Introduction
Posttraumatic stress in childhood and adolescence
Exposure to traumatic events during childhood and adolescence is not uncommon. Many children witness severe domestic violence (Meltzer et al., Reference Meltzer, Doos, Vostanis, Ford and Goodman2009) and experience abuse (Finkelhor et al., Reference Finkelhor, Turner, Shattuck and Hamby2015), war trauma, natural disasters, and serious accidents (Costello et al., Reference Costello, Erkanli, Fairbank and Angold2002). A meta-analysis concluded that 15.9% of children exposed to traumatic events subsequently develop Posttraumatic Stress Disorder (PTSD) (Alisic et al., Reference Alisic, Zalta, van Wesel, Larsen, Hafstad, Hassanpour and Smid2014). Whilst it is necessary for a child to have been directly or indirectly exposed to a traumatic event to diagnose PTSD, it is recognized that exposure to a traumatic event alone is not sufficient and several risk factors have been identified as increasing the likelihood of developing PTSD. Individual risk factors such as low social support and social withdrawal, along with peri-traumatic risk factors such as peri-trauma fear have been identified as increasing a child’s risk of developing PTSD (Trickey et al., Reference Trickey, Siddaway, Meiser-Stedman, Serpell and Field2012). Exposure to interpersonal trauma can lead to more severe Posttraumatic Stress Symptoms (PTSS) when compared to events which are non-interpersonal in nature (for a review, see Charuvastra & Cloitre, Reference Charuvastra and Cloitre2008). This has led to recommendations for research to further investigate the role of social factors in the development of PTSD.
Attachment theory and posttraumatic stress
Attachment theory highlights the importance for children’s socioemotional development and resilience of the provision of a safe haven by their caregivers (Bowlby, Reference Bowlby1969). Ainsworth and colleagues carried out extensive research and observations of caregiver-infant dyads which led to the classification of attachment patterns: secure, insecure-resistant, and insecure-avoidant, with the later addition of disorganized attachment (Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978; Main & Solomon, Reference Main, Solomon, Brazelton and Yogman1986). There are also two traditions of attachment research, stemming from developmental psychology and social psychology. Developmental psychologists tend to use observational measures to study young children’s attachment relationships, and narrative interviews or projective measures such as doll play with older children. Social psychologists tend to use self-report methods and treat individual differences in attachment as structured by two latent factors, anxiety and avoidance, as opposed to four categories.
Extensive research efforts have been carried out to determine whether attachment representations are associated with difficulties with social and emotional adjustment in children. Meta-analytic reviews of this research have documented effect sizes of d = .15 in the relation between attachment insecurity and internalizing problems (Groh et al., Reference Groh, Roisman, van Ijzendoorn, Bakermans-Kranenburg and Fearon2012) and d = .31 in the relation between attachment insecurity and externalizing problems (Fearon et al., Reference Fearon, Bakermans-Kranenburg, van Ijzendoorn, Lapsley and Roisman2010). Further meta-analytic evidence indicates a moderate relationship between attachment insecurity and depression (Spruit et al., Reference Spruit, Goos, Weenik, Rodenburg, Niemeyer, Stams and Colonnesi2020) and anxiety (Colonnesi et al., Reference Colonnesi, Draijer, Stam, Van der Bruggen, Bogels and Noom2011) in children and adolescents. There have been calls for research to examine the causality of these relationships, which has led to the development of a number of theoretical models. For example, the social model of PTSD (Woodhouse et al., Reference Woodhouse, Brown and Ayers2018) highlights the role of fearful attachment and social processes in the development of PTSD. The authors propose that group identification, social acknowledgement and posttraumatic cognitions have a role in the symptom severity of PTSD.
A child’s ability to recover from a traumatic event is presumed to be influenced by the quality of their attachment to the caregiver and the caregiver’s ability to respond to distress in a sensitive way. This is considered an important part of the relevance of attachment to clinical practice (e.g., Allen, Reference Allen2018; Gomez-Perales, Reference Gomez-Perales2015). A range of specific pathways and mechanisms for the putative relationship between attachment and posttraumatic psychopathology such as PTSD have been proposed. Some accounts posit PTSD as resulting from a disrupted attachment system (de Zulueta, Reference de Zulueta2007), whereby an infant develops a psychobiological response to feeling threatened by their caregiver. MacDonald et al. (Reference Macdonald, Beeghly, Grant-Knight, Augustyns, Woods, Cabral, Rose-Jacobs, Saxe and Frank2008) highlighted that disorganized attachment during infancy may increase vulnerability to dissociative and externalizing symptoms when trauma is experienced later in life. Such accounts particularly consider the role of disorganized attachment during early childhood. More recently, theorists have tried to identify a role for attachment within social-cognitive models of PTSD (e.g., Sharp et al., Reference Sharp, Fonagy and Allen2012). According to such accounts, traumatic experiences with caregivers may lead to impaired mentalizing, which in turn places an individual at greater risk of developing psychopathology such as PTSD (e.g., through difficulties in making effective use of social support) when confronted with later trauma.
Authors within the field have proposed that we can expect the attachment behavioral system to be activated in response to stressful and traumatic life events. For example, Mikulincer et al. (Reference Mikulincer, Shaver and Solomon2015) discussed that emotional responses to stressful and traumatic events, which include feelings of panic and vulnerability (Horowitz, Reference Horowitz, Millon, Green and Meagher1982), are likely to activate the attachment behavioral system, thus encouraging a person to seek support from others at times of distress. They argued that a person with a secure attachment may expect others to offer care and support in order to reduce distress, whereas a person with an insecure attachment may not have expectations of others being supportive, thus preventing the opportunity for regulation of distress (Mikulincer et al., Reference Mikulincer, Shaver and Solomon2015). Further, children still rely on parents for a sense of safety and support following exposure to a traumatic event (Ensink et al., Reference Ensink, Fonagy, Normandin, Rozenberg, Marquez, Godbout and Borelli2021).
