Introduction
The birth of a child can take a physical, emotional, and social toll on mothers. In addition to the permanency of change and the adoption of a new identity, mothers are met with a series of demands and expectations (e.g., frequent feedings, infant sleep routines, child nurturance) requiring immense energy that is often most onerous between infancy and toddlerhood (Abrams & Curran, Reference Abrams and Curran2011). Consequently, some mothers may go on to develop long-lasting depressive, anxiety, or post-traumatic related symptoms, otherwise described as internalizing distress (Holditch-Davis et al., Reference Holditch-Davis, Santos, Levy, White-Traut, O’Shea, Geraldo and David2015). Internalizing distress, characterized by a wide spectrum of unpleasant feelings (e.g., fatigue, restlessness, or irritability) or negative emotions (e.g., feeling hopeless, worthless, and sad), is often triggered by major life transitions such as childbirth. Consequently, internalizing distress can impair mothers’ daily functioning and confer risk for maladaptive child behaviors (e.g., withdrawal, aggression, inattentiveness; Goodman & Garber, Reference Goodman and Garber2017; Horwitz, Reference Horwitz2007). Notably, internalizing distress is a core characteristic of and contributor to several mental health disorders such as major depressive disorder (MDD; American Psychiatric Association, 2013; Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby, Brown, Carpenter, Caspi, Clark, Eaton, Forbes, Forbush, Goldberg, Hasin, Hyman, Ivanova, Lynam, Markon and Zimmerman2017).
Mothers’ internalizing distress and child adjustment
The first five years of a child’s life are critical for brain and socioemotional development and set the foundation for school readiness and later socioemotional skills (Grantham-McGregor et al., Reference Grantham-McGregor, Cheun, Cueto, Gleww, Richter and Strupp2007; Ruble, Reference Ruble and Zanna1994). However, the presence of internalizing distress among mothers may hinder healthy child development (Harris & Santos, Reference Harris and Santos2020; O’Conner et al., Reference O’Conner, Langer and Tompson2017). Goodman and Gotlib (Reference Goodman and Gotlib1999) posit that maternal distress may impair mother–child interactions, which may lead to children’s adverse psychological and behavioral outcomes (e.g., anxiety, depression, aggression, or hyperactivity). These outcomes may increase the risk for difficulties, including impaired cognitive, social, academic, and mental health functioning in adolescence and later adulthood (Hinshaw, Reference Hinshaw1992a, Reference Hinshaw1992b). Despite these negative implications, there is little research examining the longitudinal impact of mothers’ mental health on child outcomes, especially among disadvantaged populations where the risk of psychopathology is highest (Harris & Santos, Reference Harris and Santos2020).
Despite a large body of research linking maternal mental health to child development, the majority of these samples were non-Hispanic White (Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Harris & Santos, Reference Harris and Santos2020; Park et al., Reference Park, Brain, Grunau, Diamond and Oberlander2018). However, marginalized populations may be more susceptible to internalizing distress given possible disproportionate exposure to stressors such as perceived racial/ethnic discrimination, financial hardship, an anti-immigrant climate, acculturative stress, and interpersonal trauma (Beeber et al., Reference Beeber, Schwartz, Martinez, Holditch, Bledsoe, Canuso and Lewis2014; Halim et al., Reference Halim, Moy and Yoshikawa2015; Harris & Santos, Reference Harris and Santos2020; Valdez et al., Reference Valdez, Raines, Davies and D’Costa2018). Indeed, 30–60% of Latina American and African American mothers reported postpartum distress compared to 10–15% of non-Hispanic White mothers (Anokye et al., Reference Anokye, Acheampong, Budu-Ainooson, Obeng and Akwasi2018; Beeber et al., Reference Beeber, Schwartz, Martinez, Holditch, Bledsoe, Canuso and Lewis2014; Breslau et al., Reference Breslau, Aguilar-Gaxiola, Kendler, Su, William and Kessler2006; McGuire & Miranda, Reference McGuire and Miranda2008). Thus, more attention is needed to understanding the timing and chronicity of postpartum mental health of ethnic minoritized mothers and its impact on child adjustment outcomes.
However, to our knowledge, no research to date has prospectively considered the timing and chronicity of maternal internalizing distress with a focus on ethnic minoritized families. Further, most studies looking at the timing and chronicity of maternal psychological distress are typically limited to two to three time points or assessed at different periods of development (e.g., pregnancy, early postpartum; Harris & Santos, Reference Harris and Santos2020). Few studies examine trajectories of mothers’ psychological distress over multiple time points across the first 6 years postpartum as the current study does.
