Introduction
Self-care disability is difficulty with or dependence on others to perform activities of daily living (ADLs), such as bathing, eating, and dressing (Gill, Reference Gill2010). Disablement is increasing self-care disability measured over time (Verbrugge & Jette, Reference Verbrugge and Jette1994). As the global population of older adults with multiple chronic conditions grows, the population prevalence of self-care disability (henceforth “disability”) in this population is also expected to increase (Atun, Reference Atun2015). Older adults with disability experience more hospitalizations (Kruse, Petroski, Mehr, Banaszak-Holl, & Intrator, Reference Kruse, Petroski, Mehr, Banaszak-Holl and Intrator2013), have higher health care costs (Lindholm, Gustavsson, Jonsson, & Wimo, Reference Lindholm, Gustavsson, Jonsson and Wimo2013; Perrin et al., Reference Perrin, Stiefel, Mosen, Bauck, Shuster and Dirks2011), and report lower quality of life (Andersen, Wittrup-Jensen, Lolk, Andersen, & Kragh-Sorensen, Reference Andersen, Wittrup-Jensen, Lolk, Andersen and Kragh-Sorensen2004; Covinsky et al., Reference Covinsky, Wu, Landefeld, Connors, Phillips, Tsevat and Fortinsky1999; Lam & Wodchis, Reference Lam and Wodchis2010). Delaying the onset of disability and the progression of disablement could thus improve older adults’ quality of life while reducing health system costs. A conceptual framework of the factors associated with disablement can help achieve these patient and system outcomes by guiding interventions as well as research questions and analytic choices in empirical research and evidence syntheses (Johnston & Dixon, Reference Johnston and Dixon2014). Verbrugge and Jette’s disablement process model (DPM) (1994) is an example of one such conceptual framework that has received more than 1,500 citations since its publication in 1994.
A key strength of the DPM for disablement research on older adults is that it distinguishes between characteristics intrinsic to older adults (i.e., “intra-individual factors”) such as age, sex, pathologies, and impairments, and extrinsic (“extra-individual”) factors such as medications, assistive devices, rehabilitation programs, and built environment (Figure 1). According to the DPM, these intrinsic and extrinsic factors interact to determine the rate at which older adults experience disablement. This notion of disablement as a person-environment interaction is shared with other commonly used conceptual frameworks of disability, including the International Classification of Functioning Disability and Health (World Health Organization, 2001), and the Social Model of Disability (Oliver, Reference Oliver1990, p. 22). Assuming that disablement is the product of interactions between intrinsic and extrinsic factors, identification of significant extrinsic factors associated with disablement depends on appropriate specification of relevant intrinsic factors, and vice versa.
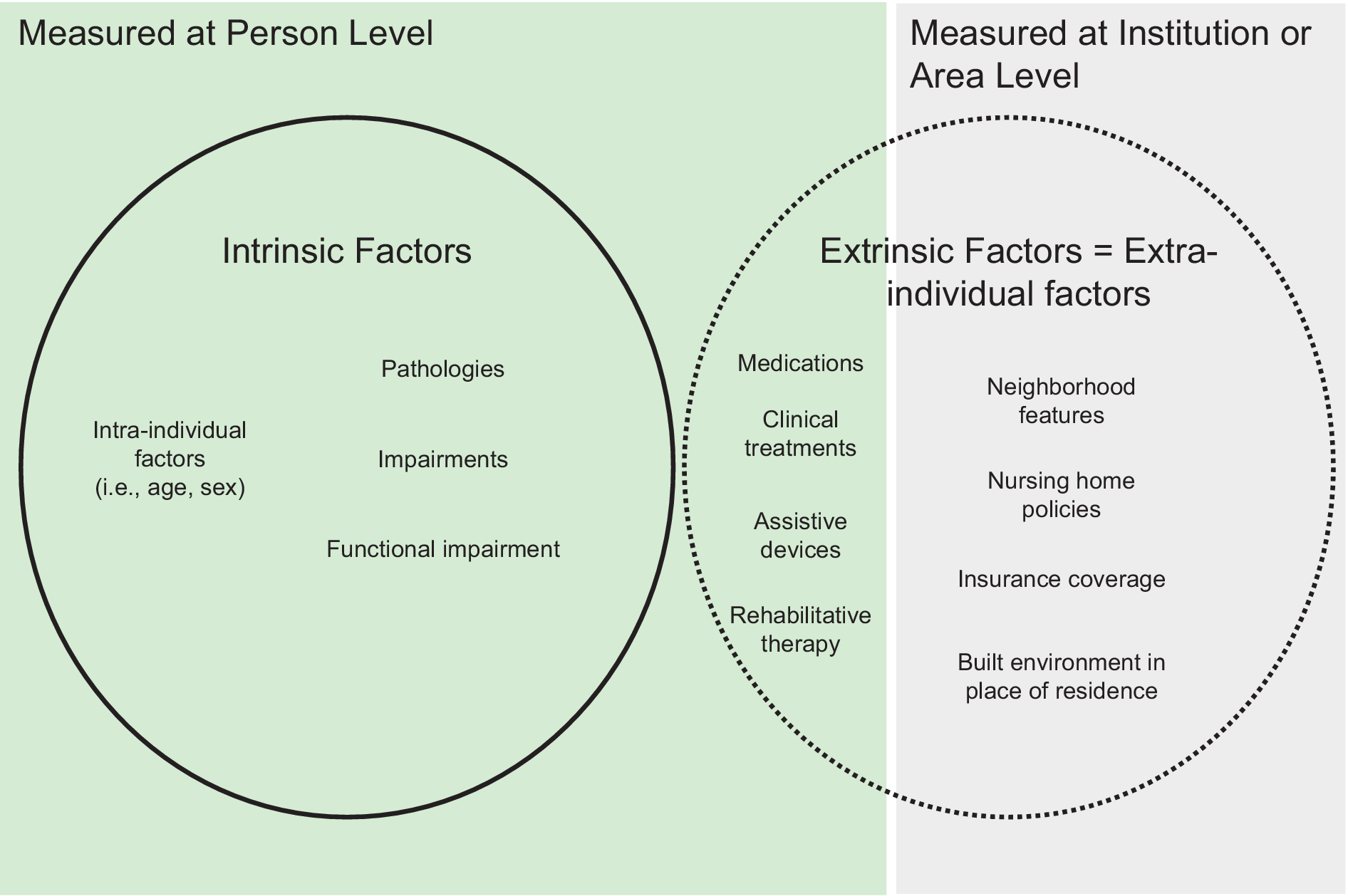
Figure 1: Relationship of DPM intra- and extra-individual factors to definitions of intrinsic and extrinsic factors and their measurement
