Aging in Place
Older adults want to determine where and how they live, with many preferring to live in their own home in the community versus in a care facility (Dalmer, Reference Dalmer2019; Iecovich, Reference Iecovich2014; Wiles, Leibing, Guberman, Reeve, & Allen, Reference Wiles, Leibing, Guberman, Reeve and Allen2012). Aging in place can provide a sense of stability, independence, autonomy, and privacy (Fernandez-Carro, Reference Fernandez-Carro2016; Hatcher, Chang, Schmied, & Garrido, Reference Hatcher, Chang, Schmied and Garrido2019; Stones & Gullifer, Reference Stones and Gullifer2016) while potentially reducing health care costs related to residential care (Czaja, Reference Czaja2016; Dalmer, Reference Dalmer2019). However, aging in place requires resources, including supports from family and friend caregivers (Abramsson & Andersson, Reference Abramsson and Andersson2016; O’Rourke, Cappeliez, & Guindon, Reference O’Rourke, Cappeliez and Guindon2003; Pannell, Aldridge, & Kenway, Reference Pannell, Aldridge and Kenway2012; Wolff et al., Reference Wolff, Mulcahy, Huang, Roth, Covinsky and Kasper2018). When older adults and their caregivers are not adequately supported, aging in place can create stress, anxiety, and relational tensions (Ahn, Reference Ahn2017; Mittelman, Roth, Clay, & Haley, Reference Mittelman, Roth, Clay and Haley2007). Various forms of technology have been developed to provide supports to older adults and their family and friend caregivers.
Technology to Support Aging in Place
Increasingly, technologies have been developed to support older adults to remain living in their own homes. For example, various telehealth technologies have been developed to facilitate older adults’ self-management and to record data that health care providers find useful in maintaining the health of their patients, implementing care plans, or determining a diagnosis (Gatto & Tak, Reference Gatto and Tak2008; Grant, Rockwood, & Stennes, Reference Grant, Rockwood and Stennes2015; Kim, Gollamudi, & Steinhubl, Reference Kim, Gollamudi and Steinhubl2017). Wearable technologies include devices worn on the body to activate in the event of an emergency (Blackman et al., Reference Blackman, Matlo, Bobrovitskiy, Waldoch, Fang and Jackson2016) or clothes that contain information-gathering and communication capability such as heart rate, temperature, and movement (Eltis, Reference Eltis2005; Evans et al., Reference Evans, Papadopoulos, Silvers, Charness, Boot and Schlachta-Fairchild2016; Hanson, Takahashi, & Pecina, Reference Hanson, Takahashi and Pecina2013). Robots, artificial intelligence, and smart devices can contribute to aging in place through providing social interaction/companionship, safety reminders, information, and cleaning (Blackman et al., Reference Blackman, Matlo, Bobrovitskiy, Waldoch, Fang and Jackson2016; Choi, Demiris, & Thompson, Reference Choi, Demiris and Thompson2018; Queirós & da Rocha, Reference Queirós, da Rocha, Queirós and Rocha2018). Many of these technologies require active engagement, diligence, and high adherence on the part of the individual being monitored, making them unsuitable for some older adults with mobility and/or cognitive decline, such as patients with advanced Alzheimer’s or older adults with multiple illnesses (Kim et al., Reference Kim, Gollamudi and Steinhubl2017). Passive remote monitoring (PRM) technologies may thus provide certain advantages.
Passive Remote Monitoring Technologies
PRM technologies involve placing sensors unobtrusively within the home, sending information to health care providers or family/friend caregivers who can use this information to plan for and provide health care or intervene if necessary (Czaja, Reference Czaja2016; Khosravi & Ghapanchi, Reference Khosravi and Ghapanchi2016). These technologies do not require any actions or input on the part of the person being monitored.
Much of the research on PRM technologies to date has focused on specifics of information system platforms, developing and testing the platforms in pilot projects for function and usability, and investigating the potential of PRM platforms to fill the gaps in health care services (Payandeh & Park, Reference Payandeh and Park2020; Wang, Reference Wang2018). Because of the heterogeneity of research designs, technology involved, and outcomes measured in this area, the evidence of the impacts of in-home PRM technologies, specifically on older adults, their caregivers, and health care and social services, is often difficult to tease out. As the implementation of PRM technologies are advancing very quickly, it is imperative to synthesize current empirical knowledge on the outcomes of these technologies (Berridge, Reference Berridge2019).
Related Systematic Reviews
Systematic reviews have been conducted on technological devices such as wearable sensors (e.g., Baig, Afifi, Gholam, & Mirza, Reference Baig, Afifi, Gholam and Mirza2019; Majumder, Mondal, & Deen, Reference Majumder, Mondal and Deen2017; Noah et al., Reference Noah, Keller, Mosadeghi, Stein, Johl and Delshad2018) to monitor older adults’ health, but our definition of PRM technologies does not include wearable sensors that could be removed by the older person or not activated appropriately. Systematic reviews have also been conducted on smart homes that include monitoring technologies and other technologies to support older adults in their everyday lives to continue living in their own home (Liu, Stroulia, Nikolaidis, Miguel-Cruz, & Rincon, Reference Liu, Stroulia, Nikolaidis, Miguel-Cruz and Rincon2016; Turjamaa, Pehkonen, & Kangasniemi, Reference Turjamaa, Pehkonen and Kangasniemi2019). Lussier et al. (Reference Lussier, Lavoie, Giroux, Consel, Guay and Macoir2019) conducted a systematic review specifically on the detection of mild cognitive impairment utilizing in smart home sensors. Smart home technologies do not focus exclusively on PRM technologies and can include technologies that help older adults perform everyday activities.
