Introduction
Maintaining the ability to access the community on foot and in vehicles is fundamental to active aging, allowing older adults to lead dynamic and independent lives (Webber, Porter, & Menec, Reference Webber, Porter and Menec2010; World Health Organization, 2007). Impaired mobility has been shown to be an early predictor of physical disability and, ultimately, to be associated with falling, loss of independence, institutionalization, and death (Hirvensalo, Rantanen, & Heikkinen, Reference Hirvensalo, Rantanen and Heikkinen2000; Mackey et al., Reference Mackey, Lui, Cawthon, Ensrud, Yaffe and Cummings2016; Rubenstein, Powers, & MacLean, Reference Rubenstein, Powers and MacLean2001; von Bonsdorff, Rantanen, Laukkanen, Suutama, & Heikkinen, Reference von Bonsdorff, Rantanen, Laukkanen, Suutama and Heikkinen2006). While many factors that influence community mobility are related to the lower extremities and walking (e.g., distances, speeds, and terrains tolerated) (Patla & Shumway-Cook, Reference Patla and Shumway-Cook1999), it has also been recognized that movement of the upper body, in particular the neck, is important for safe travel outside the home (Bennett, Schenk, & Simmons, Reference Bennett, Schenk and Simmons2002).
Neck range of motion (ROM) decreases with age and degenerative changes (Nilsson, Hartvigsen, & Christensen, Reference Nilsson, Hartvigsen and Christensen1996; Sforza, Grassi, Fragnito, Turci, & Ferrario, Reference Sforza, Grassi, Fragnito, Turci and Ferrario2002; Simpson, Biswas, Emerson, Lawrence, & Grauer, Reference Simpson, Biswas, Emerson, Lawrence and Grauer2008; Youdas et al., Reference Youdas, Garrett, Suman, Bogard, Hallman and Carey1992). These changes may negatively influence safe community mobility in older adults. Limited neck rotation has been shown to be associated with a greater incidence of self-reported adverse driving events in older adults compared to their peers with normal ROM (Marottoli et al., Reference Marottoli, Richardson, Stowe, Miller, Brass, Cooney and Tinetti1998). In a study of 227 older adults, the spine was the most frequently reported body region associated with health-related symptoms, and stiffness of the neck was the most commonly reported specific spine symptom (Tuokko, Rhodes, & Dean, Reference Tuokko, Rhodes and Dean2007). Twenty-two per cent of older drivers reported having conditions involving the spine that negatively affected their driving, which was second only to vision problems influencing driving (31%) (Tuokko et al., Reference Tuokko, Rhodes and Dean2007). Studies have determined neck rotation ROM thresholds required for safe walking and driving. For example, checking for traffic while walking across the street requires up to 54 degrees of unilateral neck rotation (Bennett et al., Reference Bennett, Schenk and Simmons2002). Driving and making lane changes on residential streets and highways require 36–43 degrees of rotation (Shugg, Jackson, & Dickey, Reference Shugg, Jackson and Dickey2011), and looking out the rear window while reversing a vehicle necessitates the greatest amount of rotation (68 degrees) (Bennett et al., Reference Bennett, Schenk and Simmons2002).
