Introduction
Adolescents and adults in the United States are exposed to high rates of gun violence (Finkelhor et al., Reference Finkelhor, Turner, Shattuck and Hamby2015; Parker et al., Reference Parker, Horowitz, Igielnik, Oliphant and Brown2017). The goal of the current paper was to use a quasi-experimental approach – comparing siblings who were differentially exposed to gun violence – to test whether exposure to gun violence has long-term consequences for the mental health of those who witness or experience it.
Much of the national conversation about gun violence tends to focus on mass shootings, which are unquestionably tragic events, but account for approximately 1% of violence in the United States (Rozel & Mulvey, Reference Rozel and Mulvey2017). In contrast, the gun violence experienced in many American cities is a daily event (Gun Violence Archive, 2021) and disproportionately affects communities of color (Sanchez et al., Reference Sanchez, Jaguan, Shaikh, McKenney and Elkbuli2020). Individuals who experience the loss of someone they know to gun violence report elevated rates of PTSD and major depressive disorder (McDevitt-Murphy et al., Reference McDevitt-Murphy, Neimeyer, Burke, Williams and Lawson2011; Rheingold & Williams, Reference Rheingold and Williams2015; Smith et al., Reference Smith, Sharpe, Richardson, Pahwa, Smith and DeVylder2020). Those who are victims of nonfatal gun violence are also at risk for mental health problems, most prominently PTSD (Breslau et al., Reference Breslau, Kessler, Chilcoat, Schultz, Davis and Andreski1998; Vella et al., Reference Vella, Warshauer, Tortorello, Fernandez-Moure, Giacolone, Chen, Cabulong, Chreiman, Sims, Schwab, Reilly, Lane-Fall and Seamon2020), symptoms of which have been shown to worsen in the months following a shooting (Greenspan & Kellermann, Reference Greenspan and Kellermann2002).
Recent studies have strengthened causal claims about exposure to community violence and mental illness by employing a variety of quasi-experimental designs. These include comparisons of children living in the same neighborhoods who have been differentially exposed to violence (Cuartas & Leventhal, Reference Cuartas and Leventhal2020; Vasan et al., Reference Vasan, Mitchell, Fein, Buckler, Wiebe and South2021). For example, among 7- to 11-year-old children living in the same neighborhoods in Bogotá, Colombia, those who lived closer to the location of a violent crime reported more symptoms of emotional and behavioral problems in the subsequent year compared with children from the same neighborhoods who lived farther away (Cuartas & Leventhal, Reference Cuartas and Leventhal2020). In a sample of children and adolescents presenting to a pediatric emergency department in a large, urban center, those who lived within two to three blocks of a shooting were more likely to have a mental health-related presentation up to 60 days following the shooting compared with youth from the same two to three block radius who presented in the 60 days prior to the shooting (Vasan et al., Reference Vasan, Mitchell, Fein, Buckler, Wiebe and South2021). Other studies compare children’s functioning on days when they were (versus were not) exposed to violence (Deane et al., Reference Deane, Richards and Santiago2021; Heissel et al., Reference Heissel, Sharkey, Torrats-Espinosa, Grant and Adam2018; Sharkey et al., Reference Sharkey, Tirado-Strayer, Papachristos and Raver2012). For example, Deane et al. (Reference Deane, Richards and Santiago2021) gathered information about adolescents’ exposure to community violence during a one-week experience sampling study. They found that on days adolescents reported exposure to violence (compared with days they were not exposed), they also reported more symptoms of post-traumatic stress and dysphoria that same day and more symptoms of post-traumatic stress and hostility the following day. Similarly, in a 4-day diary study, Heissel et al. (Reference Heissel, Sharkey, Torrats-Espinosa, Grant and Adam2018) found that children had disrupted waking cortisol the morning after a violent crime in their neighborhoods compared with the morning after no such crimes occurred and Sharkey et al. (Reference Sharkey, Tirado-Strayer, Papachristos and Raver2012) reported that preschoolers had significantly lower attention, impulse control, and standardized vocabulary test scores if they were tested within 7 days of a homicide occurring within 1500 feet of their home compared with a different testing occasion when there had been no homicides in the prior week.
