Introduction
Lumbar degenerative disease (lumbar spondylosis) and low-back pain (LBP) are common conditions, with more than 12 million Americans diagnosed each year, and 70%-85% of adults are affected by LBP at some point in their lifetime.Reference Fourney, Dettori, Hall, Hartl, McGirt and Daubs1, Reference Yavin, Casha and Wiebe2 The sequelae of LBP are among the leading causes of functional incapacity and a familiar source of chronic disability in the working years.Reference Driscoll, Jacklyn and Orchard3 Similarly, cervical degenerative diseases (cervical spondylosis) can cause neck pain and arm pain or spinal cord compression resulting in functional disability. Furthermore, with the expanding and aging population, increasing number of patients are suffering from degenerative spine diseases, leading to increased referral to spine surgeons by primary care physicians.Reference Yavin, Casha and Wiebe2–Reference St-Pierre, Yang, Bourget-Murray, Thomas, Hurlbert and Matthes4 However, up to 85% of referrals to spine surgeons are not surgical candidates, leading to inefficient use of healthcare resources.Reference Murphy, Blake, Power and Fullen5
In the Canadian healthcare system, the limited number of spine surgeons available to meet the increased demand of referrals has caused a ballooning in wait time.Reference Barua and Esmail6–Reference Robertson-Steel9 Long wait times for consultation entails increased cost for both individuals and society, including lost work time, psychological distress, and decreased productivity.Reference Salomon, Vos and Hogan10 The decision on whether to offer surgery is often based on patient history, signs and symptoms, and functional metrics that are consistent with a surgical pathology and an expected favorable response to surgery. However, information included in primary care physician referrals are often inadequate to help triage patients effectively. Innovative strategies such as nonphysician clinician spinal triage programs have been developed and have been proven to be successful.Reference Bath, Grona and Janzen7 However, triage systems such as these are costly and may not be accessible to spine surgeons.Reference McEvoy, Wiles, Bernhardsson and Grimmer11 To tackle this issue, the Spine Triage and Assessment Clinic (STAC) at the University of Calgary developed an electronic survey called the patient-derived intake module; all referred patients are required to complete this module before seeing a spine surgeon. This survey collects a plethora of clinical variables such as patient demographics, comorbidities, functional capacity, history of presenting illness, previous surgeries, and various quality-of-life assessment questionnaires. The goal of this study is to determine which patient parameters from the patient-derived intake module are best able to predict whether a patient will have a high or low probability of being a surgical candidate. We also propose a clinical scoring system that may aid spine surgeons in triaging their outpatient referrals. By effectively triaging patients who have a low probability of being surgical candidates to other health professionals, wait times for patients who will benefit from surgery may be improved.
Methods
We performed an ambispective cohort study on patients referred to the Neurosurgery STAC at the Foothills Medical Centre, Canada, between May 2013 and January 2015. This clinic evaluates all outpatient referrals made to the neurosurgery spine service, as such patients were recruited in a consecutive manner. Patients requiring urgent surgical management are not referred to this clinic. All patients were consented and prospectively completed the patient-derived intake module, which was administered before the clinic visit. Variables collected included, but were not limited to, basic patient demographics, presenting symptoms, Short Form-12 (SF-12), patient disability questionnaire-9, McGill pain index, Charlson comorbidity index, visual analogue scale for pain, alleviating/aggravating factors, medications, occupational variables, and previous surgeries/injections. Details of the patient questionnaire can be found in Table 1.
Table 1 Patient-derived intake module questionnaire

The primary outcome was whether surgery was offered. Patients seen through the STAC are initially evaluated by international medical graduates who have received Doctor of Medicine equivalent training. All cases are then reviewed by four complex spine subspecialty trained neurosurgeons, and the decision to offer surgery was determined by the surgeon. A case conference process to determine surgical candidacy was not used. Whether surgery was offered was retrospectively collected through electronic paper charts in December 2016 and updated in October 2017. Other variables that were collected retrospectively include the proportion of patients with MRI studies before the clinic, patients declining surgery, and patients who had their operation at the time of this study. Institutional approval was obtained through the Conjoint Health Research Ethics Board at the University of Calgary.
Statistical Analysis
Descriptive statistics was used to summarize included patients. A multivariable logistical regression using the random forest method was used to determine the odds of being offered surgery based on preoperative variables found in the patient-derived intake module. There were few missing data, which were imputed using random forest imputation. The remainder of preprocessing included removal of features with near-zero variance, scaling, and centering data. The feature space was filtered using additive construction of a random forest model, with the most important variables subsequently used to initialize a logistic regression model that was then tuned using recursive feature elimination (e.g., the most important features from the random forest model were used in the first logistic regression model, and the nonsignificant variables thereafter removed). Logistic regression was selected for interpretability. The level of significance was set at 0.05, and 95% confidence intervals (CIs) were calculated for odds ratios (ORs). All statistical analyses were performed using RStudio v. 0.99.489.