As neck rotation ROM is thought to be important for driving, measures of neck ROM have been included in test batteries aimed at assessing older drivers (Marottoli et al., Reference Marottoli, Richardson, Stowe, Miller, Brass, Cooney and Tinetti1998; Staplin & Dinh-Zarr, Reference Staplin and Dinh-Zarr2006). In addition, exercises designed to improve neck ROM have been included in training programs designed to improve driving in older adults (Marottoli et al., Reference Marottoli, Allore, Araujo, Iannone, Acampora, Gottschalk, Charpentier, Kasl and Peduzzi2007; Ostrow, Shaffron, & McPherson, Reference Ostrow, Shaffron and McPherson1992). In a randomized controlled trial, Marottoli et al. (Reference Marottoli, Allore, Araujo, Iannone, Acampora, Gottschalk, Charpentier, Kasl and Peduzzi2007) reported improvements in on-road driving performance in older drivers after they had participated in a 12- week physical conditioning program. However, the daily exercise program was a combination program that included neck stretching exercises along with ROM and conditioning exercises for the trunk, shoulders, and lower extremities. Additionally, the program included coordination exercises and input on gait and foot abnormalities. Therefore, it is not clear which elements of the program were effective in improving on-road driving performance. Also, the authors did not measure whether any changes in neck ROM actually occurred. In another study, Ostrow et al. (Reference Ostrow, Shaffron and McPherson1992) examined the effects of an 8-week ROM program (neck, trunk, shoulders) on driving performance in individuals 60–85 years of age. Participants were instructed to perform 5 to 10 repetitions of six different neck, trunk, and shoulder ROM exercises daily at home prior to entering their vehicle. Participants demonstrated improvements in observational responses (e.g., looking to the rear and to the side) during driving maneuvers and greater shoulder and trunk ROM but no significant changes in neck flexion/extension, side flexion, or rotation ROM. Of note, neck ROM was measured in this study with a head-mounted goniometer using a protocol developed and tested in the researchers’ lab, and the assessor was not blinded to participant group assignment. Interestingly, other general stretching intervention studies not aimed at driving improvement have shown positive effects on neck ROM in healthy older adults (Raab, Agre, McAdam, & Smith, Reference Raab, Agre, McAdam and Smith1988; Swank, Funk, Durham, & Roberts, Reference Swank, Funk, Durham and Roberts2003).
At present, physical activity guidelines (Canadian Society for Exercise Physiology, 2020; Piercy et al., Reference Piercy, Troiano, Ballard, Carlson, Fulton, Galuska, George and Olson2018) do not directly recommend stretching exercises, and there is little consensus on their optimal type, dose, or frequency (Freitas et al., Reference Freitas, Mendes, Le Sant, Andrade, Nordez and Milanovic2018; Stathokostas, Little, Vandervoort, & Paterson, Reference Stathokostas, Little, Vandervoort and Paterson2012). Although stretching for older adults is advocated by many organizations, evidence for the functional benefits of flexibility programs is limited (Piercy et al., Reference Piercy, Troiano, Ballard, Carlson, Fulton, Galuska, George and Olson2018; Stathokostas et al., Reference Stathokostas, Little, Vandervoort and Paterson2012). Despite this, because neck ROM is recognized as being important for safe driving and walking in the community, older adults are often encouraged to engage in neck stretching exercises.
The purpose of this randomized controlled trial was to determine whether a stretching program could improve ROM of the neck, trunk, and shoulders in a group of mobility-impaired older women. In particular, we were interested in neck rotation because of its importance in driving and walking near traffic or through crowd situations. Based on previous literature (Ostrow et al., Reference Ostrow, Shaffron and McPherson1992; Raab et al., Reference Raab, Agre, McAdam and Smith1988; Swank et al., Reference Swank, Funk, Durham and Roberts2003), we hypothesized that neck, trunk, and shoulder ROM would improve a small but significant amount in response to the training.
Methods
Participants
Participants were part of a larger randomized single blind controlled trial investigating the effects of ankle power training on movement time in mobility-impaired older women (Webber & Porter, Reference Webber and Porter2010). We were interested in studying older women because they typically live longer than older men and have more disability and functional limitations (Leveille, Penninx, Melzer, Izmirlian, & Guralnik, Reference Leveille, Penninx, Melzer, Izmirlian and Guralnik2000). Research has shown that women tend to exhibit slower maximum movement velocities compared to men (Wocjik, Thelen, Schultz, Ashton-Miller, & Alexander, Reference Wocjik, Thelen, Schultz, Ashton-Miller and Alexander1999), and this may contribute to both motor vehicle crashes and falls. The recruitment procedures, randomization protocol, inclusion/exclusion criteria, and sample size justification have been previously described (Webber & Porter, Reference Webber and Porter2010). Briefly, community-dwelling women 70 years of age and older who reported they were unable to walk 1 mile at a moderate pace were recruited to the study. Women who had participated in structured exercise more than once per week in the previous 6 months were not eligible. We instructed participants not to change their activity levels while they were involved in the program, with the exception of the supervised exercise components of the study. Participants were randomly assigned to one of three groups (two lower extremity power training groups and one upper body ROM group). All groups attended supervised exercise sessions twice per week for 12 weeks. A blinded assessor conducted evaluations before participants were randomized and after they completed 12 weeks of training. For the purposes of this analysis, participants in the lower body power training groups were combined to serve as the active control participants (n = 33) for the upper body ROM group (n = 15), and the primary outcome variable of interest was neck rotation ROM.