Present research
The current prospective, longitudinal study explored the variation in patterns and developmental trajectories of maternal internalizing distress over the course of the first six years following childbirth among African American, Mexican immigrant, and Dominican immigrant mothers. We hypothesized that distinct longitudinal patterns in mothers’ internalizing distress trajectories would predict different adjustment outcomes for their children in first grade. Specifically, we expected that mothers who experienced greater levels of internalizing distress that continued across the first six years following childbirth would have first graders who exhibited more maladaptive child adjustment outcomes (e.g., greater internalizing behaviors, externalizing behaviors, and hyperactivity) compared to mothers who consistently experienced lower levels of internalizing distress across the first six years following childbirth.
Methods
Participants and procedure
Participants were recruited as part of a larger study on culture and school readiness. Recruitment and data collection were conducted by the New York University Center for Research on Culture, Development, and Education following approval from the institutional review board at New York University and three participating public hospitals within a large metropolitan area. Through stratified sampling, a community-based sample (N = 324) of 34.6% African American (n = 112), 29.9% Mexican immigrant (n = 97), and 35.5% Dominican immigrant (n = 115) mother–child dyads were recruited from maternity wards following childbirth (see Table 1). Participants were eligible if they were over 18 years of age, were not living in a shelter, and had given birth to a full-term baby with a healthy weight (greater than 2500 g). Focal children ranged from being first-born (37.5%; 30.9% second-born, 16.9% third-born) to eighth-born and on average were second-born (M = 2.24, SD = 1.47). Informed consent was collected either in person, at the hospital, or via mail. The final sample (N = 272) included data for 33.8% African American (n = 92), 29.8% Mexican immigrant (n = 81), and 36.4% Dominican immigrant (n = 99) mothers (see Figure S1 and Table S1 for missing data).
Table 1. Descriptive statistics of sample demographics
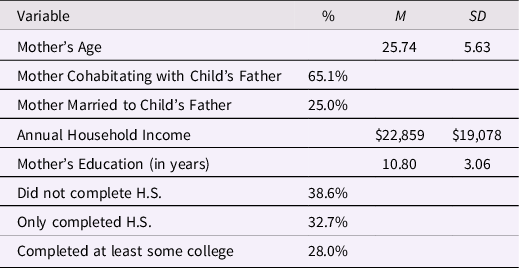
Note. Participants were eligible if they were over 18 years of age, were not living in a shelter, and had given birth to a full-term baby with a healthy weight (greater than 2500 g).
Participants were interviewed and assessed by a trained, bilingual female research assistant in the mother’s preferred language (English, Spanish, or both English and Spanish) at various assessment time points over a six-year timeframe at six, 14, 24, 36, 52, 64, and 79 months following childbirth. Given the participants’ varying levels of literacy, interviewers verbally read all interview questions to participants. The six-month interview was completed over the phone and participants received $40 for their time. The 14-, 24-, and 36-month interviews were completed in person within the participant’s home and they were given $75 for each visit. Finally, the 52-, 64-, and 79-month interviews were completed in person at the university’s research lab and participants were compensated $100 for each visit. The duration of each interview was approximately 2–3 hours at each wave.
Measures
Mother’s internalizing distress
Internalizing distress was assessed at seven time points using the Kessler Psychological Distress Scale (K6), a generalized distress scale often used as a mental health screening questionnaire for mood disorders (e.g., MDD), at approximately six, 14, 24, 36, 52, 64, and 79 months following childbirth (Kessler et al., Reference Kessler, Andrews, Colpe, Hiripi, Mroczek, Normand, Walters and Zaslavsky2002). The K6 is a six-item questionnaire that queries symptoms of anxiety and depression in the past 30 days (e.g., “In the last 30 days, how often did you feel hopeless?”) using a five-point scale (1 = None, 2 = A little of the time, 3 = Some of the time, 4 = Most of the time, 5 = All of the time). Responses on these six items were averaged together to yield an internalizing distress score ranging from 1 (no distress) to 5 (severe distress) for each time point (grand M = 1.82, SD = 0.67; actual range = 1.00 to 5.00). Higher scores on the K6 indicated higher levels of internalizing distress. The K6 has evidenced clinical validity with structured diagnostic interviews and has been validated among ethnic minoritized samples in previous studies (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Koretz, Merikangas, Rush, Walters and Wang2003; Prochaska et al., Reference Prochaska, Sung, Max, Shi and Ong2012; Valdez & Langellier, Reference Valdez and Langellier2015). In this sample, internal reliability was adequate at each wave (α = 0.76, 0.81, 0.76, 0.82, 0.79, 0.81, and 0.81, for 6, 14, 24, 36, 52, 64, and 79 months, respectively), with an average α = 0.80 across all waves, and a reliability of change of R C = 0.90. Additionally, native Spanish speakers, who were also fluent in English, translated the K6 into Spanish with back-translations, while also referring to the previously validated Spanish version (National Comorbidity Survey, n.d.). Depending on the participant’s preference, the K6 was administered in either English (n = 114, α = 0.86), Spanish (n = 97, α = 0.91), or both Spanish and English (n = 61, α = 0.91).