The current study adds to this literature by rigorously testing the causal relationship between cumulative exposure to gun or knife violence from adolescence to adulthood and depression in young adulthood using a sibling fixed effects model. Using data from a nationally representative, longitudinal study, we compare full siblings, some of whom are discordant for their exposure to gun or knife violence, to determine whether the sibling who is more exposed to gun or knife violence reports more symptoms of depression as an adult. Like the analytic approaches described above, the sibling fixed effects method, by design, eliminates a number of sources of unobserved heterogeneity. Siblings growing up in the same families share neighborhoods, family circumstances, and they are more genetically similar than individuals selected at random. To the extent that siblings differ and these differences might explain any observed association between their exposure to gun or knife violence and their symptoms of depression, these factors can be included as measured variables in sibling fixed effects models. All quasi-experimental designs have different strengths and weaknesses; convergence across a range of designs increases confidence in causal inference.
The current study also extends the existing literature. Current studies are based on samples from specific cities and they follow respondents (who are children and adolescents) for, at most, a year after their exposure to violence (Cuartas & Leventhal, Reference Cuartas and Leventhal2020; Deane et al., Reference Deane, Richards and Santiago2021; Heissel et al., Reference Heissel, Sharkey, Torrats-Espinosa, Grant and Adam2018; Sharkey et al., Reference Sharkey, Tirado-Strayer, Papachristos and Raver2012; Vasan et al., Reference Vasan, Mitchell, Fein, Buckler, Wiebe and South2021). In contrast, the current study involves individuals from a nationally representative sample in the United States. This study identifies their cumulative exposure to gun or knife violence, starting in adolescence and extending into adulthood, and estimates the effect of this cumulative exposure on depression in adulthood. Finally, the size of the sample allows us to test whether there are racial or ethnic differences in exposure to gun or knife violence or in the impact of gun or knife violence on depression symptoms. Black and Hispanic adolescents and adults are exposed to higher rates of many forms of violence – including gun violence fatalities – compared with non-Hispanic Whites (Sheats et al., Reference Sheats, Irving, Mercy, Simon, Crosby, Ford, Merrick, Annor and Morgan2018; Smith et al., Reference Smith, Sharpe, Richardson, Pahwa, Smith and DeVylder2020). In a study of adults from four urban communities in the United States, exposure to gun violence was more strongly associated with Hispanic adults’ symptoms of depression and psychological distress than it was with Black or White respondents’ symptoms (Smith et al., Reference Smith, Sharpe, Richardson, Pahwa, Smith and DeVylder2020).
Given the current literature, we hypothesize (1) in the sample overall, adjusting for demographic and individual-level covariates (including exposure to other forms of violence), more cumulative exposure to gun or knife violence from adolescence to adulthood will be associated with more symptoms of depression in adulthood and greater risk for meeting the criterion for clinically significant levels of depression in adulthood; (2) in sibling fixed effects analyses, the sibling who has been exposed to more gun or knife violence will also have more symptoms of depression in adulthood; and (3) Black and Hispanic respondents will, cumulatively, be exposed to more gun or knife violence than white respondents. We will test whether the strength of the association between cumulative exposure to gun or knife violence and depression varies as a function of race/ethnicity, but given the paucity of studies to inform a directional hypothesis, this test is exploratory.
Method
Sample
Respondents are members of the National Longitudinal Study of Adolescent to Adult Health (Add Health). Add Health is a school-based, longitudinal study of a nationally representative sample of adolescents who were in grades 7 to 12 in 1994–95 at Wave 1 (mean age = 15.97, SD = 1.80). At Wave 1, data were collected from 90,118 students, sampled from 145 middle and high schools using a stratified, random school selection procedure. Of the students who completed questionnaires in schools, 20,745 students and 17,670 of their parents also completed in-home interviews in 1995. Add Health respondents were followed up in 1995–1996 (Wave 2; n = 14,738), 2001–2002 (Wave 3; n = 15,197) and 2007–2008 (Wave 4; n = 15,701) by which time participants ranged in age from 24 to 32 years. Add Health study procedures were approved by the Human Subjects Review Committee of the University of North Carolina at Chapel Hill and analyses were exempted from review by the University of Pennsylvania’s IRB.
Measures
Exposure to gun or knife violence
At Waves 1 through 4, participants reported whether they saw a shooting or stabbing, someone pulled a knife or gun on them, or someone shot or stabbed them in the past 12 months. We summed exposures from Waves 1 through 4.
