Disasters are defined by the World Health Organization (WHO) as disruptions to a community that exceed its capacity to adjust. 1 Mass casualty incidents (MCIs), also referred to as major incidents in some context, are disasters in which the number and severity of casualties overwhelm the abilities of the local health-care system. 1–Reference Ahmad3 The heterogeneity of MCIs ranges from natural hazards to manmade events such as infrastructure failures, terrorism, and civil disorder, among many others. Reference Lomaglio, Ansaloni and Catena4 MCIs can result from abrupt events, such as in the case of a gas leak explosion, or occur over a more protracted course, when patients arrive more gradually over the course of several hours or even days. Both situations may lead to overwhelmed emergency medical response systems. Reference De Silva and Kawasaki5
The ever-present threat of MCIs has led to the global prioritization of disaster risk reduction (DRR), especially as urbanization has increased globally. Reference Abdul6 Densely populated cities are at increased risk of MCIs tied to environmental, socioeconomic, and security factors. The United Nations’ Office for Disaster Risk Reduction (UNDRR) has urged the development and implementation of transdisciplinary, multi-hazard system-based approaches toward addressing MCIs in metropolitan areas, given the complex and dynamic nature of urban risk, coupled with unplanned population growth in low- and middle-income countries (LMICs). Reference Valdes and Purcell7–Reference Aitsi-Selmi, Egawa and Sasaki9 Critical to the implementation of these recommendations is the capacity of regional emergency medical response systems, which are responsible for delivering life-saving medical care during any MCI. 10 Emergency medical response systems tend to be complex, requiring coordination between community members, health-care service providers, government agencies, media, and law enforcement, integrating different domains. Reference Smiley, Loboda and Starling11,Reference Lee, Booth and Challen12 Furthermore, response systems in LMICs, which are typically less centralized, make assessment of the system as a whole especially difficult. Understanding components of emergency medical response systems based upon measures of effectiveness is necessary to assess preparedness for MCIs. Accordingly, the study team sought to answer the question: What are the essential components of an emergency medical response system in the immediate aftermath of an MCI?
Methods
As a guiding strategy, we focused on manmade MCIs, excluding events that did not leave an intact health system, given the disproportionately increasing number of manmade MCIs in LMICs. Reference Nekoie-Moghadam, Kurland and Moosazadeh13–15
Search Strategy and Databases
A search strategy for peer-reviewed sources was developed in collaboration with a university informationist and modified for different databases. English language articles highlighting emergency response components, and relevant assessments, were identified through structured searches of PubMed, Embase, Global Health, and Scopus spanning a 20-year period from 2000 to 2020. Combinations of search terms, including medical subject headings and keywords, were organized in 3 groups: (1) mass casualty and emergency disasters; (2) response, preparedness, and planning; (3) instruments, measurements, evaluations, and assessments. Human subjects, year, and language restrictions were applied. The detailed search strategy adapted for each electronic database are included in the Supplementary Text S1. The “similar articles” section of the PubMed website and reference lists of the identified articles were also examined to capture other potentially relevant articles. All references were exported to Covidence (Melbourne, Australia) and duplicate studies were excluded. 16 This review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) format (Figure 1).

Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Diagram.
Inclusion and Exclusion Criteria
Articles included in this review encompassed peer-reviewed English language studies, guidelines, tools, and instruments focused on outlining essential components and measures for evaluation of MCI response at the prehospital, hospital, city, and national levels. The inclusion criteria for citations were intentionally broad, capturing scientific publications, committee reports, evaluations, tools, organizational and governmental guidelines, and emergency preparedness plans and exercises. For the purposes of this review, MCIs that compromised the structural integrity of an emergency medical system or disrupted the ability to deliver emergency care through workforce attrition were not considered. Accordingly, large-scale public health emergencies, infectious outbreaks, and complex protracted humanitarian emergencies were excluded. Articles without full text available in English language were excluded from further analysis. Criteria of eligible studies are outlined in Table 1.
