Degenerative retro-odontoid pseudotumour is an uncommon condition that is thought to be a manifestation of biomechanical stressors at the cranio-cervical junction. It is frequently attributed to atlanto-axial instability (AAI),Reference Sze, Brant-Zawadzki, Wilson, Norman and Newton 1 although it has also been identified in patients with adjacent segment ankylosis, or ossification of the anterior or posterior longitudinal ligaments.Reference Crockard, Sett, Geddes, Stevens, Kendall and Pringle 2 The histopathology of reported cases is consistent in that this entity comprises benign, fibrous tissue suspected to be a reactive process secondary to chronic mechanical stress of the posterior ligamentous complex.Reference Sze, Brant-Zawadzki, Wilson, Norman and Newton 1 , Reference Crockard, Sett, Geddes, Stevens, Kendall and Pringle 2
Treatment aims to stabilise this segment of the spine, and surgical instrumentation is the dominant strategy in the literature, comprising case reports and small series.Reference Barbagallo, Certo, Visocchi, Palmucci, Sciacca and Albanese 3 - Reference Yanni, Halim and Alexandru 5 Managing AAI in a collar is not novel, although it has not been well described in the treatment of degenerative pseudotumour. Our case demonstrates collar treatment of retro-odontoid pseudotumour presenting with myelopathy, resulting in mass regression and clinical improvement. The context is in a poor surgical candidate with a sizeable lesion, and no evidence of underlying inflammatory pathology.
An 80-year-old woman presented with a 4-month history of neck pain, decreased dexterity, and extremity paresthesias. She could ambulate with a walker, and had no bowel and bladder dysfunction. Review of systems was non-contributory—no history of trauma, infection, malignancy, or other rheumatologic sequelae. Notable examination findings included upper-extremity hyper-reflexia. Plantar and Hoffmann’s reflexes were negative. Patchy, non-dermatomal sensory loss was noted in the upper and lower extremities.
Cervical spine MRI revealed a retro-odontoid soft tissue mass, peripherally enhancing and mixed in signal intensity, measuring 1.5×2.2×1.2 cm (Figure 1). There was severe compression of the thecal sac at the level of the mass with local T2-hyperintense cord changes. Degenerative changes were present throughout the cervical spine. No atlanto-axial erosion was noted to suggest rheumatologic pannus or depositional arthropathy, nor was there surrounding bony destruction or enhancement to suggest malignancy. There was no widening of the atlanto-dental interval appreciated on these initial studies. These findings were corroborated with computed tomography for high-resolution bony visualisation.
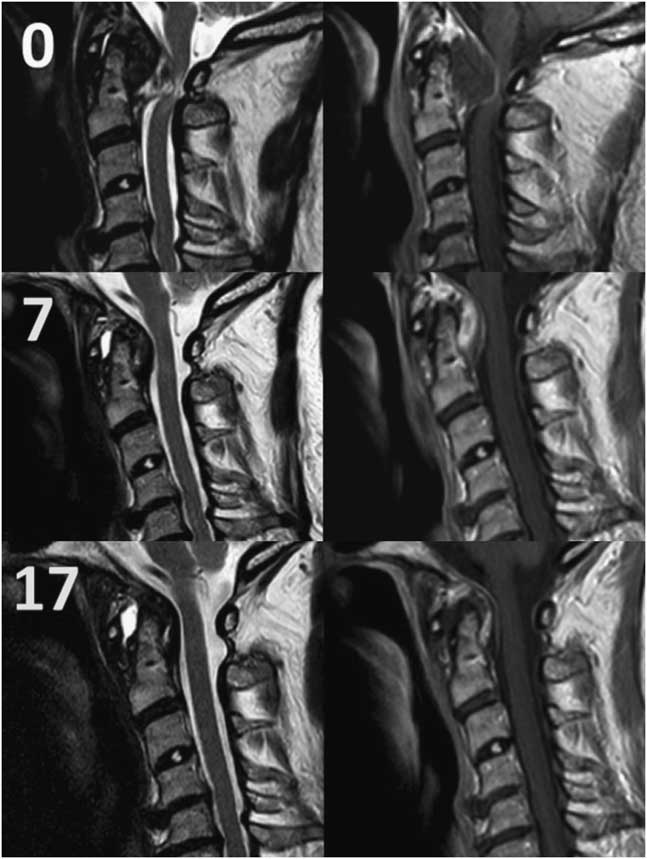
Figure 1 Sagittal T2-weighted (left) and T1-post-Gadolinium contrast media (right) MRI of the cervical spine, at initial presentation, 7 months, and 17 months (from top to bottom).