With the growing use of routinely collected health data in gerontology research, the availability of person-level data to represent intrinsic DPM constructs has outpaced the synthesis of evidence on specific variables’ roles in the disablement process. Routinely collected health data include disease registries, primary care databases, health administrative data, standardized clinical assessments in home care and nursing homes, and public health reporting data that are collected for non-research purposes without specific a priori research questions developed in advance (Benchimol et al., Reference Benchimol, Smeeth, Guttmann, Harron, Moher, Petersen and Langan2015). Researchers seeking to understand the intrinsic and extrinsic drivers of disablement in older adults using routinely collected health data are left to arbitrarily select variables from these data to measure constructs in the DPM or related frameworks. This leads to inconsistent conclusions about the effect size and direction of exposures associated with disability and disablement in older adults. Also, the DPM was originally developed to conceptualize “the trajectory of functional consequences over time and the factors that affect their direction, pace and patterns of change” (Verbrugge & Jette, Reference Verbrugge and Jette1994, p. 3), but it is used extensively in cross-sectional studies of disability. A synthesis of empirical evidence for this extended conceptualization of the DPM has yet to be undertaken.
Overview of Key Disablement Process Model Concepts and Definitions
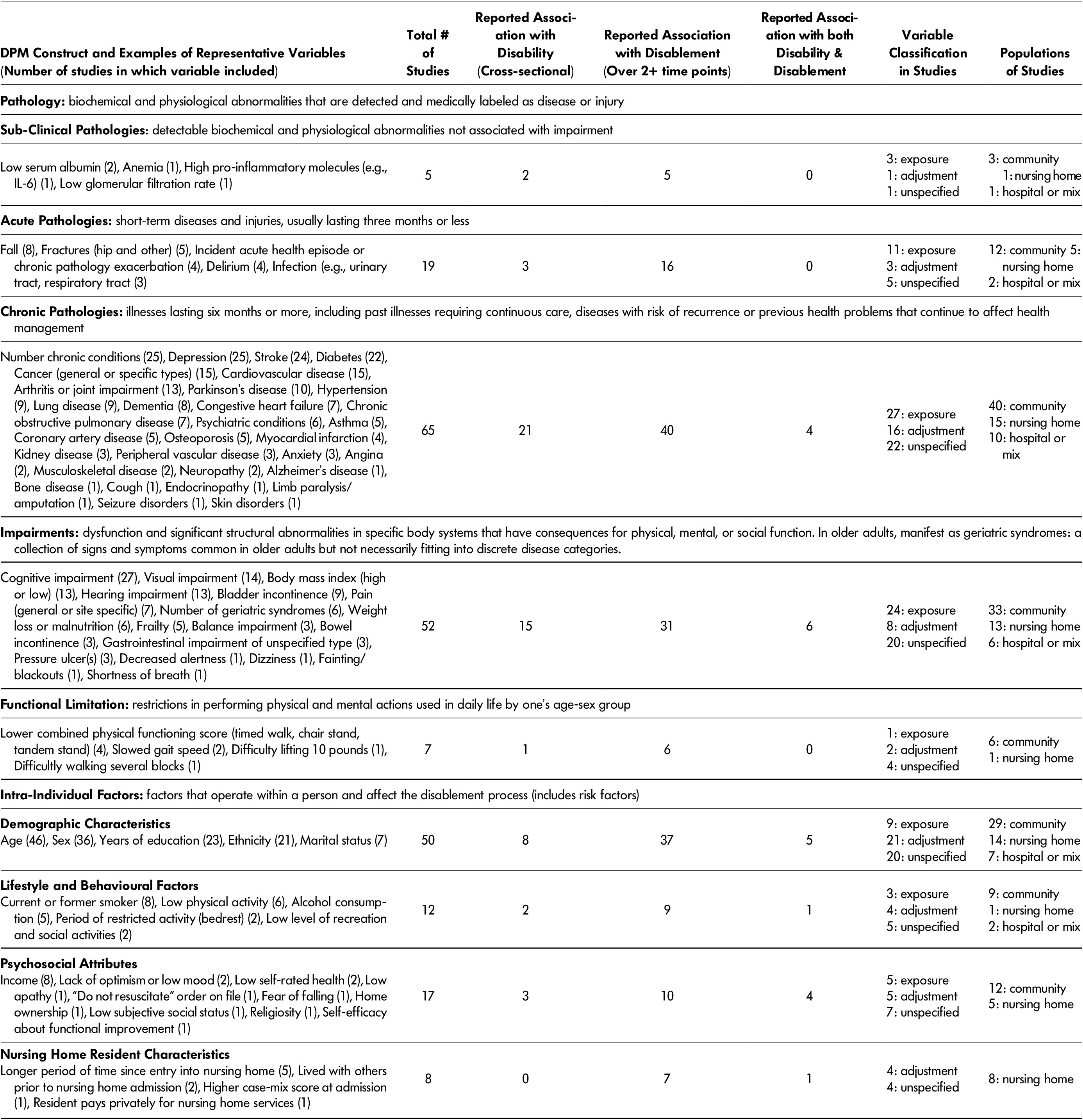
We describe the main constructs in the DPM here, and identify which constructs were included in our critical review. Published in 1994, the DPM builds on concepts proposed by Nagi (Reference Nagi and Susman1965), the social model of disability (Oliver, Reference Oliver1990), and the International Classification of Impairments, Disabilities and Handicaps (World Health Organization, 1980). It identifies a pathway through which pathologies lead to impairments, then limitations in functional capacity and ultimately disability in the context of people’s social and physical world (Verbrugge & Jette, Reference Verbrugge and Jette1994). For the purpose of this study, we defined constructs in the DPM for pathology (including sub-clinical, acute and chronic), impairment, functional limitation, and “intra-individual factors” (i.e., socio-demographic characteristics measured at the person level) in keeping with the original DPM paper (Table 1) (Verbrugge & Jette, Reference Verbrugge and Jette1994). All of these constructs are intrinsic factors, in that they are characteristics of individuals occurring and measured at the person level and not externally provided interventions from health care providers. Because the “risk factors” construct in the original DPM contained only intra-individual factors, these constructs were combined in Table 1, with the understanding that they may affect the disablement process at any stage, including its initiation. The DPM also contains an “extra-individual factors” construct, which includes extrinsic variables that can be measured at the person level (e.g., receipt of rehabilitative care or medications) and extrinsic variables that can measured at the institution or area level (e.g., features of the built environment, access to medical care) (Figure 1).
Table 1: Definition, measurement, and analysis of variables measured in individuals (DPM: disablement process model)