Of the 192 women who responded to study advertisements and participated in telephone screening, 118 women were excluded because they did not meet the inclusion criteria, and 13 declined to participate, leaving 61 women to be randomized (Figure 1, n = 20 to upper body ROM, and n = 41 to the control group for this study). Fifteen participants in the ROM group and 33 in the control group completed 12 weeks of training and a final test. Participants provided their written informed consent at the initial evaluation session. The Education/Nursing Research Ethics Board of the University of Manitoba granted ethical approval for this study.

Figure 1. Flowchart outlining numbers of participants at various stages of the study.
Descriptive Measures and Upper Body ROM Measures
We measured lower extremity strength, power, and movement time as previously reported (Webber & Porter, Reference Webber and Porter2010). Participants answered basic questions about their health and demographics, and we measured neck, trunk, and shoulder ROM. Indirect tests of both neck and trunk ROM (Marottoli et al., Reference Marottoli, Richardson, Stowe, Miller, Brass, Cooney and Tinetti1998) were conducted. For neck ROM, the participant stood against a wall and rotated her head in order to see a number written on a card placed in line with the acromion process at the level of the ear. For trunk ROM, the participant was seated and turned her torso to reach across her body with her hand to try to touch the wall behind the opposite shoulder. Both of these tests were scored as pass/fail.
Direct measures of neck ROM were performed using a cervical range of motion (CROM) gravity referenced inclinometer system (Performance Attainment Associates, University of Minnesota, St. Paul, MN) (Youdas et al., Reference Youdas, Garrett, Suman, Bogard, Hallman and Carey1992). The CROM consists of three inclinometers in a plastic frame that fits on the head. It has been shown to have moderate (ICC 0.60–0.80) to good (ICC ≥ 0.80) intraobserver and interobserver reliability and reasonable concurrent criterion validity in multiple studies (Williams, McCarthy, Chorti, Cooke, & Gates, Reference Williams, McCarthy, Chorti, Cooke and Gates2010). The minimal detectable change values for CROM measurements have been reported to vary between 3.6 and 6.5 degrees (Audette, Dumas, Côté, & De Serres, Reference Audette, Dumas, Côté and De Serres2010; Gugliotti et al., Reference Gugliotti, Tau, Gallo, Sagliocca, Horan, Sussman and Wisnewski2020). In our study, the device was used to detect axial, frontal, and sagittal rotations (rotation, side-flexion, and neck flexion in that order). Participants started all movements with the head in a neutral position (head level with eyes looking forward). They performed one practice repetition for each movement to ensure they were conducting the movement properly. This was then followed by two test repetitions for each movement. The average of the two test repetitions was used in the analysis. The CROM’s magnetic compass was zeroed after each repetition, and each repetition was held for approximately 1 second for the examiner to read the rotation angle achieved to the nearest 2 degrees.
In addition, participants also completed the back-scratch test from the Seniors Fitness Test (Rikli & Jones, Reference Rikli and Jones1999). This test involves trying to touch the middle fingers of both hands together behind the back when one hand reaches down behind the head and the other reaches up behind the back. The degree of overlap (or distance) between the third fingers is measured. Positive numbers indicate the extent of overlap of the middle fingers (in centimeters), whereas negative numbers refer to the distance (in centimeters) between the fingers. The test has been shown to be able to discriminate between older adults of different ages and different activity levels (Rikli & Jones, Reference Rikli and Jones1999).