Study Purpose and Relevance
The purpose of this scoping review was to synthesize research on PRM technology utilized to support community-dwelling older adults and the impact of this technology on older adults, their family and friend caregivers, and the health care system. To our knowledge, there has been no scoping review exclusively on PRM technologies integrated into older adults’ homes.
This review makes a timely contribution to the research literature by providing an overview of the current evidence about PRM designed to help older adults live in their homes longer. The results of this scoping review will also be instrumental in identifying gaps in our knowledge and informing future research, including the feasibility of using PRM technology with community-dwelling older adults.
Methods
Design
We conducted a scoping review using the steps outlined by Arksey and O’Malley (Reference Arksey and O’Malley2005) and refined by Levac, Colquhoun, and O’Brien (Reference Levac, Colquhoun and O’Brien2010). These steps included (1) developing the research question; (2) designing and conducting a search strategy in conjunction with a university librarian with database expertise; (3) selecting relevant studies from the list of retrieved articles, screening first by title, then abstract, then full text; (4) data extraction and charting; and (5) summarizing the studies.
Search Strategy
In consultation with a research librarian, we developed a “decision plan” (Levac et al., Reference Levac, Colquhoun and O’Brien2010) for our search strategy (Table 1). The design of the search strategy was guided by the research question: “What evidence exists about the effects of PRM technologies that support community-dwelling older adults to remain safely in their homes?” The research question was parsed using the elements of Population–Concept–Context (PCC), the methodology recommended by the Joanna Briggs Institute for scoping reviews (JBI, 2015). Search, subject, and MeSH terms were selected for each of these three elements. A search string including these terms was developed and used to search databases. The databases searched were Embase, CINAHL, PubMed, and Scopus. The initial search was conducted in May 2018. A second search was conducted in February 2019 to update the results and include any articles meeting the inclusion criteria that had been published since the initial search. This resulted in the addition of one additional study added to the included studies.
Table 1. Decision plan for developing the search

Inclusion criteria
Any peer-reviewed study or dissertation about older adults living in their homes with PRM technology from 2008 until February 2019 in English only.
Exclusion criteria
We did not include review articles, studies about wearable technology, telephone-based care, studies that describe a technology or algorithm (e.g., validation of an AI method or sensor technology), or studies of in-home simulation (e.g., apartments used as labs).
Literature Screening Protocol
A spreadsheet was used to create an article database to conduct article screening by title and abstract. Duplicate articles were identified and removed from the screening process. Screening of articles was conducted in three stages: (1) title screening, (2) abstract screening, and (3) full-text screening. The screening process is detailed in Figure 1.

Figure 1. Scoping review screening process.
Following the recommendations of Levac et al. (Reference Levac, Colquhoun and O’Brien2010), two reviewers independently screened the articles by title using the inclusion and exclusion criteria. If unsure whether an article should be included based on its title, the reviewers included the article for screening during the next stage. Reviewers’ decisions for inclusion of each article in the database were tracked, and discrepancies were flagged and resolved by a third reviewer.
The same process was applied to abstract screening. References of selected articles were searched as well as review articles that were excluded. Another reviewer screened these articles by title and abstract before adding the included articles to the full-text review. At the full-text screening stage, two teams of two reviewers screened articles for relevance by reading the full articles. Independent decisions on each article were compiled in spreadsheets, and one reviewer met with each team to discuss and reconcile discrepancies about inclusion.
