Maternal depressive symptoms (MDS) involve affective symptoms such as depressed mood, feelings of hopelessness, and sleep disturbance. MDS occur at higher rates in mothers living in unsafe environments (Hill & Herman-Stahl, Reference Hill and Herman-Stahl2002). In addition, the stress associated with ethnic minority status and experiences of racism may increase the risk for depression among African American mothers of young children, making this a particularly important population to examine when considering the effects of MDS on child development (Baker et al., Reference Baker, Brooks-Gunn and Gouskova2020; Segre et al., Reference Segre, O'Hara and Losch2006). In fact, samples of mothers with children in Head Start comprised of substantial African American and Latina participants often report mean depressive symptoms at or above the clinical cutoff (Berlin et al., Reference Berlin, Whiteside-Mansell, Roggman, Green, Robinson and Spieker2011; Lanzi et al., Reference Lanzi, Pascoe, Keltner and Ramey1999; Spieker et al., Reference Spieker, Nelson, DeKlyen, Staerkel, Berlin, Ziv, Amaya-Jackson and Greenberg2005). Cummings and Davies (Reference Cummings and Davies1994) suggest that MDS cascade through parental characteristics, parent–child interactions (e.g., negativity, intrusiveness, withdrawal), and marital functioning to shape child characteristics and in turn, child development. Research has found that MDS reduce effective parenting (Albright & Tamis-LeMonda, Reference Albright and Tamis-LeMonda2002) and increase children’s risk for emotional and behavioral problems (Brennan et al., Reference Brennan, Hammen, Andersen, Bor, Najman and Williams2000; Kouros & Garber, Reference Kouros and Garber2010; Lyons-Ruth et al., Reference Lyons-Ruth, Alpern and Repacholi1993, Reference Lyons-Ruth, Easterbrooks and Cibelli1997).
For instance, considerable research indicates positive associations between MDS and child internalizing behavior problems—involving emotional distress and symptoms linked to depression and anxiety—and externalizing behavior problems—involving aggression, hyperactivity, and delinquency (Achenbach & Rescorla, Reference Achenbach and Rescorla2000). For example, a study of low-income families found that mothers’ elevated MDS when children were 1–5 years predicted greater child internalizing and externalizing behavior problems at age 7 (Lyons-Ruth et al., Reference Lyons-Ruth, Easterbrooks and Cibelli1997). Similarly, another study of low-income families found that mothers who reported elevated MDS when their children were 4 years old had children with more internalizing behaviors (i.e., anxious and withdrawn) at age 6, and mothers who reported elevated MDS at when children were both 4 and 6 years of age had children with greater externalizing behavior problems at school and at home at age 6 (Alpern & Lyons-Ruth, Reference Alpern and Lyons-Ruth1993). Additionally, in a study of 224 youth and their mothers, McCarty and McMahon (Reference McCarty and McMahon2003) found that MDS were associated with lower quality parent–child relationships and lower social support, which predicted more child internalizing and externalizing behavior problems across the school years; race did not moderate these links. Finally, in a sample of 184 African American mothers of Head Start children, MDS were positively associated with their preschoolers’ internalizing and externalizing behavior problems (Koblinsky et al., Reference Koblinsky, Kuvalanka and Randolph2006). Together, these studies suggest that relationship factors may play an important role in understanding MDS-related risk for child behavior problems across diverse populations (for related meta-analytic evidence linking maternal depression and child behavior problems see Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011). Further, longitudinal analyses by Baker et al. (Reference Baker, Brooks-Gunn and Gouskova2020) suggest that there may be reciprocal relations between MDS and child behavior problems, particularly among African American families; thus, we consider the possibility of reciprocal effects in the present study.
It is important to examine factors that may protect against child behavior problems in the face of parental risk because such problems in childhood have lasting consequences for adolescent and adult functioning (e.g., Cicchetti & Cohen, Reference Cicchetti and Cohen1995; Masten et al., Reference Masten, Best and Garmezy1990; Reef et al., Reference Reef, Diamantopoulou, van Meurs, Verhulst and van der Ende2011). One important contributor to child mental health that has been shown to protect against external stressors is the quality of the parent–child relationship, and specifically child attachment security. Attachment theory posits that children have a biologically based propensity to seek proximity to caregivers to ensure protection in times of trouble (Bowlby, Reference Bowlby1969/1982, Reference Bowlby1988). In service of this and through repeated interactions with caregivers, children form internal working models of relationships that predictably guide social behavior (Bowlby, Reference Bowlby1969/1982, Reference Bowlby1988; Main et al., Reference Main, Kaplan and Cassidy1985). Attachment security, born out of experiences of sensitive and responsive caregiving, reflects the child’s confidence in the availability of a caregiver to provide a secure base in times of distress. Attachment avoidance (one type of attachment insecurity), on the other hand, results from experiences of rejecting or insensitive caregiving and reflects the child’s hesitancy to seek comfort and difficulty relying on others (Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978).