Training Program
All intervention participants attended 45-minute supervised group exercise sessions twice per week for 12 weeks. The same 15-minute warm-up and 5-minute cool-down were performed by all participants and consisted of seated marching, knee extension, and ankle movements. The upper body ROM group performed static stretches for the following movements: trunk side flexion, shoulder retraction and protraction, neck side flexion, neck rotation, forward neck flexion, neck retraction, and diagonal neck movements. All stretches were done three to four times in each direction and held for 8 to 10 seconds (Pollock et al., Reference Pollock, Gaesser, Butcher, Depres, Dishman, Franklin and Garber1998). In addition, participants completed eight repetitions of shoulder girdle circles (each forwards and backwards) and eight repetitions of arm circles (each small, medium, and large circles, both forwards and backwards). Participants in the control group took part in ankle power training using either Hammer Strength Tibia Dorsi Flexion and Super Horizontal Calf weight training machines (Life Fitness, Schiller Park, IL) or Thera-Band elastic resistance bands (The Hygenic Corporation, Akron, OH). They performed three sets of 8–10 repetitions of concentric ankle dorsiflexion and plantarflexion against a 1 repetition maximum load (weight training machines) or three sets of 8 repetitions of the same concentric movements against elastic band resistance (Thera-Band). All participants in the control group were encouraged to perform the concentric movements “as fast as possible.” Further details regarding the training program are provided by Webber and Porter (Reference Webber and Porter2010).
Statistical Analysis
Analyses were conducted using SigmaPlot, version 11.0 (Systat Software Inc., San Jose, CA) and SPSS 15.0 (IBM Corporation, Armonk, NY). Our data demonstrated no violations to the assumptions for using analysis of variance (ANOVA). Two-way ANOVA tests with repeated measures were used to determine between (group) and within (time) factors, with CROM and back-scratch test measurements as the dependent variables (p < 0.05). Tukey’s multiple comparison test was used for post-hoc analyses when indicated.
Results
Participants
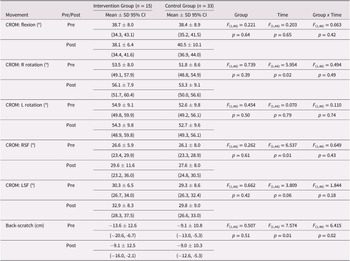