In contrast with intrinsic factors, the extrinsic factors measured at the person level are external interventions that are happen to individuals, rather than processes or characteristics occurring within them. Such interventions can be randomised in clinical trials and their effects summarised in systematic reviews, thus they will not be explored in this article. Extrinsic factors occurring at the institutional and area level warrant critical review and have been summarised elsewhere (Ågotnes, Jacobsen, Harrington, & Petersen, Reference Ågotnes, Jacobsen, Harrington and Petersen2016; Clarke & Nieuwenhuijsen, Reference Clarke and Nieuwenhuijsen2009; Liebel, Friedman, Watson, & Powers, Reference Liebel, Friedman, Watson and Powers2009; Philibert, Pampalon, & Daniel, Reference Philibert, Pampalon and Daniel2015; Pickett & Pearl, Reference Pickett and Pearl2001; Wahl, Fange, Oswald, Gitlin, & Iwarsson, Reference Wahl, Fange, Oswald, Gitlin and Iwarsson2009). To address the salient research gap on intrinsic factors in the DPM and maintain a feasible scope, this critical review focuses only on intrinsic DPM constructs for which variables are often available in routinely collected health data.
According to the DPM, disability encompasses dependence on others for self-care, as well as for instrumental ADLs (e.g., household chores, grocery shopping), mobility, and social and occupational roles (Verbrugge & Jette, Reference Verbrugge and Jette1994). Our study focuses exclusively on self-care disability and disablement as outcomes due to their prevalence and impacts, and because they are the most frequently assessed forms of disability in older adults (Yang, Ding, & Dong, Reference Yang, Ding and Dong2014). In a preliminary review of the literature, we determined that the intrinsic factors associated with other types of disability (e.g., dependence in instrumental ADLs) were not interchangeably associated with self-care disability (Jackson et al., Reference Jackson, Jones, Tooth, Mishra, Byles and Dobson2015). To summarise the empirical evidence linking specific constructs with a specific outcome, our definition of disability was therefore limited to self-care disability, in contrast with the broad definition used in the DPM.
As indicated in Table 1, the chronic pathologies construct consisted of “illnesses lasting six months or more, including past illnesses requiring continuous care, diseases with risk of recurrence or previous health problems that continue to affect health management” (Abad-Diez et al., Reference Abad-Diez, Calderon-Larranaga, Poncel-Falco, Poblador-Plou, Calderon-Meza, Sicras-Mainar and Prados-Torres2014, p. 2). Because older adults were our focus, the impairments construct consisted of “geriatric syndromes”, defined as “a collection of signs and symptoms common in older adults but not necessarily fitting into discrete disease categories” (Chen, Yen, Dai, Wang, & Huang, Reference Chen, Yen, Dai, Wang and Huang2011, p. 1). We also distinguish between “disability” – a measure of self-care disability at one point in time – and “disablement” which indicates intensifying self-care disability measured over at least two points in time. The “disablement process” refers to the process through which pathologies, impairments, functional limitations, and intra- or extra-individual factors lead to disability or disablement (Verbrugge & Jette, Reference Verbrugge and Jette1994).