Theory and research suggest that attachment security may contribute to resilience (Masten, Reference Masten2001; Rutter, Reference Rutter1985) by supporting children’s self-regulation of emotion (Calkins & Leerkes, Reference Calkins, Leerkes, Vohs and Baumeister2011; Cassidy, Reference Cassidy1994) and physiological responses to stress (Cassidy et al., Reference Cassidy, Ehrlich, Sherman, Mikulincer and Shaver2013; Diamond, Reference Diamond, Simpson and Rholes2015); in contrast, forms of insecurity such as avoidance may undermine effective self-regulation and help-seeking, exacerbating psychological risk (Cassidy, Reference Cassidy1994; Kotler et al., Reference Kotler, Buzwell, Romeo and Bowland1994). Meta-analytic evidence links avoidance specifically to increased risk of internalizing symptoms (Groh et al., Reference Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg and Fearon2012). Further, security has been shown to serve as a protective factor in the transmission of mental health risk, meaning that it “ameliorate[s] a person’s response to some environmental hazard that predisposes to a maladaptive outcome” (Rutter, Reference Rutter1985, p. 600). For example, parenting stress has been shown to predict greater child aggression and attention problems at age 3 among children who were insecurely attached as infants, but not among those who were secure (Tharner et al., Reference Tharner, Luijk, Raat, IJzendoorn, Bakermans-Kranenburg, Moll, Jaddoe, Hofman, Verhulst, T and iemeier2012). It is possible that security plays a similar protective role against some of the emotional and behavioral risks associated with MDS.
To our knowledge, previous research on this topic is limited in that no studies have examined child attachment as a moderator of the link between MDS specifically (as opposed to MDS as part of a broader risk composite; Easterbrooks et al., Reference Easterbrooks, Davidson and Chazan1993) and both child internalizing and externalizing behavior problems (as opposed to child fearfulness or child depressive symptoms; Bergman et al., Reference Bergman, Sarkar, Glover and O.’Connor2008; Fox & Borelli, Reference Fox and Borelli2015; Milan et al., Reference Milan, Snow and Belay2009). Further, the majority of studies on the moderating role of attachment have focused on predominantly White samples, limiting generalizability to more diverse populations. Thus, there is a critical need to examine child attachment as a moderator of MDS-associated risk for both internalizing and externalizing behavior problems in populations of parents and children who have been underrepresented in research.
The present study addresses these gaps by examining attachment security as a moderator of the link between MDS and child behavior problems (both internalizing and externalizing) in a predominantly low-SES African American sample. African American families are often underrepresented in psychology research, yet they are overrepresented in exposure to systemic inequities—including racial discrimination, higher rates of poverty, and limited access to quality mental health care—that increase risk for mental health struggles, including MDS (e.g., Belle & Doucet, Reference Belle and Doucet2003). Thus, it is particularly important to examine resilience factors such as the quality of the parent–child relationship in this population (Stern et al., Reference Stern, Barbarin and Cassidy2021), which may also be more at risk for insecure attachment due to exposure to ecological stressors (Bakermans-Kranenburg et al., Reference Bakermans-Kranenburg, van IJzendoorn and Kroonenberg2004; Malda & Mesman, Reference Malda, Mesman, Cabrera and Leyendecker2017; but see also Dexter et al., Reference Dexter, Wong, Stacks, Beeghly and Barnett2013 for evidence to the contrary). We focus on preschool as a critical time to examine these processes because preventing behavior problems is imperative for a successful transition to kindergarten (Ladd & Price, Reference Ladd and Price1987). Specifically, this study examines child attachment security assessed with an observational laboratory procedure as a moderator of the association between MDS and child internalizing and externalizing behavior problems among mothers and their 3- to 5-year-old children from low-income neighborhoods in Baltimore, Maryland. To understand how these developmental processes unfold over time, we leverage data on MDS and child behavior problems from two time points. We hypothesize that MDS will be positively associated with internalizing and externalizing behavior problems at each time point and will predict relative increases in behavior problems over time. However, in line with resilience literature noting attachment security as a protective factor (Masten et al., Reference Masten, Lucke, Nelson and Stallworthy2021), we also predict that these main effects will be moderated by attachment security, such that children who are more securely attached to their mother will be less negatively affected by their mother’s depressive symptoms. In addition to these primary hypotheses, we conducted two sets of exploratory analyses to test (a) if attachment avoidance might similarly interact with MDS to exacerbate risk for child internalizing and externalizing problems, and (b) if there were any reciprocal effects of child behavior problems predicting relative increases in maternal depression over time.
Method
Participants
Mothers (N = 164; M age = 29.68 years, SD = 6.35) and their 3- to 5-year-old children were recruited from four Head Start centers in low-income neighborhoods in Baltimore, Maryland. The sample (66 boys and 98 girls; M age = 44.67 months, SD = 7.14) was diverse (mothers were 76% African American, 12% White/non-Hispanic, 12% other). The demographics of the 137 dyads included in the principal analyses (see Missing Data section; M materal age = 29.73 years, SD = 6.38; 58 boys and 79 girls; M child age = 44.94 months, SD = 7.02; mothers were 76% African American, 12% White/non-Hispanic, 12% other) were nearly identical to those of the larger sample. Participants were part of a larger parenting intervention study (see Cassidy et al., Reference Cassidy, Brett, Gross, Stern, Martin, Mohr and Woodhouse2017, for details).
Procedure
Data were collected at two time points. At Time 1 (T1), mothers provided informed consent and completed a demographic questionnaire and measures of MDS and child behavior problems. Time 2 (T2) data collection, approximately 4–6 months later (M child age = 51.87 months, SD = 6.07), began with a videotaped observational assessment of child attachment. Mothers then completed the same questionnaires assessing MDS and child behavior problems in a separate room while the child completed tasks not relevant to the present study. The session ended with mothers being debriefed and compensated for their time.
Measures
Center for Epidemiological Studies Depression Scale
At T1 and T2, mothers completed this widely used 20-item self-report questionnaire that measures how often depressive symptoms were experienced over the past week (e.g., “I had trouble keeping my mind on what I was doing”). Statements are rated on a 4-point frequency scale, ranging from 0 = rarely or never to 3 = most or all of the time. The measure shows good validity and good internal reliability across diverse samples (Clark et al., Reference Clark, Mahoney, Clark and Eriksen2002; Radloff, Reference Radloff1977, Reference Radloff1991). Items were summed to derive the total score for depressive symptoms used in analyses (αT1 = 0.91, αT2 = 0.91; possible range = 0–60).