Details of participant characteristics are presented in Table 1. The mean age of participants in both the control and intervention groups was 75 years. The two groups were similar in their self-report of falls, use of pain relievers and in rating their health for their age as “good”. Equal proportions of individuals in both groups reported having non-arthritic related neck or back problems, whereas 22/33 participants in the control reported having arthritis compared to only 7/15 in the upper body ROM group.
Table 1. Participant characteristics
Range of Motion
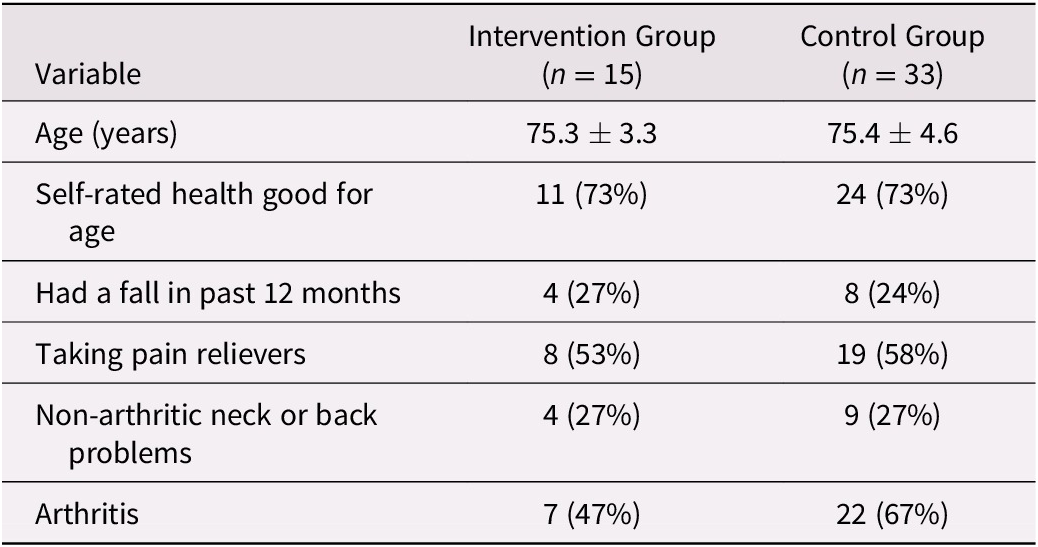
After training, participants in both groups demonstrated small increases (≤ 3 degrees) in right-sided neck rotation (p = 0.02) and side flexion (p = 0.01, Table 2); however, these differences did not exceed minimal detectable change levels for the CROM, and the group x time interactions were not significant. There were no significant effects for flexion, or the left-sided tests. The time and group x time factors were significant for the back-scratch test (p = 0.01). Post-hoc Tukey’s multiple comparison tests revealed that participants in the upper body ROM group improved by 4.5 cm (p = 0.003), whereas the control participants did not change (0.2 cm, p = 0.85). This represented an average improvement of 33% for the intervention group.
Table 2. Pre- and post-training cervical range of motion (CROM) and back-scratch measurements with repeated measures ANOVA results
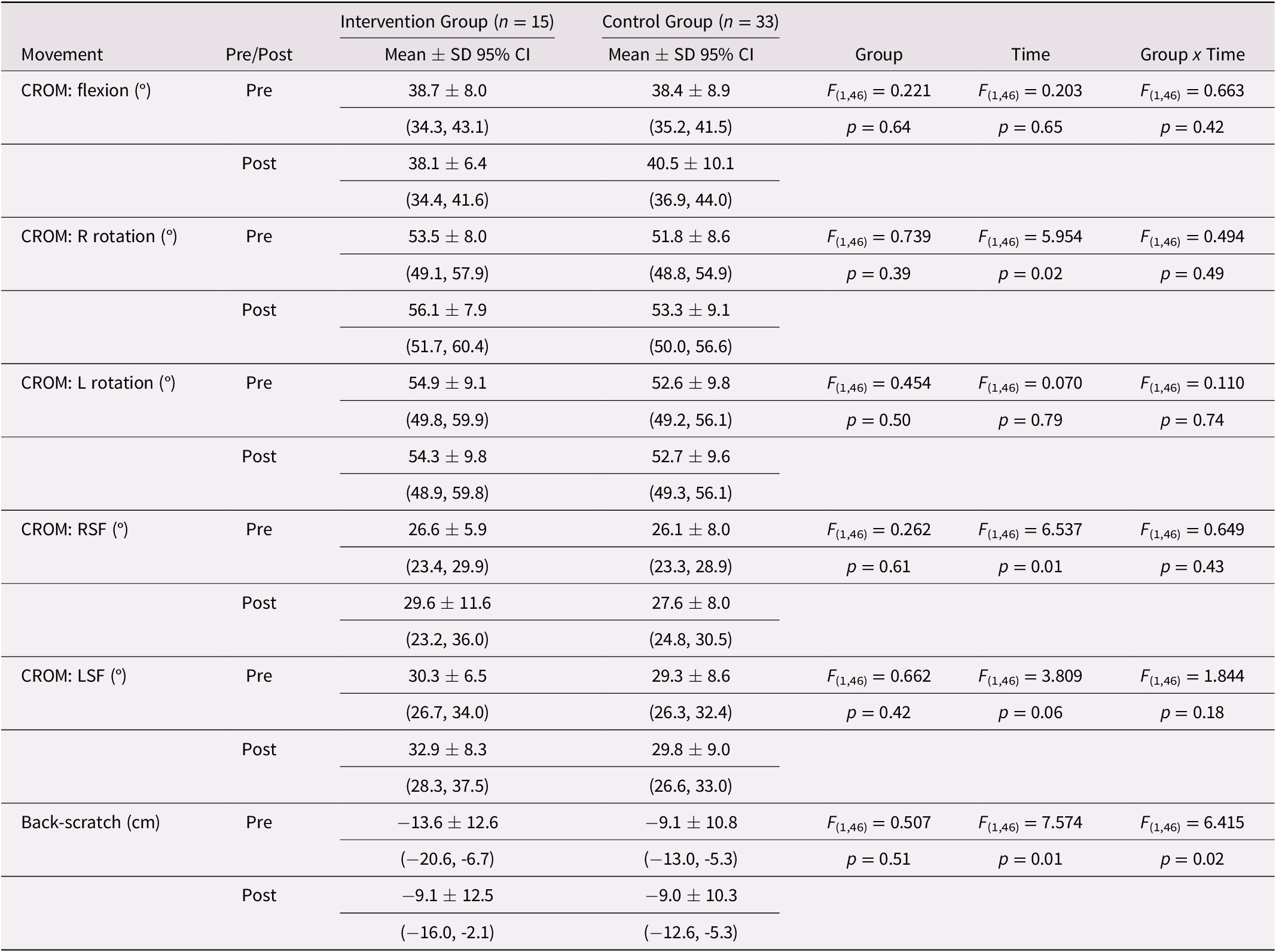
ANOVA = analysis of variance; SD = standard deviation; CI = confidence interval; CROM = cervical range of motion; R = right, L = left; RSF = right side flexion; LSF = left side flexion.
For the indirect tests of neck and trunk ROM, the number of participants able to successfully complete the tests at baseline was relatively high for the neck (intervention = 12/15 for both directions; control = 25/33 right, 23/33 left) and the trunk (intervention = 8/15 right, 9/15 left; control = 22/33 right, 21/33 left). Perhaps because of the relatively high baseline results, very few participants improved their scores. For the neck, only one individual improved in the intervention group (from fail to pass, both right and left directions), whereas, in the control group, five individuals made improvements (one direction each). For the trunk, a similar pattern was found with one intervention participant improving