Physical assault
At Waves 1 and 2, participants reported whether they were “jumped”; at waves 3 and 4, participants reported whether they were beaten up in the past 12 months. We summed exposures from Waves 1 through 4.
Intimate partner violence
At Waves 2 through 4, respondents identified intimate partners (numbers varied across waves) and reported if partners engaged in any of four (Wave 4) or five (Waves 2 and 3) abusive behaviors in the past 12 months (e.g., threatened you in public, shoved you, threw something at you, slapped, kick, or hit you). For each item at each wave, respondents received a score of 1 if any partner engaged in the behavior and a score of 0 if no partners engaged in the behavior. We summed the intimate partner violence scores from Waves 2 through 4.
Depression symptoms were measured with the Centers for Epidemiological Studies of Depression Survey, which asks about symptoms of depression in the past week. At Wave 1, 18 (of the original 20) items were administered (items for crying spells and restless sleep were not included; α = 0.87). The 10 item version of the CESD was administered at Wave 4 (α = 0.84). A score of 11 or higher is indicative of clinically-significant levels of depression on the 10-item measure (see https://scireproject.com/outcome-measures/outcome-measure-tool/center-for-epidemiological-studies-depression-scale-ces-d-and-ces-d-10/#1467983894080-2c29ca8d-88af for additional details). Nineteen percent of respondents exceeded the clinical threshold for depression at Wave 4.
Statistical analysis
Descriptive statistics for the full sample are presented in Table 1. We conducted ordinary least squares and logistic regression analyses, respectively, to test whether the number of gun or knife violence exposures over 14 years was associated with depression symptom scores and clinically significant levels of depression at Wave 4. Covariates included age, sex, race/ethnicity, Wave 1 income (logged), exposure to intimate partner violence and physical assault, and Wave 1 depression symptom scores. We conducted these analyses for the sample overall and for Black, Hispanic, and White sub-groups. We used fixed effect regression analyses in the sibling sub-sample to test whether there was a within-families effect of exposure to gun or knife violence on symptoms of depression in young adulthood (Petersen & Lange, Reference Petersen and Lange2020). The sibling sub-sample included full, same-sex siblings (1,318 nontwin full siblings, 564 dizygotic twins, and 564 monozygotic twins) from 1,223 families. Covariates included age, exposure to intimate partner violence or physical assault, and Wave 1 depression symptoms scores. As per study design, many siblings did not have sample weights, so we did not restrict the sibling sub-sample to individuals with valid sample weights, as has been the convention in other sibling comparison studies in Add Health (Bauldry et al., Reference Bauldry, Shanahan, Russo, Roberts and Damian2016; Jaffee et al., Reference Jaffee, Lombardi and Coley2013).
Table 1. Descriptive statistics, full sample
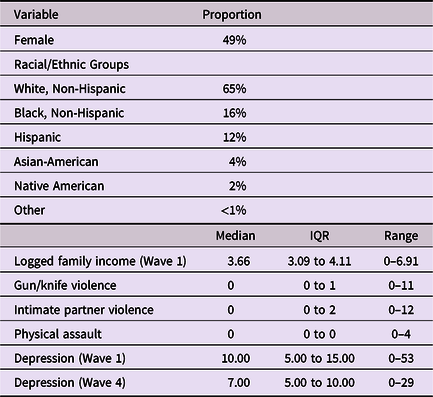
Note: IQR = interquartile range.
Missing data
Data were missing for 0 to 28% (Wave 4 depression scores) of the 20,774 respondents who participated across waves of the study, with only 54% of respondents having complete data. We used the Stata 17.0 (StataCorp, 2021) mvn procedure to impute 10 data sets – a number deemed sufficient given that the highest Fraction of Missing Information (proportion of total sampling variance due to missing data) was 10%. The mvn procedure uses Markov Chain Monte Carlo procedures to impute variables using a multivariate normal distribution. Simulation studies have shown that, given a sufficient sample size, assuming a multivariate normal distribution leads to reliable estimates even when the normality assumption is violated (Demirtas et al., Reference Demirtas, Freels and Yucel2008; Lee & Carlin, Reference Lee and Carlin2010). Analyses were conducted within the imputed data sets and combined using svy: mi to adjust for the multistage sampling design and nonresponse. This resulted in a total sample size of 14,800, reflecting missingness on the Wave 4 sampling weight variable, which we did not impute.
