD, were excluded. No restrictions were made in relation to gender, disease duration and disease severity.
Intervention
A variety of hand dexterity rehabilitation programmes and interventions based on physiotherapy practice were included to gain a comprehensive overview of current approaches. The interventions were directed to the PD patient themselves. The type of treatment was not limited to a specific mode as all treatments were included.
Outcome measures
Primary outcomes of interest were hand dexterity and ADL. Secondary outcomes of interest were upper limb motor function, QoL, adverse events, adherence and compliance and quality of intervention.
Study selection
Following the search through the databases, the initial result was finalised, and the title, abstract and full text of all studies were independently screened by three reviewers (LMH, CPK and FWH) to identify studies for possible inclusion in the review, as well as removing duplicate articles. The inclusion criteria for study selection were (1) studies that included adult participants diagnosed with PD, (2) RCTs that evaluated the effects of physiotherapeutic interventions in improving hand dexterity, and (3) full-text studies published in English between 2010 and 2020. Papers that did not meet the inclusion criteria were excluded. Disagreements that arose were resolved through discussion or with the help of an experienced external reviewer (DTV) to provide an independent decision when necessary.
Methodological quality
The modified McMaster Critical Appraisal Tool Reference Law, Stewart and Pollock8 was used to assess the methodological quality of the eligible studies. The tool scoring used a dichotomous rating scale of yes/no options to rate the methodological quality of the study where Yes = 1 and No = 0, with a maximum score of 14.
The risk of bias for every study was also determined. The Cochrane Risk of Bias tool Reference Higgins, Thomas and Chandler9 was used to identify the risk of bias for every study. The risk of bias of each study was classified as either high, low or unclear risk. Articles that fulfilled at least four of the six criteria were considered to be at low risk of bias.
The evidence hierarchy from the National Health and Medical Research Council (NHMRC) Reference Coleman, Norris and Weston10 Designation of Levels of Evidence was used to measure the level of evidence of the individual paper. The study design of each selected study was assessed according to its rank in the hierarchy system, which classified the body of evidence into four levels (Level I, Level II, Level III-1, Level III-2, Level III-3, Level IV). The grades of recommendations from the NHMRC guideline were used to assess the individual components of the studies. Four components were graded, namely study quality, findings consistency, clinical impact and results generalisability, with “Excellent,” “Good,” “Satisfactory” or “Poor.” Any disagreements were resolved through discussion or with the help of an experienced external reviewer (DTV) only when necessary.
Data extraction
Customised data extraction tables were constructed and developed for this review to organise and summarise information from the studies. Data from the studies were then extracted onto the tables for data collection purposes. The data extraction tables contained information such as study characteristics, participants details, outcome measures, intervention outlines and study results. Any disagreements or conflicts were resolved through discussion or with the help of an external reviewer (DTV) when the group could not come to an agreement. Study authors of the articles were contacted for additional information when necessary.
Data synthesis
Descriptive data synthesis of narrative summary and tabulation was used in this review due to the disparate outcome measures and interventions employed in each selected study. A general descriptive discussion of the research findings gave an overview of the study results and its importance. The characteristics of the studies were presented in multiple tables. This allows a comparison of results to be made between studies, and the reviewer’s views about the research can then be formulated. For studies that included effect size in its result, the following range of effect size was used as a standard in this review: 0.2 to 0.49 was considered to be small, 0.5 to 0.79 was considered to be medium, and 0.8 or above was considered to be large. Reference Chung and Mak11
Results
Search results
A total of 6,114 studies were identified through initial database searches using the search strategy. Titles and abstracts of 2,510 studies were screened based on the established criteria. Studies that did not meet the predefined inclusion criteria were excluded. From these, 27 full-text articles were evaluated for eligibility. Following a thorough final screening, 11 full-text studies were eligible for inclusion in this systematic review, Reference Allen, Song and Paul12,Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Cikajlo and Peterlin Potisk14,Reference Taghizadeh, Azad and Kashefi21–Reference Vanbellingen, Nyffeler and Nigg22 while 16 full-text articles were excluded for not meeting the inclusion criteria. The reasons for exclusion included other focus of study (n = 3), other study design (n = 6), other study population (n = 4) and other outcome measure (n = 3). A PRISMA flow diagram that presents the study selection process for searches is outlined in Figure 1.

Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart.