Table 1. Inclusion and exclusion criteria

Data Abstraction
Seven team members (A.U., A.M., S.R., A.E., A.A., O.A., and J.D.) independently screened the titles and abstracts of all retrieved studies to identify the relevant studies according to the eligibility criteria, with each title and abstract screened by 2 separate reviewers. Conflicts were resolved by consensus among the reviewers during weekly research meetings, while remaining unsettled votes were arbitrated by the lead author (A.U.). After title and abstract screening, the studies underwent full-text review by the same independent reviewers. Studies were evaluated by the type of study, location, year of publication, key response components addressed, and methods of evaluation. Data extraction was performed using a data extraction sheet developed by 2 team members (A.U., A.M.). Included articles were organized by authors’ name and year of publication with an indication of whether the article outlined response activities from a high-income country (HIC) or LMIC. The World Bank classification of countries by income was used to define low-income, lower middle-income, and middle-income countries; this classification is based on gross national income (GNI) per capita. 17
Data Analysis
Thematic analysis was performed by 2 team members (AU and AM) using traditional content analysis to evaluate the full text of each included article. Reference Hsieh and Shannon18 Emerging themes pertaining to the essential components and evaluation of emergency medical response systems were included. Domains or components of emergency medical responses most frequently mentioned and discussed within the included studies were designated as essential. Included studies were characterized according to the essential components explored (Supplementary Table S2), with quality assessment of the articles conducted with guidance from the Institute of Medicine Standards for Systematic Reviews. Reference Eden, Levit and Berg19
Results
Of 20,456 screened citations, 181 articles were included in the qualitative analyses (Figure 1). A large number of studies were observational and approximately a third of all articles included reports and resource documents as shown in Table 2. Most of the included studies, 165 of the 181, were in HIC contexts (Figure 2). Seven major themes emerged from the content analysis as essential domains of an emergency medical response system: (1) communication; (2) safety and security; (3) human resources; (4) planning, policy, and procedures; (5) command, control, and coordination of the disaster response; (6) care delivery; and (7) health finance for disaster planning and response. Additionally, 40 sub-themes were found to support the essential components of an MCI response as shown in Table 3. A large number of publications focused on care delivery (67%), leadership and coordination (30%), communications (23%), and human resources (19%). Safety and security, as well as planning, policy, and procedures to execute response and assist recovery were also important domains identified in the literature. Each identified essential component and subcomponent of an emergency medical response system is italicized.
Table 2. Study design of included articles (n = 181)

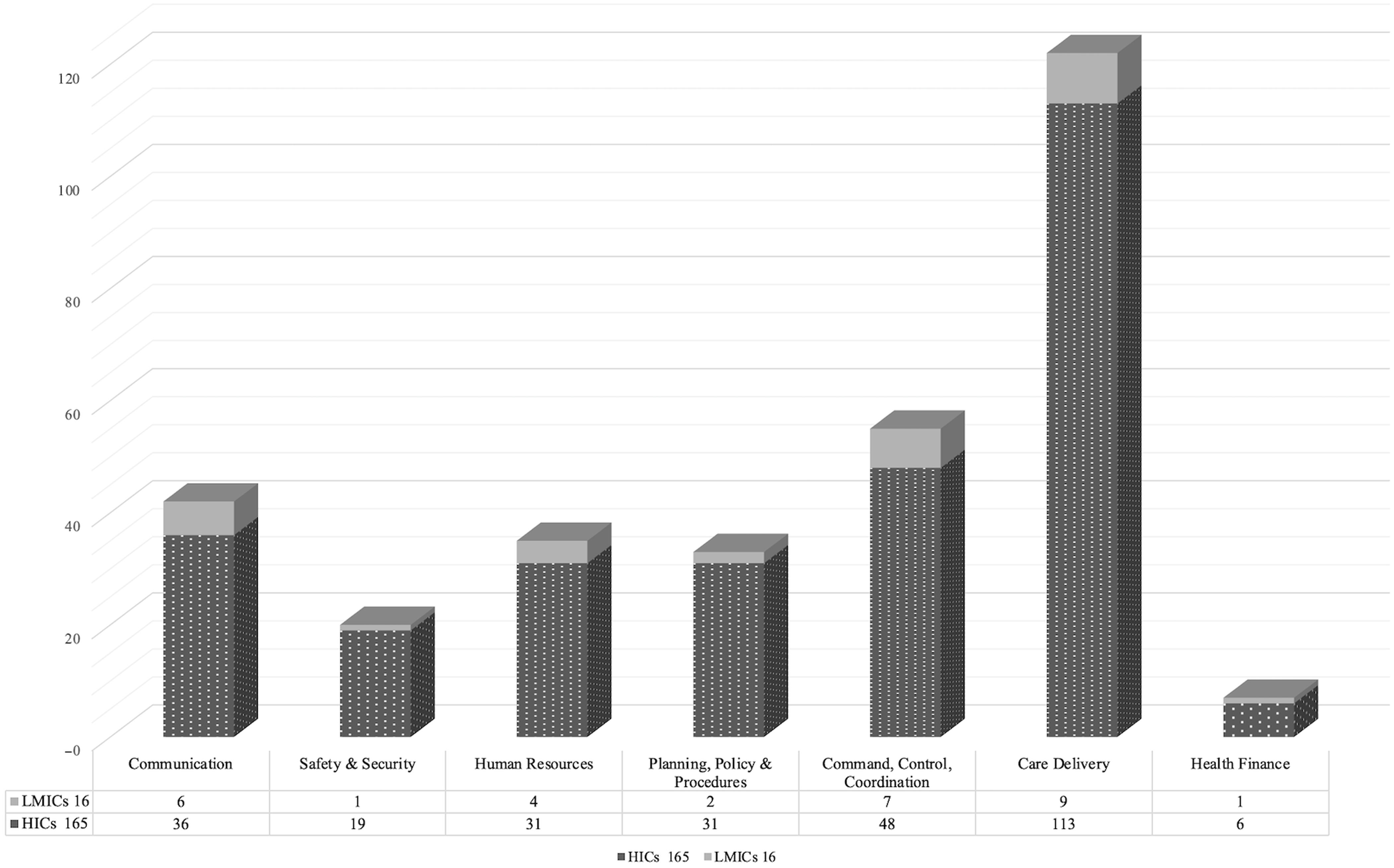
Figure 2. Comparison of included studies from HICs versus LMICs.
Table 3. Essential components and sub-components of an emergency medical response

What Are the Essential Components of an Emergency Medical Response System in the Immediate Aftermath of an MCI?
Communication