Results
Prevalence of exposure to gun or knife violence
Thirty-two percent of respondents reported at least one exposure to gun or knife violence over the 15 years of the study (Table 2). Exposure to gun or knife violence was positively associated with reports of intimate partner violence (b = 0.13, 95% C. I. = 0.11 to .15) and physical assault (b = 1.26, 95% C. I. = 1.17 to 1.35). Black and Hispanic respondents reported significantly more exposure to violence than White respondents. Sixty-five percent of those who reported any exposure were exposed in one wave, with 9–11% of Black and Hispanic respondents exposed in three or four waves compared with 7% of White respondents.
Table 2. Prevalence of exposure to gun or knife violence and other forms of violence
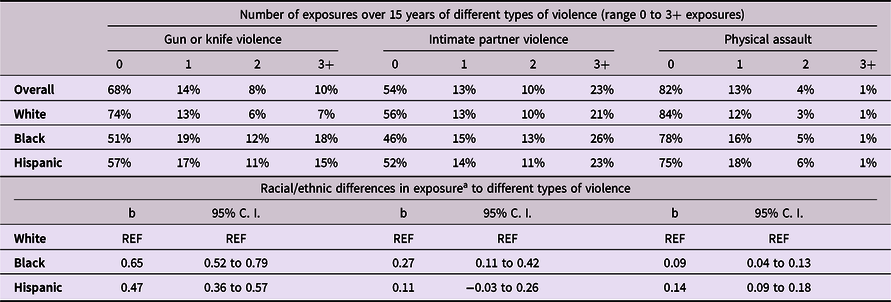
Note: number of exposures (0 to 3+) differs from number of study waves in which respondents reported exposures (0 to 4);
a based on full range of exposures.
Is there an association between exposure to gun or knife violence and depression?
Exposure to gun or knife violence over 14 years, starting in adolescence, was associated with symptoms of depression in adulthood (at Wave 4; Table 3). In fully adjusted models, the effect of exposure to gun or knife violence remained significant and the risk of clinically significant levels of depression increased by 7%.
Table 3. Effects of exposure to gun or knife violence over 15 years on depression in young adulthood (wave 4), weighted to population estimates
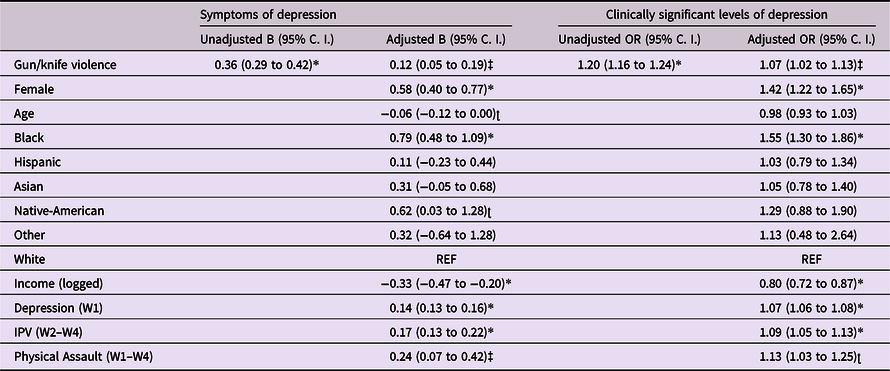
*p < .001; ‡ p < .01; ʈ p < .05; IPV = Intimate Partner Violence.
Although the association between gun or knife violence exposure and depression was only significant for the Hispanic subgroup in fully adjusted models (Table 4), a formal test of the interaction between race/ethnicity and exposure to gun or knife violence was statistically non-significant (F [2, 127] = 0.23, p = 0.80), indicating that the magnitude of the coefficient for exposure to gun or knife violence did not differ across White, Black, and Hispanic groups.