Rationale for current study
To our knowledge, three existing reviews (specifically Barazzone et al., Reference Barazzone, Santos, McGowan and Donaghay-Spire2019; Marshall & Frazier, Reference Marshall and Frazier2019; Woodhouse et al., Reference Woodhouse, Ayers and Field2015) have examined the relationship between attachment and PTSS, though they have focused exclusively on research within adult populations. Woodhouse et al. (Reference Woodhouse, Ayers and Field2015) conducted a quantitative synthesis of studies and identified an association between secure attachment and lower PTSS (
![]() $$\hat \rho $$
= −.27), and an association in the opposite direction between insecure attachment and PTSS (
$$\hat \rho $$
= −.27), and an association in the opposite direction between insecure attachment and PTSS (
![]() $$\hat \rho $$
= .26). Yet there has been no synthesis to date of findings regarding children and adolescents. Though it is not possible to establish causality, some benefits are nonetheless anticipated from such a synthesis. Improved understanding of the extent of the relevance of attachment for PTSS in children and adolescents, and vice versa, may assist in clinical assessment and intervention. For instance, current models of PTSD incorporate prior experiences and the coping capacity of the individual but do not incorporate attachment (e.g., Ehlers & Clark, Reference Ehlers and Clark2000).
$$\hat \rho $$
= .26). Yet there has been no synthesis to date of findings regarding children and adolescents. Though it is not possible to establish causality, some benefits are nonetheless anticipated from such a synthesis. Improved understanding of the extent of the relevance of attachment for PTSS in children and adolescents, and vice versa, may assist in clinical assessment and intervention. For instance, current models of PTSD incorporate prior experiences and the coping capacity of the individual but do not incorporate attachment (e.g., Ehlers & Clark, Reference Ehlers and Clark2000).
Aims
The aim of this meta-analytic review is to provide a quantitative synthesis of studies examining the relationship between attachment and PTSS in children and adolescents. This meta-analysis also aims to identify whether the relationship between attachment and PTSS differs according to the type of traumatic event experienced, specifically the experience of childhood maltreatment compared to other types of trauma. This was because of the concern that maltreated children may be at particular risk of insecure/disorganized attachments with their primary caregiver (Cicchetti & Doyle, Reference Cicchetti and Doyle2016), and therefore at greater risk of developing PTSS. Moreover, we sought to consider whether the type of attachment measure used – that is, derived from the developmental tradition as opposed to the social tradition – changed the strength of the relationship between attached and PTSS.
It is recognized that many children experience symptoms of posttraumatic stress without meeting the diagnostic criteria for PTSD. This review will focus on PTSS rather than diagnosed PTSD to ensure that findings are generalizable to both clinical and non-clinical populations, and to take account of the greater sensitivity and power that arises from using continuous outcome measures.
The research questions are as follows:
-
1. What is the strength of the relationship between attachment style and PTSS in children and adolescents?
-
2. Does the relationship between attachment orientation and posttraumatic stress differ in children and adolescents who have experienced maltreatment compared to other types of traumatic events?
It is hypothesized that attachment security will be associated with lower levels of PTSS and attachment insecurity will be associated with higher levels of PTSS and that exposure to maltreatment will lead to increased PTSS when compared with other types of traumatic events.
Method
Protocol and registration
The review was pre-registered on PROSPERO in April 2019 (registration number CRD42019132799).
Inclusion and exclusion criteria
Study inclusion criteria were i) both attachment and PTSS were measured in the same sample, ii) the study allowed for an effect to be derived for the relationship between these two variables, and iii) the study comprised individuals with an average age of under 18 (i.e., children and/or adolescents). The following exclusion criteria were applied:
-
Attachment was not measured
-
PTSS was not measured
-
There was insufficient information to calculate a correlation coefficient
-
Studies were not written in the English language
-
Study sample consisted of adult participants (i.e., an average age of over 18 years)
-
Participants had neurodevelopmental disorders or learning disabilities
It was agreed a priori that it may be difficult to assess attachment difficulties in children and adolescents with neurodevelopmental disorders as these can present in a similar way to attachment difficulties, and this decision led to the exclusion criteria of studies based on a sample of children or adolescents with learning disabilities and neurodevelopmental disorders.
Database searches
A systematic search was conducted in May 2019 and updated in June 2022 using four literature databases (PubMed, PsycINFO, Web of Science, OpenGrey, and ProQuest Dissertations and Theses). Search terms were selected by reviewing terms used in similar reviews and refining to allow for identification of relevant papers within the current area. The following search terms were entered within each database: (“posttraumatic stress” OR “posttraumatic stress disorder” OR “post-traumatic stress” OR “post-traumatic stress disorder” OR “traumatic stress” OR “acute stress disorder” OR PTSD OR PTSS) AND (attachment OR attach* OR “strange situation”). Age-specific search terms were not included at this stage to allow for the identification of studies which report on both child and adult samples. Four researchers screened the abstracts and conducted full-text reviews. The initial searches identified 2932 articles which were transferred to Endnote. Endnote removed 534 duplicates, leaving 2398 abstracts for screening. Following a review of all titles and abstracts, irrelevant papers were excluded leaving 143 articles for full-text review. The search terms returned one meta-analysis and five systematic reviews. The reference lists of these papers were searched and no additional papers were identified.
Of the 143 full papers that were reviewed, 113 were excluded leaving 30 papers for inclusion in the meta-analysis. Preferred Reporting Items for Systematic Reviews and Meta-analysis (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009) was used during the article selection process which is reported in Figure 1. The papers included in the meta-analysis are marked with a * in the reference section.

Figure 1. PRISMA flow diagram demonstrating article screening and selection based on Moher et al. (Reference Moher, Liberati, Tetzlaff and Altman2009).
Data extraction
Two researchers carried out data extraction for the review. The following information was extracted from each study: country of origin, study design (e.g., prospective, cross-sectional), sample size, type of traumatic event, mean participant age and age range, percentage male and female, participant ethnicity, type of sample (e.g., trauma-exposed, clinic-recruited, community sample, and randomized controlled trial baseline sample), name of attachment measure, type of attachment measure (e.g., interview, questionnaire), type of attachment classification (e.g., categorical, continuous), name of PTSS measure, PTSS measure type (e.g., interview, questionnaire), study quality and effect size. Four studies reported a correlation coefficient of the relationship between attachment orientation and PTSS for each parent. The majority of the remaining studies (k = 26) reported on the relationship where the attachment figure being rated was the mother. Where correlation coefficients for both parents were available, information for the mother relationship was chosen to ensure consistency between studies and these data were used in the main meta-analyses. Sensitivity analyses were then conducted to incorporate attachment to father by transforming the correlation coefficient to Fishers Z to calculate the average, then transforming back to Pearson’s r. This value was then entered in to the sensitivity analysis.