Child adjustment outcomes
Mothers completed a six-item Internalizing Behaviors scale that was originally adapted by the Head Start REDI Project from the Children’s Behavioral Questionnaire (CBQ; Putnam & Rothbart, Reference Putnam and Rothbart2006) and the Observation of Child Adaptation-Revised questionnaire (Werthamer-Larrson et al., Reference Werthamer-Larrson, Kellam and Wheeler1991) (see Willner et al., Reference Willner, Gatzke-Kopp and Bray2016) when children were in 1st grade. Items measured withdrawal behaviors (e.g., “Avoids playing with other children,” “Keeps to [him/herself], tends to withdraw”) and internalizing symptoms (e.g., “Sad, unhappy (anxious/depressed),” “low energy, lethargic, or inactive”). Responses were rated based on the frequency of a child’s certain behavior (0 = Never, 1 = Rarely, 2 = Sometimes, 3 = Often, 4 = Very Often, and 5 = Always) (possible range = 0.00 to 30.00). The six items were summed together with higher scores indicating increased internalizing behaviors (M = 9.51, SD = 3.07; actual range = 3.00 to 18.00; α = 0.84).
Mothers also completed two six-item subscales of the Social Skills Rating Scale (SSRS) of Problem Behaviors (Gresham & Elliot, Reference Gresham and Elliot1990) that assessed their child’s externalizing and hyperactive behaviors. Items assessed the frequency (0 = Never, 1 = Sometimes, 2 = Very often) of behaviors such as poor control of temper, arguing, and verbal or physical aggression towards others [externalizing] (e.g., “Fights with others”), and excessive movement or fidgeting and impulsive reactions [hyperactivity] (e.g., “Acts impulsively”). Scores were summed and could range from 0-12 for both externalizing (M = 4.19, SD = 2.41; α = 0.71; actual range = 0.00 to 10.00) and hyperactivity subscales (M = 3.45, SD = 2.15; α = 0.78; actual range = 0.00 to 11.00). Higher scores indicated greater externalizing and hyperactive behaviors. Although externalizing behavior and hyperactivity were moderately correlated in this sample, r(153) = 0.65, p = 0.001, we made the decision a priori to examine these two behaviors separately based on existing evidence indicating that these are two distinct constructs (Hinshaw, Reference Hinshaw1987).
Demographics
Demographic variables were collected as covariates from participants at baseline following childbirth. Participants were asked to report their ethnicity, age, marital and cohabitational status, and socioeconomic status (i.e., household income and education) (see Table 1) and focal child’s birth order. Analyses showed that the child’s birth order was not significantly linked to any of the primary variables in the study (mother’s internalizing distress, child’s internalizing, externalizing and hyperactivity behaviors) and was thus not included as a covariate for the sake of parsimony.
Analytic approach
We adopted a stepwise approach to first establish base classification of individuals into trajectory classes/groups (i.e., measurement model) and then used those trajectory classes/groups to predict differences in downstream child outcomes adjusting for demographic factors (i.e., structural model). A growth mixture model (GMM) using full information maximum likelihood estimation was performed to identify common patterns of internalizing distress trajectories among African American and Latina immigrant mothers from shortly after their child’s birth to when their child entered first grade. GMM can identify classes of categorically similar average response profiles when a variable is assessed across multiple time points (see Figure 1A; Kreuter & Muthén, Reference Kreuter and Muthén2008; Muthén & Shedden, Reference Muthén and Shedden1999). Although intraindividual changes (i.e., individual trajectories) were observed over the six years, classes were estimated such that between-person (interindividual) differences that shared common growth trajectories or patterns of change were assigned to the same class based on average distress symptoms. This first part of the analysis served to determine the optimal number of classes that would account for the variability in mothers’ individual internalizing distress trajectories. Criteria used to evaluate the number of classes that best fit the data included examining relative entropy (i.e., latent class categorization precision; Muthén, Reference Muthén2008), the Vuong-Lo-Mendell-Rubin (VLMR) Likelihood Ratio Test (LRT), and the parametric bootstrap LRT of models with different numbers of classes. Unlike latent transition analysis (LTA), which describes individual transitions between different classes, GMMs take the mean at each time point to create specific latent profiles with each individual being associated with a single class or subgroup (Lane et al., Reference Lane, Bluestone and Burke2013). In addition, GMMs can handle missing data at assessment time points allowing us to include all available data, including participants with incomplete data (see Figure S1). Furthermore, the GMM approach helps to reduce the possibility of making Type I errors by aggregating the waves of data across each mother’s set of distress reports.