Data Extraction and Charting
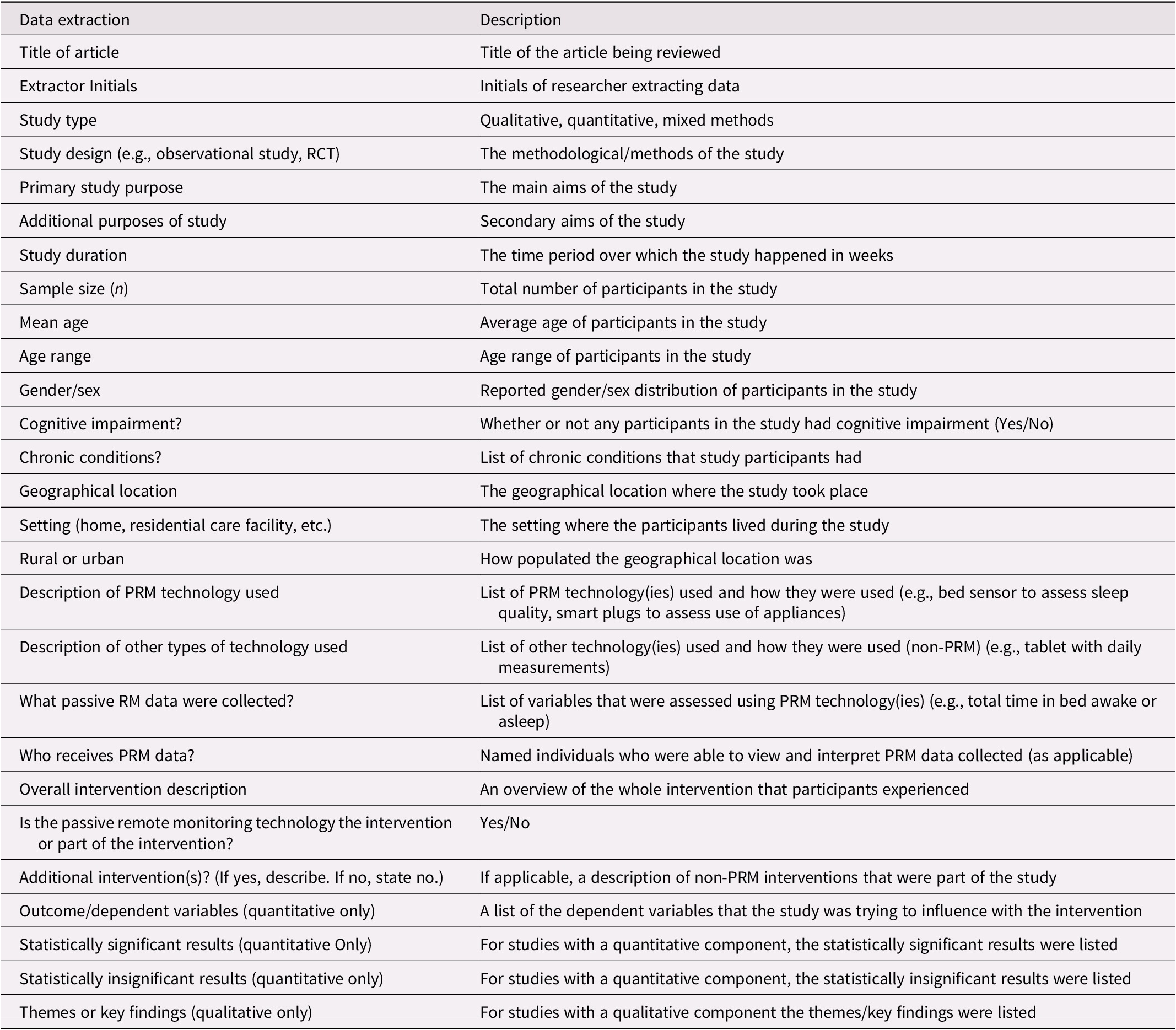
The review team collectively developed the data charting process, which included selecting and entering data from each included article into a customized spreadsheet. Following the recommendations of Levac et al. (Reference Levac, Colquhoun and O’Brien2010), the team first discussed variables to be extracted and developed the data extraction form (Table 2). To test the process, two articles were selected randomly for data extraction by all four reviewers. We then compared our findings for these articles and refined the process to enhance consistency. After this step, two teams of two reviewers were assigned one half of the articles each. Each reviewer independently reviewed the articles and charted the data using the data extraction form. Each pair of reviewers then compared their findings for each article. Where differences were identified, a fifth reviewer went back to the original articles to confirm the correct information was used.
Table 2. Data extraction template details
Summarizing the Studies
After charting the data from each study, we collated the results from all team members to create a descriptive numerical summary and synthesize the findings.
Results
Search Results
From an initial 486 unique articles, 14 articles met our inclusion criteria (see Figure 1). Seven articles were quantitative studies, four were qualitative studies, and three used mixed methods to respond to their respective research questions. Of the quantitative articles, one study was a pilot randomized controlled trial (RCT), five were longitudinal observational studies, and one was a pre-post observational study. All four of the qualitative studies used one-on-one interviews, with one using participatory research to develop and test a PRM system for older adults living with dementia and their family/friend caregivers. The mixed methods studies used a combination of longitudinal observation, survey, interviews, and case studies (Table 3).