Categoriation of attachment
The studies included in the meta-analysis reported effect sizes to estimate the strength of the relationship between PTSS and seven types of attachment classification. These are summarized as secure (n = 20), insecure (n = 4), avoidant (n = 9), anxious (n = 7), disorganized (n = 5), ambivalent (n = 2), and dependent (n = 2). Studies reporting effect sizes for forms of insecure attachment (i.e., avoidant attachment, disorganized attachment, ambivalent attachment, anxious attachment, dependent attachment) were grouped together for one meta-analysis. Studies reporting effect sizes for secure attachment were grouped together for one meta-analysis. Avoidant attachment, anxious attachment, and disorganized attachment were then analyzed separately in order to provide effect sizes for distinct attachment patterns. This categorization of attachment classification led to five separate meta-analyses. Two studies reported ambivalent attachment (Levendosky et al., Reference Levendosky, Huth-Bocks and Semel2002; Punamaki et al., Reference Punamaki, Palosaari, Diab, Peltonen and Qouta2015) and two reported dependent attachment (Ferrajao & Elklit, Reference Ferrajao and Elklit2021; Zerach & Elklit, Reference Zerach and Elklit2020). These have not been meta-analyzed because they are included in the overall insecure attachment meta-analysis. Nine continuous measures and four categorical measures of attachment were reported by studies in the review.
Calculation of effect size
A correlation coefficient (Pearson’s r) was selected to represent effect sizes because it was reported in the majority of studies eligible for inclusion and could be estimated from other effect size statistics. Where a correlation coefficient was not reported, calculations were carried out to estimate Pearson’s r from the reported statistic such as Cohen’s d (Rosenthal, Reference Rosenthal1994), odds ratio (Borenstein et al., Reference Borenstein, Hedges, Higgins and Rothstein2009) and standardized regression coefficient (β) (Peterson & Brown, Reference Peterson and Brown2005). In cases where studies reported two correlation coefficients for two different types of insecure attachment classification for the insecure attachment meta-analysis, both correlation coefficients were transformed to Fisher’s Z and the mean of both scores was calculated. The mean was then transformed back to Pearson’s r.
Quality assessment and risk of bias tool
An adapted version of the quality assessment tool for observational cohort and cross-sectional studies (National Heart, Lung and Blood Institute, 2014) was used to assess quality and risk of bias (see Supplementary Material 1). Scores for individual items were summed and converted to a percentage. Sixteen studies were assessed for quality and risk of bias independently by two researchers. Inter-rater reliability was calculated (85.7%).
Meta-analytic method
Meta-analytic calculations were undertaken using MAVIS version 1.1.3 (Hamilton, Reference Hamilton2017) which uses the metafor package for R (Viechtbauer, Reference Viechtbauer2010). A random effects model (Hedges & Vevea, Reference Hedges and Vevea1998) was used in each of the meta-analyses. Following Cohen (Reference Cohen1988), effect sizes greater than .1 were classed as being small, effect sizes greater than .3 as medium, and effect sizes greater than .5 as large. Moderator analyses were conducted to examine whether the relationship between attachment and PTSS differed according to whether the sample had been exposed to maltreatment compared with other types of traumatic events. It is recommended that a minimum of four studies are required to run moderator analyses (Fu et al., Reference Fu, Gartlehner, Grant, Shamliyan, Sedrakyan, Wilt, Griffith, Oremus, Raina, Santaguida, Lau and Trikalinos2011).
Where there were concerns about the methodology employed by studies, sensitivity analyses were undertaken to see if these studies had an undue influence on the overall result. Two studies included in the review reported effect sizes based on odds ratio statistics (Bosquet-Enlow et al., Reference Bosquet-Enlow, Egeland, Carlson, Blood and Wright2014; Punamaki et al., Reference Punamaki, Palosaari, Diab, Peltonen and Qouta2015) which were a different measure of effect size in comparison to Pearson’s r; this raised the potential for over or under-estimation of Pearson’s r when estimating from an odds ratio statistic. Sensitivity analyses were run to examine whether the removal of these studies made a difference to the overall estimated effect size.
Two studies included in the meta-analysis used proxy measures of attachment. For example, Feldman and Vengrober (Reference Feldman and Vengrober2011) made behavioral observations of child participants during the discussion of trauma memories. Mother and child behavior was coded according to the Coding Interactive Behaviour (Feldman, Reference Feldman1998) in order to derive scores of secure base and avoidant behavior. Coding Interactive Behaviour is a coding system designed for adult and child interactions. Observations were coded in accordance with maternal sensitivity (α = .82), child secure base behavior (α = .84), and child avoidant behavior (α = .81). Boeckel et al. (Reference Boeckel, Wagner and Grassi-Oliviera2015) used the Maternal Bond Inventory (Boeckel et al., Reference Boeckel, Wagner, Sohne, Schein and Grassi-Oliviera2011) as a proxy measure for the measurement of secure attachment. The Maternal Bond Inventory is a 26-tem questionnaire which was developed based on the Maternal Attachment Inventory (Muller, Reference Muller1994). Boeckel et al. (Reference Boeckel, Wagner, Sohne, Schein and Grassi-Oliviera2011) identified two factors: 1) interaction and affection of the mother towards her child and 2) the mother’s perception of the bond towards her child. The questionnaire is based on a 5-point Likert scale whereby higher scores indicate a stronger maternal bond, an index of attachment security in this meta-analysis. Internal consistency was reported as α = .93 in the study sample. Sensitivity analyses were conducted to assess whether the removal of these studies had an effect on the overall estimated effect size.
Five studies used measures of attachment rooted in the social psychology tradition. Therefore, sensitivity analyses were run to examine whether removal of these studies made a difference to the overall estimated effect size. Five studies used a prospective design. Sensitivity analysis were conducted to assess whether the removal of these studies made a difference to the overall estimated effect size. Finally, all studies using a prospective design were analyzed separately.
Results
Study characteristics
Thirty studies were included in the review. Study characteristics are reported in Table 1. Within the studies included, the sample size ranged from 19 to 3232; the total sample size was 10,431. The majority of studies used a cross-sectional design (k = 25) with five studies using a prospective design. Of the studies that used a prospective design, three studies measured attachment prior to the child’s exposure to a traumatic event. A range of measures were used to assess attachment style and PTSS which are summarized in Table 1. Fourteen attachment assessments were used, ranging from self-report (e.g., Experiences in Close Relationships – Short Form; Wei et al., Reference Wei, Russell, Mallinckrodt and Vogel2007), interview-based assessments (e.g., Child Attachment Interview;Target et al., Reference Target, Fonagy and Shmueli-Goetz2003), and observation-based assessments (e.g., Strange Situation Procedure;Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978). This led to varying types of reporting of attachment such as classification and dimensions. Of the 14 attachment assessments identified, nine were based within the developmental tradition and five were based on the social tradition of attachment classification. Twelve measures were used to assess PTSS, ranging from self-report (e.g., Impact of Events Scale Revised; Weiss & Marmar, Reference Weiss and Marmar1997) and interview-based measures (e.g., Diagnostic Interview of Children and Adolescents – PTSD Section; Reich et al., Reference Reich, Welner and Herkanic1995), and the majority were based on DSM diagnostic criteria for PTSD.