Results
A total of 1194 unique patients were included in the analysis. The mean age was 53.3 years (SD: 14), and 626 (52.4%) patients were male. The most common location of presenting pathology was in the thoracolumbar (68.5%) and cervical regions (30.0%). Twenty-six percent of patients were offered surgery, and among them 65 (20.9%) patients declined surgery. At the time of outcomes data collection, 58.4% of patients who were offered surgery had received their operation (October 2017). The majority of patients (89.2%) obtained an MRI before their clinic visit. Table 2 describes the baseline characteristics of the included patients.
Table 2 Baseline characteristics of included patients (n=1194)
Predictors of Surgical Candidacy
We found 11 independent significant preoperative patient factors that either increased or decreased the odds of patients being offered surgery. According to the multivariable model, the patient factors that reduced the odds of surgery being offered include the following: mild pain (OR 0.37 [95%CI 0.17-0.74], p=0.008), normal walking distance (OR 0.51 [95%CI 0.29-0.84], p=0.007), and normal sitting tolerance (OR 0.58 [95%CI 0.38-0.87], p=0.01) (Figure 1). Mild pain is defined as numeric rating scale or verbal rating scale for pain of 0 to 4 out of 10. Normal sitting tolerance is defined as sitting tolerance >60 minutes.
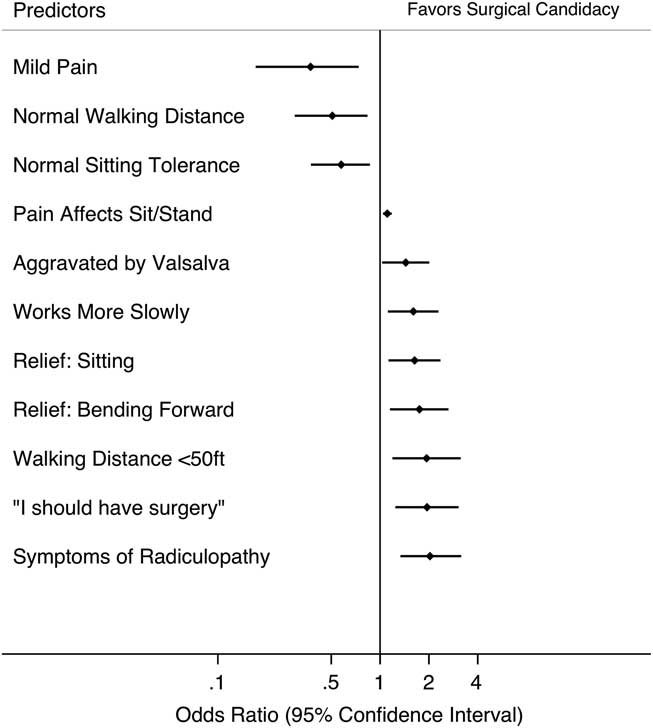
Figure 1 Significant preoperative patient factors that increase or decrease the odds of surgery being offered.
Factors that increased the odds of surgery being offered included radiculopathy (OR 2.0 [95%CI 1.3-3.2], p=0.001), patient’s belief that they should have surgery (OR 1.9 [95%CI 1.2-3.0], p=0.003), walking distance <50 ft (OR 1.9 [95%CI 1.2-3.1], p=0.01), relief when bending forward (OR 1.7 [95%CI 1.2-2.6], p=0.008), sitting (OR 1.6 [95%CI 1.1-2.4], p=0.009), works more slowly (OR 1.6 [95%CI 1.1-2.3], p=0.01), aggravation of symptoms by Valsalva (OR 1.4 [95%CI 1.03-2.0], p=0.03), and pain affecting sitting or standing (OR 1.1 [95%CI 1.04-1.2] p=0.001) (Figure 1). Other variables such as comorbidities, duration of symptoms, history of opioid therapy, pain quality, preoperative pain intensity, history of spinal injections, history of surgery, and items in the patient disability questionnaire and SF-12 were not predictive of significantly increasing or decreasing the odds of a patient being offered surgery.