Table 3. Characteristics and key findings from included studies
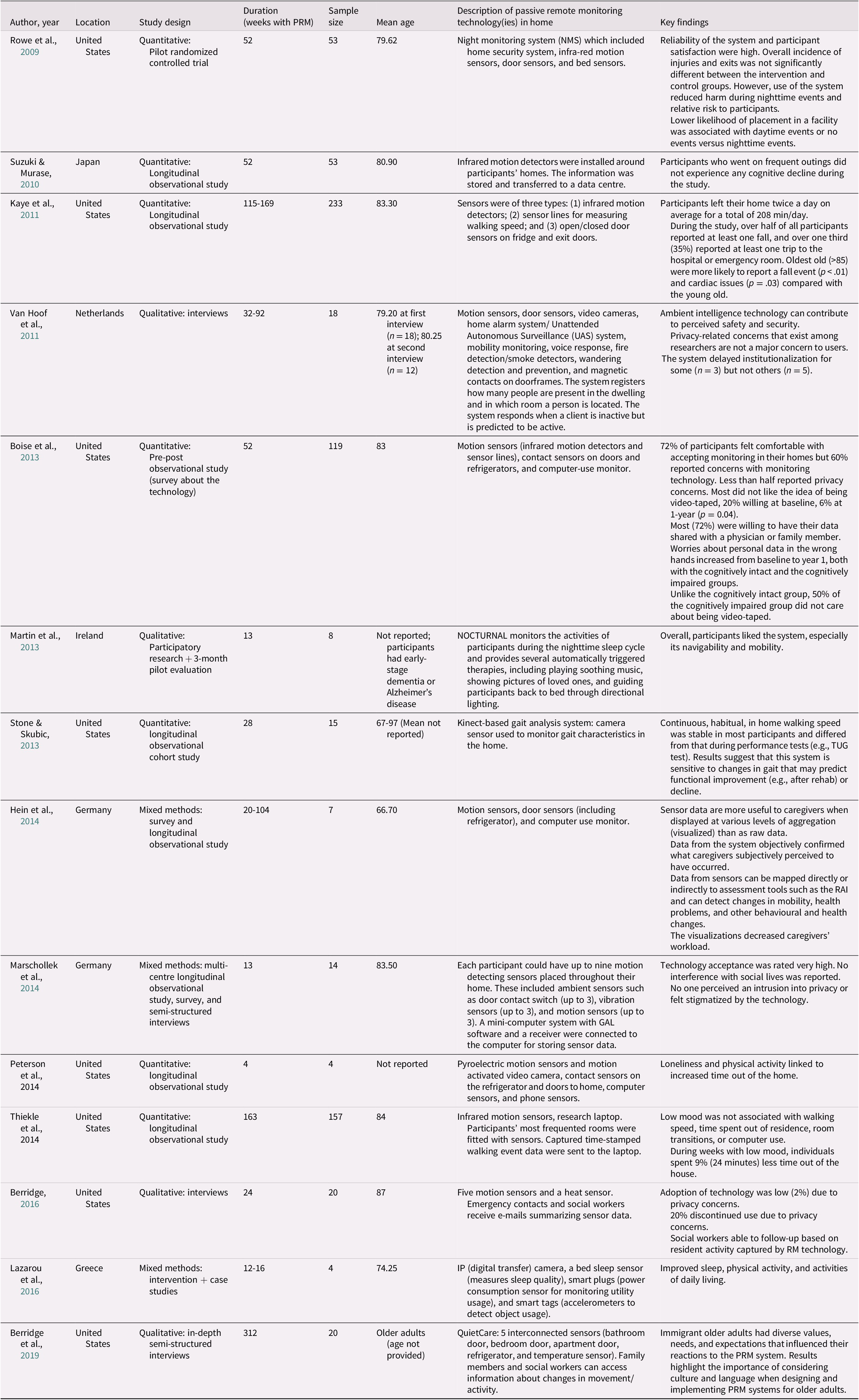
Although the PRM systems in every study collected data about participants, most studies were observational rather than interventional in nature. The observational studies used PRM systems to collect data (i.e., observe client behaviour) but did not initiate any sort of intervention based on the information collected. These studies typically collected data on variables that were likely to predict an adverse health event such as falls, cognitive decline, or institutionalization. Those that used the PRM system as an intervention generally operated by setting conditions that, when met, would trigger an intervention from a third party (e.g., family/friend caregiver or health care team). For instance, Rowe et al. (Reference Rowe, Kelly, Horne, Lane, Campbell and Lehman2009) measured nighttime events for cognitively impaired older adults by using a PRM system that detected when the users were out of bed during certain nighttime hours, waking the in-home caregiver to guide the user back to bed. In the study by Lazarou et al. (Reference Lazarou, Karakostas, Stavropoulos, Tsompanidis, Meditskos and Kompatsiaris2016), participants received tailored, adaptive clinical interventions from their health care team based on their needs and the observational data continually collected by the PRM system in their home.
The duration of PRM technology use in the home ranged from 4 to 312 weeks. Eight studies were conducted in the United States, two in Germany, and one each in the Netherlands, Japan, Ireland, and Greece. Eight studies were conducted in urban centres; one included both urban and rural settings, and five did not specify whether the context was urban or rural.
Nature of PRM System Configuration
PRM systems in the reviewed articles were determined based on what the investigators wished to understand. Sensor configurations ranged from a single sensor to a large array of sensors, cameras, and other passive monitoring devices (Table 4). PRM system configurations varied significantly in the number of sensors, sensor types, data acquired from systems, and interventions from the systems. The most frequently used sensor type reported in the studies was motion sensors for open spaces (n = 10), followed by door sensors (motion sensors that detect doors opening and closing or wireless magnetic contact sensors; n = 8), cameras, bed sensors and other sensors (n = 4 for each), and smart plugs (n = 1). PRM was sometimes combined with wearable (n = 1) and active, non-wearable (n = 3) technologies. The systems were configured to monitor and record a variety of behaviours, including gait parameters, sleep quality and nighttime activity, time outside of the home, level of daily activity, computer use, ADLs and personal hygiene, and falls and unusual periods of inactivity.
Table 4. PRM system configurations

Note: “X” indicates types of technology used in each study.
Participants
Research participants ranged from 4 to 233 individuals ranging in age from 49 to 97 years. Eleven of the 14 studies focused exclusively on older adults; one included both older adults and their caregivers, one looked at older adults and their social workers, and one looked primarily at older adults but also included cognitively impaired adults who were not necessarily older. Seven studies included adults with cognitive impairment, and one study included both family/friend caregivers and persons with dementia. The inclusion of caregivers and social workers accounts for the lower bound of the age range of participants (49 years). Eleven studies included both males and females, one study included only females, and two studies did not state the sex of their participants.