What This Study Adds
We aimed to strengthen the application of the DPM to studies of disability and disablement in older adults that use routinely collected health data. To achieve this goal, we undertook a critical review (Grant & Booth, Reference Grant and Booth2009) of intrinsic DPM variables associated with disability and disablement in older adults, focusing on those variables commonly available in routinely collected health data. Our specific aims were as follows:
-
1) Summarize variables associated with disability and disablement in older adults, organized according to the intrinsic constructs in the DPM;
-
2) Report on the identified role of these variables (i.e., exposure vs. adjustment) in included studies, the settings in which variables were studied (i.e., nursing home vs. community), and whether variables act as effect modifiers in the DPM;
-
3) Examine the evidence for application of the DPM to cross-sectional studies; and
-
4) Identify common methodological limitations of gerontology research on disability and disablement and offer pragmatic guidance for future research.
Gerontology researchers studying disability and disablement in older adults can use outputs from aims 1 and 2 to guide choices about which intrinsic variables from routinely collected health data to include in their DPM-guided studies. Outputs from aims 3 and 4 can be used by gerontologists to enhance the rigour of their theory-driven research on disability and disablement.
Methods
Type of Literature Review
We identified a critical review as the most appropriate review type to achieve our study aims. Grant and Booth (Reference Grant and Booth2009, p. 94) described a critical review as designed to “demonstrate [that the] writer has extensively researched literature and critically evaluated its quality”. Tricco et al. (Reference Tricco, Antony, Soobiah, Kastner, Cogo, MacDonald and Straus2016, Appendix C, p. 15) similarly described a critical interpretive synthesis as a “Synthesis method using an iterative approach to refine the research question, search and select articles from the literature, and define and apply codes and categories”. These features align with our study aims 1–3, which aim to identify how and in what settings different variables were used to measure DPM constructs, and to determine whether the DPM could be applied to cross-sectional studies. Grant and Booth further described the appraisal methods in a critical review as having “no formal quality assessment” and suggested that studies be “evaluated according to [their] contribution” (2009, p. 94). Tricco et al. (Reference Tricco, Antony, Soobiah, Kastner, Cogo, MacDonald and Straus2016, p. 39) also noted that this type of review should exclude “fatally flawed” studies, but there are no specific thresholds defining this criterion. In our critical review, the inclusion of methodologically flawed studies was key to achieving study aim 4: identifying common limitations of extant research and offering guidance for future research.
Study Search and Appraisal
The aim of the search phase of a critical literature review is to identify the most significant items in a given field (Grant & Booth, Reference Grant and Booth2009; Tricco et al., Reference Tricco, Antony, Soobiah, Kastner, Cogo, MacDonald and Straus2016). To achieve this goal, we searched Medline and Google Scholar using combinations of medical subject headings (MeSH) terms (activities of daily living, risk factors, long-term care, independent living, and homes for the aged), as well as several keywords and commonly used synonyms for disability (disability, functional limitation, disablement, functional capacity, activities of daily living, ADL), determinants (determin*, risk, predict*, associat*), and populations (community, nursing home). We searched reference lists of original studies and used Scopus to identify studies that had cited key manuscripts, such as Verbrugge and Jette’s disablement process paper. Searches were not limited to specific Medline-defined age group categories, but only those studies focused on adults aged 50 and older were eligible; doing so erred on the side of inclusivity while excluding populations (children, young adults) in whom the disablement process is less common and quite distinct from that in older adults. Studies published or in press on any date up to June 30, 2015, were included, as were those that combined eligible and ineligible measures of disability (i.e., outcome scales of combined ADL and IADL dependence).
We excluded studies if they met any of the following criteria: (a) not an original quantitative study of intrinsic variables independently associated (Brotman, Walker, Lauer, & O'Brien, Reference Brotman, Walker, Lauer and O’Brien2005) with either disability or disablement; (b) did not have a comparator group; (c) did not define the activities assessed in measures of disability or disablement, or cited inaccessible articles for descriptions of activities; or (d) published in a language other than English.
The appraisal stage of a critical review is intended to evaluate papers according to their contribution to understanding of a construct (Grant & Booth, Reference Grant and Booth2009). Only “fatally flawed” studies are to be excluded at the appraisal stage so that during the analysis stage limitations of extant research can be identified and critically assessed (Tricco et al., Reference Tricco, Antony, Soobiah, Kastner, Cogo, MacDonald and Straus2016). A theoretical sampling approach is optimal to achieve these goals when conducted by experts in the field (Mays, Pope, & Popay, Reference Mays, Pope and Popay2005; Tricco et al., Reference Tricco, Antony, Soobiah, Kastner, Cogo, MacDonald and Straus2016). We thus determined which studies were included in the full review based on the insight they provided into variables representing DPM constructs; beyond the above-mentioned exclusion criteria, no studies were excluded due to quality issues. Our goal was to identify how and in what settings different variables researchers used to measure intrinsic DPM constructs, rather than draw conclusions about the presence or absence of specific variable relationships. Therefore, we conducted searches and appraisals iteratively and stopped when they began to yield studies that suggested no new variables to measure intrinsic DPM constructs.
Synthesis and Analysis of Study Findings
Our synthesis goals were to provide examples of measures of each intrinsic DPM construct, report on the presumed roles of these measures in included studies, examine whether measures were associated with both disability and disablement, and identify common methodologic limitations of included studies. We summarized the following information for each included study (where applicable) in Supplementary Table 1 (available online): lead author name, country, year of publication, sample size, sample’s location of dwelling (community, nursing home, mix of both), measures of disability (or disablement measured over 2 vs. 2+ time points), and which variables were independent predictors of disability or disablement in the study. Variables in each study were further labelled to indicate whether they were (a) exposure variables identified a priori by study authors, (b) adjustment variables, or (c) part of a predictive model or of an unspecified role. Variables in the first category were those that study authors identified as exposures of interest in either their Introduction or Methods section, whereas adjustment variables were those that were described as being added to models to control for confounding between exposures and outcomes of interest. Variables that were added to models without a specific rational provided were identified as being in the final category.