in both directions, and three control participants improving (two in both directions and one in one direction). There were also individuals who were unable to do one or more of the tests after the training program who had previously been able to do them (intervention = 3; control = 10). Because of the small proportions, these results were not examined statistically.
Discussion
The main finding of this study was that older women who completed a 12-week upper body stretching program did not improve their neck ROM more than an active control group. At baseline, our participants’ mean neck ROM values were very similar to normative data for older women and were approximately 20 degrees lower than those demonstrated in women in their twenties (Youdas et al., Reference Youdas, Garrett, Suman, Bogard, Hallman and Carey1992). Women in our intervention and control groups averaged 52–56 degrees of neck rotation, which reaches the threshold required for safely making lane changes in a vehicle (Shugg et al., Reference Shugg, Jackson and Dickey2011) but is not enough for looking out the rear window when reversing (Bennett et al., Reference Bennett, Schenk and Simmons2002). Despite having typical age-related reductions in neck ROM, the stretching intervention did not elicit significant changes in neck ROM in the stretching group beyond those of the control group, even though shoulder ROM did improve by 33%.
Stretching programs can increase ROM in older adults, although not consistently across all muscle groups (Stathokostas et al., Reference Stathokostas, Little, Vandervoort and Paterson2012). Current Canadian 24-hour movement guidelines for older adults do not include stretching activities (Canadian Society for Exercise Physiology, 2020). Similar to the Canadian guidelines, American physical activity guidelines for older adults do not directly recommend stretching or ROM exercises (Piercy et al., Reference Piercy, Troiano, Ballard, Carlson, Fulton, Galuska, George and Olson2018). They state that the “health benefits of these activities alone are not known and they have not been demonstrated to reduce risk of activity-related injuries” (p. 73). However, they do acknowledge that stretching is a legitimate part of an activity program, and enhanced ROM could enable people to do activities with greater ease if large amounts of ROM are needed.