Table 1. Study characteristics

Note. C = PTSD-CL = Child PTSD Checklist (Amaya-Jackson et al., Reference Amaya-Jackson, McCarthy, Cherney and Newman1995). CITES-II = Children’s Impact of Events Scale II (Wolfe, Reference Wolfe2002). CPSS = Child PTSD Symptom Scale (Foa et al., Reference Foa, Johnson, Treadwell and Kimberli2001). CRIES = Children’s Revised Impact of Events Scale (Children and War Foundation, 1998). CS = Cross-sectional. DC:0-3R = Diagnostic classification: 0–3 revised (Zero To Three, 2005). DICA = Diagnostic Interview of Children and Adolescents – PTSD Section (Reich et al., Reference Reich, Welner and Herkanic1995). IES-R = Impact of Events Scale Revised (Weiss & Marmar, Reference Weiss and Marmar1997). K-SADS = Kiddie Schedule for Affective Disorders and Schizophrenia (Orvaschel et al., Reference Orvaschel, Puig-Antich, Chambers, Tabrizi and Johnson1982). LASC = Los Angeles Symptom Checklist (King et al., Reference King, King, Leskin and Foy1995). NR = Not reported. PCL-5 = PTSD Checklist for DSM-5 (Weathers, Reference Weathers2013). PTS-PRP = The Posttraumatic Stress Scale from Personal and Relationships Profile (Straus & Mouradian Reference Straus and Mouradian1999). PTSDSSI = The Posttraumatic Stress Disorder Semi-Structured Interview and Observational Record for Infants and Young Children (Scheeringa & Zeanah, Reference Scheeringa and Zeanah1994). P = Prospective. TSCC = Trauma Symptom Checklist for Children (Briere, Reference Briere1996). UCLA PTSD RI = UCLA PTSD Reaction Index (Pynoos et al., Reference Pynoos, Rodriquez, Steinberg, Stuber and Frederick1998).
Attachment measures marked with a * used proxy measures of attachment and were removed in the sensitivity analyses. Attachment measures marked with an “(S)” are in the social tradition (as opposed to the developmental tradition).
Sample characteristics
The mean age of participants in the studies ranged from 33 months to 17.5 years, with an overall mean age of 12.7 years. Of the studies that reported demographic information of participant sex (k = 28), gender split ranged from 23.8% female to 100% female with the gender split of the total sample being 51.1% female. The nature of trauma exposure varied from maltreatment (k = 9), war trauma (k = 7), and natural disaster (k = 4). Four studies did not specify the type of trauma exposure. Participant recruitment ranged from samples who were recruited due to trauma exposure (k = 14), clinic-based recruitment (k = 7), community samples (k = 7) and randomized controlled trial baseline samples (k = 2).
Assessment of study quality and risk of bias
The majority of studies were rated as being high quality (k = 20) and the remaining studies were rated as being medium quality (k = 10) using the quality assessment tool as rated by two researchers.
Meta-analysis of secure attachment and PTSS
Twenty of the included studies reported an effect size of the relationship between secure attachment and PTSS (N = 8544). The pooled effect size was r = −.16 (95% CI = −.24, −.07, z = −3.87, p = .0001; for forest plot, see Figure 2). Heterogeneity estimates indicated that there was significant variance within the included studies (Q = 185.23, df = 19, p < .0001); I2 was 89.7%, indicating a high level of heterogeneity. A funnel plot was approximately symmetrical upon visual inspection and suggested three missing studies in the meta-analysis. Kendall’s tau was −.1474, p = .3859, indicating no significant asymmetry.
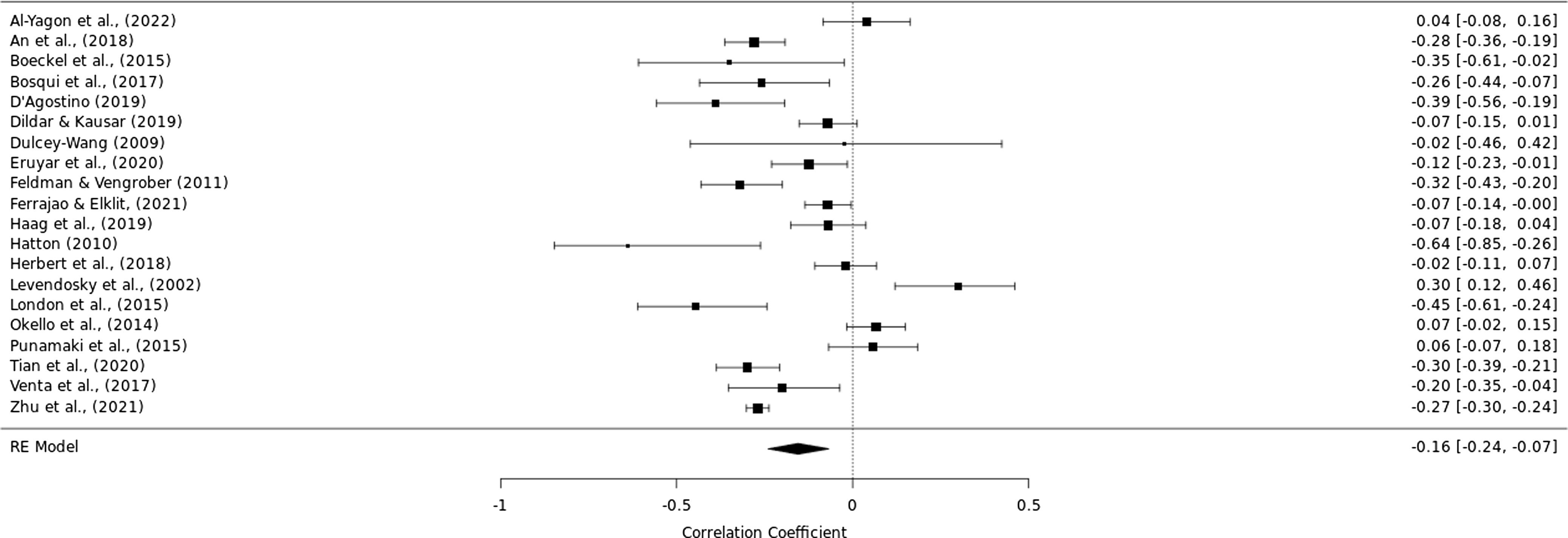
Figure 2. Forest plot for studies reporting the relationship between secure attachment and PTSS.