In keeping with our aim of strengthening the application of the DPM to gerontology studies using routinely collected health data, a final synthesis step incorporated the combination of variables and the DPM constructs they measured into Table 1. This table lists variables in order of the frequency in which they appeared in our review and contains only variables that at least one included study found was associated with disability or disablement. To facilitate extension of the DPM to cross-sectional studies, in the table we also highlight the proportion of studies that measure each DPM construct in association with disability (measured at one time point) or disablement (measured longitudinally), as well as the proportion of studies examining each DPM construct as an exposure, adjustment, or unspecified variable. To examine the distribution of included evidence across settings, we also recorded the proportion of evidence for each construct from studies done in community or nursing home settings. We defined a nursing home as a non-acute care residence in which most residents require daily nursing care (Comondore et al., Reference Comondore, Devereaux, Zhou, Stone, Busse, Ravindran and Guyatt2009). We included “skilled nursing facilities” in this category, but we classified rehabilitation hospitals – in which patients were admitted briefly due to their temporary need for daily rehabilitation services – as hospitals. Studies that included individuals from a combination of community, nursing home, or hospital populations were classified as “mix”.
Results
Characteristics of Critically Reviewed Studies
Of 88 critically reviewed studies, 56 were studies of community-dwelling older adults; 20, of residents of nursing homes; and 12, of a mix of older adults from the community or nursing homes, some of whom were hospitalized. The majority of studies (68 of 88) examined variable relationships with disablement over two or more points of time, whereas 20 studies reported independent associations with disability measured at one point in time. Only seven studies reported variable associations with both disability and disablement. Of the 68 studies that included longitudinal assessments of disablement, 46 considered only two measures (i.e., pre- and post-) of disability, and 22 measured disablement over at least three time points.
Supplementary Table 1 (available online) contains detailed information extracted from each of the 88 studies, including those variables not associated with disability or disablement in adjusted analyses. Details from our critical review on the association of DPM variables with disability and disablement can be found in the online Supplementary Tables 2 through 5. Our findings suggest that variables associated with disablement (measured longitudinally) also tend to be associated with disability (measured at one time point); however, contradictory findings for the independent association of variables with disability and disablement were extremely common: For example, Supplementary Table 2 shows that although 10 studies found cardiovascular disease to be positively associated with disability and disablement, five studies found no such association. These inconsistent findings are difficult to interpret due to variation in intrinsic and extrinsic factors adjusted for in each study.
Measurement and Analysis of Intrinsic DPM Constructs
Table 1 presents a summary of variables we used to measure intrinsic DPM constructs in older adults and independently associated with either disability or disablement. Variables are classified by the DPM constructs that they represent. Of 65 studies that examined the effects of chronic pathologies, such as depression or arthritis, 41 per cent were focused on chronic pathologies as an exposure variable. Of the 52 studies that examined the independent effects of impairments – which encompass most geriatric syndromes – 28 included these variables in analyses as adjustment variables or variables with unspecified roles. Forty of 65 included studies of chronic conditions or geriatric syndrome effects on disability were done in community-dwelling older adults.
The most frequently measured intra-individual variables in included studies were demographic characteristics such as age and sex; however, these variables were considered to be exposure variables in only six of 48 studies that included them. Across the 36 studies that measured sex, male and female sex were both found to be associated with disability and disablement, depending on the patient population and other variables included in models (see Supplementary Table 5). Older age had a similarly inconsistent positive and negative association with disability across studies, but younger age was consistently associated with increased rate of disablement over time (see Supplementary Table 6). Eight reviewed studies examined intrinsic characteristics associated with disablement specific to nursing home residents, the most frequent of which (present in 5 out of 8 studies) was time since entry into a nursing home. Other variables specific to nursing home residents were (a) whether they had lived with others prior to admission, (b) their case mix score at admission, and (c) whether they paid privately for nursing home services.
We also identified intrinsic variables that may act as effect modifiers, meaning that they have significant statistical interactions with other exposures in predicting disability outcomes (Kraemer, Kiernan, Essex, & Kupfer, Reference Kraemer, Kiernan, Essex and Kupfer2008). Older adults with arthritis and stroke have significantly higher odds of having disability than would be expected given the additive effects of arthritis and stroke on disability (Fried, Bandeen-Roche, Kasper, & Guralnik, Reference Fried, Bandeen-Roche, Kasper and Guralnik1999), whereas those with diabetes have greater risk of disablement over time if they have co-existing cognitive impairment (Fultz, Ofstedal, Herzog, & Wallace, Reference Fultz, Ofstedal, Herzog and Wallace2003). The effect of pathologies and impairments on disability outcomes was also found to be modified by sex (Carrière et al., Reference Carrière, Gutierrez, Pérès, Berr, Barberger-Gateau, Ritchie and Ancelin2011) and advanced age (Piernik-Yoder & Ketchum, Reference Piernik-Yoder and Ketchum2013).