Studies that have specifically examined neck and trunk ROM in older adults in response to stretching programs have not provided consistent results. Ostrow et al. (Reference Ostrow, Shaffron and McPherson1992) found that right trunk rotation improved slightly (about 3 degrees) in their randomly assigned experimental group relative to the control group, but neck rotation and left trunk rotation did not change. Our program differed from Ostrow’s in that our exercise sessions were supervised, included a general whole-body 15-minute warm-up before the stretching exercises were conducted, and training was extended over 12 weeks versus 8 weeks. We also used a reliable tool (the CROM) to measure neck ROM, and the assessor was blinded to group allotment. Despite these differences in the two studies, we also found no significant improvements in neck ROM. Raab et al. (Reference Raab, Agre, McAdam and Smith1988) studied the effects of an exercise program with and without added wrist and ankle weights on neck ROM in older women (63 to 88 years old). Surprisingly, the older women did not show age-related limitations in neck rotation ROM at baseline. After training, the exercisers demonstrated non-significant improvements in right neck rotation (average change of 5 degrees) and statistically improved left neck rotation (6 degrees) compared to controls (who improved by only 2 degrees). Similarly, Swank et al. (Reference Swank, Funk, Durham and Roberts2003) found that older adults who participated in a stretching program with added hand/cuff weights had greater neck rotation ROM compared to control participants and compared to those in the stretching program who did not use any weights. Participants in the program with added hand/cuff weights increased neck rotation by an incredible 10–20 degrees, yet none of the reported ROM exercises actually focused on the neck (all were general upper and lower extremity movements). Both of these positive trials had limitations because they were non-randomized, used a less reliable way of measuring neck rotation ROM, and there was no mention of blinding of the assessment process. As Liu, LaValley, and Latham (Reference Liu, LaValley and Latham2011) demonstrated in a meta-analysis of exercise studies, “Reported effects were exaggerated in trials that used unblinded assessors” (p. 190). In addition, it is unclear how adding hand/cuff weights to stretching exercises would assist with increasing neck rotation ROM.
Consistent with findings reported by Ostrow et al. (Reference Ostrow, Shaffron and McPherson1992), the results of our trial suggest that age-related reductions in neck rotation ROM may not be amenable to change with a stretching program. What could explain this finding? First, it could be argued that our sample size was too small (n = 15 for the intervention group). However, the effects seen did not even indicate a strong trend toward a positive effect. For example, for the left rotation, the p values for both the time and group x time effects were > 0.7. For the right rotation, the time effect was significant, but the group x time effect was not (p = 0.49). In addition, even though there was a significant time effect, the mean change for the intervention group was only 2.6 degrees, and the change in the control group was 1.5 degrees. Both of these values are within the measurement error associated with using an inclinometer (Fletcher & Bandy, Reference Fletcher and Bandy2008) and are likely to have little clinical significance. Second, it is possible that our stretching program was not done frequently enough. Our participants performed stretching twice per week, which is in line with the minimum of previous American College of Sports Medicine recommendations (Reference Chodzko-Zajko, Proctor, Fiatarone Singh, Minson and Nigg2009). However, as mentioned previously, intervention dosage related to stretching has not been well established. In these same participants from our study, shoulder ROM improved 33% in the intervention group, whereas the control group did not change. It appears that 2 days per week were sufficient for shoulder ROM to improve. Perhaps the neck requires more frequent stretching as compared to the shoulders, or perhaps the lack of change in neck ROM was due to the movement itself, the anatomical structures involved directly and indirectly in neck rotation, and/or age-related changes. Holding static stretches for a longer duration (e.g., up to 30 seconds or 1 minute) is now generally recommended (Riebe, Reference Riebe2018); however, further research is required to determine whether this would be safe or beneficial in addressing neck ROM in older adults. With aging, thoracic kyphosis (increased forward curvature of the spine) is known to occur. Quek, Pua, Clark, and Bryant (Reference Quek, Pua, Clark and Bryant2013) have shown that increased thoracic kyphosis results in increased forward head posture, which has a negative effect on neck ROM. In addition to postural changes, osteoarthritis affects the neck with increased prevalence and severity with age. A recent study found that 93% of people over the age of 70 have significant osteoarthritic changes, including osteophytes at the atlanto-axial joint (Liu et al., Reference Liu, Lü, Cheng, Guo, Liu and Song2014). This joint, located between the first and second cervical vertebrae, is responsible for providing approximately 50% of the total rotation in the neck (32–36 degrees) (Hu et al., Reference Hu, Gu, He, Xu, Ma, Zhao, Liang and Zhong2010; Roche, King, Dangerfield, & Carty, Reference Roche, King, Dangerfield and Carty2002).