Preschool Strange Situation
At T2, child attachment security and avoidance were measured using an adapted version of Ainsworth’s Strange Situation Procedure (Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978; Cassidy et al., Reference Cassidy and Marvin1992; see Solomon & George, Reference Solomon, George, Cassidy and Shaver2016). In the preschool version, children and mothers participate in a 20-min video-recorded lab session that begins with play time with the mother present (approximately 3 min), followed by two separations of mother and child (one 3-min and one 5-min separation), each of which is followed by a 3-min reunion.
The videos were coded for the quality of the reunion on two 9-point scales. Our a priori decision to use the continuous scores (rather than classifications) was based on (a) recent evidence that security is best captured using continuous scores (first from Fraley & Spieker, Reference Fraley and Spieker2003, using the large NICHD Study of Early Child Care and Youth Development [2005] data set; further discussed by Fearon & Roisman, Reference Fearon and Roisman2017, and Groh et al., Reference Groh, Roisman, Booth-LaForce, Fraley, Owen, Cox and Burchinal2014), and (b) in order to obtain greater power. High scores on security indicate positive and warm reunions between mother and child, typically characterized by fluid conversation and often involving contact or close proximity; low scores indicate reunions that are less comfortable, less close in verbal or physical interaction, or show hostility, ambivalence, or odd behaviors such as freezing. High scores on avoidance indicate purposeful limiting of physical or psychological closeness by the child to the mother.
A trained, reliable coder coded all video cases, with 26% coded at random by a second trained coder. Both coders were unaware of study hypotheses. Disagreements were resolved through conferencing. Interrater reliability was strong (ICCsecurity = .89, p < .001; ICCavoidance = .96, p < .001).
Child Behavior Checklist 1.5–5 years
At T1 and following the Strange Situation at T2, mothers completed the standard 100-item report of their children’s behaviors for children ages 1.5–5 years (Achenbach & Rescorla, Reference Achenbach and Rescorla2000). The scale includes dimensions of children’s internalizing (e.g., “sulks”) and externalizing (e.g., “is disobedient”) behavior problems. Items are rated on a 3-point scale, where 0 = not true, 1 = somewhat/sometimes true, 2 = very/often true. This measure shows strong psychometric properties and is used widely in developmental research (Achenbach & Rescorla, Reference Achenbach and Rescorla2000; Nakamura et al., Reference Nakamura, Ebesutani, Bernstein and Chorpita2009). Items were summed to create subscale scores for internalizing (αT1 = 0.88, αT2 = 0.87; possible range = 0–72) and externalizing (αT1 = 0.92, αT2 = 0.92; possible range = 0–48) behavior problems. T-score distributions, reflecting clinical cutoffs for behavior problems, for the current sample are presented in Table 1. At T1, 5% of children scored in the subclinical range and 15% in the clinical range for externalizing behavior problems; 7% scored in the subclinical range and 18% in the clinical range for internalizing problems. At T2, 3% of children scored in the subclinical range and 10% in the clinical range for externalizing behavior problems; 1% scored in the subclinical range and 13% in the clinical range for internalizing problems.
Table 1. Descriptive statistics of key study variables

Note. T1 = Time 1; T2 = Time 2.
* T-scores on the Child Behavior Checklist identify clinical levels of problem behavior. For the internalizing and externalizing behavior problem subscales, scores above 63 reflect clinical problems.
Analytic plan
To investigate whether MDS were associated with child behavior problems over time, and whether these associations were moderated by child attachment, we ran two crosslagged panel models (CLPM) examining child internalizing problems (Model 1) and child externalizing problems (Model 2). This approach allows for examination of both (a) autoregressive paths—denoting the rank-order stability of individual differences in MDS and child behavior problems from T1 to T2—and (b) crosslagged paths—denoting the extent to which T1 levels of one variable relate to T2 levels of the other variable (Biesanz, Reference Biesanz and Hoyle2012). In addition to these standard CLPM paths, we also entered child attachment security at T2, as well as its two-way interactions with MDS at T1 and T2, as predictors of child behavior problems at T2 to test our main study hypotheses. Analyses were completed in Mplus version 7 (Muthén & Muthén, Reference Muthén and Muthén2017) and estimated using maximum likelihood (ML) to account for missing data (Graham, Reference Graham2009; Schafer & Graham, Reference Schafer and Graham2002).
For each model, we followed our a priori plan for the selection of empirically derived covariates: First, we ran an unadjusted model including all possible covariates. Child sex, as well as maternal age, race, education, and marital status were chosen a priori as covariates, as all have been identified as correlates or moderators of environmental effects on children’s developing behavior problems (e.g., Berlin et al., Reference Berlin, Ispa, Fine, Malone, Brooks-Gunn, Brady-Smith, Ayoub and Bai2009; Cassiano et al., Reference Cassiano, Provenzi, Linhares, Gaspardo and Montirosso2018; Coe et al., Reference Coe, Micalizzi, Josefson, Parade, Seifer and Tyrka2020; Kuruczova et al., Reference Kuruczova, Klanova, Jarkovsky, Pikhart and Bienertova-Vasku2020). Child sex (0 = boy; 1 = girl), marital status (0 = not married; 1 = married), maternal education (0 = less than a GED; 1 = GED or above), and maternal race (0 = African American; 1 = not African American) were dichotomized. In addition, we included intervention status (0 = control group, 1 = intervention group; see Cassidy et al., Reference Cassidy, Brett, Gross, Stern, Martin, Mohr and Woodhouse2017), as well as the Head Start site from which each dyad was recruited as an effect-coded covariate to account for clustering. Because our sample was not appropriate for multilevel modeling due to the small number of clusters (N = 4), effect coding was used to return fixed-effect estimates similar to those from multilevel models (McNeish & Stapleton, Reference McNeish and Stapleton2016). Second, we removed all nonsignificant covariates and reran the simplified models to retain power and model parsimony.