Study characteristics
All studies were published between 2011 and 2020. Of the 11 articles included in this review, a plurality was conducted in Spain, Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15,Reference Mateos‐Toset, Cabrera‐Martos, Torres‐Sánchez, Ortiz‐Rubio, González‐Jiménez and Valenza19 whereas the others came from Korea, Reference Lee, Lee and Hwang18 Slovenia, Reference Cikajlo and Peterlin Potisk14 Australia, Reference Allen, Song and Paul12 Thailand, Reference Vanbellingen, Nyffeler and Nigg22 Italy, Reference Ferrazzoli, Ortelli and Zivi16 Switzerland, Reference Taghizadeh, Azad and Kashefi21 Iran, Reference Quinn, Busse and Dal Bello-Haas20 and the USA. Reference Horin, McNeely and Harrison17
Sample characteristics
A total of 11 studies involving 647 participants with PD were included for analysis in this review. Of the 11 studies, 399 males (59%) and 272 females (41%) were reported on baseline, with mean ages ranging from 59.15 ± 11.26 years to 83.0 ± 7.6 years. Study sample sizes varied from 20 to 234, and mean disease duration reported in most samples was more than six years. Disease severity of the included participants ranged from stages I to IV on the Hoehn and Yahr scale, with no study recruiting patients with stage-V PD. The participant characteristics during the baseline assessments are summarised in Table 3.
Table 3. Participants baseline characteristic

SD = Standard Deviation; H&Y = Hoehn and Yahr; EG = experimental group; CG = control group; NAD = not addressed.
Methodological quality
A summary of critical appraisal scores using the modified McMaster Critical Appraisal Tool for all study methodologies are given in Table 4.
Table 4. Methodological quality

1. A clearly stated study purpose; 2. Sufficient background literature; 3. Study design; 4a. Sample size; 4b. Detailed sample description; 4c. Sample size justification; 5a. Use of reliable outcome measures; 5b. Use of valid outcome measures; 6a. Detailed intervention description; 6b. Absence of contamination; 6c. Absence of cointervention; 7a. Statistical significance reported; 7b. Appropriate analysis methods; 7c. Clinical importance reported; 7d. Dropouts reported; 8. Appropriate conclusion.
Y = yes; N = no; NAD = not addressed; RCT = randomised controlled trial.
Four studies Reference Allen, Song and Paul12,Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Ferrazzoli, Ortelli and Zivi16,Reference Taghizadeh, Azad and Kashefi21 have scored 13 out of 14 for their relatively good methodology quality following the methodological quality assessment. The remaining seven studies achieved a moderate methodological quality rating, with scores ranging from 10 to 11.
Table 5 shows the risk of bias for each of the included studies. Four of the 11 studies were considered to be at low risk of bias. Reference Allen, Song and Paul12,Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Mateos‐Toset, Cabrera‐Martos, Torres‐Sánchez, Ortiz‐Rubio, González‐Jiménez and Valenza19,Reference Taghizadeh, Azad and Kashefi21 The remaining 7 studies were considered as high or unclear risk of bias.
Table 5. Risk of bias

Table 6 summarises the ratings of the NHMRC Evidence Statement Form. The body of evidence showed that the interventions aimed to improve hand dexterity might be effective. However, the results should be interpreted with caution due to the varied outcome measures, and interventions used.
Table 6. National Health and Medical Research Council body of evidence

PD = Parkinson’s disease; RCT = randomised controlled trial.
Interventions
The overview of the contents of the interventions including the quality of each intervention for both experimental and control groups is provided in Table 7. The intervention period varied between studies, with the total training period ranging from a 15-minute single session to 12 weeks of training. The intervention settings differed between studies, with only four studies taking place in a home-based setting, Reference Allen, Song and Paul12,Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Horin, McNeely and Harrison17,Reference Vanbellingen, Nyffeler and Nigg22 rehabilitation centre, Reference Cikajlo and Peterlin Potisk14 Aparkan Association, Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15 hospital, Reference Ferrazzoli, Ortelli and Zivi16 laboratory, Reference Mateos‐Toset, Cabrera‐Martos, Torres‐Sánchez, Ortiz‐Rubio, González‐Jiménez and Valenza19 and neurologic clinic. Reference Vorasoot, Termsarasab and Thadanipon23 Two studies did not specify the setting of the study. Reference Lee, Lee and Hwang18,Reference Taghizadeh, Azad and Kashefi21 The intervention quality varied in frequency from two times a week to daily sessions, and duration lasted from 15 minutes to 3 hours per session.