Moderators of the relationship between secure attachment and PTSS. A moderator analysis was conducted to assess whether exposure to maltreatment had a moderating effect on the strength of the relationship between secure attachment and PTSS compared to other types of trauma. Maltreatment did not moderate the relationship between secure attachment and PTSS (see Table 2 for sub-group and moderation test results).
Table 2. Trauma type as a moderator of the relationship between secure attachment and PTSS

Note. l. CI refers to the lower limit of the 95% confidence interval; u.CI refers to the upper limit of the 95% confidence interval.
Meta-analysis of insecure attachment and PTSS
Sixteen studies reported an effect size of the relationship between insecure attachment (i.e., including attachment orientations labeled avoidant, disorganized, ambivalent and anxious attachment, as well as classifications of general insecurity) and PTSS (N = 4019). A pooled effect size of r = .20 (95% CI = .14, .27, z = 5.24, p < .0001) was derived (for forest plot see Figure 3). Heterogeneity estimates indicated that there was significant variance between effect sizes (Q = 78.77, df = 15, p < .0001). I2 was 81%, indicating a moderate degree of variance in effect sizes. The funnel plot was deemed to be approximately symmetrical upon visual inspection and suggested no studies missing from the meta-analysis. Kendall’s tau was −.0753, p = .6850, indicating no significant asymmetry.
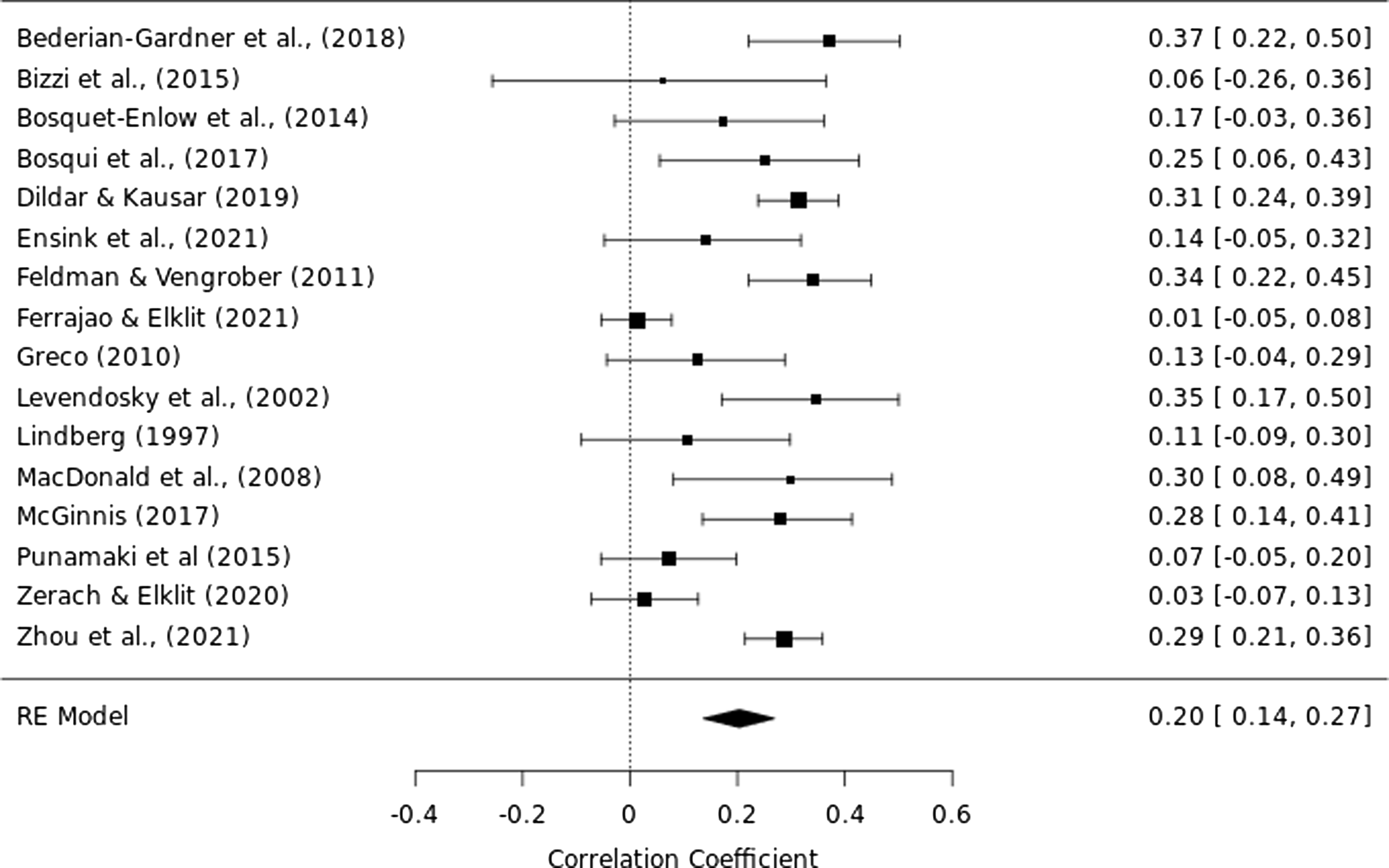
Figure 3. Forest plot for studies reporting the relationship between insecure attachment and PTSS.
Moderators of the relationship between insecure attachment and PTSS. A moderator analysis was conducted to assess whether exposure to maltreatment had a moderating effect on the strength of the relationship between insecure attachment and PTSS compared to other types of trauma. Maltreatment did moderate the relationship between insecure attachment and PTSS (see Table 3 for sub-group and moderation test results).
Table 3. Trauma type as a moderator of the relationship between insecure attachment and PTSS

Note. l. CI refers to the lower limit of the 95% confidence interval; u.CI refers to the upper limit of the 95% confidence interval.
Meta-analysis of avoidant attachment and PTSS
Nine studies reported an effect size of the relationship between an avidant attachment style and PTSS (N = 2242). The pooled effect size was r = .20 (95% CI = .11, .29, z = 4.57, p < .0001; for forest plot see Figure 4). Heterogeneity estimates indicated significant variability between effect sizes (Q = 30.68, df = 8, p = .0002). I 2 was 73.9%, demonstrating a moderate degree of variance between study effect sizes. Funnel plots suggested that there were no studies missing from the meta-analysis. Kendall’s tau = .2222, p = .4767, indicating no significant asymmetry.

Figure 4. Forest plot for studies reporting the relationship between avoidant attachment and PTSS.