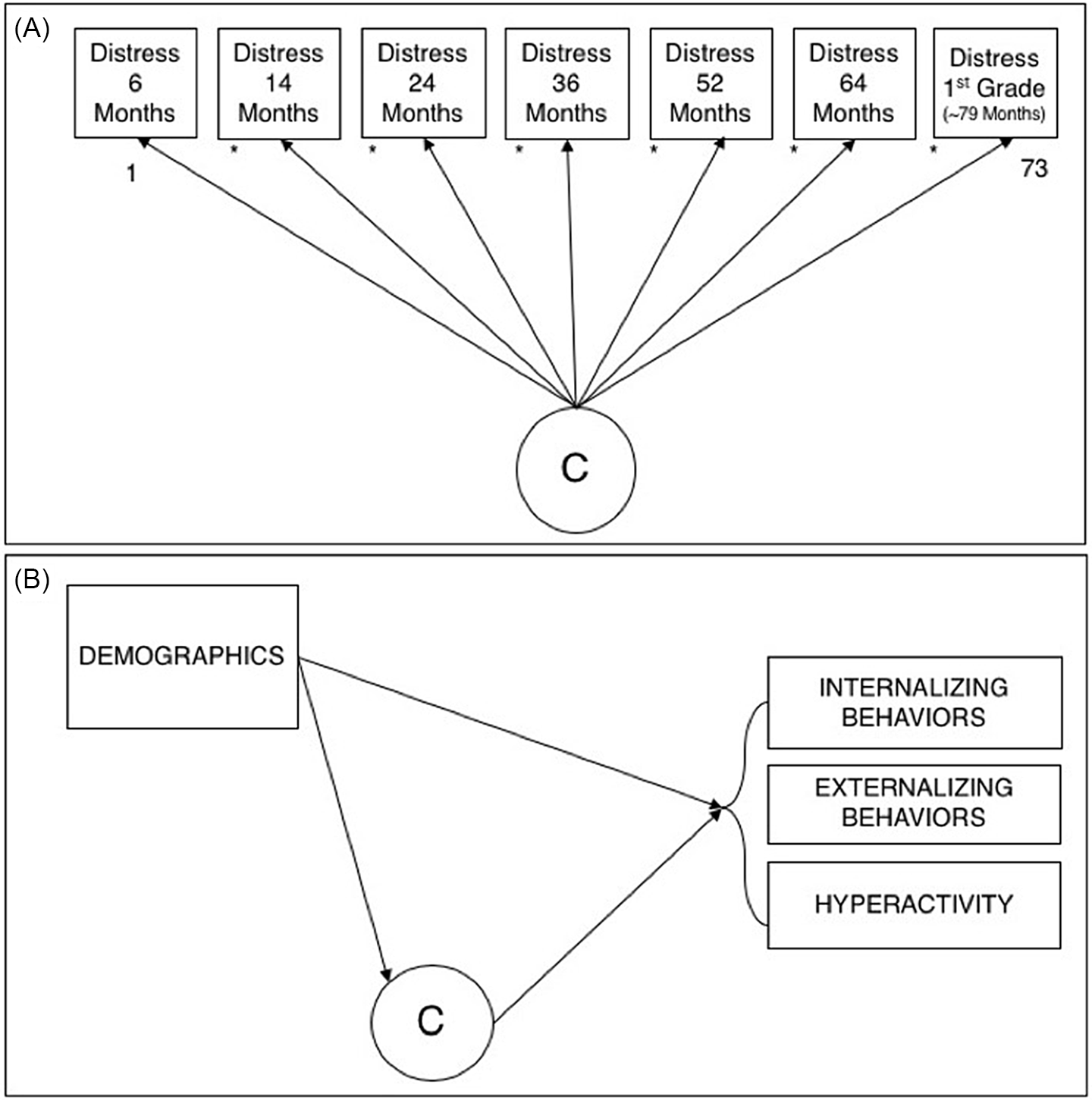
Figure 1. Path diagrams of the fitted (A) growth mixture model and (B) between-class model. Both panels were estimated simultaneously. The random intercept of internalizing distress scores across time points (i.e., 6 months to 1st grade) is taken to create specific latent profiles or classes (I) in Path Diagram A. Demographic covariates (i.e., maternal age, ethnicity, education, income, marital status, and cohabitational status) and mother’s distress class (C) are treated as predictors to child adjustment outcomes (i.e., internalizing behaviors, externalizing behaviors, and hyperactivity) in Path Diagram B. Demographic covariates were also treated as predictors of mother’s internalizing distress class (C).
