A 13-year-old boy with accelerated growth underwent brain MRI for pituitary assessment, which incidentally demonstrated a nonenhancing, T2-hyperintense right occipital lesion (Figure 1A). No diffusion-weighted imaging (DWI) sequences were obtained, and the lesion was thought to represent encephalomalacia. Five years later, he developed left visual field difficulties and repeated MRI-identified lesional growth (Figure 1B) with high DWI (Figure 1C) and low apparent diffusion coefficient (ADC) signal (Figure 1D).
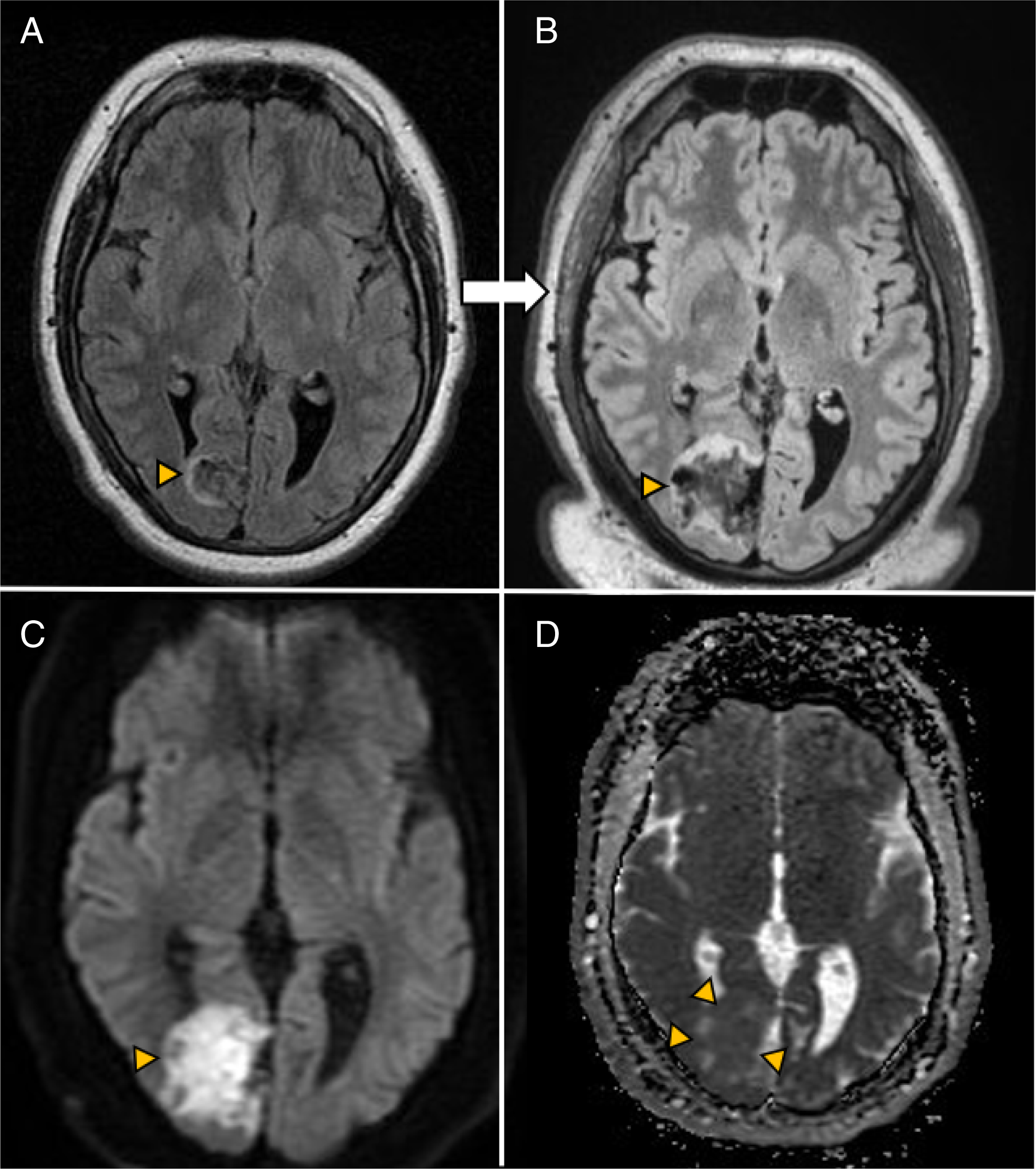
Figure 1: Brain MRI findings of an epidermoid cyst. (A) Initial T2-weighted FLAIR MRI demonstrating a right occipital lobe, nonenhancing, T2-hyperintense lesion (arrowhead). (B) 3D-weighted FLAIR MRI showing the lesion’s growth after 5 years (arrowhead). (C) DWI MRI revealing diffusion restriction of the lesion (arrowhead). (D) ADC MRI demonstrating lesion hypointensity (arrowheads).