Results
Missing data
Of the original 164 dyads, 23 did not participate in the second laboratory visit, and four attachment assessments were lost due to technical error; thus, complete attachment data were available for 137 children. Complete maternal reports of child internalizing behavior problems at T2 were available for 139 children, and of externalizing behavior problems for 140 children. To maximize statistical power, ML estimation was used for the main analyses. Note that because ML’s use of missing data theory does not apply to cases missing both an X (attachment) and Y (T2 MDS and behavior problems) variable, the final analytic sample included only the 137 children with valid attachment data. Participants who dropped out did not differ significantly from those who did not on Time 1 assessments of MDS, child internalizing or externalizing symptoms, or demographic characteristics (age, race, marital status, education).
Preliminary analyses
Descriptive statistics and correlations among main study variables are presented in Tables 1 and 2, respectively. MDS were elevated in the present sample, with 46% and 44% of mothers reporting symptoms above the clinical cutoff of 16 at T1 and T2, respectively. MDS were positively associated with both child internalizing and externalizing behavior problems at both time points, with moderate effect sizes (see Table 2).
Table 2. Correlation matrix of study variables
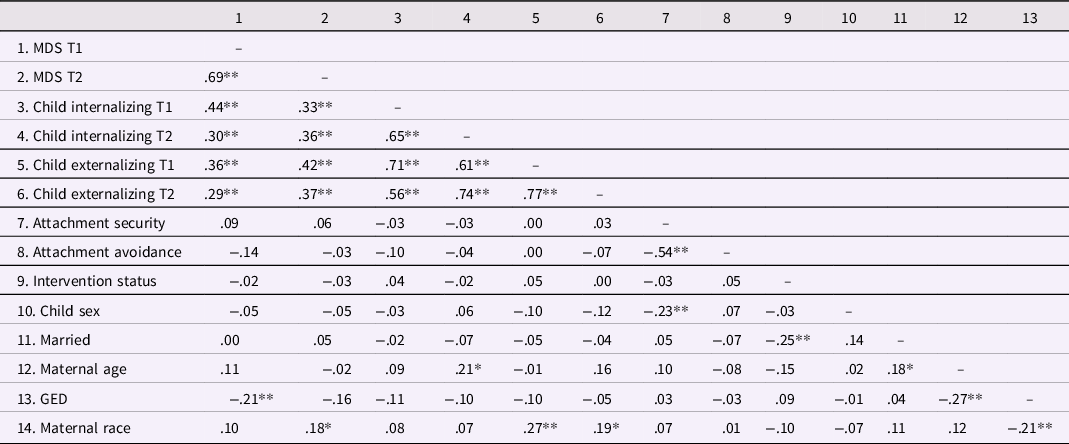
Note. *p < .05, **p < .01. MDS = maternal depressive symptoms. Child sex (0 = boy; 1 = girl), marital status (0 = not married; 1 = married), maternal education (0 = less than a GED; 1 = GED or above), and maternal race (0 = African American; 1 = not African American) were dichotomized and represent point biserial correlations.
Table 3 displays the initial models including all potential covariates, and Table 4 shows the final models retaining only significant covariates. Intervention status, child sex, marital status, maternal race, and Head Start site were not significant and thus were dropped from the final models to retain power and model parsimony. Maternal age significantly predicted MDS at T2 and thus was retained as a covariate.
Table 3. Initial crosslagged panel models examining longitudinal links between maternal depressive symptoms and child internalizing and externalizing behavior problems, moderated by child attachment security, with all covariates included
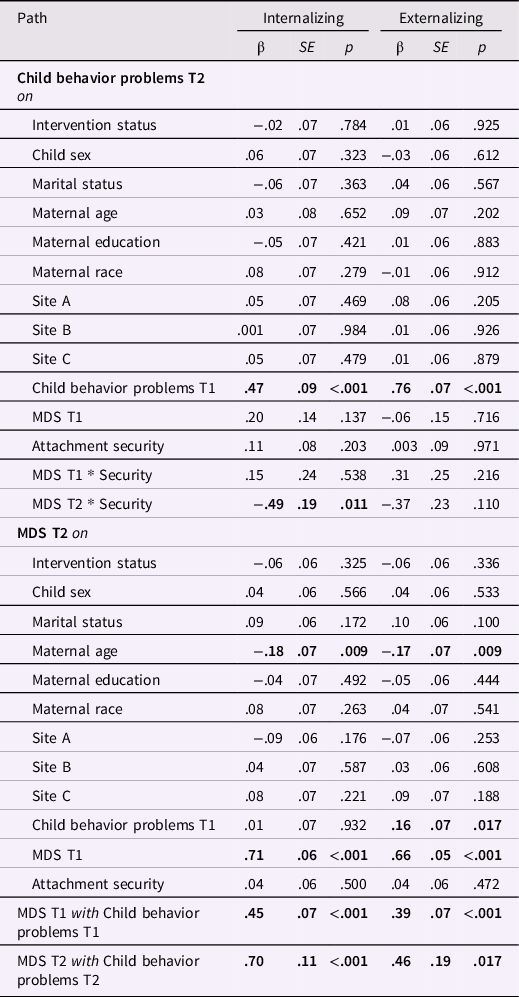
Note. MDS = maternal depressive symptoms. Child sex (0 = boy; 1 = girl), marital status (0 = not married; 1 = married), maternal education (0 = less than a GED; 1 = GED or above), and maternal race (0 = African American; 1 = not African American) were dichotomized. Site = effect-coded Head Start site. Boldface indicates statistical significance at p < .05. Predictors and covariates were allowed to covary.