To test our second research aim as to whether internalizing distress classes among mothers would be associated with child adjustment outcomes (see Figure 1B), we estimated a structural equation model as an extension of the GMM described above, with comparisons across the outcome associations tested using equality constraints and associated Wald tests. Demographic variables (ethnicity dummy code 1 and ethnicity dummy code 2 [African American as the reference group], age, marital status [single mothers as the reference group], cohabitation status [not living with child’s father as the reference group], income, and education dummy code 1 and education dummy code 2 [less than a high school education as the reference group]) at baseline were also included in the analyses as covariates. All continuous demographic variables were mean-centered. All analyses were performed using Mplus v8.3 (Muthén & Muthén, Reference Muthén and Muthén1998-2019).
Results
Zero-order correlations between all variables can be found in Table 2.
Table 2. Zero-order correlations

† p < 0.10, *p < 0.05, **p < 0.01. ***p < 0.001.
Note. Demographic variables were collected as covariates from participants at baseline following childbirth. Participants were asked to report their ethnicity, age, marital and cohabitational status, and socioeconomic status (i.e., household income and education). Ethnicity was dummy coded into two variables with African Americans (0) as the reference group (1 = Dominican immigrant in one dummy code variable, 1 = Mexican immigrant in another dummy code variable). Age and household income were mean-centered. Marital and cohabitational status with the focus child’s biological father were dichotomous variables (e.g., 0 = No or 1 = Yes). Participant’s education was dummy coded into two variables with having no high school diploma/GED (0) as the reference group (1 = high school diploma/GED only in one dummy code variable, 1 = some education beyond high school in another dummy code variable.
Trajectories of mothers’ internalizing distress
Our first aim was to identify trajectories of mothers’ internalizing distress. Preliminary analysis fit a GMM that included a fixed intercept and linear slope to identify classes. This analysis suggested two distinct classes; however, both classes were estimated to have essentially zero (and nonsignificant) linear slopes, with corresponding flat trajectories of internalizing distress from 6 months postpartum to when children were in first grade. However, there was significant variability in the slope of the class with the lower overall internalizing distress mean. We subsequently fit a free curve for the slope to estimate nonlinear trajectories (Wood et al., Reference Wood, Steinley and Jackson2015), which also provided near-zero slope estimates, did not improve fit, and did not increase substantive interpretability. The resulting final model included an intercept only, with all loadings freely estimated in determining class membership for model parsimony and convergence (Curran et al., Reference Curran, Obeidat and Losardo2010). This final GMM revealed two distinct trajectory classes that classified mothers’ trajectories of internalizing distress, which we refer to as low stable (i.e., Class 1) or moderate, late decline (i.e., Class 2). These labels were generated based on the free-curve intercept differences that were particularly pronounced and statistically significantly different from the other cross-class intercept comparisons at the 64- and 79-month measurements – Range β Diff12, 64/79-6/14/24/36/52 = 0.059 – 0.079, ps < 0.05. Figure 2 plots the predicted trajectories of these two classes that were empirically derived from the data. See Table 3 for descriptive statistics and Table S3 for loadings. This 2-class solution was compared, in terms of model fit and substantive parsimony in accounting for observed associations, to parallel 1- and 3-class models (model comparisons – 1 class vs. 2 classes: VLMR LRT = −1831.21, p = 0.425, LMR Adjusted LRT = 94.44, p = 0.430, parametric bootstrapped LRT = −1831.21, p < 0.001; 2 classes vs. 3 classes: VLMR LRT = −1783.57, p = 0.520, LMR Adjusted LRT = 74.57, p = 0.524, parametric bootstrapped LRT = −1783.57, p = 0.040; fit indices – 1 class: AIC = 3735.58, BIC = 3924.70; 2 classes: entropy = 0.69, AIC = 3691.14, BIC = 3912.38; 3 classes: entropy = 0.74, AIC = 3655.90, BIC = 3948.51). These different fit indices regarding the optimal number of classes were not always in agreement. Ultimately, we opted for a two-class solution in the interest of parsimony. Some of these indices indicated that a three-class solution was preferred, however, the third class was very small (n < 10), which is consistent with population estimates of severely distressed mothers. Though higher in distress than the moderate, late decline class, the class of severely distressed mothers versus the class of moderate, late decline mothers were statistically indistinguishable. Inferences with respect to the third class (severely distressed mothers) would be severely underpowered. Further, descriptively, the third class’s (severely distressed mothers) primary difference from the moderate, late decline class was mean levels of distress, not trajectory or associations with the outcomes.