Discussion
Spine surgery for degenerative conditions makes up a significant proportion of spine practices. In carefully selected patients, surgery can provide significant relief and positively affect the quality of life and physical function.Reference St-Pierre, Yang, Bourget-Murray, Thomas, Hurlbert and Matthes4, Reference Gibson, Grant and Waddell12, Reference Gibson, Waddell and Grant13 However, the vast majority of referrals from primary care physicians have nonsurgical pathologies leading to inefficient use of healthcare resources. In this study, we found that patients who indicated that they have radicular symptoms had a strong belief that they should have surgery, and having a walking distance <50 ft increased their odds of being a surgical candidate by approximately two-fold. However, patients who report only mild pain, a normal walking distance, and a normal sitting tolerance had approximately 50%-60% reduction in the odds of being a surgical candidate.
In Canada, the median wait time to see a neurosurgeon or orthopedic surgeon is 17.4 and 18.5 weeks, respectively.Reference Barua and Esmail6 However, the clinically reasonable wait time as determined by specialist consensus is 5.1 and 11.8 weeks for neurosurgery and orthopedic surgery, respectively.Reference Barua and Esmail6 Moreover, the median time between initial primary care referral to treatment is 24.7 and 39.6 weeks for neurosurgery and orthopedic surgery, respectively.Reference Barua and Esmail6 Prolonged wait time to surgery can have detrimental effects on patient-perceived function and quality of life, not only while waiting for surgery but also negatively affecting surgical outcome.Reference Freeman14 Given the aging population, these wait times are likely to get longer as more patients suffer from degenerative spine conditions unless innovative solutions are developed to direct care appropriately. Spine triage programs have been developed to tackle increased wait times and improve referral appropriateness. In a recent systematic review by McEvoy et al (2017),Reference McEvoy, Wiles, Bernhardsson and Grimmer11 the authors identified 11 spine triage programs led by physiotherapists and three programs by nurses.Reference Fourney, Dettori, Hall, Hartl, McGirt and Daubs1, Reference Bath, Grona and Janzen7, Reference Paskowski, Schneider, Stevans, Ventura and Justice15 Three of these programs were located in Canada: Saskatoon, Ottawa, and Toronto.Reference Fourney, Dettori, Hall, Hartl, McGirt and Daubs1, Reference Bath, Grona and Janzen7, Reference Sarro, Rampersaud and Lewis16, Reference Simon, Coyle, Dagenais, O’Neil and Wai17 These nonphysician clinicians work either as a sole practitioner performing triage or in combination with a medical specialist or surgeon. These programs have been shown to be effective in reducing wait times, ranging between 3 and 54 weeks.Reference Bath, Grona and Janzen7, Reference McEvoy, Wiles, Bernhardsson and Grimmer11, Reference Paskowski, Schneider, Stevans, Ventura and Justice15, Reference Crossley, Mueller and Horstman18 The most marked improvement was reported by Curley et al (2009)Reference Curley, Cassells, Cooke and Dowling19, with a decrease in wait time for surgical review from 15 months to 6 weeks after introduction of the physiotherapist-led triage program. These programs have also cited high rates of identifying surgical candidates.Reference McEvoy, Wiles, Bernhardsson and Grimmer11 The same authors reported that 97% of patients referred from their triage program had a surgical pathology.Reference Curley, Cassells, Cooke and Dowling19 Although effective, these programs are resource-intensive to establish, costly to maintain, and inaccessible to many spine surgeons.Reference McEvoy, Wiles, Bernhardsson and Grimmer11 As such, there continues to be a need for a simple, low-cost method to triage spine patients.
In this study, we found three patient factors that decreased the odds of someone being offered surgery (mild pain, normal walking distance, and normal sitting tolerance). These three clinical variables are an indication of the patient’s functional status. It is unlikely for a patient to be offered surgery if they only have mild pain and have no functional disability when walking or sitting. On the other hand, patients complaining of paresthesia (numbness/tingling) in their upper or lower extremity and pain exacerbated by Valsalva suggests that the patient has radiculopathy.Reference Kawakami, Tamaki, Hayashi, Hashizume and Nishi20, Reference Rubinstein, Pool, van Tulder, Riphagen and de Vet21 Many different pathologies can cause radiculopathy, but a herniated disc or progressive spondylosis of the spine is most likely. The surgical outcomes of disc herniation causing radiculopathy are excellent, with a median time to recovery of 4 weeks compared with 12 weeks in the conservative therapy group, as reported by Peul et al (2007).Reference Peul, van Houwelingen and van den Hout22 Patients who have a walking distance of <50 feet and have relief when sitting or bending forward point to a patient with neurogenic claudication caused by lumbar canal stenosis. A study by Nadeau et al (2013)Reference Nadeau, Rosas-Arellano and Gurr23 showed that alleviation of leg pain when sitting and bending forward has a positive likelihood ratio of 3.8 and 1.7, respectively, for neurogenic claudication. Other variables such as working more slowly and pain affecting sitting/standing are also indicators of the functional status of patients. It was interesting to find that the patient’s belief of whether they should have surgery greatly influenced whether surgery was offered to the patient. The rationale for this is unclear, but this could be a surrogate for patient’s overall poor functional status and quality of life, thereby increasing their chance of being offered surgery. Cervical myelopathy was not found to be a significant predictor for surgical candidacy in this study. This is owing to the lack of myelopathy-specific questions in the patient-derived intake module. Future iterations of this module will include myelopathy-specific questions.
