On September 20, 2017, category 4 Hurricane Maria made landfall in Puerto Rico. Reference Santos-Burgoa, Sandberg and Suárez1 The island’s already fragile power grid was devastated, initially leaving all 3.4 million US citizens without electricity with only 50% of all consumers having electricity restored approximately 3 mo later. Reference Keerthisinghe, Ahumada-Paras and Pozzo2 The lack of power in rural areas was significantly higher. For example, the mayor of Jayuya, a rural municipality in the center of the island, reported 55% of customers without power at the beginning of March 2018. 3 Jayuya reported one of the largest numbers of excess deaths following Maria. Reference Robles, Davis and Fink4
Although early official reports indicated 64 deaths due to Hurricane Maria, a study subsequently commissioned by the Government of Puerto Rico estimated the death toll to be 2975, while other estimates were as high as 4645. Reference Santos-Burgoa, Sandberg and Suárez1 It was also reported that deaths due to diabetes (+31%), breathing disorders (+43%), sepsis (+47%), and pneumonia (+45%) increased. Reference Robles, Davis and Fink4
The US Department of Health and Human Services has established a database (emPOWER) for use by first responders and communities to better prepare for and respond to disasters. 5 The emPOWER database tracks individuals served by Medicare who use the following types of electricity-dependent medical devices: ventilator, bilevel or continuous positive airway pressure [CPAP] machines, internal feeding, IV infusion pump, suction pump, at-home dialysis, electric wheelchair, electric bed equipment, oxygen concentrator, or implanted cardiac devices. emPOWER indicated that individuals who are medically dependent on electricity represent 4.67% of US, 4.69% of Puerto Rican, and 3.81% of Jayuya Medicare beneficiaries. Santos-Burgoa and colleagues found that individuals 65 and older and individuals from lower socioeconomic regions of Puerto Rico were at higher risk of mortality even 6 mo after Maria. Reference Santos-Burgoa, Sandberg and Suárez1 A significant fraction of the Medicare population is threatened by power interruptions. When these take place in rural locations with poor access to medical facilities, the risks are further increased.
To counter this increased health risk, we developed and distributed rooftop solar-powered battery systems to selected rural residents of Puerto Rico. Then we assessed the degree to which these devices were accepted, successfully used, and positively perceived to inform public health policy.
Methods
The project team, consisting of engineering and public health faculty and students at the University of Washington, visited Puerto Rico in November 2017, March 2018, and July 2018. The University of Washington Human Subjects Division determined the project is human subjects research qualifying for exempt status.
November 20-24, 2017
During this fact-finding trip, we met with Jayuya’s mayor, director of the water authority, clinicians at the central clinic, directors of assisted and nonassisted living health facilities, and other community leaders to determine how Maria had affected the community. Four solar-powered battery systems were installed in homes, and 14 family members were informally interviewed to inform the preparation of more complete installations and design topic guides for interviews during subsequent visits.
March 17-23, 2018
In preparation for selecting families to receive solar powered battery systems, we developed semi-structured topic guides. The questions included open-ended prompts related to how the extended lack of power affected the family, current use of a generator, and perception of solar-powered battery systems. We followed a purposive sampling strategy. We first consulted with local community leaders and jointly selected rural areas of Jayuya which were less likely to have power from the grid. With help from local clinicians (doctors, community health nurses, social workers), we identified within these rural areas 25 families who used electrically powered medical devices.
Fluent Spanish speakers from the team were trained to conduct interviews. Two interviewers were present at each interview, 1 asking the questions and the other taking verbatim notes. They interviewed the 25 families for a baseline assessment of need for and appropriateness of a solar powered battery system to power their medical device. Within each family, all adults who were interested were interviewed. Interviewers used the topic guide questions to lead a conversation with the participants, probing for additional relevant information based on their responses. All interviews were conducted in Spanish and were audio-recorded with approval from the participants.
Following these interviews, 17 families were selected to receive a solar-powered battery system based upon lack of access to a functioning grid or solar power, use by at least 1 family member of a medical device dependent upon electricity, and willingness to try a solar-powered battery system. The systems (100-400 W) were installed within a day or 2 of the interviews. A more complete description and photo of the solar-powered battery systems is presented by Keerthisinghe and colleagues. Reference Keerthisinghe, Ahumada-Paras and Pozzo2
July 1-6, 2018
We were able to conduct at-home follow-up interviews with 15 of the 17 families that received solar-powered battery systems. Families that were not interviewed had either relocated to the continental United States or received a faulty system that was replaced but shortly became unnecessary because power was restored. Topic guides with open-ended questions were used to assess actual use of solar-powered battery systems (medical conditions addressed, devices powered, hours of use); problems encountered with solar-powered battery systems (nature of breakdowns, clarity of instructions, adequate skills, sources of help); and perceptions of solar-powered battery systems (pros and cons of solar versus generators, cost, satisfaction of needs, willingness to pay for solar, overall satisfaction).