Figure 2. Mothers’ internalizing distress trajectories for moderate, late decline and low stable classes across the six-year timeframe.
Table 3. Descriptive statistics of maternal internalizing distress and child outcomes

a Significant between-group differences among child outcomes.
Note. Possible ranges of variables: Internalizing Distress (1 to 5), Internalizing Behaviors (0 to 30), Externalizing Behaviors (0 to 36), and Hyperactive Behaviors (0 to 36). Mean levels of each child adjustment outcome are significantly different between the low stable and moderate, late decline classes for mother’s internalizing distress.
Thus, under the two-class solution, a total of 82.4% of mothers were classified into the low stable distress group. Mothers in this class on average had a distress intercept of M = 1.59, SE = 0.07 (on a scale from 1 to 5 – between “none” to “a little of the time”) when their infants were 6 months old. Means were consistently low with very little change across all other time points. Further, the variability in the intercepts for this class remained consistently low, σ2 = 0.06, SE = 0.02, throughout the six-year trajectory.
Next, a total of 17.6% of mothers were classified into the moderate, late decline distress group. Mothers in this class on average had a distress intercept of M = 2.63, SE = 0.17 (on a scale from 1 to 5 – between “a little of the time” to “some of the time”) when their infants were 6 months old. The trajectory was generally flat from when children were 6 months old to 52 months old. Interestingly, this group showed a decline in internalizing distress when children were 64 months old (M = 2.20) and in first grade (M = 2.15). Moreover, the moderate, late decline class demonstrated more variability than the low stable class, as mothers’ distress symptoms fluctuated across time points considerably more, σ2 = 0.28, SE = 0.06.
Child adjustment outcomes
Consistent with our hypothesis, children whose mothers were in the moderate, late decline distress class were more likely to exhibit internalizing behaviors (M = 11.12, SE = 0.90; Wald = 5.99, p = 0.014), externalizing behaviors (M = 4.53, SE = .60; Wald = 4.60, p = 0.032), and hyperactivity behaviors (M = 5.74, SE = 0.80; Wald = 4.87, p = 0.027) in first grade compared to children whose mothers were in the low stable distress class (M Internalizing = 9.08, SE = .57; M Externalizing = 3.32, SE = 0.37; M Hyperactivity = 3.88, SE = 0.43) (see Figure 3).

Figure 3. Child adjustment outcomes (i.e., internalizing behaviors, externalizing behaviors, and hyperactivity) for mothers within the moderate, late decline and low stable classes of internalizing distress. Children whose mothers were in the moderate, late decline class had more problematic adjustment outcomes compared to children whose mothers were in the low stable class. Each difference was statistically significant within outcome type (p = 0.014, p = 0.032, p = 0.027 from left to right).
None of the demographic covariates (ethnicity, cohabitation status, marital status, household income, maternal education) included predicted any of the child outcomes, with one exception (see Table S2 for demographic coefficients). Maternal age was positively associated with greater hyperactivity behaviors among children, β = 0.18 (0.09), p = 0.048.