Effects of PRM
The included studies investigated the effects of PRM on a wide variety of outcomes ranging from incidence of injuries and falls to older adults’ and caregivers’ perceptions of safety and privacy. We grouped these outcomes into five main categories: (1) acceptance of PRM, (2) physical health, (3) mental health, (4) requiring higher level of care, and (5) effects on caregivers. Each will be described below, and categories are presented in Table 5.
Table 5. Effects of PRM on outcomes by category

User acceptance of PRM
Although almost every study (n = 11) examined user acceptance of the PRM system employed in their study, this varied considerably across studies, in how it was both conceptualized and measured. Participant satisfaction, perceived safety and security, privacy, technology acceptance, and adoption rate/dropout rate were concepts used by different research teams to get at the idea of participant acceptance of PRM.
Two studies examined participant satisfaction with PRM. Rowe et al. (Reference Rowe, Kelly, Horne, Lane, Campbell and Lehman2009) used the Quebec User Evaluation with Assistive Technology questionnaire (Demers, Weiss-Lambrou, & Ska, Reference Demers, Weiss-Lambrou and Ska2000) to assess participants’ satisfaction with PRM in terms of usability, ease of use, and effectiveness. They found that, on average, users were very satisfied with the nighttime monitoring system used in their study after 7 and 12 months of use. Martin et al. (Reference Martin, Augusto, McCullagh, Carswell, Zheng and Wang2013) used a participatory qualitative research design to understand the needs of people with dementia and inform the development of a nighttime monitoring system, which was then tested for three months in participants’ homes (n = 8). In this study, participant attrition was high because participant-reported dementia disease status was often more advanced than initially stated. However, for those who were able to participate, user acceptance of the PRM was high and several positive themes were identified through one-on-one interviews. These included: promoting independence, maintaining dignity, maximizing social inclusion, managing risk, and providing stimulation.
PRM was perceived as safe and secure by participants in a single qualitative study. Authors van Hoof, Kort, Rutten, and Duijnstee (Reference van Hoof, Kort, Rutten and Duijnstee2011) interviewed 18 older adults in the Netherlands three weeks before or immediately after having a PRM system installed in their home (see Table 4 for configuration of the system). Before installation, respondents expressed a strong desire to age in place and viewed the PRM system as a support tool that would keep them safe and secure. Many participants had already taken the initiative to ensure their safety at home by installing extra locks and/or barred windows to prevent burglary, installing fire detectors, and removing gas cooktops. After installation of the PRM system, most participants reported a heightened sense of safety and security knowing that the system was monitoring them 24/7 and that they would be able to get help if they needed it (e.g., during a fall where they could not get to the phone). However, the technology made one participant feel restless and uneasy, resulting in their having it removed.
The impact of PRM on privacy, as well as the impact of privacy on PRM adoption, was investigated in four studies. In van Hoof et al.’s (Reference van Hoof, Kort, Rutten and Duijnstee2011) study, privacy was only identified as a concern for 1 participant; for the other 17, it was a non-issue. Boise et al. (Reference Boise, Wild, Mattek, Ruhl, Dodge and Kaye2013) conducted a longitudinal survey to assess older adults’ willingness to share health and activity data with their physician or family members and their concerns about privacy and security after one year of in-home PRM. Of those who were cognitively intact (n = 92), 84% (n = 77) at baseline and 83% (n = 76) at 12 months were receptive to PRM (non-visual monitoring) in their home. For those with mild cognitive impairment (n = 27), 92% (n = 25) at baseline and 72% (n = 19) at 12 months were receptive to PRM in their home. However, responses to people being videotaped at home were quite different. At baseline, only 20% (n = 18) of those who were cognitively intact and 45% (n =12) of those with mild cognitive impairment were receptive to the idea of videotaped monitoring at home. This dropped to 7% (n = 6) and 30% (n = 8) for the two groups, respectively, at 12 months. Lastly, participant concerns about privacy with home-based PRM increased over the year of use; 41% (n = 38) of the cognitively intact and 32% (n = 8) of the mild cognitive impairment groups indicated concerns about their personal privacy at baseline, whereas 52% of both groups reported privacy concerns at 12 months (n = 48 and n = 12 for cognitively intact and mild cognitive impairment groups, respectively). In contrast, Marschollek et al. (Reference Marschollek, Becker, Bauer, Bente, Dasenbrock and Elbers2014) reported that none of their participants felt that their privacy was invaded by the PRM system used in their study, which consisted of door and motion sensors. They also reported that users did not feel stigmatized by having the technology in their homes.
Lastly, Berridge (Reference Berridge2016) found that only 20/1,000 (2%) older adults living in independent living residences in an American city were willing to try out the PRM technology; 98% (n = 980) rejected it because they felt that it was intrusive and would invade their privacy. In addition, 20% of users (n = 5) later discontinued its use for the same reasons. However, some users felt that because there were no cameras involved, their privacy was adequately protected. They also expressed that PRM felt less invasive than having a paid caregiver come into their home and provide personal care. In this care model, social workers were the recipients of residents’ data. While social workers felt that it provided them with valuable data to follow-up with residents, they also had to be careful about how they approached residents so that they did not feel like they were “being spied on”.