Finally, although our focus was on self-care disability as an outcome, incidental findings from included studies suggested that other forms of baseline disability are also independently associated with subsequent disablement in ADLs. In multivariable models adjusted for age, gender, admission diagnosis, co-morbid diagnoses, number of chronic conditions, renal function, and baseline ADL dependence, Barnes et al. (Reference Barnes, Mehta, Boscardin, Fortinsky, Palmer, Kirby and Landefeld2013) showed that odds of ADL dependence in the year following a hospitalization were 2.60 (95% CI: 1.43–4.76) times greater in older adults with three or more IADL impairments at baseline than those without. Similarly, Clark, Stump, Tu, and Miller (Reference Clark, Stump, Tu and Miller2012) found that needing help with personal finances (an IADL) at baseline was associated with 3.69 (95% CI: 2.56–5.31) times greater risk of new onset ADL disability in older adults, adjusting for multiple confounders.
Reviewed studies also showed that a baseline level of self-care disability is independently associated with a subsequent rate of disablement; however, the direction of this association was inconsistent. Kruse et al. (Reference Kruse, Petroski, Mehr, Banaszak-Holl and Intrator2013) and Wolinsky et al. (Reference Wolinsky, Bentler, Hockenberry, Jones, Obrizan, Weigel and Wallace2011) examined confounder-adjusted trajectories of disablement in nursing home and community-dwelling older adults, respectively, and found that individuals with the least baseline ADL disability had the greatest rate of decline during follow-up. Conversely, Abizanda et al. (Reference Abizanda, Romero, Sanchez-Jurado, Martinez-Reig, Alfonso-Silguero and Rodriguez-Manas2014) found that the adjusted odds of incident or worsening disability was 1.70 (95% CI: 1.07–2.75) times greater in older adults with baseline ADL disability present versus absent.
Common Methodological Limitations of Existing Studies
Within the 88 studies we reviewed, several methodological limitations recurred; we identify them here and suggest strategies to address them in the proceeding Discussion section. Only 22 of 55 reviewed studies of disablement included more than two time points at which disability was measured. This may have introduced bias as a result of large fluctuations in disability levels between two time points misrepresenting the extent of disablement that would be apparent with multiple follow-up points (Wolinsky et al., Reference Wolinsky, Bentler, Hockenberry, Jones, Obrizan, Weigel and Wallace2011).
One of the stated goals of the original DPM was to simplify and standardize the “bedlam vocabulary” use in disability research (Verbrugge & Jette, Reference Verbrugge and Jette1994). Our review and others (Gill, Reference Gill2010; Jette, Reference Jette2006) found that this goal has not been achieved. Authors commonly substitute the term “functional decline” for disablement (Marengoni, Von Strauss, Rizzuto, Winblad, & Fratiglioni, Reference Marengoni, Von Strauss, Rizzuto, Winblad and Fratiglioni2009; McLaren, Lamantia, & Callahan, Reference McLaren, Lamantia and Callahan2013), even when citing the DPM as their guiding framework. Other authors have incorporated new constructs into the DPM, but identified operationalising specific variables to measure those constructs as out of scope (Meade, Mahmoudi, & Lee, Reference Meade, Mahmoudi and Lee2015).
Even among those researchers whose conceptualisation of disability and disablement aligned with the DPM, the tools used to measure these outcomes varied significantly across studies. Of the 88 studies reviewed, 42 classified disability based on a count of ADLs older adults had difficulty or needed assistance with, many of which were dichotomised to “disability present” versus “not” based on the presence of dependence in or difficulty with any ADLs (Supplementary Table 6). These count-based classifications varied in their composition, scoring, and overlap with validated disability assessment tools (Yang et al., Reference Yang, Ding and Dong2014). Of 56 reviewed studies of community-dwelling older adults, 34 collected primary data on disability using counts of dependent ADLs, whereas 13 of 20 included studies in nursing homes used routinely collected health data to determine residents’ disability (Supplementary Table 6); such differences in outcome measurement across settings renders cross-setting comparisons of disablement processes difficult.
Discussion
As the prevalence of disability increases in older adults (Atun, Reference Atun2015), a growing body of researchers are pairing the DPM and related conceptual frameworks with routinely collected health data to learn how to prevent or slow its progression. The DPM is also frequently applied to cross-sectional disability studies beyond the scope of the original model. To facilitate the application of the DPM in theory-driven knowledge generation, we undertook a critical review (Grant & Booth, Reference Grant and Booth2009) of 88 studies, summarised research on disability and disablement in the context of intrinsic DPM constructs (Table 1), and identified methodological limitations and pragmatic guidance for future research. We also examined evidence for the relationship between DPM constructs and disability measured at one time point to facilitate an evidence-based extension of the DPM to cross-sectional studies. We used this research summary to inform recommendations on measurement and modelling of DPM constructs.
Definition and Measurement of DPM Variables in Research
The relationships between constructs in the DPM are much more complex than they are often treated in empirical research. Intra-individual variables such as age and sex that are typically adjusted for as confounders may also act as effect modifiers of the relationships between DPM constructs (Carrière et al., Reference Carrière, Gutierrez, Pérès, Berr, Barberger-Gateau, Ritchie and Ancelin2011; Piernik-Yoder & Ketchum, Reference Piernik-Yoder and Ketchum2013). We also identified pathologies and impairments that have synergistic effects with other pathologies in their association with disability (Fried et al., Reference Fried, Bandeen-Roche, Kasper and Guralnik1999; Fultz et al., Reference Fultz, Ofstedal, Herzog and Wallace2003). These conceptual relationships have important implications for research design; if the level of an effect modifier is imbalanced among older adults in a study sample, it may skew results. We have identified a few effect modifiers in this study, but our list is not exhaustive. Gerontologists should have a low index of suspicion that putative confounders may be effect modifiers in the DPM and identify these a priori. At the analysis stage, results should be examined and reported by level of intrinsic effect modifiers to produce results specific to populations who experience disablement differently (Carrière et al., 2009).