Table 7. Contents of the interventions

NAD = not addressed; N/A = not applicable; UL = upper limb; LMC = Leap Motion Controller; MIRT = Multidisciplinary Intensive Rehabilitation Treatment; CIMT = constraint-induced movement therapy; ROM = range of motion; SMT = sensory-motor training; HOMEDEXT = home-based dexterity programme.
The selected study evaluated the effects of intervention such as Exergames, Reference Allen, Song and Paul12 a single hand-exercise session, Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13 Immersive 3D virtual, Reference Cikajlo and Peterlin Potisk14 multidisciplinary, aerobic, motor-cognitive and intensive rehabilitation treatment (MIRT), Reference Ferrazzoli, Ortelli and Zivi16 therapeutic putty exercises, Reference Mateos‐Toset, Cabrera‐Martos, Torres‐Sánchez, Ortiz‐Rubio, González‐Jiménez and Valenza19 home-based dexterity programme, Reference Taghizadeh, Azad and Kashefi21 handwriting exercise, Reference Vanbellingen, Nyffeler and Nigg22 and one study used a smartphone application. Reference Horin, McNeely and Harrison17 Majority of the study aimed to evaluate the effects on manual dexterity, hand grip, functional improvements, ADL performance as well as the levels of satisfaction, motivation aspects and compliance among patients in mild-to-moderate stages of the disease. The game-based study investigated the acceptability and feasibility of these games, Reference Allen, Song and Paul12,Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15 clinical effectiveness between immersive and non-immersive virtual reality exergaming. Reference Cikajlo and Peterlin Potisk14 The study used a mobile health smartphone application examined the effect of adherence and assessed usability of the mHealth application in addition to gait, speech and dexterity. Reference Horin, McNeely and Harrison17
Effects of interventions
An overview of the measures for dexterity, ADLs, upper limb motor function, QoL and other miscellaneous outcomes used for each study along with its main findings are presented in Tables 7 and 8.
Table 8. Major findings
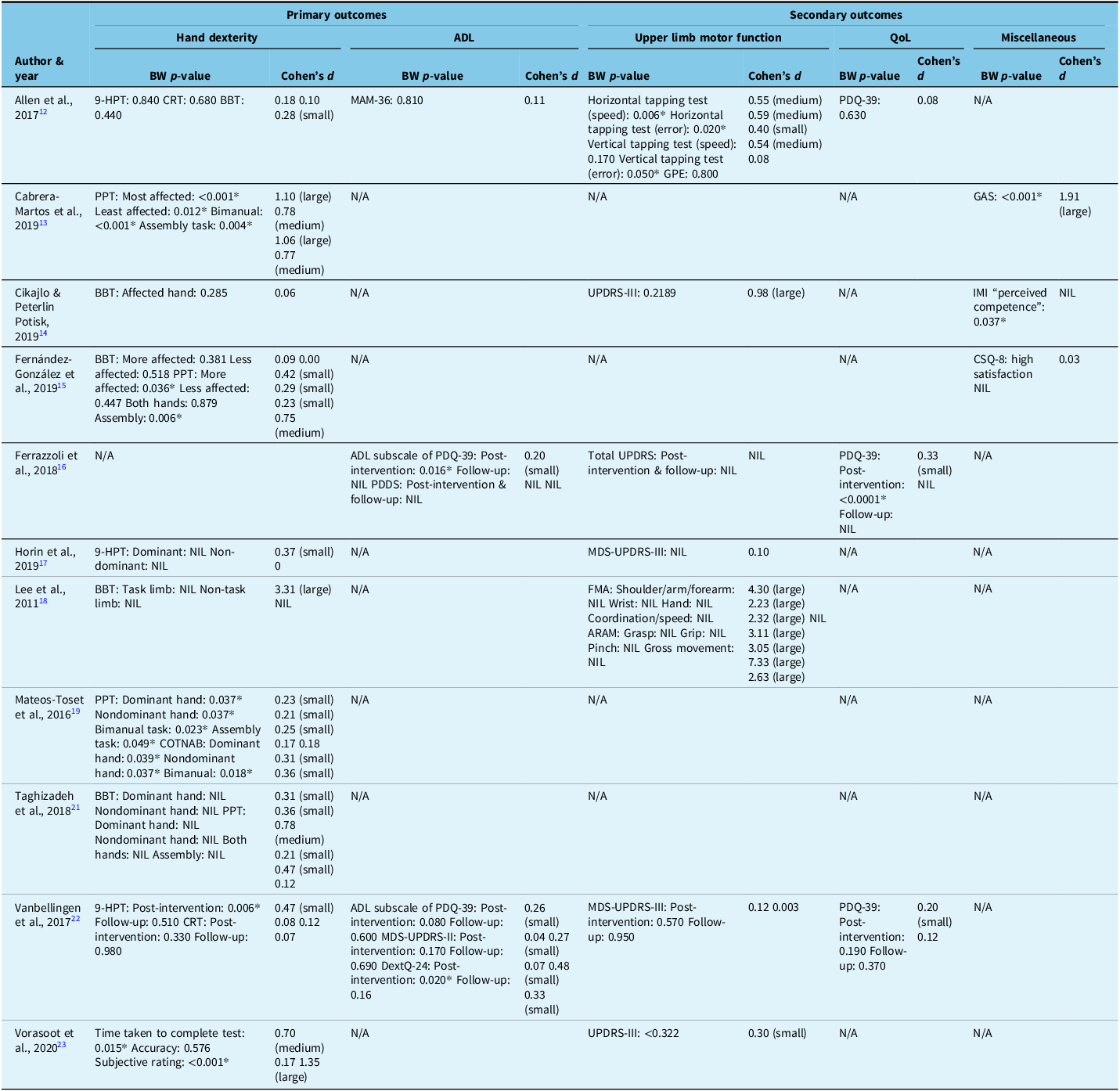
ND = no difference; N/A = not applicable; NIL = not in the list; BW = between-groups; Hand dexterity: 9-HPT = Nine-Hole Peg Test; CRT = coin rotation task; BBT = Box and Block Test; PPT = Purdue Pegboard Test; COTNAB = Chessington Occupational Therapy Neurologic Assessment Battery; ADL = Activities of daily living: MAM-36 = Manual Ability Measure-36 questionnaire; PDQ-39 Parkinson’s Disease Questionnaire; PDDS = Parkinson’s Disease Disability Scale; MDS-UPDRS = Movement Disorders Society Unified Parkinson’s Disease Rating Scale; Upper limb motor function: GPE = Global Perceived Effect scale; UPDRS = Unified Parkinson’s Disease Rating Scale; MDS-UPDRS = Movement Disorders Society Unified Parkinson’s Disease Rating Scale; FMA = Fugl-Meyer Assessment; ARAM = Action Research Arm Test; QoL = Quality of life: PDQ-39 Parkinson’s Disease Questionnaire Miscellaneous: GAS = Goal Attainment Scaling; IMI = Intrinsic Motivation Inventory; CSQ-8 = Client Satisfaction Questionnaire.
*= statistically significant (p<0.05).
Primary outcome – hand dexterity
A total of five Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15,Reference Mateos‐Toset, Cabrera‐Martos, Torres‐Sánchez, Ortiz‐Rubio, González‐Jiménez and Valenza19,Reference Taghizadeh, Azad and Kashefi21,Reference Vanbellingen, Nyffeler and Nigg22 out of 11 studies Reference Allen, Song and Paul12–Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15,Reference Horin, McNeely and Harrison17–Reference Vanbellingen, Nyffeler and Nigg22 that measured hand dexterity using different outcome measures reported significant between-group results.
Six out of 11 studies had small effects size. Reference Allen, Song and Paul12,Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15,Reference Horin, McNeely and Harrison17,Reference Mateos‐Toset, Cabrera‐Martos, Torres‐Sánchez, Ortiz‐Rubio, González‐Jiménez and Valenza19–Reference Taghizadeh, Azad and Kashefi21 The study by Fernández-González et al. Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15 and Taghizadeh et al. Reference Quinn, Busse and Dal Bello-Haas20 produced both small and medium effect sizes in different outcomes. Four out of the 11 studies Reference Allen, Song and Paul12,Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Horin, McNeely and Harrison17,Reference Vanbellingen, Nyffeler and Nigg22 were conducted in a home-based setting, had both medium and large effect sizes in the outcomes, while three studies Reference Cikajlo and Peterlin Potisk14,Reference Ferrazzoli, Ortelli and Zivi16,Reference Vorasoot, Termsarasab and Thadanipon23 are conducted in hospital or clinic-based settings. Most of the studies had an average duration of 4–12 weeks and were administered with an average frequency of 3 days per week. The study by Lee et al. Reference Lee, Lee and Hwang18 involved a 4-week intervention which consisted of five sessions per week, each lasting for 3 hours demonstrated a significant large effect size.