Discussion
The current study explored the trajectories of internalizing distress over the course of six years among ethnic minoritized mothers and examined the consequences of distinctive patterns on child adjustment outcomes. Findings revealed two distinct trajectories, or patterns, of mothers’ internalizing distress, low stable (82.4%) and moderate, late decline (17.6%). These trajectories are somewhat consistent with a previous U.S. national longitudinal study that found low stable (45.6%) and moderate stable (36.4%) distress to be the two largest trajectory groups among a large sample of mothers (approximately three-quarters non-Hispanic White, and one quarter ethnic minoritized) from birth to when their children were 7 years old (Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007). Similarly, Park and colleagues (2018) found that the low stable trajectory was the largest group (71.4%) from the prenatal period to 3 years postpartum (no ethnicity data explicitly reported) compared to increasing (18.3%) or moderate (10.2%) trajectories of internalizing distress symptoms. This suggests that most mothers in our sample generally experienced few distress symptoms.
Speculations as to why we only found two major patterns instead of 3 or 5, as found previously (Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Park et al., Reference Park, Brain, Grunau, Diamond and Oberlander2018) could be that the current study’s sample size (N = 272) was too small to extract additional sufficiently distinct subgroups. Thus, less variability in mothers’ individual distress trajectories may have restricted the number of subgroups or classes of trajectories found. Another possible explanation could be the time frame used to measure maternal distress. Perhaps, greater variability in distress fluctuations may be more apparent prior to childbirth (e.g., during pregnancy) when stress hormones or cortisol patterns are more susceptible to alterations. Previous literature suggests cortisol levels and perceptions of stress tend to be higher during pregnancy, but typically decrease immediately following childbirth. Mothers whose cortisol levels do not drop or remain flat following childbirth are at greater risk for postpartum internalizing symptoms (Scheyer & Urizar, Reference Scheyer and Urizar2016). Examining internalizing distress trajectories during pregnancy when cortisol patterns tend to fluctuate most may have demonstrated more individual variability and thus paved way for more distinct trajectory subgroups or classes. In addition, the two previously mentioned studies (Campbell et al., Reference Campbell, Matestic, von Stauffenberg, Mohan and Kirchner2007; Park et al., Reference Park, Brain, Grunau, Diamond and Oberlander2018) examined depressive symptoms with different samples, whereas our study looked at a more generalized form of internalizing distress specifically among Latina immigrant and African American mothers. Nonetheless, our findings align with previous studies that suggest that mothers with chronic elevated symptoms, such as those in the moderate, late decline class, are at greater risk for adverse child outcomes (Prochaska et al., Reference Prochaska, Sung, Max, Shi and Ong2012).
It is also important to note that while mothers’ average distress scores were relatively low across all six years, some mothers reported experiencing moderate to severe distress at least once during the six-year postpartum period. For instance, 39.3% of the current sample met the cut off criterion for moderate distress (i.e., sum of scores ranging from 13 to 20; Valdez & Langellier, Reference Valdez and Langellier2015) and 5.1% met the criteria for severe mental distress indicative of a diagnosable mental disorder (i.e., sum of scores ranging from 21 to 30) in at least one wave across all seven waves. These instances are not mutually exclusive, and it is likely that some mothers may have experienced severe distress at one point and moderate distress at another. Our findings are consistent with past work that have found higher prevalence of postpartum distress among immigrant mothers (20%; Dennis et al., Reference Dennis, Brown, Wanigaratne, Fung, Vigod, Grigoriadis, Marini and Brennenstuhl2018; O’Hara & Swain, Reference O’Hara and Swain1996) and Latina American and African American mothers (30-60%; Anokye et al., Reference Anokye, Acheampong, Budu-Ainooson, Obeng and Akwasi2018; Beeber et al., Reference Beeber, Schwartz, Martinez, Holditch, Bledsoe, Canuso and Lewis2014; Breslau et al., Reference Breslau, Aguilar-Gaxiola, Kendler, Su, William and Kessler2006; McGuire & Miranda, Reference McGuire and Miranda2008). It is likely that in addition to the stresses of motherhood, mothers within marginalized communities are exposed to a disproportionate number of stressors and barriers (i.e., racial/ethnic discrimination, an anti-immigrant climate, acculturative stress) that native-born or non-Hispanic White mothers may not otherwise experience (Beeber et al., Reference Beeber, Schwartz, Martinez, Holditch, Bledsoe, Canuso and Lewis2014; Halim et al., Reference Halim, Moy and Yoshikawa2015; Harris & Santos, Reference Harris and Santos2020; Valdez et al., Reference Valdez, Raines, Davies and D’Costa2018). Our findings add to existing research that suggests mothers of ethnic minority background or immigrant status are more vulnerable to mental disorders, highlighting the need to address these disparities.
