Take-Home Points
1. The dopamine hypothesis of psychosis has become a classic and one of the most enduring ideas in psychopharmacology, especially as it relates to schizophrenia.
2. However, schizophrenia is not the only psychosis and dopamine is not the only neurotransmitter linked to psychosis.
3. Increasing evidence implicates both serotonin and glutamate networks as well as dopamine networks in the pathophysiology and treatment of some forms of psychosis, especially those related to Parkinson’s disease, dementias, and psychotomimetic drugs.
Introduction
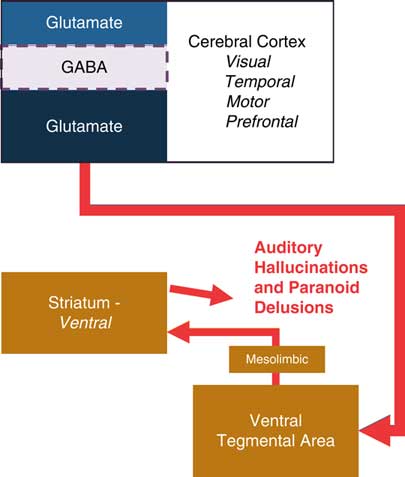
If one had asked any mental health clinician or researcher over the past 50 years what neurotransmitter was linked to psychosis, the resounding answer would have been dopamine, and specifically dopamine hyperactivity at D2 dopamine receptors in the mesolimbic pathway.Reference Meltzer and Stahl 1 , Reference Stahl 2 This so-called dopamine hypothesis of psychosis (Table 1 and Figure 1) makes sense because release of dopamine by amphetamine causes a paranoid psychosis similar to schizophrenia psychosis (Table 2), and drugs that block dopamine D2 receptors in the ventral striatum, part of the mesolimbic dopamine pathway, have been the mainstay of treatment for essentially all forms of psychosis for over 50 years.Reference Meltzer and Stahl 1 , Reference Stahl 2 This dopamine theory has proven so powerful that some may assume that all positive symptoms of psychosis are caused by excessive dopamine in the mesolimbic pathway and that all treatments must block dopamine D2 receptors there. As it turns out, however, there is much more to psychosis than dopamine, and there is much more to treatment of psychosis then D2 antagonists, as recently demonstrated by pimavanserin, a new treatment for Parkinson’s disease psychosis and an agent with serotonin 2A antagonist properties but no D2 antagonist properties at all.Reference Stahl 3 Thus, we are rapidly learning that psychosis is a condition involving dysregulation of multiple neurotransmitters in multiple pathways (Tables 1 and 2 and Figures 1–4)Reference Meltzer and Stahl 1 – Reference Rolland, Jardi, Amad, Thomas, Cottencin and Bordet 9 ; this understanding may lead to novel treatments that target pathways and receptors other than just D2 dopamine receptors in the mesolimbic pathway.

Figure 1 The dopamine hypothesis of psychosis. For half a century, psychosis, particularly auditory hallucinations and paranoid delusions, have been thought to be the result of hyperactivation of the dopaminergic mesolimbic pathway. The mesolimbic pathway projects from the ventral tegmental area (VTA) to the ventral striatum. The dorsal striatum is not thought to be affected by this hyperactivity because it is innervated via the nigrostriatal pathway from the substantia nigra and controls motor movements.
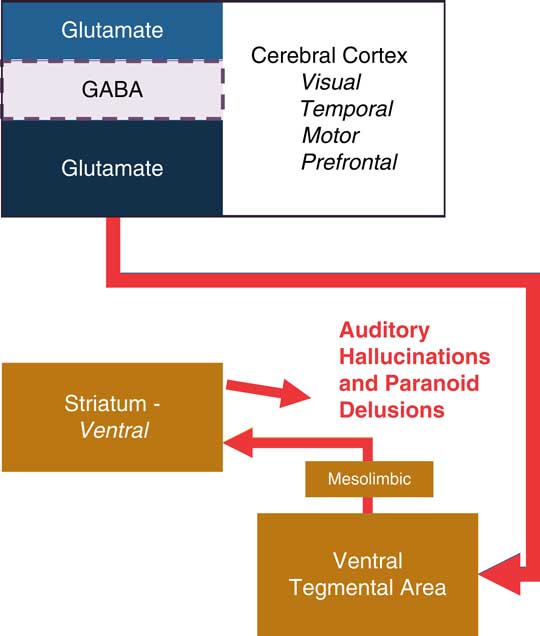
Figure 2 A recent theory suggests that psychosis in schizophrenia may be the result of hypofunctional NMDA receptors on GABA interneurons in the cerebral cortex This hypofunction may lead to overactivation of downstream glutamate signaling to the ventral tegmental area. Overactivation of this pathway may result in turn in excess dopamine in the ventral striatum via the mesolimbic pathway.