Three studies reported findings about technology acceptance. The findings of Boise et al. (Reference Boise, Wild, Mattek, Ruhl, Dodge and Kaye2013) and Marschollek et al. (Reference Marschollek, Becker, Bauer, Bente, Dasenbrock and Elbers2014) are reported above. In addition, Berridge, Chan, and Choi (Reference Berridge, Chan and Choi2019) found that cultural values and beliefs had a significant impact on the low acceptance of PRM technology by immigrant older adults in the United States. For example, Russian-born older adults unanimously rejected PRM, citing a preference for “hands-on” care from people rather than “a piece of plastic”. Meanwhile, Chinese- and Korean-born older adults expressed a desire not to burden their children by having them receive system alerts; they often accepted the PRM technology reluctantly to please their social worker.
Adoption rate/drop-out rate was reported in one study. As mentioned above, Berridge et al. (Reference Berridge2016) reported that only 2% (n = 20/1000) of older adults adopted the available PRM system and that 20% (n = 5) of adopters eventually discontinued its use due to privacy concerns.
Physical health
More than half (8/14) of the included studies examined the effects of PRM on physical health outcomes (Kaye et al., Reference Kaye, Maxwell, Mattek, Hayes, Dodge and Pavel2011; Lazarou et al., Reference Lazarou, Karakostas, Stavropoulos, Tsompanidis, Meditskos and Kompatsiaris2016; Martin et al., Reference Martin, Augusto, McCullagh, Carswell, Zheng and Wang2013; Petersen, Austin, Kaye, Pavel, & Hayes, Reference Petersen, Austin, Kaye, Pavel and Hayes2014; Rowe et al., Reference Rowe, Kelly, Horne, Lane, Campbell and Lehman2009; Stone & Skubic, Reference Stone and Skubic2013; Suzuki & Murase, Reference Suzuki and Murase2010; Tchalla et al., Reference Tchalla, Lachal, Cardinaud, Saulnier, Bhalla and Roquejoffre2012; Thielke et al., Reference Thielke, Mattek, Hayes, Dodge, Quiñones and Austin2014). Outcomes studied included falls, physical function and ADLs, physical activity, sleep, and unsafe exits from one’s home.
Three studies examined the incidence and outcome of falls using PRM. Kaye et al. (Reference Kaye, Maxwell, Mattek, Hayes, Dodge and Pavel2011) found that 56% (n = 130) of participants reported having at least one fall over the year-long study. Falls were self-reported weekly (not measured by the PRM system) and were significantly associated with older age. No associations were tested between falls and other data collected by the PRM system. Stone and Skubic (Reference Stone and Skubic2013) examined the feasibility, validity, and reliability of assessing fall risk using continuous in-home gait monitoring with the Microsoft Kinect camera and conducted gait analysis with the collected video data. These results showed that, for most people, gait analysis of the video data was comparable to validated physical performance tests that assess fall risk: the habitual gait speed (HGS) test and the timed up and go (TUG) test. However, there were certain situations, such as apartments with limited walking spaces and individuals with limited mobility, that reduced the effectiveness of the analysis. Tchalla et al. (Reference Tchalla, Lachal, Cardinaud, Saulnier, Bhalla and Roquejoffre2012) focused on reducing falls at night by using a motion sensor-activated light path that was activated when the participant would get out of bed. This intervention was shown to significantly decrease fall risk among community-dwelling older adults. In total, the proportion of falls at home was 9.6% for the intervention group (n = 94) and 25% for the control group (n = 96).
Physical function and physical activity were examined in a handful of studies. Kaye et al. (Reference Kaye, Maxwell, Mattek, Hayes, Dodge and Pavel2011) used sensors to measure walking speed, consistent periods away from the home, computer use, and where participants spent their time within their home. Participants, on average, left their home twice/day for almost two hours (108 minutes) total time. As noted above, Stone and Skubic (Reference Stone and Skubic2013) used PRM to assess gait as a way to measure fall risk. Thielke et al. (Reference Thielke, Mattek, Hayes, Dodge, Quiñones and Austin2014) used PRM to assess walking speed, time spent out of residence, and room transitions. In another study, Lazarou et al. (Reference Lazarou, Karakostas, Stavropoulos, Tsompanidis, Meditskos and Kompatsiaris2016) conducted a tailored, iterative intervention for four older adults with cognitive impairment. In this study, the PRM system collected data, which were then used to inform tailored weekly visits, interventions, and progress updates. The results showed that after the 12- to 16-week intervention, participants experienced significant improvements in moving intensity and ADLs, including bathroom and kitchen presence, as well as reduced time sitting and watching TV. An important finding in this study was that increased moving intensity resulted in longer durations of deep sleep and total sleep.
Few studies used PRM to assess the relationship between physical activity and psychosocial outcomes. For example, Peterson et al. (Reference Petersen, Austin, Kaye, Pavel and Hayes2014) used PRM to examine the relationship between loneliness and physical activity among older adults. They found that time spent out of the house was not an accurate measure of self-reported physical activity and that it was negatively correlated with loneliness (r = −0.44, p = 0.01). In another study, Suzuki and Murase (Reference Suzuki and Murase2010) investigated the association between daily activity and cognitive decline. Results indicated that cognitive decline was significantly associated with fewer outings (8.8 vs. 17.3).