Meta-analysis of anxious attachment and PTSS
Seven studies reported an effect size of the relationship between an anxious attachment style and PTSS (N = 2842). The pooled effect size was r = .32 (95% CI = .26, .37, z = 11.01, p < .0001; for forest plot see Figure 5). Heterogeneity estimates indicated no significant variability between effect sizes (Q = 12.46, df = 6, p = .0524). I 2 was 51.9%, demonstrating a moderate degree of variance between study effect sizes. Funnel plots suggested that there were no studies missing from the meta-analysis. Kendall’s tau = −.1429, p = .7726, indicating no significant asymmetry.
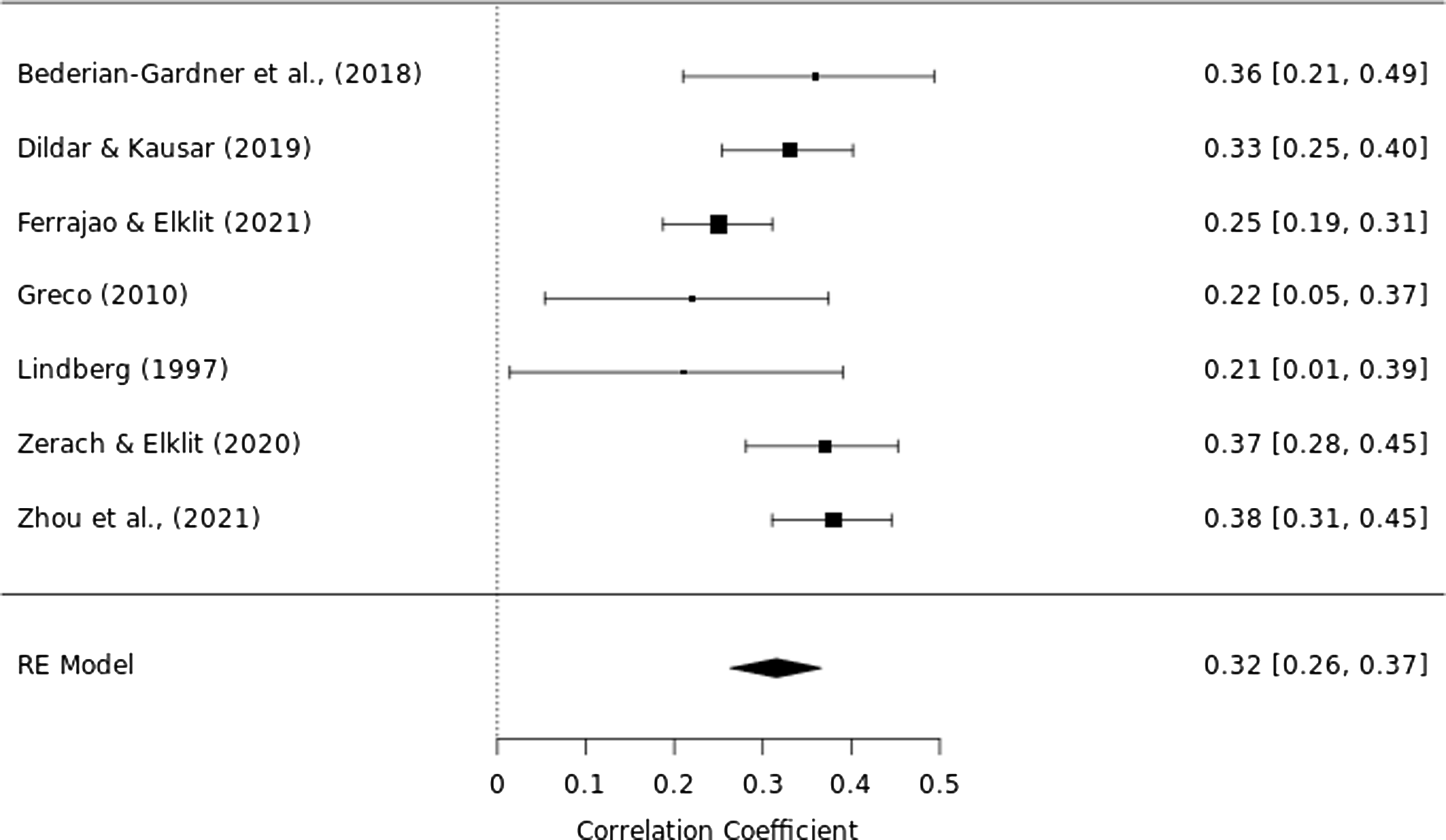
Figure 5. Forest plot for studies reporting the relationship between anxious attachment and PTSS.
Meta-analysis of disorganized attachment and PTSS
Five studies reported an effect size of the relationship between disorganized attachment (as assessed by the Strange Situation Procedure and Child Attachment Interview) and PTSS (N = 214). The pooled effect size for r was .17 (95% CI = .06, .28, z = 3.02, p = .0025; for forest plot, see Figure 6). Heterogeneity estimates indicated that there was no significant variability between studies (Q = 2.28, df = 4, p = .6841; I 2 = 0%). A funnel plot suggested that there were two missing studies from the meta-analysis. Kendall’s tau = −.1054, p = .8005, indicating no significant asymmetry.