Communication is an indispensable component of a coordinated MCI response. Effective communication during an MCI requires using modern communication devices with adequate backup, or redundant systems (eg, radio, satellites, geographic positioning systems), or other innovative technology to enable real-time situational awareness and information sharing. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adelaine, Shoaf and Harvey20–Reference Zafar, Jawad and Shamim62 The evolving role of social media such as live Twitter feeds, Facebook updates, text messages, and chat rooms has been explored for their ability to contribute to situational awareness, communication with the victims and their loved ones, and information sharing among the media, key stakeholders, and frontline providers. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adelaine, Shoaf and Harvey20,Reference Aten, Leavell and Gonzalez24,Reference Biddinger, Cadigan and Auerbach28,Reference Biddinger, Reisman and Seger29,Reference Bradt31,Reference Brands, Hernandez and Stenberg32,Reference Callaway, Peabody and Hoffman35,Reference Cha, Kim and Kim36,Reference El Sayed, Chami and Hitti39–Reference Giacobe and Soule42,Reference Hick, Koenig and Barbisch46,Reference Juffermans and Bierens50,Reference Kearns, Skarote and Peterson51,Reference Moser, Connelly and Baker55,Reference Stander, Wallis and Smith59–Reference Wurmb, Schorscher and Justice61,Reference Farmer, Stoerger and Vyavahare63–Reference Wachira, Abdalla and Wallis66 Pre-determined contacts for designated personnel, collaborating entities and other agencies, improves efficiency and the flow of information. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adelaine, Shoaf and Harvey20,Reference Adini, Bodas and Nilsson21,Reference Homier, Hamad and Larocque48,Reference Hsu, Jenckes and Catlett49,Reference Stander, Wallis and Smith59,Reference Avidan, Hersch and Spira67–Reference Lynn, Gurr and Memon74 Standard and ad-hoc channels of communication help provide situational awareness, clarify misinformation, address concerns, and facilitate response activities. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adelaine, Shoaf and Harvey20–Reference Almogy and Rivkind23,Reference Balasegaram, Kar-Purkayastha and Bussell25,Reference Bernardo and Veenema26,Reference Broeze, Falder and Rea33,Reference El Sayed, Chami and Hitti39,Reference Gotham, Sottolano and Hennessy44–Reference Hick, Koenig and Barbisch46,Reference Moser, Connelly and Baker55,Reference Wild, Maher and Frazee60,Reference Avidan, Hersch and Spira67,Reference Lynn, Gurr and Memon74–Reference Currie and Heslop77
Safety and Security
Safety and security must always be prioritized with any MCI, recognizing that some incidents, such as terror attacks or chemical hazards, require containment and pose a greater security threat than others. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Brands, Hernandez and Stenberg32,Reference Bukowski34,Reference Crawford, Mackway-Jones and Russell37,Reference El Sayed, Chami and Hitti39,Reference Holgersson47,Reference Little, Cooper and Gope54,Reference Stander, Wallis and Smith59,Reference Zafar, Jawad and Shamim62,Reference Albanese, Burich and Smith75,Reference Currie and Heslop77–Reference Weyand, Junck and Kang92 Moreover, security officials maintain the law and order at the scene and at the hospitals receiving injured patients, controlling access points, and restricting it to only authorized personnel, monitoring for suspicious activities, and preventing crowds from interfering with emergency operations. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Brands, Hernandez and Stenberg32,Reference Bukowski34,Reference El Sayed, Chami and Hitti39,Reference Gabbe, Veitch and Curtis40,Reference Holgersson47,Reference Hsu, Jenckes and Catlett49,Reference Stander, Wallis and Smith59,Reference Zafar, Jawad and Shamim62,Reference Jenckes, Catlett and Hsu73,Reference Autrey, Hick and Bramer81,Reference Golabek-Goldman87,Reference Brooke Lerner, O’Connor and Schwartz91–Reference Seaton, Maier and Sachdeva94 Deploying a safety officer to identify potential threats and implement appropriate safety procedures is essential in virtually all MCIs. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Cha, Kim and Kim36,Reference El Sayed, Chami and Hitti39,Reference Holgersson47,Reference O’Neill56,Reference Albanese, Burich and Smith75,Reference Autrey, Hick and Bramer81,Reference Liebergall, Braverman and Shapira93 In response to the safety and security challenges adopted in some settings is the introduction of Tactical medicine, in which out-of-hospital care is provided by specially trained practitioners, many with military and/or law enforcement training, who operate in hostile environments. Reference Broeze, Falder and Rea33,Reference Autrey, Hick and Bramer81,Reference Golabek-Goldman87,Reference Jacobs95–Reference Madzimbamuto97
Human Resources
MCI response depends upon adequate and appropriate personnel capacity. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adelaine, Shoaf and Harvey20,Reference Almogy and Rivkind23,Reference Bernardo and Veenema26,Reference Biddinger, Cadigan and Auerbach28,Reference Bradt31,Reference Gabbe, Veitch and Curtis40,Reference Hick, Koenig and Barbisch46,Reference Holgersson47,Reference Little, Cooper and Gope54,Reference Moser, Connelly and Baker55,Reference Avidan, Hersch and Spira67–Reference Berger, Körner and Bernstein69,Reference Lynn, Gurr and Memon74,Reference Autrey, Hick and Bramer81,Reference Baker82,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Brandenburg and Arneson98–Reference Smith, Paturas and Tomassoni104 Human resources are not limited to paramedics, nurses and doctors, but include all who care for patients during an MCI, such as uninjured or mildly injured survivors, bystanders and community volunteers. Reference Almogy and Rivkind23,Reference Broeze, Falder and Rea33,Reference El Sayed, Chami and Hitti39,Reference Zafar, Jawad and Shamim62,Reference Baldwin and Wilson68,Reference Baker82,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Halpern, Tsai and Arnold102,Reference Aliyu105,Reference Ching and Preparation106 Depending upon the extent, location and duration of an MCI, fire, rescue and security services, incident management teams, ambulance and transport crew, hospital ancillary staff, translators, information technology (IT) specialists and engineers, as well as social services—who can assist with emotional trauma and maintain a family information center—should remain engaged and involved in providing acute care. Reference Almogy and Rivkind23,Reference Biddinger, Baggish and Harrington27,Reference Einav, Schecter and Matot38,Reference Ghanchi41,Reference Little, Cooper and Gope54,Reference Baldwin and Wilson68,Reference Lynn, Gurr and Memon74,Reference Autrey, Hick and Bramer81,Reference Baker82,Reference Brandenburg and Arneson98,Reference Ablah, Tinius and Konda107–Reference Deelen, Costermans and Moss113 Some experts outlined core competencies for frontline responders participating in an MCI response. Reference Bloch, Schwartz and Pinkert30,Reference Broeze, Falder and Rea33,Reference Bukowski34,Reference