Sleep and nighttime activity were other important physical health outcomes addressed in several studies. Three of these involved PRM-enabled sleep interventions. In 2009, Rowe et al. tested a night-monitoring system designed to reduce nighttime injuries and unsafe home exits in persons with dementia. Once motion detectors were activated, the system would alert a designated caregiver, which would allow the caregiver to wake up and assist the older adult. The results showed that when the system was in use, older adults were less likely to sustain an injury or leave their home at night. Another nighttime monitoring system called NOCTURNAL was developed by Martin et al. (Reference Martin, Augusto, McCullagh, Carswell, Zheng and Wang2013), using a participatory research design with people with dementia and their caregivers. This highly customizable tablet-based platform could be linked to a variety of sensors and allowed older adults and their caregivers to monitor the older adults’ nighttime behaviours and create tailored triggers to address them (e.g., lighting, music, photographs). Qualitative results suggested that both older adults and their family/friend caregivers felt comforted by having the system in place. It was unclear whether it improved sleep or reduced nighttime events. Lastly, sleep interventions were common in the Lazarou et al. (Reference Lazarou, Karakostas, Stavropoulos, Tsompanidis, Meditskos and Kompatsiaris2016) study that used PRM data to inform and adapt tailored interventions for study participants. All four participants had problems with their sleep at the beginning of the study and experienced improvements in their sleep as a result of the sleep data (total sleep time, time spent in different stages of sleep, sleep interruptions, and time spent awake in bed) generated from the PRM system and used by health care providers to develop effective interventions.
Mental health
Mental health variables investigated in the included studies included cognitive decline, loneliness, and mood (Marschollek et al., Reference Marschollek, Becker, Bauer, Bente, Dasenbrock and Elbers2014; Petersen et al., Reference Petersen, Austin, Kaye, Pavel and Hayes2014; Suzuki & Murase, Reference Suzuki and Murase2010; Thielke et al., Reference Thielke, Mattek, Hayes, Dodge, Quiñones and Austin2014). As discussed previously, Suzuki and Murase (Reference Suzuki and Murase2010) found that older adults who went on more outings were less likely to experience cognitive decline. PRM sensors were used to measure outings. Similarly, Petersen et al. (Reference Petersen, Austin, Kaye, Pavel and Hayes2014) found that older adults who left their home more often were less likely to report experiencing loneliness. Finally, Thielke et al. (Reference Thielke, Mattek, Hayes, Dodge, Quiñones and Austin2014) found that during weeks when participants reported low mood, they spent significantly less time out of their residence with no changes in physical activity parameters within the home (e.g., walking speed).
Requiring higher level of care
Two studies measured variables related to requiring a higher level of care (Kaye et al., Reference Kaye, Maxwell, Mattek, Hayes, Dodge and Pavel2011; van Hoof et al., Reference van Hoof, Kort, Rutten and Duijnstee2011). In the qualitative study by van Hoof et al. (Reference van Hoof, Kort, Rutten and Duijnstee2011), older adults consistently expressed a strong desire to age in place and perceived PRM as a support tool that could help them avoid going to a nursing home. Kaye et al. (Reference Kaye, Maxwell, Mattek, Hayes, Dodge and Pavel2011) reported that 35% (n = 82) of the participants in their study reported at least one trip to the hospital or emergency room during their study. There was no control group in this study and hospital/ER usage was not associated with use of the PRM system.
Effects on caregivers
Some studies provided evidence that PRM systems had significant implications for both formal and family/friend caregivers of older adults. For example, social workers reported that having data from PRM improved their knowledge of clients’ needs, allowing more efficient follow-up care with older adults (Berridge, Reference Berridge2016). However, as discussed, the social workers were attuned to participants’ privacy concerns and felt that they needed to be cautious in appearing too knowledgeable about participants’ needs and thoughtful in their approach to providing participant care. Hein et al. (Reference Hein, Steen, Thiel, Hülsken-Giesler, Wist and Helmer2014) found that paid caregivers’ perceived workload decreased when they had access to PRM data about their clients. Similarly, in the Lazarou et al. (Reference Lazarou, Karakostas, Stavropoulos, Tsompanidis, Meditskos and Kompatsiaris2016) study, family/friend caregivers reported that having access to older adults’ data through a computer dashboard provided them with a great sense of relief and comfort. They also reported that this particular intervention had significantly improved the health and well-being of their family member/friend, resulting in decreased stress, improved sleep, and quality of life for themselves as well.
Discussion
The findings from this scoping review reveal very limited research about the effects of PRM technology used in older adults’ homes to support aging in place. Most of the studies investigated the use of door and motion sensors, with less focus on other types of PRM technologies. Thus, questions remain about their impact. Significant variability was found in the aims, techniques, and system configurations employed across studies. This is likely the result of both the relative novelty of PRM technology and the limited degree of customization possible with more traditional health technologies or services. In addition, there was significant variation in research design, outcomes of interest, and measurement of outcomes across the included studies. This heterogeneity makes it challenging to compare systems and their effects on older adults and their caregivers, and highlights the appropriateness of conducting a scoping review, rather than a systematic review, to explore the research conducted in this area to date. Our findings are consistent with others’ that identified the need for larger studies that (1) are conducted by interdisciplinary research teams, (2) are theory-informed intervention studies, (3) seek longitudinal findings, (4) investigate an intersection of relevant outcomes, and (5) provide insight into the cost-benefits (financial, social, physical) of technology-enabled care (Liu et al., Reference Liu, Stroulia, Nikolaidis, Miguel-Cruz and Rincon2016; Noah et al., Reference Noah, Keller, Mosadeghi, Stein, Johl and Delshad2018; Schulz et al., Reference Schulz, Wahl, Matthew, DeVito, Beach and Czaja2015). These strategies need to be considered against the research challenges of participant recruitment, the short lifespan of technologies, limited insight regarding data collection, data ownership, and privacy concerns regarding commercial technology devices/systems (Liu et al., Reference Liu, Stroulia, Nikolaidis, Miguel-Cruz and Rincon2016; Noah et al., Reference Noah, Keller, Mosadeghi, Stein, Johl and Delshad2018; Schulz et al., Reference Schulz, Wahl, Matthew, DeVito, Beach and Czaja2015). This is an evolving field, and we anticipate that new and innovative forms of technology will continue to be available and need to be evaluated.