Table 4. Effects of exposure to gun or knife violence on depression over 15 years in young adulthood in Black, Hispanic, and White sub-groups (weighted to population estimates)
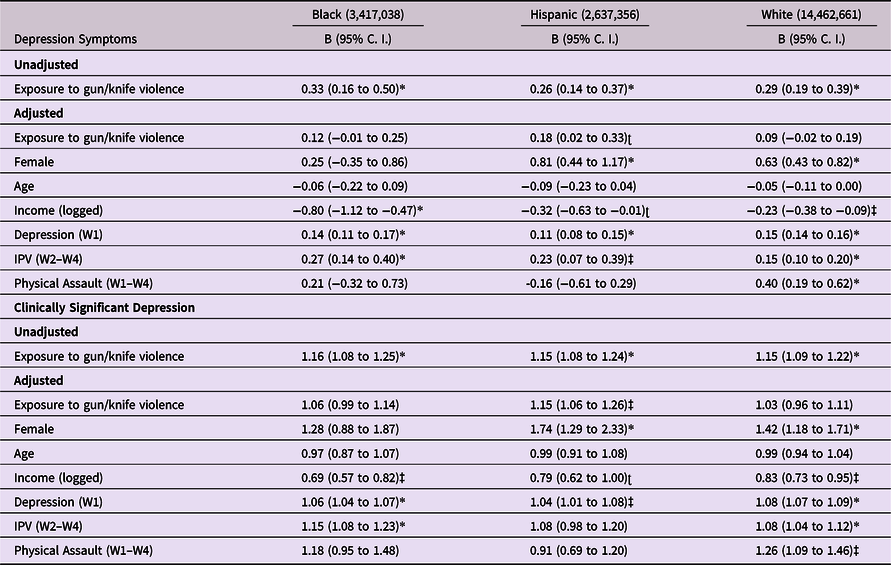
*p < 0.001; ‡ p < 0.01; ʈ p < 0.05; IPV = Intimate Partner Violence.
Is there a within-families association between exposure to gun or knife violence and risk for depression?
Twenty-two percent of sibling pairs (n = 271 pairs) differed by one gun or knife violence exposure and an additional 21% (n = 257 pairs) differed by two or more exposures. As shown in Table 5, within families, the sibling who reported more gun or knife violence exposures also reported more symptoms of depression in young adulthood, even adjusting for sibling differences in age, depression at Wave 1, and other violence exposures. In adjusted models, a difference of one exposure was associated with an increase of roughly one-fifth of a point on the depression scale. The study was not powered to test whether sibling differences in exposure to violence were associated with sibling differences in clinically significant levels of depression.
Table 5. Fixed effects regression estimating within-families effect of exposure to gun or knife violence on depression in young adulthood
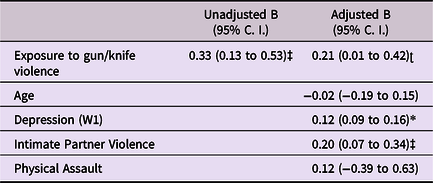
*p < .001; ‡ p < .01; ʈ p < 0.05.
Discussion
In this nationally representative sample of young adults in the United States, exposure to gun or knife violence was common, with nearly double the number of Hispanic (43%) and Black respondents (49%) reporting at least one exposure compared with Whites (26%).
Individuals who were exposed to gun or knife violence reported more symptoms of depression and greater risk for clinically significant levels of depression in young adulthood with each additional exposure increasing the risk of clinically significant depression by 7% in fully adjusted models. Among differentially exposed siblings, the more violence-exposed sibling reported more symptoms of depression. This sibling comparison increases confidence that the results are not due to differences in socioeconomic conditions or other family-specific characteristics. These findings are consistent with a small number of studies that have used quasi-experimental methods to strengthen causal inference about the relationship between children’s exposure to violence in the community and academic and health outcomes (Cuartas & Leventhal, Reference Cuartas and Leventhal2020; Deane et al., Reference Deane, Richards and Santiago2021; Heissel et al., Reference Heissel, Sharkey, Torrats-Espinosa, Grant and Adam2018; Sharkey et al., Reference Sharkey, Tirado-Strayer, Papachristos and Raver2012; Vasan et al., Reference Vasan, Mitchell, Fein, Buckler, Wiebe and South2021) and adds to the evidence that gun violence is a cause of mental health problems rather than the reverse (Rozel & Mulvey, Reference Rozel and Mulvey2017).