The differential diagnosis for a diffusion-restricting cortical lesion is broad and includes acute ischemic stroke, abscess, demyelination, Creutzfeldt Jakob disease, encephalitis, and epidermoid cyst. Reference Schembri and Grech1,Reference Sheerin, Pretorius, Briley and Meagher2 Our patient underwent resection of the right occipital lobe lesion. Histopathology revealed keratin encapsulated by squamous epithelium, consistent with an epidermoid cyst (Figure 2). Reference Kaido, Okazaki, Kurokawa and Tsukamoto3
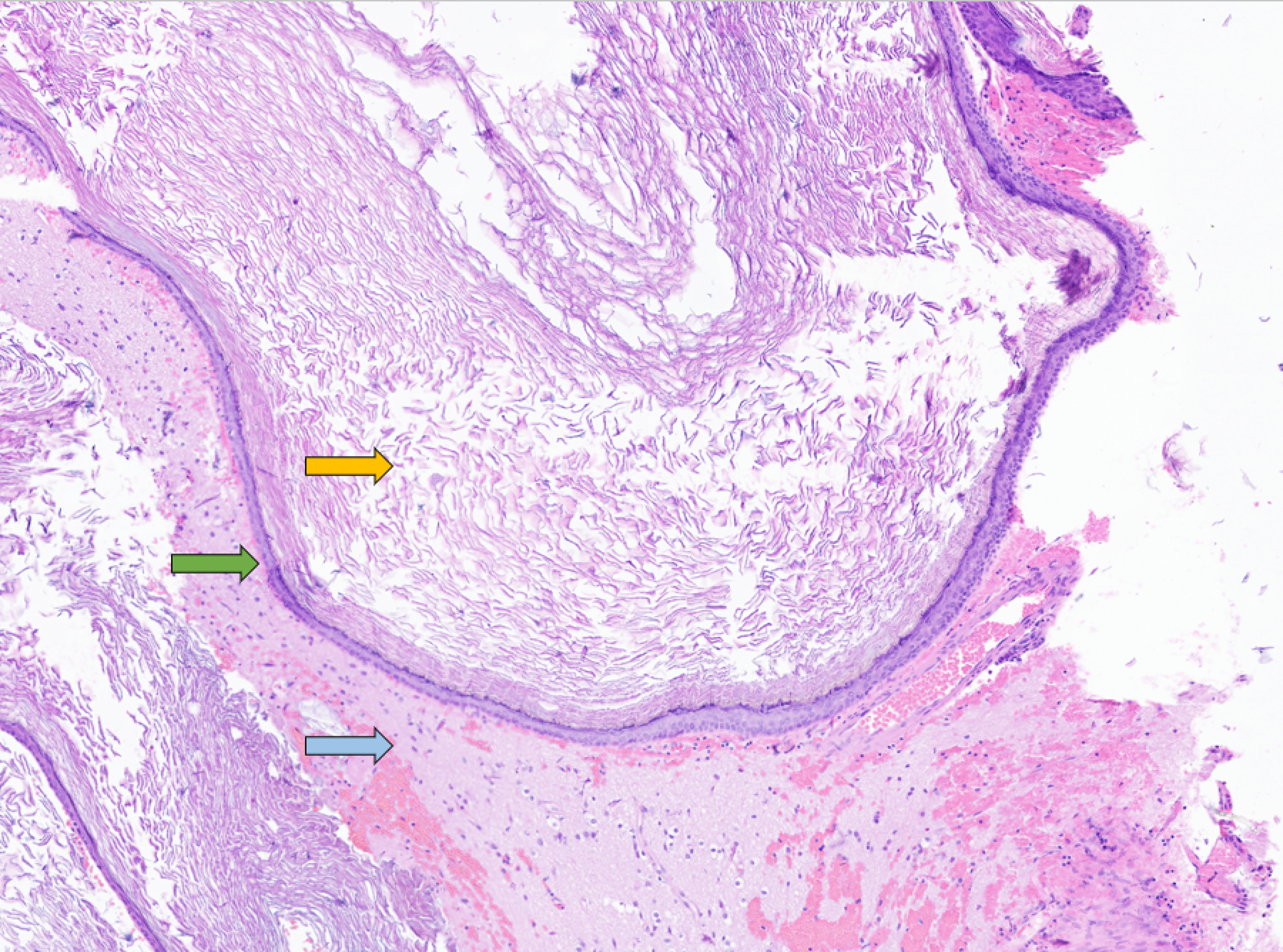
Figure 2: Epidermoid cyst pathology. Pathology image (magnification ×4) of the intracranial epidermoid cyst, demonstrating keratin debris (yellow arrow), lined by squamous epithelium (green arrow), surrounded by brain parenchyma (blue arrow).
Intracranial epidermoid cysts comprise 1% of primary intracranial tumors and are derived from ectodermal inclusions during neural tube closure. Reference Schembri and Grech1 They are usually present in middle age due to the mass effect on adjacent structures. Reference Gaillard, Haouimi and Weerakkody4 Intracranial epidermoid cysts most commonly occur at the cerebellopontine angle or in the parasellar region. Reference Kaido, Okazaki, Kurokawa and Tsukamoto3,Reference Kachhara, Bhattacharya and Radhakrishnan5 A cortical location of an intracranial epidermoid cyst, as in our patient’s case, is very rare. The presence of diffusion restriction on MRI helped narrow our differential diagnosis.
The MRI signal intensity of the epidermoid cyst is variable due to its composition of keratin and lipids. Reference Kaido, Okazaki, Kurokawa and Tsukamoto3 There is usually no associated edema. Reference Kaido, Okazaki, Kurokawa and Tsukamoto3
Total surgical excision is the mainstay of treatment for intracranial epidermoid cyst. Reference Kachhara, Bhattacharya and Radhakrishnan5 Recurrence is not uncommon, but growth is usually slow over many years. Reference Gaillard, Haouimi and Weerakkody4 Our patient is currently doing well, and his left visual field vision is improved.
Disclosures
The authors have no conflicts of interest to disclose.
Statement of authorship
L.W. reviewed the medical record and drafted the manuscript. T.B. is the neurosurgeon who cared for the patient, resected the epidermoid cyst, and provided critical review of the manuscript. P.Z. assessed the pathology of the lesion, confirmed the diagnosis pathologically, and provided the histopathology image. U.S. cared for the patient as his neuro-oncologist, conceptualized the case as an educational opportunity for other clinicians, and provided a critical review of the manuscript.