Primary outcome – activities of daily living
Only two Reference Ferrazzoli, Ortelli and Zivi16,Reference Vanbellingen, Nyffeler and Nigg22 out of three studies Reference Allen, Song and Paul12,Reference Ferrazzoli, Ortelli and Zivi16,Reference Vanbellingen, Nyffeler and Nigg22 that assessed ADL showed significant between-group results. Both the studies reported a small effect size in ADL. Out of these three studies two of them were received home-based exercise game Reference Allen, Song and Paul12,Reference Vanbellingen, Nyffeler and Nigg22 with an average frequency of 3 days per week.
Secondary outcome – upper limb motor function
Two Reference Allen, Song and Paul12,Reference Vanbellingen, Nyffeler and Nigg22 of the seven studies Reference Allen, Song and Paul12,Reference Cikajlo and Peterlin Potisk14,Reference Ferrazzoli, Ortelli and Zivi16–Reference Lee, Lee and Hwang18,Reference Taghizadeh, Azad and Kashefi21–Reference Vanbellingen, Nyffeler and Nigg22 that assessed upper limb motor function reported significant between-group results on motor function after the intervention. Two studies had small effect size Reference Allen, Song and Paul12,Reference Vanbellingen, Nyffeler and Nigg22 and a study by Allen et al. Reference Allen, Song and Paul12 also showed medium effect size. On the other hand, large effect size was reported by two studies. Reference Cikajlo and Peterlin Potisk14,Reference Lee, Lee and Hwang18
Secondary outcome – quality of life
Only Reference Ferrazzoli, Ortelli and Zivi16 one of three studies Reference Allen, Song and Paul12,Reference Ferrazzoli, Ortelli and Zivi16,Reference Taghizadeh, Azad and Kashefi21 reported that assessed QoL shows significant between-groups improvement was perceived after their interventions in improving QoL. Also, two studies Reference Ferrazzoli, Ortelli and Zivi16,Reference Taghizadeh, Azad and Kashefi21 had produced a small effect size.
Secondary outcome – miscellaneous
In the study conducted by Cabrera-Martos et al, Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13 the between-groups result on Goal Attainment Scaling (GAS) reported a significant achievement with a large effect size.
The results of the study conducted by Cikajlo & Peterlin Potisk Reference Cikajlo and Peterlin Potisk14 on Intrinsic Motivation Inventory (IMI) reported significant differences in “perceived competence” and increased “effort/importance” in the experimental group. The between-group result revealed significant differences in “perceived competence.”
The study by Fernández-González et al. Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15 used Client Satisfaction Questionnaire (CSQ-8) for user satisfaction evaluation. The result for the experimental group and control group obtained a similar satisfaction score with no effect size.
Secondary outcome – adverse events
Two studies Reference Allen, Song and Paul12,Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15 have examined adverse side effects such as muscle soreness and undue fatigue. However, none of the participants reported experiencing adverse events following their participation in the intervention. To evaluate adverse side effects comprehensively, a follow-up assessment is necessary, and conducting more intensive dosage regimens is required to verify these results thoroughly. Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15
Secondary outcome – adherence and compliance
Nine studies Reference Allen, Song and Paul12–Reference Lee, Lee and Hwang18,Reference Taghizadeh, Azad and Kashefi21,Reference Vanbellingen, Nyffeler and Nigg22 have assessed adherence and compliance, with five Reference Allen, Song and Paul12,Reference Ferrazzoli, Ortelli and Zivi16–Reference Lee, Lee and Hwang18,Reference Taghizadeh, Azad and Kashefi21 reported dropouts due to personal reasons. In addition, the study conducted by Allen et al. Reference Allen, Song and Paul12 focused on exercise compliance, and participant feedback showed that the results in the experimental group were satisfying. The study conducted by Vanbellingen et al. Reference Taghizadeh, Azad and Kashefi21 also required participants to document details of the interventions in a diary. The results showed that the experimental group has higher adherence than the control group. However, the protocol was deemed to bring patients fatigue and daily stress, and lack of motivation. Next, the study by Fernández-González et al. Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15 and Vorasoot et al. Reference Vanbellingen, Nyffeler and Nigg22 reported that all subjects showed excellent adherence and compliance to protocol. Finally, the adherence of the experimental group to the mHealth application dexterity exercises in the study conducted by Horin et al. Reference Horin, McNeely and Harrison17 was lower than the other studies. The exit survey regarding the mHealth application completed by the subjects from the experimental group revealed that there is more negative feedback than positive feedback due to technical issues and repetitive exercises.