Table 4. Final crosslagged panel models examining longitudinal links between maternal depressive symptoms and child internalizing and externalizing behavior problems, moderated by child attachment security
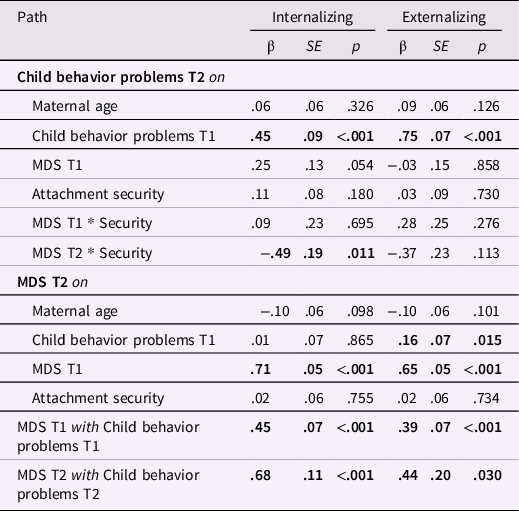
Note. MDS = maternal depressive symptoms. Boldface indicates statistical significance at p < .05. Predictors and covariates were allowed to covary.
Principal analyses
Child internalizing behavior problems
The final models are summarized in Figure 1 and Table 4. With regard to autoregressive paths, both MDS and child internalizing problems showed significant stability from T1 to T2, ps < .001. Additionally, MDS were concurrently associated with child internalizing problems at T1 and T2, ps < .001. With regard to crosslagged paths, child internalizing symptoms at T1 did not predict relative increases in MDS from T1 to T2, p = .865, suggesting no child-driven effects on MDS. MDS at T1 predicted relative increases in child internalizing symptoms from T1 to T2, but this trend was only marginally significant, β = .25, p = .054. There were no significant effects of attachment security on MDS or child internalizing at T2; however, a significant interaction emerged between MDS at T2 and child security predicting child internalizing at T2, p = .011. We probed this interaction using values that were at the mean, one standard deviation above, and one standard deviation below the mean of child security. Simple slopes analyses revealed that MDS at T2 were a significant positive predictor of child internalizing behavior problems at T2 when child attachment security was low (−1 SD below the mean; b = .34, SE = .07; p < .001), and at the mean (b = .23, SE = .06, p < .001), and the effect was attenuated when attachment security was high (+1 SD above the mean; b = .13, SE = .06; p = .038) (Figure 2). Johnson–Neyman regions of significance tests revealed that MDS was no longer a significant predictor of child internalizing when attachment security was +1.8 SD above the mean (18% of the sample).

Figure 1. Final crosslagged models of maternal depressive symptoms and child internalizing (A) and externalizing (B) behavior problems, moderated by attachment security. Values indicate standardized path coefficients (straight lines) and covariances (curved lines). MDS = maternal depressive symptoms; Int = child internalizing problems, Ext = child externalizing problems, *S = interaction with attachment security; Numbers 1 or 2 indicate that the construct was assessed at Time 1 or Time 2, respectively.
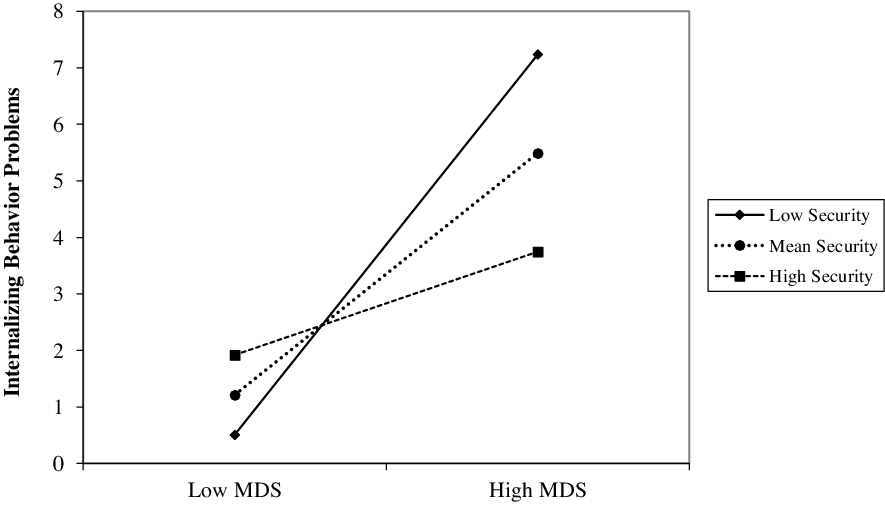
Figure 2. Child attachment security as a moderator of the link between maternal depressive symptoms and child internalizing problems. MDS = maternal depressive symptoms. Maternal depressive symptoms at Time 2 were a significant positive predictor of child internalizing problems at Time 2 when child attachment security was low (−1 SD below the mean; b = .34; p < .001) and at the mean (b = .23, p < .001), and the effect was attenuated when attachment security was high (+1 SD above the mean; b = .13; p = .038). These effects control for covariates, as well as Time 1 levels of MDS and child internalizing.