In summary, this patient presented with progressive cervical myelopathy in the context of a retro-odontoid mass. She was admitted for further testing, including rheumatologic bloodwork and consultation and work-up for primary malignancy, which was negative. As such the working diagnosis was degenerative pseudotumour, and treatment was initiated with a rigid cervical collar. Surgery was considered, although ultimately opted against owing to risks associated with the patient’s osteopaenic bone quality, small stature, and vertebral artery anatomy.
She was seen in clinic 1 month post discharge and described significant improvement of neck pain and diminished myelopathic symptoms. In subsequent visits, fine motor function, walking distance, and gait continued to improve. She no longer required any gait aids. Repeat imaging at 7 months demonstrated significant lesion regression (Figure 1), as well as radiologic signs of AAI including increased pre-dental interval and mild subluxation (2.7 mm) on flexion-extension films. The patient reported compliance with the collar, although she found it uncomfortable and challenging. At 8 months, it was decided that the patient be weaned off the collar over the course of a month, with time off during the day while maintaining a soft collar at night. Moreover, she was instructed to be vigilant for symptoms of progressive myelopathy. At 17 months—9 months post weaning—her MRI did not show any recurrence (Figure 1).
Treatment approaches for retro-odontoid pseudotumour include decompression of the neural elements and atlanto-axial immobilisation. In many cases, immobilisation without decompression has proven to be effective. Our case report describes clinical and radiographic improvement of degenerative pseudotumour managed in a collar exclusively, and is the first case report we were able to identify with this specific combination of condition and treatment. It is important to emphasise that this patient was a high-risk operative candidate and did not have evidence of inflammatory arthropathy. Generally, moderate to severe myelopathy should be treated surgically, as non-operative management confers a greater risk of progression. Regular and careful follow-up is crucial if non-operative management is to be considered.
In patients with pseudotumour and evidence of AAI, both from degenerativeReference Barbagallo, Certo, Visocchi, Palmucci, Sciacca and Albanese 3 - Reference Yanni, Halim and Alexandru 5 and inflammatory aetiologies,Reference Grob, Würsch, Grauer, Sturzenegger and Dvorak 6 , Reference Zygmunt, Säveland, Brattström, Ljunggren, Larsson and Wollheim 7 posterior fixation withReference Barbagallo, Certo, Visocchi, Palmucci, Sciacca and Albanese 3 - Reference Grob, Würsch, Grauer, Sturzenegger and Dvorak 6 and without decompressionReference Barbagallo, Certo, Visocchi, Palmucci, Sciacca and Albanese 3 , Reference Zygmunt, Säveland, Brattström, Ljunggren, Larsson and Wollheim 7 has been described. Non-operatively, Isono et alReference Isono, Ishii, Kamida, Fujiki, Goda and Kobayashi 4 attempted collar management, which failed, and then proceeded with posterior decompression and fixation. Another patient with rheumatoid pannus underwent C1 laminectomy and C1-2 fusion was attempted, although it could not be instrumented owing to poor bone quality; they achieved clinical and radiographic recovery after treatment in a rigid collar 8 weeks postoperatively, which was stepped down to a soft collar for 4 weeks and then discontinued.Reference Oseni, Kakavas, Scholz and Petridis 8 There was no progression of symptoms at 1 year.
Our conservative approach does not definitively solve the problem of instability, which is often implicated in pseudotumour, but does demonstrate a viable treatment option particularly for lower-demand patients with mild instability who are high-risk operative candidates. The marked size reduction despite the size of the index lesion should be noted. However, larger series of patients are certainly required to better understand this treatment. If there has been improvement, both clinically and radiographically, we propose that a trial of collar removal be considered on a case-by-case basis—in reliable patients with close follow-up. Our patient did not experience any recurrence 9 months after weaning and will continue to be monitored regularly.
Acknowledgement
The authors thank the Injury Prevention Research Office for administrative support during this project.
Disclosure
PK, JW, and MC have nothing to disclose.
Conflicts of Interest
There are no conflicts of interest to disclose for any of the authors.
Statement of Authorship
PGK reviewed the case, performed literature review, and wrote the manuscript. JW cared for the patient, reviewed the case, and reviewed the manuscript. MC supervised the project, cared for the patient, reviewed the case, and reviewed the manuscript.