Discussion
This systematic review investigated the current intervention available to improve hand dexterity in PD patients, with the primary objective of identifying the best intervention in enhancing the dexterous hand function of PD patients. This review included 11 RCTs with moderate to excellent methodological quality. Quantitative meta-analysis was not carried out in this review due to the use of various outcome measures and diverse interventions. In addition, there were also several methodological flaws and risks of bias in the included studies following the methodological quality assessments. Hence, the dearth of evidence made it difficult to support any one intervention as the best intervention when compared to the other PD treatments.
Based on the data extracted, improvements in primary and secondary outcomes of interest were reported in each study. In terms of primary outcomes, eight studies Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13–Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15,Reference Lee, Lee and Hwang18–Reference Vanbellingen, Nyffeler and Nigg22 reported significant results on hand dexterity, and two studies Reference Ferrazzoli, Ortelli and Zivi16,Reference Taghizadeh, Azad and Kashefi21 showed significant results on ADL. As for secondary outcomes, four studies Reference Allen, Song and Paul12,Reference Ferrazzoli, Ortelli and Zivi16,Reference Lee, Lee and Hwang18,Reference Vanbellingen, Nyffeler and Nigg22 reported improvements in motor function, two studies Reference Ferrazzoli, Ortelli and Zivi16,Reference Taghizadeh, Azad and Kashefi21 reported significant results in improving QoL, and two studies which were conducted by Cabrera-Martos et al. Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13 and Cikajlo & Peterlin Potisk Reference Cikajlo and Peterlin Potisk14 showed significant results on Goal Attainment Scaling and IMI under miscellaneous outcome measures, respectively.
In addition, no studies reported adverse events after the intervention, indicating that their interventions may be safe for individuals with PD. Among the nine studies Reference Allen, Song and Paul12–Reference Lee, Lee and Hwang18,Reference Taghizadeh, Azad and Kashefi21,Reference Vanbellingen, Nyffeler and Nigg22 that reported dropouts during the study period, most reasons were unrelated to the intervention. However, there were subjects from the experimental group that discontinued participation Reference Ferrazzoli, Ortelli and Zivi16,Reference Horin, McNeely and Harrison17,Reference Taghizadeh, Azad and Kashefi21 without providing specific reasons. In general, studies that showed high adherence or compliance, by way of dropout rate, total hour of training, or satisfaction, were Allen et al, Reference Allen, Song and Paul12 , Cabrera-Martos et al, Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13 Cikajlo & Peterlin Potisk, Reference Cikajlo and Peterlin Potisk14 Fernández-González et al, Reference Fernández-González, Carratalá-Tejada and Monge-Pereira15 Vanbellingen et al. Reference Taghizadeh, Azad and Kashefi21 and Vorasoot et al. Reference Vanbellingen, Nyffeler and Nigg22
The study conducted by Horin et al. Reference Horin, McNeely and Harrison17 did not provide any guidance from the therapist to the participants as they had to perform the exercises independently and depend solely on the mHealth application. The study results reported no improvements after the intervention and suggested that using the application alone was insufficient to significantly improve motor function in PD patients. This result was shown to be valid according to Keus et al, Reference Vorasoot, Termsarasab and Thadanipon23 who stated that supervised training in the short term typically produces a better result than non-supervised programmes. Dexterity deficits primarily affect the patients’ daily activity and participation, which often occur within the community setting, particularly the home environment. Thus, rehabilitation focused on improving ADLs should be delivered in a real-world context as it is closer to the patients’ daily environment. Reference Vorasoot, Termsarasab and Thadanipon23 Home-based rehabilitation allows patients to practice movements more comfortably and allows therapists to evaluate patient performance and intervention effect with ease. Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13 In short, it is suggested that rehabilitation with minimal therapist supervision taking place in a home-based setting undoubtedly were more convenient to PD patients and produced a better result. The convenient home-based setting was employed by four of the 11 included studies. Reference Allen, Song and Paul12,Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13,Reference Horin, McNeely and Harrison17,Reference Taghizadeh, Azad and Kashefi21
According to Ackerman et al, Reference Ackerman, Asindua and Blouin25 a multidisciplinary rehabilitation service is effective and efficient as it ensures the continuity of care and maximises patient functional outcomes. However, it may also be inconvenient for patients and healthcare personnel to liaise with one another on the rehabilitation programme. For instance, although the study conducted by Ferrazzoli et al. Reference Ferrazzoli, Ortelli and Zivi16 showed significant improvements in several aspects, it was multidisciplinary and involved different healthcare professions. At the end of the study period, it was reported that three participants each discontinued participation and did not attend the follow-up assessment without providing specific reasons. Hence, for outpatient rehabilitation, a multidisciplinary rehabilitation programme may not be feasible for mainstream care.