Child externalizing behavior problems
As in the previous model, autoregressive paths showed strong stability of MDS and child externalizing problems from T1 to T2, ps < .001. Additionally, MDS was concurrently associated with child externalizing problems at T1 and T2, ps < .05. With regard to crosslagged paths, child externalizing problems at T1 significantly predicted relative increases in MDS from T1 to T2, β = .16, p = .015, indicating child-driven effects. In contrast, MDS at T1 did not significantly predict child externalizing at T2, p = .858. There were no effects of attachment security on MDS or child externalizing at T2, and no significant interactions between attachment security and MDS at either time point.
Exploratory analyses
We also tested the same models using child attachment avoidance scores as the moderator (see Table 5). In the model predicting child internalizing symptoms, only maternal age was retained as a covariate. There was no effect of child attachment avoidance on MDS at T2, but, contrary to expectations, avoidance negatively predicted child internalizing at T2, accounting for T1 levels, β = −.23, p = .021. This effect was qualified by a significant interaction between avoidance and MDS at T2 predicting child internalizing at T2, β = .41, p = .048. Simple slopes analyses revealed that MDS at T2 predicted child internalizing at T2 when attachment avoidance was high (b = .31, SE = .06, p < .001) or at the mean (b = .20, SE = .06, p = .001), but not when avoidance was low (b = .08, SE = .07, p = .240). Johnson–Neyman regions of significance tests showed that MDS no longer predicted child internalizing when attachment avoidance was −.97 SD below the mean (37% of the sample).
Table 5. Final exploratory crosslagged panel models examining longitudinal links between maternal depressive symptoms and child internalizing and externalizing behavior problems, moderated by child attachment avoidance
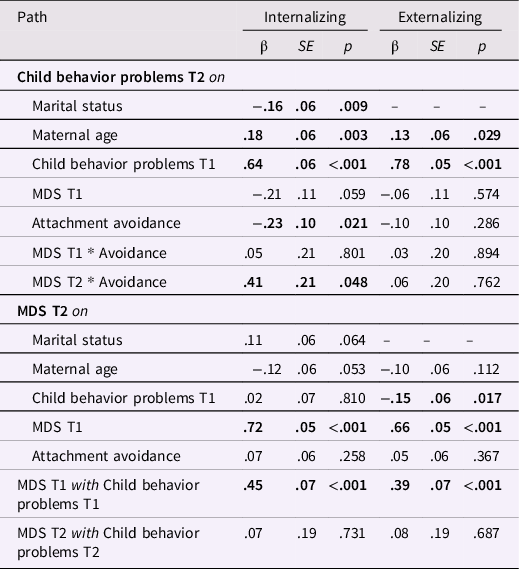
Note. MDS = maternal depressive symptoms. Marital status was dichotomized (0 = not married; 1 = married). Boldface indicates statistical significance at p < .05. Predictors and covariates were allowed to covary.
In the model predicting child externalizing symptoms, only maternal age was retained as a covariate in the final model. There was no effect of avoidance on MDS or child externalizing at T2, and no significant interactions between avoidance and MDS at T1 or T2 (see Table 5).
Finally, to further probe the child-driven effects of externalizing on MDS, we conducted follow-up analyses to explore whether this effect might be moderated by child attachment security or avoidance. In this variation of the crosslagged path model, MDS at T2 was regressed on covariates, T1 MDS levels, child externalizing at T1, attachment security, attachment avoidance, and the two-way interactions between T1 externalizing and the attachment variables. Maternal age and marital status were retained as significant covariates in the final model. There was no significant interaction between T1 externalizing and attachment security, β = −.03, p = .850. However, a significant interaction emerged between T1 externalizing and attachment avoidance, β = .32, p = .020. Simple slopes revealed that child externalizing problems at T1 predicted MDS at T2 when attachment avoidance was high (b = .40, p = .002) or at the mean (b = .23, p = .011), but not when avoidance was low (b = .06, p = .619). Johnson–Neyman regions of significance tests showed that externalizing no longer predicted MDS when attachment avoidance was −.45 SD below the mean (52% of the sample).
Discussion
This study examined child attachment as a moderator of the link between MDS and child internalizing and externalizing behavior problems in an economically stressed, predominantly African American sample at two time points. We found that mothers’ depressive symptoms were concurrently associated with elevated internalizing and externalizing problems in their preschool-aged children, replicating previous findings (Koblinsky et al., Reference Koblinsky, Kuvalanka and Randolph2006). Further, baseline levels of MDS predicted relative increases in child internalizing over time. For child internalizing problems, this association was moderated by child attachment security, such that MDS predicted increases in children’s internalizing problems when security was low; the association was attenuated for highly secure children, providing support for the study hypothesis in relation to child internalizing behavior problems. This moderating effect was specific to internalizing: Attachment security did not moderate the association between MDS and externalizing behavior problems, contrary to predictions. Exploratory analyses revealed that attachment avoidance moderated the effects of MDS on child internalizing in a way that mirrored results for attachment security; specifically, MDS predicted greater internalizing symptoms at T2 when avoidance was average or high, but not when it was low. This study provides key evidence that among families facing multiple contextual risk factors, a high-quality parent–child relationship may serve as an important protective factor against the intergenerational transmission of internalizing symptoms.