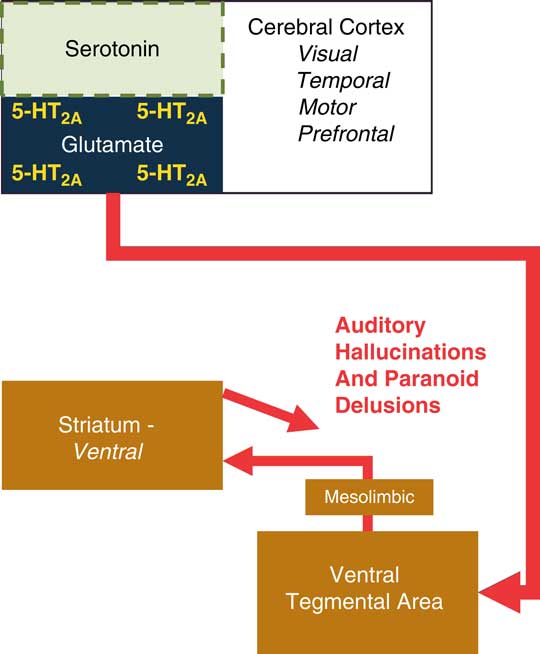
Figure 3 Psychosis cam be the result of hyperactivation of 5-HT 2A receptors on glutamate neurons. This hyperactivation may be due to excess serotonin, upregulated 5-HT2A receptors, or a psychedelic hallucinogenic 5-HT 2A agonist, all of which could lead to downstream release of glutamate. Glutamate release in the VTA may activate the mesolimbic pathway, resulting in excess dopamine in the ventral striatum.
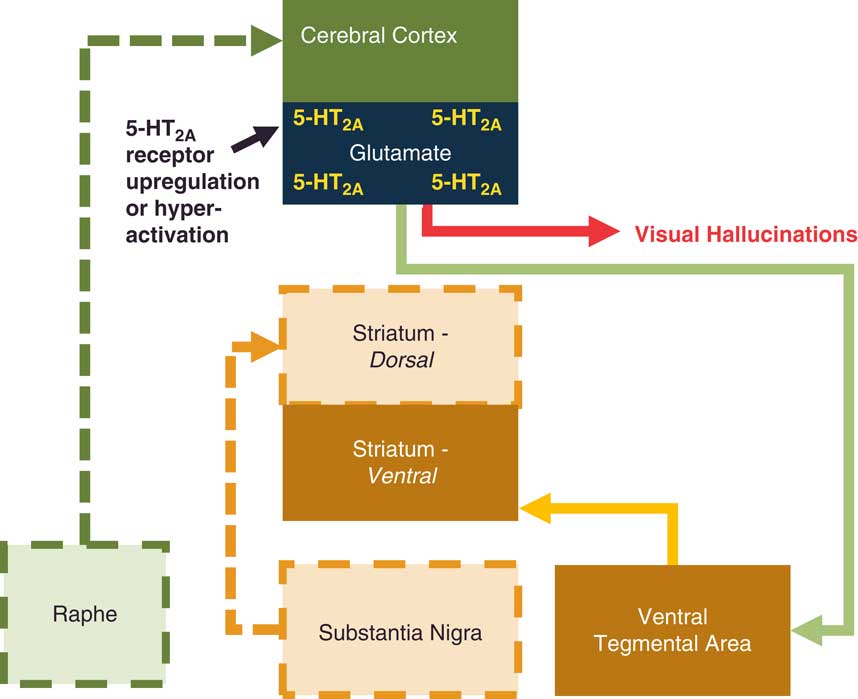
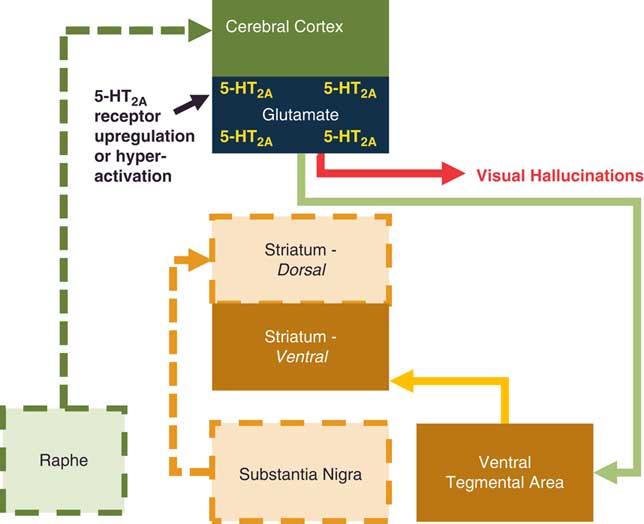
Figure 4 Excess glutamate signaling in the cerebral cortex, particularly the visual cortex, is thought to be associated with visual hallucinations. Upregulated 5-HT2A receptors on glutamate neurons, excessive serotonin release, or a psychedelic hallucinogenic 5HT1A agonist could all increase signaling to visual cortex and cause visual hallucinations.