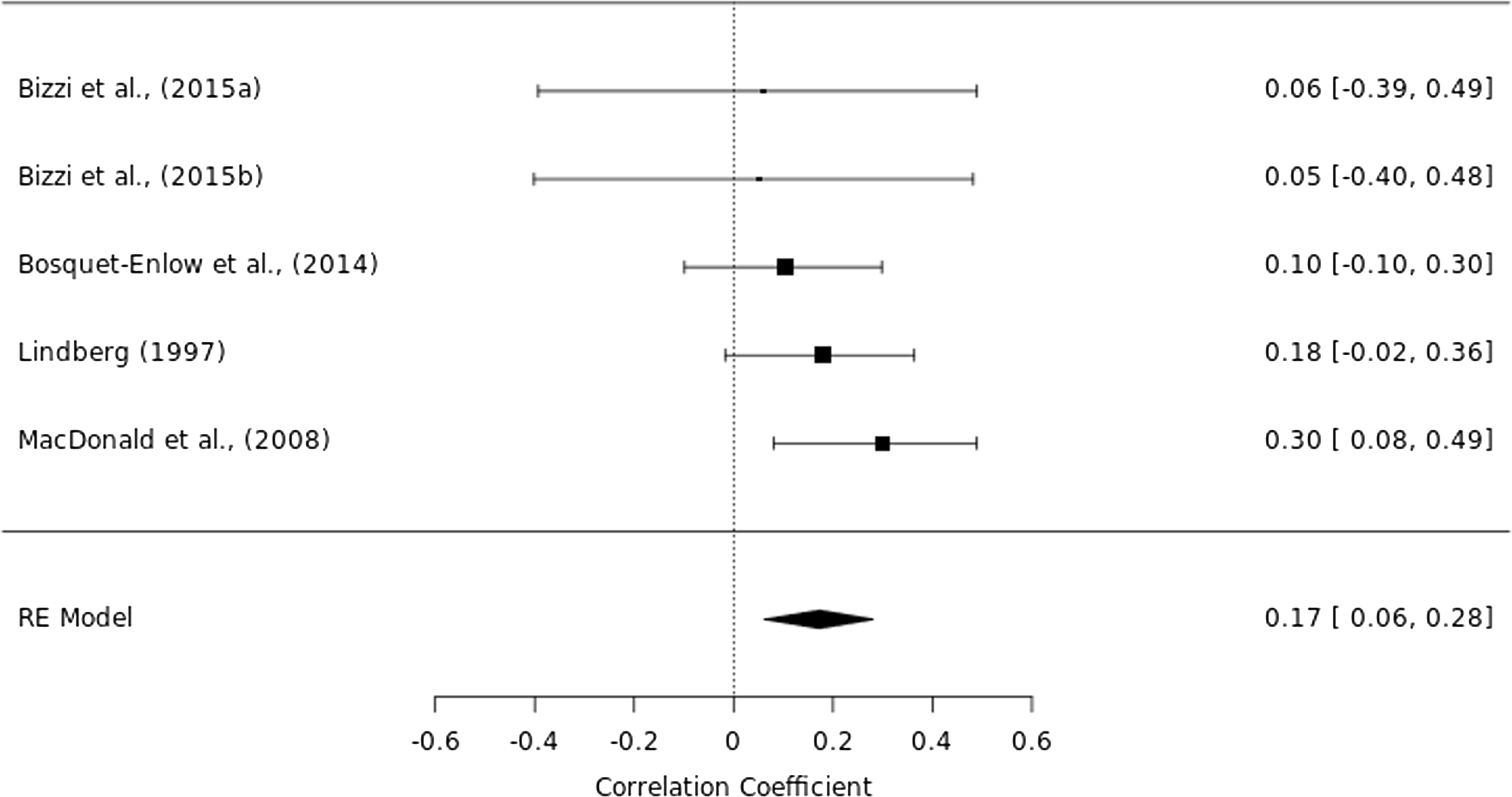
Figure 6. Forest plot for studies reporting the relationship between disorganized attachment and PTSS.
Sensitivity analyses
Sensitivity analyses were undertaken to examine whether differences in methodology applied to individual studies impacted the overall results. Results of all sensitivity analyses are reported in Table 4. Sensitivity analyses for the secure attachment meta-analysis indicate that when studies using a proxy measure of attachment were removed, the strength of the relationship between secure attachment and reduced PTSS increased. When studies using a prospective design and studies using measures from the social tradition of attachment were analyzed separately, the relationship between attachment and PTSS became nonsignificant, which was likely due to a loss of statistical power due to a limited number of studies in these meta-analyses. Sensitivity analyses for the insecure attachment meta-analyses demonstrated that the removal of studies where effect sizes were derived from Odds Ratio statistics and studies which used a proxy measure of attachment did not change the overall effect size. The inclusion of father ratings in the secure and disorganized attachment meta-analyses did not change the overall effect size.
Table 4. Summary of sensitivity analyses

Note. OR = Odds Ratio (studies reporting Odds Ratio statistic removed). CS = Cross-Sectional studies only. P = Prospective studies only. AM = Attachment Measure (proxy attachment measures removed). TT-S = Social Theoretical Tradition only. TT-D = Developmental Theoretical Tradition only. FR = Father Ratings included. l.CI refers to the lower limit of the 95% confidence interval; u.CI refers to the upper limit of the 95% confidence interval.
Discussion
Summary of findings
Thirty articles were included in this review. The five meta-analyses undertaken demonstrated: i) a negative correlation between secure attachment and PTSS (r = −.16), ii) a positive correlation between insecure attachment and PTSS (r = .20), iii) a positive correlation between avoidant attachment and PTSS (r = .20), and iv) a positive correlation between anxious attachment (r = .32) and PTSS (r = .17), and v) a positive correlation between disorganized attachment and PTSS (r = .17). All correlations were statistically significant, but also involved significant heterogeneity, with the exception of the estimate for disorganized attachment.
The overall effect size estimate for the relationship between avoidant attachment and anxious attachment and PTSS was comparable to findings by a previous meta-analytic review with adults (Woodhouse et al., Reference Woodhouse, Ayers and Field2015). Previous research examining the relationship between avoidant attachment and PTSS has revealed somewhat mixed findings (Fraley et al., Reference Fraley, Fazzari, Bonanno and Dekel2006); the current findings clarify the strength of this relationship in child and adolescent populations. The current findings indicate that the relationship between anxious attachment and PTSS was stronger than the relationship between avoidant attachment and PTSS. When reporting on associations between attachment classification and PTSS within the child literature, studies do not consistently assess the full range of attachment classifications; this appears to be in part due to studies using a range of attachment measures which draw on both social and developmental theoretical traditions.
Moderator analyses examining whether exposure to maltreatment strengthened the relationship between attachment and PTSS were limited by the number of available studies. Our findings indicate that exposure to maltreatment did not moderate the relationship between secure attachment and PTSS, which was contrary to our hypotheses. This evidence, while only preliminary, suggests the protective effect of secure attachment on PTSS (or the negative impact of PTSS on secure attachment) is unlikely to differ for maltreatment as compared to other trauma types. However, given that the overall relationship was small, it may be very inherently difficult to identify any variables that moderate this relationship, that is, a large number of studies may be required. Our findings did indicate that exposure to maltreatment did strengthen the relationship between insecure attachment and PTSS. It is important to acknowledge that only six studies reported maltreatment in the study sample, and four studies did not report the type of trauma exposure, therefore this review was not well-equipped to draw meaningful conclusions about the moderating effects of maltreatment. Moderating effects of exposure to maltreatment on the relationship between attachment and PTSS should be viewed within the context of these limitations.