Children’s adjustment outcomes
Despite the lower levels of distress, our findings suggest that even chronic moderate internalizing distress over the course of six years can have negative implications for children of ethnic minoritized mothers. We found significant associations of maternal internalizing distress with all three child adjustment outcomes (i.e., internalizing behaviors, externalizing behaviors, and hyperactivity), which suggests that mothers’ well-being plays a significant role in their child’s psychological adjustment. Children whose mothers reported more elevated symptoms of internalizing distress within the moderate, late decline class, were rated as having more problematic adjustment outcomes (internalizing behaviors, externalizing behaviors, and hyperactivity) compared to children whose mothers reported low and stable levels of distress across the six-year course.
Limitations and future directions
Several limitations within the current study should be considered. This study relied solely on maternal self-report measures, whereas a variety of assessment methods would further confirm and triangulate findings. For instance, it is possible that mothers may have underreported their distress symptoms for fear of stigmatization or negative evaluations of their maternal competence (Abrams & Curran, Reference Abrams and Curran2011). Additionally, the K6 measure assessed internalizing distress symptoms within the last month and was assessed once annually. Given that symptoms can be episodic, it is plausible that our assessments did not capture episodes experienced prior to the 30 days from the assessment date. In addition, to be inclusive of mothers with varying degrees of literacy, researchers verbally interviewed all mothers in one-on-one sessions. This method might have heightened some social desirability concerns. Despite this possible limitation, it appears there was significant signal-to-noise in that hypothesized patterns were confirmed. It is also plausible that mothers with elevated levels of distress may perceive their child as more problematic than mothers with lower levels of distress and thereby influence biased ratings of child outcomes (Luoma et al., Reference Luoma, Tamminen, Kaukonen, Laippala, Puura, Salmelin and Almqvist2001). Although previous studies have supported the validity of using maternal ratings to assess child behavior and have been found to be accurate appraisals of child’s functioning (Conrad & Hammen, Reference Conrad and Hammen1989), future work would benefit from multi-informant assessments that include child and teacher reports.
Methodologically, while our sample was comparatively large for studies of this type, we note that it is smaller than conventional cutoffs would indicate for latent class stability or reproducibility. Indeed, as noted in the results section, different fit indices regarding the optimal number of classes were not always in agreement, but we ultimately opted for the two-class solution for the sake of parsimony. Future research would require larger samples or strong a priori theory to distinguish severely distressed mothers from moderately distressed (late decline) mothers, but such studies could provide resolution with respect to distress severity and its differential effect on child outcomes.
Finally, although we sampled Latina immigrant and African American mothers who are underrepresented in this area of research, we acknowledge that it is important for future work to test these same links among other immigrant and ethnic minoritized groups for whom postpartum depression and maternal internalizing distress can be especially prevalent (e.g., Nilaweera et al., Reference Nilaweera, Doran and Fisher2014; Vo & Desai, Reference Vo and Desai2021).
Conclusion
Traditional approaches for examining the association between mothers’ internalizing distress and child adjustment outcomes typically focus on symptom severity at specific time points without considering the impact of the chronicity or trajectory of distress (Park et al., Reference Park, Brain, Grunau, Diamond and Oberlander2018). We addressed this existing gap in the literature by examining the trajectories of mothers’ internalizing distress over a six-year timeframe. We found that among two distinct distress trajectories, children whose mothers’ experienced chronic elevated symptoms had poorer adjustment outcomes in the first grade. Furthermore, while previous studies have examined the comparative differences of psychopathology between non-Hispanic White and ethnic minoritized groups, the current study focused on the trajectory of internalizing distress specifically among ethnic minoritized and immigrant mothers. This study highlights the necessity of supportive and preventative mental health services for marginalized populations that are often underrepresented in research and underserved in mental health care, especially during critical periods (i.e., pregnancy and postpartum screenings; Kozhimannil et al., Reference Kozhimannil, Trinacty, Busch, Huskamp and Adams2011; McGuire & Miranda, Reference McGuire and Miranda2008). Elucidating the influences of internalizing distress can contribute to the development and implementation of interventions to increase detection and treatment that would help improve mothers’ well-being and reduce family psychopathology.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0954579422001031
Acknowledgment
This data was collected by the New York University Center for Research on Culture, Development, and Education. This research was funded by grants from the NSF (BCS 021859; IRADS 0721383) to Dr Catherine Tamis-LeMonda and Dr Hirokazu Yoshikawa. This research was also supported by a grant from the NIH (NIH R01AA027264) to Dr Sean Lane.
Conflict of Interest
None.