Our findings regarding internalizing problems are broadly consistent with previous research demonstrating that secure attachment protects against the transmission of depression from mother to child (Milan et al., Reference Milan, Snow and Belay2009) and that securely attached children may be less affected by contextual and parental risk factors compared insecurely attached children (Cyr et al., Reference Cyr, Pasalich, McMahon and Spieker2014; Kobak et al., Reference Kobak, Cassidy, Lyons-Ruth, Ziv, Cicchetti and Cohen2006). Our findings build on this work by moving beyond predominantly White samples (e.g., Milan et al., Reference Milan, Snow and Belay2009) to shed light on these processes among majority African American mothers and children. Results provide evidence that security plays a similarly protective role in this underrepresented population, supporting the competence hypothesis in attachment theory (i.e., that secure attachment confers benefits for social-emotional development across diverse contexts; Mesman et al., Reference Mesman, Van IJzendoorn, Sagi-Schwartz, Cassidy and Shaver2016). Moreover, our study extends previous research by providing the first indication that this moderation may hold for a broad assessment of internalizing behaviors, and not simply for child depressive symptoms.
Theory and research suggest that children who are securely attached develop more effective emotion regulation skills (Cassidy, Reference Cassidy1994; Calkins & Hill, Reference Calkins, Hill, Gross and Thompson2007; Calkins & Leerkes, Reference Calkins, Leerkes, Vohs and Baumeister2011), in part because secure children have a history of having their distress effectively responded to (Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978; Leerkes, Reference Calkins, Leerkes, Vohs and Baumeister2011). Children who develop emotion regulation skills that protect them against negative coping behaviors, such as rumination and worry, are at reduced risk for symptoms of psychopathology, including internalizing problems (Compas et al., Reference Compas, Jaser, Bettis, Watson, Gruhn, Dunbar, Williams and Thigpen2017); thus, attachment security may protect against the risks associated with MDS in part via endowing children with protective emotion regulation skills.
Notably, attachment security did not significantly moderate the association between MDS and child externalizing behavior problems, which contrasts with some previous work. For example, Easterbrooks et al. (Reference Easterbrooks, Davidson and Chazan1993) found that children exposed to multiple risk factors (including MDS, though this factor was not independently examined) who were also insecurely attached were at elevated risk for both internalizing and externalizing problems, as reported by mothers and teachers. One possibility is that security is a more potent buffer of externalizing symptoms that manifest in classroom settings, and that teacher reports are needed to capture key attachment-related variation in these symptoms. Another possibility is that the present low-income, marginalized sample may be exposed to additional stressors contributing to externalizing problems (e.g., racial discrimination; financial stress) and may therefore need multiple buffers beyond attachment security (e.g., other close, supportive relationships; positive racial socialization) to reduce MDS-related risk for externalizing behavior. Alternately, child externalizing behaviors may emerge as an attempt to cope with these unique stressors, so that attachment security may not decrease these behaviors because they are adaptations to a high-risk environment (Frankenhuis & Del Giudice, Reference Frankenhuis and Del Giudice2012).
Exploratory analyses revealed that children’s attachment avoidance did not significantly predict child internalizing or externalizing behavior problems, consistent with the results of Brumariu and Kerns’s (Reference Brumariu and Kerns2010) review. However, attachment avoidance did moderate the association between MDS and child internalizing behavior problems. Specifically, when child avoidance was at least one standard deviation below the mean, MDS were no longer positively associated with internalizing behavior problems. This suggests that avoidance specifically may undermine effective self-regulation in the context of some forms of parental risk. Given previous research linking attachment avoidance and increased risk for internalizing behavior problems (Groh et al., Reference Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg and Fearon2012), this finding underscores the importance of considering parent-child relationship quality when determining profiles of risk linked with the development of internalizing behavior problems. Future research should consider how attachment insecurity in the form anxiety/resistance or disorganization may also be more likely to exacerbate MDS-associated risk for behavior problems.
With regard to main effects, our findings linking MDS to concurrent levels of child internalizing and externalizing problems are consistent with considerable research (Baker et al., Reference Baker, Brooks-Gunn and Gouskova2020; Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011). This adds support to the notion that maternal mental health is consequential for children’s behavior problems across different contexts and populations, including majority African American families in Head Start (e.g., Baker & Brooks-Gunn, Reference Baker and Brooks-Gunn2020; Johnson & Kliewer, Reference Johnson and Kliewer1999). Moreover, we found evidence that child externalizing, but not internalizing, predicted relative increases in MDS over time, suggesting child-driven effects similar to Baker et al. (Reference Baker, Brooks-Gunn and Gouskova2020). Exploratory analyses revealed that this main effect was qualified by an interaction with child attachment avoidance, suggesting that it is the combination of child externalizing and avoidant attachment that predicts relative increases in MDS from T1 to T2 (a dual-risk model). These data speak to the important issue of bidirectional effects among children and their caregivers.
Contrary to previous research (e.g., Fearon et al., Reference Fearon, Bakermans-Kranenburg, van IJzendoorn, Lapsley and Roisman2010; Groh et al., Reference Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg and Fearon2012), however, we found no main effect of attachment on child internalizing and externalizing behavior problems. One possibility is that attachment security measured in relation to a single caregiver is less directly influential for this population of majority African American children, who often have multiple caregivers to whom they are attached, including fathers, grandparents, and fictive kin (see, e.g., Stern et al., Reference Stern, Barbarin and Cassidy2021; Tyrell & Masten, Reference Tyrell and Masten2021). A second possibility is that because mothers were the sole reporters of child behavior, it may be difficult for a single reporter to provide a full account of children’s behaviors in all contexts. Adding the perspectives of other caregivers or teachers may help to capture attachment-related variation in child behavior problems. We turn to this and other avenues for future research in the following section.