Crawford, Mackway-Jones and Russell37,Reference Savoia, Biddinger and Burstein58,Reference Bulson, Bulson and Vande Guchte84,Reference Higgins, Wainright and Lu89,Reference Brandenburg and Arneson98–Reference Chim, Yew and Song100,Reference Ablah, Tinius and Konda107,Reference Ablah, Molgaard and Fredrickson114–Reference Veenema and Toke125 Enabling factors that enhance core competencies include specific training on the incident command system framework, as well as collaborative exercises and drills to better organize a multidisciplinary and multi-agency response. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Alexander22,Reference Almogy and Rivkind23,Reference Bernardo and Veenema26–Reference Biddinger, Reisman and Seger29,Reference Bukowski34,Reference Cha, Kim and Kim36,Reference Crawford, Mackway-Jones and Russell37,Reference Gabbe, Veitch and Curtis40,Reference Gotham, Sottolano and Hennessy44,Reference Hardy, Fattah and Wisborg45,Reference Hsu, Jenckes and Catlett49,Reference Leahy, Yurt and Lazar53,Reference Little, Cooper and Gope54,Reference O’Neill56,Reference Savoia, Biddinger and Burstein58,Reference Wild, Maher and Frazee60,Reference Jenckes, Catlett and Hsu73,Reference Lynn, Gurr and Memon74,Reference Friedman, Rose and Koskan76,Reference Allen, Parrillo and Will80,Reference Baker82–Reference Bulson, Bulson and Vande Guchte84,Reference Jacobs and Burns96,Reference Burke, Iverson and Goodhue99,Reference Chim, Yew and Song100,Reference Ablah, Tinius and Konda107,Reference Abraham108,Reference Cocco and Thomas-Boaz110,Reference Collignon111,Reference Deelen, Costermans and Moss113,Reference Catlett, Jenkins and Millin118,Reference Gebbie, Peterson and Subbarao121,Reference Seifman, Ek and Menezes124,Reference Janati, Sadeghi-Bazargani and Hasanpoor126,Reference Jenkins, McCarthy and Sauer127 Cultural competency must be kept in mind when responding to any MCI, but especially those predominantly affecting minority populations, children, elderly, low-income, and alternatively abled persons. Reference Bernardo and Veenema26,Reference Gomez, Haas and Ahmed43,Reference Holgersson47,Reference Friedman, Rose and Koskan76,Reference Allen, Parrillo and Will80,Reference Bulson, Bulson and Vande Guchte84,Reference Brandenburg and Arneson98,Reference Burke, Iverson and Goodhue99,Reference Abraham108,Reference Andrulis, Siddiqui and Gantner109 Advance contingency agreements between different organizations, institutions, and jurisdictions for resource and personnel sharing can help in recruiting individuals to deal with a large influx of victims over a short period of time. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adelaine, Shoaf and Harvey20,Reference Bernardo and Veenema26,Reference Biddinger, Baggish and Harrington27,Reference Broeze, Falder and Rea33,Reference Gomez, Haas and Ahmed43,Reference Gotham, Sottolano and Hennessy44,Reference Hick, Koenig and Barbisch46,Reference Holgersson47,Reference Kearns, Skarote and Peterson51,Reference Little, Cooper and Gope54,Reference Lynn, Gurr and Memon74,Reference Golabek-Goldman87,Reference Jacobs and Burns96,Reference Corcoran, Niven and Reese101,Reference Smith, Paturas and Tomassoni104,Reference Cocco and Thomas-Boaz110,Reference Catlett, Jenkins and Millin118,Reference Avitzour, Libergal and Assaf128–Reference Shartar, Moore and Wood130 Keeping an active roster of available volunteers and required staff is often useful in rapidly building surge capacity by ensuring that personnel are both prepared and willing to participate in MCI response activities. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adelaine, Shoaf and Harvey20,Reference Adini, Bodas and Nilsson21,Reference Biddinger, Reisman and Seger29,Reference Broeze, Falder and Rea33,Reference Gabbe, Veitch and Curtis40,Reference Ghanchi41,Reference Hick, Koenig and Barbisch46,Reference Homier, Hamad and Larocque48,Reference Hsu, Jenckes and Catlett49,Reference Baldwin and Wilson68–Reference Lynn, Gurr and Memon74,Reference Corcoran, Niven and Reese101,Reference Smith, Paturas and Tomassoni104,Reference Adams and Melius115,Reference Catlett, Jenkins and Millin118,Reference Devereaux, Christian and Dichter120 Addressing the emotional trauma of the volunteers and staff in the aftermath of an MCI should be considered during an emergency medical response. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adini, Bodas and Nilsson21,Reference Gabbe, Veitch and Curtis40,Reference Ghanchi41,Reference Holgersson47,Reference Baldwin and Wilson68,Reference Albanese, Burich and Smith75,Reference Baker82,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Liebergall, Braverman and Shapira93,Reference Aliyu105,Reference Cocco and Thomas-Boaz110,Reference Catlett, Jenkins and Millin118,Reference Chang, Vacanti and Michaud119,Reference Gebbie, Peterson and Subbarao121,Reference Veenema and Toke125,Reference Biddison, Berkowitz and Courtney131
Planning, Policy, and Procedures
Local planning, policies, and procedures, or a collective MCI plan, provides the framework to activate and deactivate MCI response and guide response activities. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Alexander22,Reference Biddinger, Baggish and Harrington27,Reference Brands, Hernandez and Stenberg32,Reference Broeze, Falder and Rea33,Reference El Sayed, Chami and Hitti39,Reference Gabbe, Veitch and Curtis40,Reference Leahy, Yurt and Lazar53,Reference Moser, Connelly and Baker55,Reference Savoia, Biddinger and Burstein58,Reference Stander, Wallis and Smith59,Reference Berger, Körner and Bernstein69,Reference Farmer and Carlton71,Reference Lynn, Gurr and Memon74,Reference Baker82,Reference Higgins, Wainright and Lu89,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Liebergall, Braverman and Shapira93,Reference Liebergall, Braverman and Shapira93,Reference Seaton, Maier and Sachdeva94,Reference Brandenburg and Arneson98,Reference Cocco and Thomas-Boaz110,Reference Collignon111,Reference Carley, Mackway-Jones and Randic117,Reference Catlett, Jenkins and Millin118,Reference Devereaux, Christian and Dichter120,Reference Al-Shamsi, Moitinho de Almeida and Nyanchoka132–Reference Zoraster, Chidester and Koenig134 Following local standard operating procedures (SOP) and predetermined policies and protocols, next steps include clear role identification, delegation of responsibilities, record-keeping, patient triage, clinical care delivery, resource allocation, maintaining stockpiles of essential equipment and supplies, information flow, victim identification, and routine communication with staff, media and families. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Biddinger, Baggish and Harrington27,Reference Broeze, Falder and Rea33,Reference Bukowski34,Reference El Sayed, Chami and Hitti39,Reference Gabbe, Veitch and Curtis40,Reference Hick, Koenig and Barbisch46,Reference Leahy, Yurt and Lazar53,Reference Savoia, Biddinger and Burstein58,Reference Avidan, Hersch and Spira67,Reference Berger, Körner and Bernstein69,Reference Farmer and Carlton71,Reference Lynn, Gurr and Memon74,Reference Baker82,Reference Higgins, Wainright and Lu89,Reference Liebergall, Braverman and Shapira93,Reference