In their original DPM manuscript, Verbrugge and Jette attested that “Presumptions that some [disability] domains matter more than others should be abandoned” (1994, p. 5), and we agree. However, on the basis of our critical review, we also advise that different disability domains (e.g., self-care, IADLs, occupational, etc.) be considered as separate outcomes in research, given the incomplete overlap between variables associated with each of them (Jackson et al., Reference Jackson, Jones, Tooth, Mishra, Byles and Dobson2015). A related issue is the substitution of terms such as “functional limitation” to identify disability outcomes, even in studies using the DPM as a guiding framework. We hypothesise that this occurs due to variation in how researchers from different disciplines interpret the terms “functional limitation” and “disability”. Our study echoes Verbrugge and Jette’s distinctions between these terms, wherein functional limitation indicates inability to perform physical and mental actions at the same level as one’s age-sex group, whereas disability is the interaction between functional limitation and one’s environment (1994). According to these definitions, functional limitation (e.g., difficulty lifting 10 pounds, slow timed-walk test) should be consistent across settings, whereas disability (e.g., dependence on others for help with toileting) is context-dependent and likely to vary depending on whether older adults are in home versus hospital environments.
The distinction between pathologies and impairments in the DPM also has implications for study design and analysis. Because impairments (e.g., cognitive impairment, balance impairment) are presumed to occur downstream of pathologies (e.g., Alzheimer’s dementia, heart failure) in the DPM, researchers must be wary of adjustment for impairments in models of pathology impacts on disablement as they are potentially adjusting for variables in the causal pathway. By applying Verbrugge and Jette’s definitions to examples from 88 empirical studies, we hope to have exemplified the use of these terms for more consistent use in future research on disability. From a practice perspective, distinctions between the terms in Table 1 are also relevant: The presence of chronic conditions in older adults (“chronic pathologies” in the DPM) should trigger clinicians to manage upstream intra-individual factors and aim to prevent downstream geriatric syndromes (“impairments” in the DPM). Older adults with new impairments (e.g., incontinence, recent weight loss) should conversely be assessed for worsening chronic pathologies with sub-optimal management.
Of the 88 studies we reviewed, 42 classified disability based on a count of ADLs people had difficulty with, or a dichotomous variable to indicate the presence or absence of disability. Future research may benefit from using validated and commonly employed measures of disability (Yang et al., Reference Yang, Ding and Dong2014), such as Katz or Barthel in community-dwelling older persons or the RAI ADL long-form score in nursing home residents. We further advise against use of counts or arbitrary scoring of select ADLs or dichotomization of disability as “present versus not”, as this renders findings across studies to be incomparable and risks classifying extremely heterogeneous groups of older adults as simply “disabled” (Nusselder, Looman, & Mackenbach, Reference Nusselder, Looman and Mackenbach2006).
Many of the relationships between variables and disability that we report are based on variables added to analyses for adjustment, or to predictive models aimed at maximizing the amount of variance in disability outcomes explained. We acknowledge these as important goals, but believe that more hypothesis-driven analyses of specific exposure-outcome relationships would offer important insights into the disablement process in older adults.
Analytic Considerations for Future Disability Research on Older Adults
We propose that future DPM-guided research use the variable summary from this review to identify relevant intrinsic DPM variables and assess their potential role in the DPM. For example, if a researcher were interested in the effect of malnutrition on disablement, Table 1 shows that only six of the studies we reviewed examined the independent effects of malnutrition or weight loss on disability or disablement, and the Supplementary Table 3 indicates that half of those studies were done in community-dwelling older adults. The specific references for each study could be found in Supplementary Table 1, and looked up to identify common MeSH terms to use in a systematic review. Depending on whether the systematic review revealed a paucity or abundance of literature on malnutrition and disablement, the researcher could either stop there or conduct a DPM-guided empirical study. Cases in which relevant constructs from the DPM are not measured should also be identified and explained by researchers, with likely implications for their findings examined.
We found examples of intrinsic variables representing DPM constructs specific to older adults residing in nursing homes (Table 1). The prevalence of disability is high in nursing home residents (Canadian Institute for Health Information, 2013), many of whom continue to experience disablement throughout the course of their stay (Dutcher et al., Reference Dutcher, Rattinger, Langenberg, Chhabra, Liu, Rosenberg and Zuckerman2014). By identifying person-level DPM variables specific to nursing home residents, this review provides an important starting point for research on this population.
Only 22 of 68 studies that examined disablement over time had more than one follow-up point. We posit that this is likely due to the time-consuming nature of clinicians’ collecting and recording disablement data that become available in health administrative databases and the great expense of measuring disablement purely for research purposes. Acknowledging that a single baseline and follow-up measure may be all that was logistically feasible in considered studies, we note that such measures are more sensitive to impermanent fluctuations in disability than measures based on multiple follow-up points (Wolinsky, Armbrecht, & Wyrwich, Reference Wolinsky, Armbrecht and Wyrwich2000). Given the availability of robust analytic methods (Murphy et al., Reference Murphy, Allore, Han, Peduzzi, Gill, Xu and Lin2015) and user-friendly statistical packages to assess multiple follow-up points over time (Rabe-Hesketh & Skronda, Reference Rabe-Hesketh and Skronda2012; Raudenbush & Bryk, Reference Raudenbush and Bryk2002), we recommend an increase in research funding for collection of these longitudinal data wherever possible.