According to Abbruzzese et al, Reference Abbruzzese, Marchese and Avanzino26 significant improvements observed after physiotherapy interventions were usually not present after three months. This statement is supported by the two studies Reference Ferrazzoli, Ortelli and Zivi16,Reference Vanbellingen, Nyffeler and Nigg22 in our review, showing that hand dexterity improvement were not sustained at follow-up. This suggested that an individualised long-term training might be needed to maintain the improvement in hand function.
This review aimed to suggest a feasible intervention protocol to improve hand dexterity in PD patients that could be incorporated into one’s daily routine. The intervention protocol of the three studies by Ferrazzoli et al, Reference Ferrazzoli, Ortelli and Zivi16 Lee et al. Reference Lee, Lee and Hwang18 and Taghizadeh et al. Reference Taghizadeh, Azad and Kashefi21 had a duration of 1 to 3 hours per session for 5 to 6 days per week, which could be less suitable for integration into their routine. The European Physiotherapy Guideline for Parkinson’s Disease Reference Vorasoot, Termsarasab and Thadanipon23 recommended that rehabilitation for complex motor sequences on gait and functional mobility should include three 30-minute sessions weekly for three weeks. It was also suggested that at least four weeks of training is needed to show significant improvements in patient functional abilities. The optimal parameter for a rehabilitation programme would be a minimum of 30 minutes duration, three sessions per week for three weeks based on the above recommendations. Studies with such parameters include Allen et al, Reference Allen, Song and Paul12 Cikajlo & Peterlin Potisk, Reference Cikajlo and Peterlin Potisk14 Vanbellingen et al, Reference Vanbellingen, Nyffeler and Nigg22 and Vorasoot et al. Reference Vorasoot, Termsarasab and Thadanipon23
Reach-to-grasp movements and object manipulation can be improved with the help of cueing strategies, provision of augmented feedback and by avoiding dual-tasking, Reference Abbruzzese, Marchese and Avanzino26 which is adopted for use by eight studies included in the review. Reference Allen, Song and Paul12–Reference Ferrazzoli, Ortelli and Zivi16,Reference Mateos‐Toset, Cabrera‐Martos, Torres‐Sánchez, Ortiz‐Rubio, González‐Jiménez and Valenza19,Reference Quinn, Busse and Dal Bello-Haas20,Reference Vanbellingen, Nyffeler and Nigg22
Furthermore, the study by Cabrera-Martos et al. Reference Cabrera-Martos, Ortiz-Rubio and Torres-Sánchez13 that evaluated the effect of goal setting on an individualised programme had conveyed important information. The study results revealed that a goal-oriented intervention focusing on specific functional goals based on tasks and task components significantly improved manual dexterity and promoted goal achievement in PD subjects. The impact on participant motivation was also positively influenced, thereby increasing the attention of patients and exercise repetition. Therefore, this indicates that setting a set of specific functional goals before planning a treatment programme is essential in rehabilitation.
After thoroughly evaluating all the studies to identify the hand dexterity intervention that is most likely to produce the most significant results in PD patients, based on the aforementioned recommendations to be categorised as a good intervention, only one Reference Taghizadeh, Azad and Kashefi21 out of the 11 studies had satisfied most of the suggestions. The study on HOMEDEXT programme focusing on the key components of dexterity had shown significant improvements in hand dexterity, ADL and QoL, with no adverse event reported, high adherence to the intervention, sufficient instruction given and the quality of the intervention protocol was not too long and not too frequent, and the intervention took place in a home-based setting. This suggested that the study intervention may have the potential and feasibility to improve the hand dexterity of PD patients in mainstream care.