Although the amount of research is limited, we identified some important findings related to older adults’ acceptance of PRM systems. Older adults were more likely to accept home monitoring with systems that were perceived as safeguarding their privacy by not including video functions. This is consistent with the adoption of the technology model for remote monitoring of elders’ daily activities proposed by Mahoney (Reference Mahoney2011). Within this model, loss of privacy/intrusiveness is identified as a key barrier to use while individuals’ innovativeness/readiness to adopt PRM technologies is an important pre-disposing factor. Our findings also offer insight into successful PRM implementation strategies that allow increased familiarity of the technologies among older adults, which in turn increased older adults’ acceptance and appreciation (i.e., perceived safety) of the technology. For example, Martin et al. (Reference Martin, Augusto, McCullagh, Carswell, Zheng and Wang2013) included older adults with dementia or Alzheimer’s disease and their caregivers in the intervention design process, an approach that is both client-centred and makes adoption more likely.
There were several topics that were not well addressed by the studies in this scoping review. For example, the studies reviewed took place in urban contexts and none looked at the difference between rural health care and urban health care as they relate to PRM. The importance of this divide is that PRM systems may not be feasible in rural contexts depending on the system, its degree of connectivity, and the infrastructure that exists in a given rural context. The difference is also important for how rural community-dwelling adults interact with technologies such as PRM systems compared with their urban counterparts. Therefore, any discussion of feasibility across a broad region needs to address these issues.
In a similar vein, the research by Berridge (Reference Berridge2016) and Berridge et al. (Reference Berridge, Chan and Choi2019) highlighted an absence of the examination of the effects of cultural and economic backgrounds on the acceptance and feasibility of PRM technology. While these studies provided important information about how immigrant and low-income older adults see PRM technology, their studies show that numerous circumstances of older adults are likely to impact acceptability and these circumstances ought to be given more consideration in research design and as a research focus. Future research should examine how the design and implementation of home-based PRM technology impacts: (1) diverse populations, (2) across old-age cohorts, (3) those living alone or with limited social supports, and (4) users’ experience among the care team (i.e., older adults, family caregivers, home support workers, clinicians) (Liu et al., Reference Liu, Stroulia, Nikolaidis, Miguel-Cruz and Rincon2016; Noah et al., Reference Noah, Keller, Mosadeghi, Stein, Johl and Delshad2018). Among other important insights, the coronavirus disease (COVID-19) pandemic has called attention to the importance of technology across multiple care settings; the use of PRM among isolated (or quarantined) older adults constitutes important future research.
Overall, most of the studies looked at the impact of PRM technologies on client outcomes. Far fewer examined the impact of PRM systems on family/friend caregivers, health care providers, and the health system. The presence of family/friend caregivers is key to whether older adults with complex care needs can remain in their own home (Health Council of Canada, 2012; Williams et al., Reference Williams, Peckham, Watkins, Warrick, Tam and Rudoler2014). Yet this role can create increased risk of physical health problems, stress, burnout, and depression (Williams et al., Reference Williams, Peckham, Watkins, Warrick, Tam and Rudoler2014). While limited, the findings in this review point to PRM contributing to decreased stress among family/friend caregivers. Research is needed to explore the impact of home-based PRM systems on health care providers. Significant privacy, practice, and policy issues need to be considered for individuals providing care in clients’ homes. Similarly, there were no studies that conducted a cost analysis to consider the impact of PRM systems on health care utilization and long-term care placement. Evidence of the cost-effectiveness of PRM systems is recommended for inclusion in future research, as it will inform individual, family, and government decisions about implementation and scale-up of PRM systems within the home care setting.
One limitation of our study was that it was conducted in English only. We also included only studies that used PRM technologies in older adults’ homes. Therefore, it is possible that there is evidence about PRM technologies in other settings with different populations that are important but outside the scope of the current study. In addition, there is a diverse range of terms used to refer to PRM technology, so while we included as many terms as possible in our search strategy, it is possible that we did not include all of them.
Conclusion
PRM technologies are being used in innovative and diverse ways to support older adults aging in place and their caregivers. Our findings show that there is a need for more high-quality research on this topic. In particular, longitudinal and/or intervention studies examining the impacts of PRM technologies on both users (older adults and caregivers) and health systems are recommended avenues of future research.
Funding
This study was supported by funding from the Canadian Institutes of Health Research and the New Brunswick Health Research Foundation.