Audio recordings of all interviews, conducted in Spanish, were transcribed verbatim, and translated into English. The family was the unit of analysis. The English transcripts were coded by hand and responses grouped by topic and family to form a matrix. Two members of the research team, an engineering graduate student and a public health faculty member, independently selected key statements from each topic that were formed into code-like sentences. The coded responses were analyzed to generate brief summary narratives. Where appropriate, content analysis was used to summarize topics, such as medical conditions faced by the family, medical devises needing electric power, and problems encountered with solar-powered battery systems.
Results
March 2018 Interviews
All families receiving a solar-powered battery system in March had not received power from the grid since Maria struck in September 2017, and 12 reported the use of a generator. The mean and median reported cost of generator fuel per week were $81.70 and $52.50, respectively. When asked how the lack of power affected family members’ health, the responses were: limited ability to store meat, fruits, and vegetables (N = 8); eating more canned food (N = 5); need to refrigerate medications (N = 3); depression (N = 3); lack of electricity for inflatable mattress to prevent bedsores (N = 2); higher sodium intake (N = 2); Parkinson patient needing to avoid heat (N = 1); limited use of oxygen for chronic obstructive pulmonary disease (N = 1); and need to drive to town for asthma treatments (N = 1). Most of the recipients had heard about solar panels for the home. Their estimated cost of solar-powered battery systems ranged from $4,000 to $15,000. All indicated that they had not considered installing a system because it was too expensive.
July 2018 Interviews
The 15 families who received solar-powered battery system reported the following medical conditions: bedridden (N = 6), asthma (N = 4), diabetes (N = 3), apnea (N = 2), cancer (N = 2), and 1 each for liver transplant, osteoporosis, Alzheimer disease, heart surgery, and Parkinson disease. Table 1 presents how the systems were used by families. The systems were used a median of 8 h per day with a range of 3 to “10 or more hours.”
Table 1. How solar-powered battery systems were used

Twelve families reported the following problems with their solar-powered battery systems: low power (N = 4), defective cable (N = 2), blown fuse (N = 2), stopped working (N = 2), and 1 each for: moved panels for better sun, panel flipped from wind, inverter not working, inverter got hot and made noise, and inability to power refrigerator. When problems were encountered, 4 families relied on other family members, 3 called the study team, and 2 called a neighbor for help.
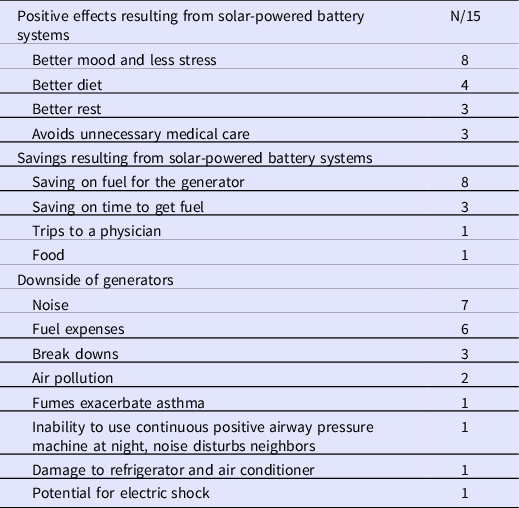
Table 2 presents the reported positive aspects of solar-powered battery systems and negative aspects of generators. The most frequently reported positive aspects of solar-powered battery systems were better mood and less stress, better diet, and savings in fuel costs. The most frequently reported downsides of generators were noise and fuel expenses.
Table 2. Benefits of solar-powered battery systems and downsides of generators as reported by families
After being told that their solar-powered battery system cost between $500 and $1500, 8 families indicated they would recommend them to a neighbor. Three families indicated that they were unsure about investing in solar and three families were positive about solar but indicated that expense was an issue. One family expanded their system, adding 8 batteries and 6 panels.
Discussion
We interviewed 25 families who used electrically powered medical devices and distributed rooftop solar-powered battery systems to 17 families predominantly in rural sections of Jayuya but also San Lorenzo, Puerto Rico, in March 2018, approximately 6 mo after Hurricane Maria struck Puerto Rico. All recipients had been without power from the grid since Maria, resulting in multiple self-reported health-related issues: disruption of a healthy diet, difficulty in refrigerating medications, depression, and inability to use inflatable mattresses to avoid bed sores or CPAP machines for sleep apnea. Twelve of the families were previously using generators and reported several shortcomings: a median cost of fuel of $52.50/wk; noise from the generator in general; noise that disturbed neighbors and made it difficult to use the generator at night for a CPAP machine; air pollution; and fumes that worsened asthma symptoms.