Table 1 Three hypotheses of psychosis
Table 2 Pharmacologic models for three types of psychosis
Overview of 3 Hypotheses of Psychosis
In addition to the classical dopamine theory of psychosis (Table 1 and Figure 1), there is also the glutamate theory of psychosis (specifically the N-methyl-d-aspartate or NMDA hypoactivity theory), which proposes that NMDA receptor hypofunction in the prefrontal cortex can result in psychosis (Table 1 and Figure 2),Reference Stahl 2 and also the serotonin theory, which posits that cortical serotonin/5-hydroxytryptamine 5-HT2A hyperfunction can also result in psychosis (Table 1 and Figure 3).Reference Stahl 3 Each of these theories and neuronal networks will be reviewed here briefly. Although there are now at least 3 major theories, 3 major neurotransmitters, and 3 major neuronal networks hypothesized to underlie one or another psychosis, it is also important to keep in mind that all 3 theories involve interconnected pathways, and it is likely that in many different forms of psychosis, more than 1 of these pathways is involved (see Figures 2–4).
If one stops to think about it, clinicians have known about these 3 neurotransmitters and how they are linked to different causes of psychosis for a long time based on pharmacological models (Table 2).Reference Mahoney, Kalechstein, De La Garza and Newton 4 – Reference Rolland, Jardi, Amad, Thomas, Cottencin and Bordet 9 That is, clinicians have long observed the psychotomimetic effects of psychostimulants, dissociative anesthetics, and psychedelics.Reference Mahoney, Kalechstein, De La Garza and Newton 4 – Reference Rolland, Jardi, Amad, Thomas, Cottencin and Bordet 9 Psychostimulants such as cocaine and amphetamine release dopamine and cause D2 receptor stimulation that results mostly in auditory hallucinations and paranoid delusions (Table 2).Reference Meltzer and Stahl 1 , Reference Stahl 2 , Reference Mahoney, Kalechstein, De La Garza and Newton 4 Dissociative anesthetics such as phencyclidine (PCP) and ketamine are NMDA antagonists that result in visual hallucinations and paranoid delusions as well as a dissociative state (Table 2).Reference Powers, Gancsos, Finn, Morgan and Corlett 5 Hallucinogens/psychedelic drugs such as lysergic acid diethylamide (LSD) and psilocybin are mostly 5-HT2A agonists that result in visual hallucinations and mystical delusions, sometimes with retained insight (Table 2).Reference Vollenweider, Vollenweider‐Scherpenhuyzen, Bäbler, Vogel and Hell 6 – Reference Rolland, Jardi, Amad, Thomas, Cottencin and Bordet 9
Supporting these pharmacologic observations of specific psychotic symptoms in users of different drugs are observations that symptoms of psychosis caused by neurological and psychiatric disorders are also not identical to each other. This suggests that different causes of psychosis involve different degrees of input from the 3 psychosis-linked pathways. For example, the auditory hallucinations and paranoid delusions of theoretically hyperactive dopamine neurons in schizophrenia are not identical to some of the symptoms of Parkinson’s disease psychosis and psychosis associated with dementia. These latter psychoses are associated with mainly visual hallucinations and persecutory or jealous delusions, often with retained insight, at least early in the course of the disease.Reference Stahl 3 , Reference Ravina, Marder and Fernandez 10 , Reference Fénelon, Soulas, Zenasni, Cleret and de Langavant 11 Also, these latter forms of psychosis can be treated with the 5HT2A antagonist pimavanserin, which lacks D2 dopamine antagonist properties.Reference Stahl 3 Such observations suggest a more robust involvement of the serotonin 2A receptor and the serotonin network in the psychosis associated with Parkinson’s disease and with dementia.
The Classical Dopamine Hypothesis of Psychosis and Hyperactivity at Dopamine D2 Receptors in Dopamine Neural Networks
The classical and well-worn theory of psychosis of course is that dopamine hyperactivity in the mesolimbic dopamine pathway at dopamine D2 receptors is the cause of the positive symptoms of schizophrenia, with all antipsychotics acting to block D2 receptors there.Reference Meltzer and Stahl 1 , Reference Stahl 2 Hyperactivity of dopamine in the ventral striatum from neuronal projections coming from the ventral tegmental area (Figure 1) is theoretically to blame for delusions, often paranoid, and hallucinations, often auditory, especially in schizophrenia and manic psychosis. The “price of doing business” in blocking D2 receptors in this mesolimbic dopamine pathway is to simultaneously block the D2 receptors in the nigrostriatal pathway from the substantia nigra to the dorsal striatum, causing movement disorders such as akathisia, drug induced parkinsonism, and long-term tardive dyskinesiaReference Meltzer and Stahl 1 , Reference Stahl 2 (see also Figure 1).