Limitations
There are several other limitations in this review. Potential bias might have arisen in the review process. It was possible to overlook some promising and relevant studies despite the execution of an in-depth, extensive and comprehensive database search.
The sample age, disease stage and disease severity of the study population were not controlled in this review. Hand dexterity performance may deteriorate as people age or symptoms worsen. Thus, this might have influenced the study results, as younger patients with less severe PD would have yielded a better result.
Some studies did not provide information on their sample size calculation. Without information on the sample size justification, it was difficult to know if the power was sufficient with the given sample size. Next, the primary focus of the study with a small sample size was to examine the intervention usability. Hence, the result did not have sufficient power to evaluate the effectiveness of the intervention. These may predispose the study results to different types of error, thereby increasing the risk of bias and affecting the validity of a study result.
Most studies only evaluated the immediate effects of intervention within a short study period. The follow-up period for the included studies was either absent or short, up to only three months long. Nine out of a total of 11 studies did not observe whether the improvements have been sustained over time. They only assessed the performance of their participants at baseline and post-intervention.
A further limitation was the potential publication bias as this review only included English language full-text RCTs published within the last 10 years. High-quality studies might be available in papers with other types of study design and languages published beyond the past 10 years.
Future recommendations
Well-designed RCTs and a more extended follow-up period are needed to evaluate the efficacy, effectiveness and impact of treatments on PD subjects. Besides, the studies should also reflect the current practice of the rehabilitation field to allow for replication of interventions by the physiotherapists as well as other healthcare personnel. Methodological quality and reporting of a study should be improved to minimise the methodological flaws and risk of bias. More studies on the current topic are needed to determine the applicability of interventions in people with PD according to different characteristics of participants and disease. Detailed information on interventions, aimed to enhance dexterity function and the content and delivery of training, should be further studied to serve as a guideline for upper extremity rehabilitation. In essence, additional study is needed to verify our findings based on a firm body of evidence. Consider setting a cut-off score for the methodological quality assessment to avoid the inclusion of low-quality studies in the review only if necessary.
Conclusion
In conclusion, this systematic review provides valuable insights into interventions aimed at improving hand dexterity in Parkinson’s disease (PD) patients. Despite the limitations and methodological flaws in the included studies, significant improvements in hand dexterity, activities of daily living (ADL) and quality of life (QoL) were reported across multiple studies. Importantly, no adverse events were reported, indicating the safety of these interventions for PD patients. Home-based rehabilitation programmes emerged as a promising approach, offering convenience and comfort for patients while allowing therapists to monitor progress effectively.
While more research is needed to establish the most effective interventions for improving hand dexterity in PD, the findings of this review provide valuable guidance for developing future rehabilitation programmes. By incorporating the recommended parameters, cueing strategies, goal-oriented approaches and considering the convenience and comfort of patients, clinicians can design interventions that enhance hand dexterity, ADL and QoL, ultimately improving the lives of individuals with Parkinson’s disease.
Furthermore, it was difficult to draw a definite conclusion on the therapeutic applications of the current best intervention to improve hand dexterity in PD due to the limitations of this review discussed earlier, further investigation is needed before concluding an intervention is assuredly effective.
Acknowledgements
The authors thank the Research and Ethics Committee of Universiti Tunku Abdul Rahman for the study approval.
Author contributions
Data curation: Lim Ming Hui, Choong Pui Kuan, Fong Wei Han, Dr Deepak Thazhakkattu Vasu, Dr Li-Wei Chou.
Formal analysis: Lim Ming Hui, Choong Pui Kuan, Fong Wei Han, Dr Deepak Thazhakkattu Vasu, Dr Li-Wei Chou.
Methodology: Lim Ming Hui, Choong Pui Kuan, Fong Wei Han, Dr Deepak Thazhakkattu Vasu. Supervision: Dr Deepak Thazhakkattu Vasu.
Writing – original draft: Lim Ming Hui, Choong Pui Kuan, Fong Wei Han.
Writing – review & editing: Dr Deepak Thazhakkattu Vasu, Dr Li-Wei Chou.
Funding statement
None.
Competing interests
None.