It can be argued that the predictors for surgical candidacy elucidated in this study are not surprising, as they mainly point to patients with cervical or lumbar radiculopathy, and neurogenic claudication. The challenge is to devise a simple strategy to obtain this information from referring physicians and to decide on the likelihood of patients being a surgical candidate. To do this, we propose a clinical scoring system based on significant predictors found in this study. The OR for each predictor was rounded to the nearest integer and adjusted using subjective interpretation of the quality of the predictor to establish each variable’s numeric clinical prediction score.Reference Tu and Naylor24 For example, “patient’s belief that they should have surgery” had an OR of 1.9; however, we subjectively modified its score to 1 as patients are usually poor at predicting whether they are surgical candidates. The inverse was taken for predictors that had ORs <1 and rounded to the nearest integer.Reference Tu and Naylor24 The clinical scoring system can be found in Table 3. Predictors that decreased the odds of being surgical candidates were given negative scores (mild pain, normal walking distance, and normal sitting tolerance). Predictors that increased the odds of being surgical candidates were given positive scores (e.g., symptoms of radiculopathy and walking distance <50 ft). The sum of scores can range between −7 and 12; positive total scores (1-12) suggest higher chance of being surgical candidates, whereas scores between −7 and 0 suggest a lower chance of being surgical candidates. Spine surgeons and nonphysician clinicians can request referring physicians to score their patients using this tool, which may lead to improvement in selection accuracy of surgical patients. However, like any clinical scoring system, this tool will need to be validated by a future prospective study.
Table 3 Clinical scoring system for surgical candidacy in spine surgery

* Numeric or verbal rating scale for pain: 0 to 4 out of 10
** Sitting tolerance >60 minutes
The strength of our study includes the prospective nature in which data collection on patient variables was conducted. The large sample size included in this study allowed us to evaluate multiple preoperative patient variables without losing statistical power in our logistic regression analysis. We also proposed a simple clinical scoring system based on significant predictors found in this study that may aid spine surgeons in triaging their outpatient referrals. However, the findings from the present report should be interpreted in the context of the study design. The patient-derived intake module contained numerous preoperative variables that were included in the multivariable analyses, leading to increased probability of committing a type I error owing to multiple comparisons. This risk was minimized by using a recursive elimination method, where nonsignificant variables were removed with each subsequent logistic regression analysis. As inherent to all observational designs, residual confounding cannot be excluded. The primary outcome (whether surgery was offered) was determined by expert opinion of the surgeon evaluating the patient, which may not be equivalent to whether the patient needs or would benefit from surgery. This is mitigated by having four independent complex spine fellowship trained neurosurgeons staff the Spine Triage and Assessment Clinic. The patient-derived intake module was not designed to detect symptoms of myelopathy, and hence the predictors found in this study are not reliable in predicting surgical candidacy in myelopathy patients.
In conclusion, we identified 11 independent significant preoperative patient factors that were predictive of whether a patient will have higher or lower odds of being offered surgery. These predictors may be used to help spine surgeons more effectively triage their referrals and reduce the number of nonsurgical consultations. Future studies will be conducted to validate the proposed clinical scoring system.
Acknowledgment
The authors thank Abraham Nunes for his assistance in performing the statistical analyses for this project.
Disclosures
MMHY, GHS, and SD have nothing to disclose.
Statement of Authorship
MMHY drafted the initial draft of the manuscript, performed data collection and data analyses, interpreted the study results, and critically reviewed the final draft of the manuscript.
GHS performed data collection and data analysis and critically reviewed the final draft of the manuscript.
SD conceptualized the study, provided mentorship and guidance, interpreted study results, and critically reviewed the final draft of the manuscript.
Financial Support
MMHY is supported by the Clinical Investigator Program at the University of Calgary and the Canadian Institute of Health Research.