Our results suggest that stretching to improve neck ROM may have limited benefit in older women. While some researchers have reported improvements in ROM with non-specific and specific neck stretching programs (Raab et al., Reference Raab, Agre, McAdam and Smith1988; Swank et al., Reference Swank, Funk, Durham and Roberts2003), other researchers have reported no significant improvements (Ostrow et al., Reference Ostrow, Shaffron and McPherson1992), similar to our findings. Additionally, there is little evidence that an improvement in neck ROM will lead to functional improvements. As Stathokostas et al. (Reference Stathokostas, Little, Vandervoort and Paterson2012) state: “Conclusive recommendations regarding flexibility training and functional outcomes for older adults remain ungrounded” (p. 28). Also, in driving, it is possible that neck rotation ROM is not as directly linked to shoulder checking behaviours as may be suspected. In a naturalistic study in our lab, we found that available neck rotation ROM had little to do with using appropriate backing up visual checking, as even those with sufficient ROM were very unlikely to turn and look out of their rear window (Porter, Conci, Huebner, & Ogborn, Reference Porter, Conci, Huebner and Ogborn2006). In order to improve shoulder checking and backing up behaviours associated with driving, instruction on appropriate techniques might be more important.
Another important concern about advocating for neck exercises lies with the possible risks associated with neck stretching. As with all interventions, an assessment of benefits and risks is necessary. As mentioned previously, the benefits of stretching are not convincing and there could be risks, particularly if exercises are done in an unsupervised environment. In our study, there were no adverse events associated with neck stretching; however, cases of vertebral artery dissection and transient ischaemic attacks have been reported in the literature (Hwang & Pless, Reference Hwang and Pless2010; Pryse-Phillips, Reference Pryse-Phillips1989).
Strengths of this study include randomization to intervention and control groups and the use of a blinded assessor for evaluation. Our sample was small and restricted to older women who reported some limitations in walking, so findings may not be generalizable to all older adults. Further investigations should include larger sample sizes and experimentation with different stretching protocols (e.g., stretches held for longer durations and/or performed more frequently). Using imaging to determine the degree of osteoarthritic changes may also provide valuable information about the effectiveness of neck stretching exercises in older adults with varying levels of osteoarthritic involvement of the cervical spine.
Conclusion
In conclusion, static neck stretching exercises combined with general upper extremity ROM exercises did not result in changes in neck or trunk ROM in older women, although shoulder ROM did improve. Adequate ROM of the upper body, especially the neck, is required for safe walking and driving in the community (Bennett et al., Reference Bennett, Schenk and Simmons2002). Researchers and clinicians should ensure that older adults with ROM limitations are aware of their deficits and focus on teaching compensatory strategies to promote maintenance of function and safe mobility.
Acknowledgements
The authors would like to thank Bronwyn Zalewski and Linda Johnson for providing technical support and conducting the testing. We also acknowledge Nancy Maskus and Heather Klassen for supervising participants during the exercise sessions.
Funding
This work was supported by the Natural Science and Engineering Research Council (227595-04); the Institute of Aging, Canadian Institutes of Health Research (fellowship SW); and the Canadian Driving Research Initiative for the Elderly (CANdrive), a New Emerging Team funded by the Institute of Aging of the Canadian Institutes of Health Research.