The current findings indicate that the relationship between disorganized attachment and PTSS was significant but small, indeed smaller than other insecure attachment subtypes. This is somewhat at odds with findings reported in similar reviews (Woodhouse et al., Reference Woodhouse, Ayers and Field2015; Barazzone et al., Reference Barazzone, Santos, McGowan and Donaghay-Spire2019). Only five studies were found to have addressed this question. It is possible that this could be explained by different ways of measuring disorganized attachment in childhood and fearful attachment in adulthood. Disorganized attachment in infancy and fearful attachment in adults have been treated by social psychologists as the same construct, but by developmental psychologists as different constructs. While our findings do not support a strong role for disorganized attachment in the onset or maintenance of PTSD, it is noteworthy that all studies included here comprised older children and adolescents rather than infants/pre-schoolers; it is in this age group that a role for disorganized attachment in the recovery from trauma has been particularly mooted (e.g., Lieberman, Reference Lieberman2004). It is important to highlight that only five studies were eligible to be included in this meta-analysis, and these studies had notably smaller sample sizes than other studies included in the review. Studies employed a range of methodology, with three studies using a cross-sectional design and two studies using a prospective design.
Overall effect size estimates of the relationship between secure attachment and PTSS were smaller in the child population in comparison to the adult population, with reported effect sizes being r = −.16 in the child and adolescent populations reviewed here, and
![]() $$\hat \rho $$
= −.27 in the adult population (e.g., Woodhouse et al., Reference Woodhouse, Ayers and Field2015). This finding indicates that secure attachment may be less protective for children in the development of PTSS in comparison to adults. However, this finding should be treated tentatively given the small number of studies present within the meta-analysis.
$$\hat \rho $$
= −.27 in the adult population (e.g., Woodhouse et al., Reference Woodhouse, Ayers and Field2015). This finding indicates that secure attachment may be less protective for children in the development of PTSS in comparison to adults. However, this finding should be treated tentatively given the small number of studies present within the meta-analysis.
Implications for clinical practice and research
Results indicate a small effect size in the relationship between insecure attachment and PTSS and a small effect size in the relationship between secure attachment and PTSS. While the literature surveyed here speaks a role for attachment in the etiology of PTSD, this role is not large. Future research needs to consider, in keeping with some of the insights provided by social-cognitive and social models of PTSD (e.g., Sharp et al., Reference Sharp, Fonagy and Allen2012; Woodhouse et al., Reference Woodhouse, Brown and Ayers2018), how the impact of attachment might be integrated with broader models of PTSD (such as cognitive or cognitive-behavioural accounts; Cohen & Mannarino, Reference Cohen and Mannarino2008; Ehlers & Clark, Reference Ehlers and Clark2000; Foa et al., Reference Foa, Johnson, Treadwell and Kimberli2001; Meiser-Stedman, Reference Meiser-Stedman2002) to further understand the etiology of PTSD in children and adolescents
The current meta-analyses highlight that most studies examining the relationship between attachment and PTSS in children and adolescents use a cross-sectional design with attachment orientation and PTSS being assessed at a single point in time. Only three studies conducted a measure of attachment during infancy, prior to the occurrence of a traumatic event. Disorganized attachment – which some scholars have particularly stressed as being important in the development of PTSD and other trauma-related psychopathology – has received little attention, with only five studies found to have addressed this form of attachment. Studies assessing attachment prior to the exposure to a traumatic event are necessary because previous research indicates that exposure to stressful life experiences (Hamilton, Reference Hamilton2000; Weinfield et al., Reference Weinfield, Sroufe and Egeland2000), and traumatic life events (Murphy et al., Reference Murphy, Elklit, Hyland and Shevlin2016; Solomon et al., Reference Solomon, Dekel and Mikulincer2008) can lead to changes in attachment style. Further, attachment can change over time (Ammaniti et al., Reference Ammaniti, van IJzendoorn, Speranza and Tambelli2000). This makes the interpretation of cross-sectional data more difficult. Understanding the direction of these relationships is an important next step.
Strengths and limitations
This meta-analysis has several important strengths. Studies were selected following a comprehensive literature review which included gray literature to reduce the risk of bias. Study quality was assessed independently by two raters with high inter-rater reliability. The current meta-analysis addressed a gap in the literature by providing a quantitative synthesis of the relationship between attachment and PTSS within the child and adolescent literature.
Despite these strengths, the findings of this meta-analysis should be considered in the context of its limitations. This meta-analysis focused on mostly cross-sectional relationships, and it was not possible to draw conclusions about causality of the relationship between attachment and PTSS. Previous research demonstrates that the relationship between attachment and PTSS is moderated by social cognition (Venta et al., Reference Venta, Hatkevich, Mellick, Vanwoerden and Sharp2017), mentalization (Ferrajao et al., Reference Ferrajao, Badoud and Oliviera2017), social support (Besser & Neria, Reference Besser and Neria2012) and negative view of self (Muller et al., Reference Muller, Sicoli and Lemieux2000), with the majority of these studies conducted with adult samples. The picture of attachment, trauma exposure and PTSS is a complex one and is in need of closer examination. Future research should examine causality and test hypotheses proposed by models which incorporate attachment security in the development of PTSS. A further limitation is that the studies included in the meta-analysis included measures of attachment from both social and developmental traditions, and these traditions correlate weakly. Only the social tradition, and not the developmental tradition, has shown a positive association with internalizing symptoms in adolescents and adults, which is strongly associated with PTSS (Dagan & Bernard, Reference Dagan and Bernard2021). The findings of this meta-analysis demonstrate that only measures based on the developmental theoretical tradition showed a negative association between secure attachment and PTSS, and not measures based on the social theoretical tradition.
A noteworthy finding of the review was that there was a small number of studies included in the meta-analysis and there was a large degree of heterogeneity in three of the meta-analyses undertaken. Heterogeneity improved when sensitivity analyses were conducted, which means the high heterogeneity in the current analyses could be explained by the types of attachment measures used, and the use of different types of effect sizes. Whilst high heterogeneity can in part be explained by these factors, the small number of studies and high heterogeneity in the meta-analyses demonstrate that further research is required in this area to strengthen our confidence in the results. Finally, exposure to multiple traumatic events was not controlled for in individual studies, which can be viewed as a source of bias in the current review.
Summary and conclusion
The results of these meta-analyses indicate that attachment orientation during childhood and adolescence has a small but significant association with PTSS. Secure attachment is associated with lower PTSS following a traumatic event and insecure and avoidant attachment is associated with increased PTSS following a traumatic event, but the evidence base is still quite limited.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579423000299
Acknowledgements
Systematic searches were completed by TC, SR, and RMS. Article screening and selection was completed by TC, SR, JM, and NM. Data extraction was completed by TC and SR. Quality checks were completed by TC and MJC.
Funding statement
Work on this paper by Robbie Duschinsky was supported by a Medical Humanities Investigator Award from the Wellcome Trust (Grant WT103343MA). Toby Cushing was a Trainee Clinical Psychologist on a Health Education England-funded training program.
Competing interests
None.