Strengths, limitations, and future directions
Findings should be considered in light of both the strengths and the limitations of the study. Strengths of the study include the use of reliable and well-validated measures such as the Preschool Strange Situation (Cassidy et al., Reference Cassidy and Marvin1992) and our focus on preschool-aged children, as the preschool period is critical for examining factors that reduce risk for behavior problems to support children’s successful transition to school. Future research could examine different age groups and follow families over time to shed light on the role of developmental timing and the chronicity of MDS.
Additionally, our focus on a majority African American, economically stressed sample is both a strength and a limitation of the present study. Given that most previous research has focused on predominantly White samples, this study sheds light on a population that is too often underrepresented in psychology research. It is important to understand how maternal depression and attachment relate to behavioral outcomes in marginalized populations, particularly given that African American families are disproportionately exposed to racism and other inequities that are consequential for physical and mental health (e.g., Belle & Doucet, Reference Belle and Doucet2003). Thus, attending to Black families’ mental health needs and reducing intergenerational transmission of mental health struggles are vital equity issues. At the same time, however, the focus on this population also limits generalizability. Future research that includes participants of a diversity of racial and ethnic groups (e.g., Latinx) and socioeconomic strata will be important.
Importantly, because our sample was drawn from an urban, low-SES population, other contextual risk factors may be present (e.g., discrimination, neighborhood violence), contributing to both mother and child symptomatology. Further, attachment security may also act as a protective factor against these additional unmeasured risk factors. Future work should seek to measure these contextual risk factors to enrich our understanding of the context in which MDS, child attachment, and behavior problems develop.
Notably, mothers were reporters for both their own depressive symptoms and their children’s internalizing and externalizing behavior problems, raising potential issues of reporter bias and shared method variance when considering links between MDS and child behavior problems. Notably, however, shared method variance is not problematic for the central findings of the present study regarding moderation by attachment, given that interaction effects are likely to be attenuated, rather than inflated, in the presence of shared method variance, even when one of the interaction terms is not a source of the shared variance (Siemsen et al., Reference Siemsen, Roth and Oliveira2010). Even so, mothers’ cognitive biases related to depressive symptomology may impact their perceptions and reporting of their child’s behavior (e.g., De Los Reyes et al., Reference De Los Reyes, Goodman, Kliewer and Reid-Quinones2008). In addition, child behavior in one context may not align with behavior in another (e.g., school). Future research drawing on other reporters (such as grandparents, childcare providers, or teachers) may give a better idea of how the children might behave in different environments and how a caregiver other than the parent may see these behaviors.
Clinical implications
Rates of maternal depression tend to be particularly high among parents of children in Head Start (e.g., 41% reported by Lanzi et al., Reference Lanzi, Pascoe, Keltner and Ramey1999); indeed, the proportion of mothers reporting clinically significant levels of depressive symptoms in the present sample (>40% at both time points) is likewise high compared to previous community samples. Given this high rate, there has been considerable interest in interventions to reduce maternal depression, and some evidence supports their success (e.g., Gelfand et al., Reference Gelfand, Douglas, Seiner and Jameson1996). Because secure attachment in early childhood is a key modifiable resilience factor buffering children from the negative effects of MDS, attending to improving parent–child relationship quality within interventions focused on parental depression could enhance children’s well-being. It is noteworthy that the few studies examining child attachment within Head Start have reported elevated levels of insecure attachment (e.g., Hoffman et al., Reference Hoffman, Marvin, Cooper and Powell2006; Spieker et al., Reference Spieker, Nelson, DeKlyen, Staerkel, Berlin, Ziv, Amaya-Jackson and Greenberg2005); our findings of the protective role of attachment security, along with the elevated risk for maternal depression within Head Start samples, highlight the importance of interventions to enhance attachment security within Head Start programs (Cassidy et al., Reference Cassidy, Brett, Gross, Stern, Martin, Mohr and Woodhouse2017; see also Spieker et al., Reference Spieker, Nelson, DeKlyen, Staerkel, Berlin, Ziv, Amaya-Jackson and Greenberg2005). Relatedly, interventions focused on parenting may provide particular benefit when they include resources for assessing and treating parental depression. Such multitargeted interventions could help protect children from the potential risks of MDS among children with insecure attachment and reduce the likelihood of the intergenerational transmission of internalizing problems. Moreover, multitargeted interventions build positive spirals to benefit both mother and child: If a parent feels competent as a secure base for her child, her self-efficacy may increase and feelings of helplessness may decrease; and if children feel secure in their relationships with their caregivers, then they may be relatively buffered from the negative effects of maternal depression.
Acknowledgments
We are grateful for the help of the following people: Jacquelyn Gross was instrumental in the study's design, data collection, coordination, tracking, and data management; Danielle Gregg and Elizabeth Thompson provided and coordinated laboratory space at the Family Center at Kennedy Krieger Institute in Baltimore, MD; Susan Paris and Bonnie Conley assisted with Strange Situation coding; and many hardworking and dedicated undergraduate research assistants assisted with data collection and coding. We are grateful to the families who generously participated in our study.
Author contributions
Paige N. Whittenburg and Jessica A. Stern contributed equally to the article.
Funding statement
This research was supported by The Zanvyl and Isabelle Krieger Fund. Manuscript preparation was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number F32HD102119 (to JS). The content is solely the responsibility of the authors and does not necessarily represent the views of the Krieger Fund or of the National Institutes of Health.
Conflicts of interest
None.