The Glutamate Hypothesis of Psychosis: Hypoactivity at NMDA Glutamate Receptors in Glutamate Networks and the Links to Downstream Dopamine Networks
An exciting and relatively more recent development in the theories of psychosis is the notion that dopamine hyperactivity is actually a downstream consequence of glutamate dysregulation in the prefrontal cortexReference Stahl 2 (Figure 2). Specifically, the NMDA hypoactivity theory of psychosis suggests that hypofunctional NMDA receptors on GABA interneurons in the prefrontal cortex—perhaps due to abnormal neurodevelopment—lead to overactive downstream glutamate signaling (Figure 2). It may be that this overactive glutamate introduced by excessively stimulating the mesolimbic dopamine pathway in the ventral tegmental area (VTA) is actually the cause of auditory hallucinations and paranoid delusions.
The Serotonin Hypothesis of Psychosis: Hyperactivity at Serotonin 5HT2A Receptors in Serotonin Networks and the Links to Downstream Dopamine Networks
If the glare of the dopamine hypothesis blinded some of us to the possibility of alternate explanations for psychosis, it created a dilemma for patients with psychosis secondary to Parkinson’s disease or Alzheimer’s disease, since treatment with D2 blockers causes harm to these patients, worsening movements in Parkinson’s disease and increasing the risk of death in Alzheimer’s disease.Reference Stahl 2 , Reference Stahl 3 , Reference Ravina, Marder and Fernandez 10 , Reference Fénelon, Soulas, Zenasni, Cleret and de Langavant 11 Dogma dictated that all psychoses were due to excessive mesolimbic dopamine and all treatments needed to block D2 receptors. While this characterization worked well for patients with manic psychosis or depressive psychosis, as well as the psychosis of schizophrenia,Reference Meltzer and Stahl 1 , Reference Stahl 2 it obviously was not ideal for patients with other types of psychosis.
The paradigm-breaking observation for these psychotic illnesses was that 5HT2A antagonism without D2 antagonism has proven effective in treatment of psychotic symptoms due to Parkinson’s disease with preliminary evidence for efficacy in psychosis of dementia as well.Reference Stahl 3 This naturally leads to the question of whether serotonin is hyperactive at 5HT2A receptors in these disorders (Figures 3 and 4),Reference Ballanger, Strafella and van Eimeren 12 , Reference Huot, Johnston and Darr 13 just like what happens when psychedelic hallucinogens cause psychosis (Table 2).Reference Vollenweider, Vollenweider‐Scherpenhuyzen, Bäbler, Vogel and Hell 6 – Reference Rolland, Jardi, Amad, Thomas, Cottencin and Bordet 9 If so, one might also ask, “How does serotonin became hyperactive at 5HT2A receptors and thus how is 5HTA antagonism without D2 antagonism therapeutic?” The answer seems to be that excess serotonin activation of 5HT2A receptors in Parkinson’s disease psychosis or the dementia of psychosis can be due to excess release of serotonin activating 5HT2A receptors, to an increase in the expression of 5-HT2A receptors, or both.Reference Stahl 3 , Reference Ballanger, Strafella and van Eimeren 12 , Reference Huot, Johnston and Darr 13 Regardless of the mechanism of activation, the result is the same: downstream release of glutamate (Figures 3 and 4). As it turns out, some of these glutamate neurons project to the VTA and activate it (Figure 3). This process can then further activate the mesolimbic dopamine pathway as part of a chain reaction leading to psychosis causing typical auditory hallucinations and paranoid delusions (Figure 3). Glutamate hyperactivity driving neurons in the visual cortex may even more commonly cause visual hallucinations (Figure 4).
Summary and Conclusions
In summary, there are 3 interconnected pathways theoretically linked to hallucinations and delusions: dopamine hyperactivity at D2 dopamine receptors in the mesolimbic pathway, which extends from the VTA to the ventral striatum; NMDA receptor hypoactivity at GABAergic interneurons in the prefronal cortex; and serotonin hyperactivity at 5-HT2A receptors on glutamate neurons in the cerebral cortex. All 3 neuronal networks and neurotransmitters are linked together, and both 5HT2A and NMDA receptor actions can result in hyperactivity of the downstream mesolimbic dopamine pathway.