Applicability of Findings to Other Models of Disability
This literature review aimed to operationalize the DPM, but is also relevant to researchers using the International Classification of Functioning Disability and Health (ICF) (World Health Organization, 2001) or the social model of disability (Oliver, Reference Oliver1990) to guide their disability research on older adults. In contrast with the DPM, the ICF is “reablement” skewed with constructs such as “activity” and “participation” mirroring the constructs of functional limitation and disability in the DPM. Many of the constructs identified in the ICF are the inverse of DPM constructs (Thyberg, Arvidsson, Thyberg, & Nordenfelt, Reference Thyberg, Arvidsson, Thyberg and Nordenfelt2015); therefore, our variable summary for intrinsic constructs could potentially be applied to operationalise the ICF as well. Similar to the DPM, the social model of disability distinguishes between physical impairments and disability, emphasising the role of societal structures in imposing restrictions on people with impairments to render them disabled (Oliver, Reference Oliver1990, p. 22). In keeping with this model, we have distinguished between functional limitations and disability (Putnam, Reference Putnam2002), and highlighted the intrinsic characteristics that may lead to the latter from the former.
Study Limitations and Strengths
We aimed to critically review the empirical evidence for intrinsic DPM constructs’ association with disability and disablement. Because the existing evidence in this area is so vast, a systematic review of evidence for relationships between variables within each DPM construct was neither appropriate nor feasible. Our non-systematic search and appraisal techniques are aligned with the aims of a critical review (Grant & Booth, Reference Grant and Booth2009; Mays et al., Reference Mays, Pope and Popay2005; Tricco et al., Reference Tricco, Antony, Soobiah, Kastner, Cogo, MacDonald and Straus2016), but may not be exactly replicable or capable of producing conclusive findings regarding variable relationships with disability. However, according to a recent review of knowledge synthesis methods for refining theory (Tricco et al., Reference Tricco, Antony, Soobiah, Kastner, Cogo, MacDonald and Straus2016), our team of academics and clinicians with expertise in this field is ideally suited to critically review extant evidence and identify significant findings.
We searched only two databases because of the large volume of studies they alone yielded, did not include grey literature or qualitative studies of older adults’ experience with disability, and may have omitted landmark research. We also may have over-sampled studies from North America, resulting from our inability to review work that was not in English and our familiarity with prevalent search terms. Our search term selection was based on terms that were familiar to our team from our past work in this field; this led to the omission of other possible search terms such as “correlat*”. Finally, due to the resource-intensive nature of this synthesis, we were unable to include studies published beyond June 30, 2015, when our synthesis began. These limitations render our findings regarding specific variable relationships with disability inconclusive. To reflect this, we have placed these variable-specific findings in the online Supplementary Tables 2 through 5 and recommend that each of these relationships be explored systematically before firm conclusions are drawn about them.
This review focused only on those variables representing intrinsic DPM constructs. We acknowledge that many of these constructs likely interact with extrinsic constructs (e.g., medications, institutional norms, area insurance policies) to affect disability and disablement; however, examination of these constructs was beyond the scope of this review for several reasons: (a) extrinsic characteristics measured at the person level are readily randomized in clinical trials and would thus be better summarized in systematic reviews; (b) extrinsic characteristics measured at the institutional and area level have already been critically reviewed elsewhere (Ågotnes et al., Reference Ågotnes, Jacobsen, Harrington and Petersen2016; Clarke & Nieuwenhuijsen, Reference Clarke and Nieuwenhuijsen2009; Liebel et al., Reference Liebel, Friedman, Watson and Powers2009; Philibert et al., Reference Philibert, Pampalon and Daniel2015; Pickett & Pearl, Reference Pickett and Pearl2001; Wahl et al., Reference Wahl, Fange, Oswald, Gitlin and Iwarsson2009); and (c) a critical review of all DPM constructs was not feasible for a single manuscript. We also did not examine activity modifications, such as changes in how older adults do everyday activities to accommodate functional limitations, as these data are not typically included in routinely collected health data. Our exclusion of these constructs is not an endorsement of their exclusion from disability and disablement research in older adults; critical reviews of evidence around these constructs are an important area of future research.
Although our methods do not allow for conclusions about causal relationships between constructs in the DPM, our critical review yielded measurement recommendations that will strengthen future studies of such relationships. This study used comprehensively described and appropriate methods to achieve clearly stated knowledge support aims that will aid researchers doing theory-driven research on disability in older adults. We also provide rich supplementary data on all 88 reviewed studies, which can be used as a launching point for specific research questions.
Conclusions
The DPM and related conceptual frameworks are critical to guide research on factors associated with disability and disablement in older adults. This study summarizes variables used to measure intrinsic DPM variables in 88 studies of older adults, the majority of whom lived in community settings. Despite evidence that age, sex, and geriatric syndromes may act as effect modifiers or relevant exposures in their own right, they were often examined only as adjustment variables, leaving knowledge gaps about their effect on disablement. Findings from 20 cross-sectional studies of disability support extension of the DPM to conceptualizing correlates of disability at single time points. Finally, common methodologic limitations of existing Gerontology research were summarized and pragmatic guidance to address them in future research was offered. These outputs can be applied by gerontologists to guide a more structured and consistent approach to theory-driven knowledge generation in this important field.
Supplementary Materials
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/S0714980819000758.