The current study extends the findings from these quasi-experimental studies in at least two ways. First, whereas existing studies estimated the effect of exposure to violence over relatively short periods – anywhere from five days to one year – the current study estimated the impact of exposure to violence over two decades, extending from adolescence into young adulthood. We found that repeated exposure to gun or knife violence as a victim or witness was common among those who had any exposure; approximately a third of exposed respondents reported being exposed in at least two waves and 10% reported exposure in three or four waves. Second, compared to White respondents, Black and Hispanic respondents reported higher levels of and more repeated exposure to gun violence over the two decades of the study, but there was only weak evidence that the strength or direction of the association between exposure to gun violence and depression was modified by race or ethnicity. This is consistent with Smith et al. (Reference Smith, Sharpe, Richardson, Pahwa, Smith and DeVylder2020) who tested whether the association between exposure to gun violence fatalities and mental health varied among White, Black, and Hispanic respondents. They reported that although Black and Hispanic respondents were exposed to substantially more gun violence fatalities than White respondents, the strength of the association between exposure to gun violence fatalities and psychosis symptoms did not vary across racial/ethnic groups (Smith et al., Reference Smith, Sharpe, Richardson, Pahwa, Smith and DeVylder2020). They did, however, find that exposure to gun violence fatalities was more strongly associated with symptoms of depression for Hispanic than for Black or White respondents. We see this same pattern in the analyses we conducted separately by racial/ethnic groups. One possibility is that the strength of the association is greatest in groups with moderate levels of exposure. Associations between exposure to gun violence and depression may be obscured in groups with high levels of exposure (e.g., Black respondents in the current study and Smith et al., Reference Smith, Sharpe, Richardson, Pahwa, Smith and DeVylder2020) where some individuals may have habituated to on-going violence and other individuals may be highly reactive (Ng-Mak et al., Reference Ng-Mak, Salzinger, Feldman and Stueve2004).
Limitations
Sibling fixed effect models automatically hold constant all factors that are similar for siblings growing up in the same family. Sibling differences in depression could, however, have been explained by sibling differences in traits or exposures other than differences in their exposure to gun or knife violence. We found that covariates such as differences in age, depression symptoms in middle- and high-school, or exposure to other forms of violence did not explain observed associations between sibling differences in exposure to gun or knife violence and sibling differences in depression. It is possible that sibling differences in exposure to nonviolent crime might explain differences in sibling differences in depression, but nonviolent crime victimization was not assessed in Add Health, with the exception of a single item at Wave 4. Results of sibling fixed effect models are most applicable to sibling-discordant families and siblings may differ in systematic ways from singletons (Petersen & Lange, Reference Petersen and Lange2020), although there is no evidence in Add Health that these groups differ in levels of depression or gun or knife violence exposure.
We note that the perpetrators and victims of violent crimes are often the same (e.g., Berg & Schreck, Reference Berg and Schreck2022). It is possible, then, that gun or knife violence perpetration (rather than victimization) is responsible for the pattern of results reported here. Gun or knife violence perpetration (including threatening someone with a knife or gun or shooting or stabbing someone), measured at the same times as gun or knife violence victimization, was not, however, significantly associated with depression symptoms in multivariate linear regression models that controlled for other forms of violence victimization (gun or knife violence victimization, physical assault, and intimate partner violence). In contrast, these other forms of victimization were significantly associated with symptoms of depression. Moreover, only 31 sibling pairs were discordant for gun or knife violence perpetration. Thus, although there is certainly victim-offender overlap in our sample, it does not explain our pattern of results.
Respondents were asked about shootings and stabbings together. Although it is possible our findings were driven by reports of stabbings rather than shootings, this seems unlikely given that the overwhelming majority of homicides in the United States involve firearms (Statista, 2021).
Given our nationally representative sample, small effect sizes may still meaningfully inform policies and programs for large populations that reduce severe violence. Because depression is a common mental health problem, even small reductions in severe violence could be expected to affect a large number of people (Rothman et al., Reference Rothman, Greenland and Lash2008).
Public health implications
The current study adds to the evidence that exposure to gun or knife violence can be a cause of depression leading into young adulthood. This can further inform adolescent health screenings and suggest the need for more rigorous symptom surveillance into young adulthood.
Acknowledgments
We are grateful to the Add Health Study for use of the data. Add Health is directed by Robert A. Hummer and funded by the National Institute on Aging cooperative agreements U01 AG071448 (Hummer) and U01 AG071450 (Aiello and Hummer) at the University of North Carolina at Chapel Hill. Waves I-V data are from the Add Health Program Project, grant P01 HD31921 (Harris) from Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Add Health was designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill.
Funding statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interests
None.