Our follow-up interview, in July 2018, indicated that almost all the families successfully used and were quite pleased with the solar-powered battery systems. The families experienced problems with the systems, but in most cases, despite little or no experience with these systems, were able to resolve the issues through help from a family member, neighbor, or the project team. In any future implementation of solar-powered battery systems during power outages, robust support needs to be available to help with problems that arise.
During the March interviews, most families indicated that they were aware of solar-powered battery systems with estimated costs varying from $4000 to $15,000. All who responded said they could not afford such a system. They were probably thinking of systems that were considerably larger than the ones they received. During the follow-up interview in July, they were told that the systems they received cost between $500 and $1500. Eight families indicated that the price range seemed reasonable, 3 were unsure, and 3 families indicated that the expense would be an issue. Targeted education regarding the benefits, feasibility, and cost of these systems is warranted. In addition, some families may need financial support to purchase solar-powered battery systems.
Keerthisinghe and colleagues estimate that around 66 days of total use would offset the purchase of a solar-powered battery system relative to a generator. Reference Keerthisinghe, Ahumada-Paras and Pozzo2 While the lack of power from the grid in Puerto Rico lasted considerably longer than 66 days following Hurricane Maria, other recent catastrophic hurricanes resulted in shorter blackouts. Reference Riddell6 However, investing in solar-powered battery systems by individual families or emergency relief organizations in regions that are subject to repeated hurricanes, other disasters, or intermittent blackouts could well be worthwhile.
Our findings leave several unanswered questions when put in the context of public health emergency management. Reference Rose, Murthy and Brooks7,Reference Rodríguez-Díaz8 What medical conditions and medical devices should have the highest priority for installing solar-powered battery systems? How does the optimal size of a system depend upon the user’s medical needs? Which at-risk regions (eg, hurricane prone), locations (eg, rural), and individuals (eg, low income) should have the highest priority for the use of such systems? Would it be advantageous for insurers, especially Medicare and Medicaid, that serve the most individuals with relevant devices, to finance the purchase of such systems? Reference Vestal9 Should the end consumer be responsible for acquiring and installing the system or would it be better to have the Strategic National Stockpile, Federal Emergency Management Agency, and Community Based Organizations, such as local clinics or first responders, house and then distribute the systems just before or after a disaster? Should the end users be asked to return the system after power has been restored?
Conclusions
The use of solar-powered battery systems by individuals using electricity-dependent medical devices can be part of public health emergency management and may well be helpful in reducing mortality following disasters such as Maria.
Acknowledgments
We thank the members of the Puerto Rico Solar Health Study Group: Charbel El Bcheraoui, PhD, Head, Evidence-Based Public Health, Center for International Health Protection at Robert Koch Institute, Berlin Germany; Institute for Health Metrics and Evaluation, University of Washington, Seattle WA, charbelbcheraoui@yahoo.com. Lauren Kang, PhD, Department of Chemistry, University of Washington, Seattle WA, lkang87@gmail.com. Chanaka Keerthisinghe, PhD, Research Fellow, Clean Energy Institute, University of Washington, Seattle WA, chanakak@ieee.org. Yohan Min MS, Graduate Student, College of Built Environments, University of Washington, Seattle WA, min25@uw.edu. Erin B Palmisano, MPH, Senior Research Manager, Institute for Health Metrics and Evaluation, University of Washington, Seattle WA, erinbpalmisano@gmail.com. Chester Pham, BS, Department of Chemical Engineering, University of Washington, Seattle WA, chesterp@uw.edu. Hugo F. Pontes, BA BS, Departments of Chemical Engineering and Biochemistry, University of Washington, Seattle WA, hpontes@uw.edu. Anya Raj, BS, Research Assistant, Department of Chemical Engineering, University of Washington, Seattle WA, anyaraj17@gmail.com. Wesley Tatum, PhD, Department of Materials Science and Engineering, University of Washington, Seattle WA, wesleyktatum@gmail.com.
Funding statement
Travel funds were provided by the University of Washington Clean Energy Institute, the Office of Global Affairs’ Global Innovation Fund, and personal funds from individuals traveling. The solar-powered battery systems installed in March 2018 were purchased with support from the Clean Energy Group’s Resilient Power Project, as well as numerous individual donors.