Seaton, Maier and Sachdeva94,Reference Brandenburg and Arneson98,Reference Cocco and Thomas-Boaz110,Reference Collignon111,Reference Carley, Mackway-Jones and Randic117,Reference Catlett, Jenkins and Millin118,Reference Devereaux, Christian and Dichter120,Reference Biddison, Berkowitz and Courtney131–Reference Zoraster, Chidester and Koenig134 When additional health-care personnel are needed, emergency credentialing could be used to facilitate the process, and providing hazard pay and benefits for first responders should be taken into consideration, including provisions providing legal indemnification to providers, support staff, institutions, and other responding agencies. Reference Broeze, Falder and Rea33,Reference El Sayed, Chami and Hitti39,Reference Gabbe, Veitch and Curtis40,Reference Hick, Koenig and Barbisch46,Reference Leahy, Yurt and Lazar53,Reference Baldwin and Wilson68,Reference Jenckes, Catlett and Hsu73,Reference Lynn, Gurr and Memon74,Reference Higgins, Wainright and Lu89,Reference Smith, Paturas and Tomassoni104,Reference Ablah, Tinius and Konda107,Reference Catlett, Jenkins and Millin118,Reference Devereaux, Christian and Dichter120,Reference Gebbie, Peterson and Subbarao121,Reference Veenema and Toke125,Reference Janati, Sadeghi-Bazargani and Hasanpoor126,Reference Shartar, Moore and Wood130,Reference Biddison, Berkowitz and Courtney131,Reference Zhong, Clark and Hou133,135–Reference Tami, Bruria and Fabiana137 Vendor agreements and inventory management policies may shorten the time to deploy essential materials and equipment to ensure their availability. Reference Bernardo and Veenema26,Reference Biddinger, Cadigan and Auerbach28,Reference Gabbe, Veitch and Curtis40,Reference Gomez, Haas and Ahmed43,Reference Hick, Koenig and Barbisch46,Reference Kearns, Skarote and Peterson51,Reference Moser, Connelly and Baker55,Reference Lynn, Gurr and Memon74,Reference Albanese, Burich and Smith75,Reference Baker82,Reference Brandenburg and Arneson98–Reference Chim, Yew and Song100,Reference Hick, Hanfling and Cantrill103,Reference Collignon111,Reference Catlett, Jenkins and Millin118,Reference Devereaux, Christian and Dichter120,Reference Shahrestanaki, Khankeh and Masoumi129,Reference Rebmann, McPhee and Osborne136,Reference Adini, Aharonson-Daniel and Israeli138–Reference Rubinson, Hick and Hanfling140 A post-MCI debriefing should be conducted during which participating organizations report their data and respond to questions fostering a culture of transparency, accountability, and community practice. Reference El Sayed, Chami and Hitti39–Reference Ghanchi41,Reference Berger, Körner and Bernstein69,Reference Baker82,Reference Madzimbamuto97,Reference Cocco and Thomas-Boaz110,Reference Deelen, Costermans and Moss113,Reference Carley, Mackway-Jones and Randic117,Reference Tami, Bruria and Fabiana137,Reference Brunner, Rocha and Chudgar141–Reference Hendrickx, D’Hoker and Michiels143 Periodic assessments of MCI response capabilities and the evaluation of training and preparedness of the responders should be incorporated into the process of ensuring readiness to respond to future MCIs. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Alexander22,Reference Almogy and Rivkind23,Reference Biddinger, Baggish and Harrington27–Reference Biddinger, Reisman and Seger29,Reference Crawford, Mackway-Jones and Russell37,Reference Hardy, Fattah and Wisborg45,Reference O’Neill56,Reference Rimstad and Braut57,Reference Zafar, Jawad and Shamim62,Reference Farmer, Stoerger and Vyavahare63,Reference Berger, Körner and Bernstein69,Reference Faccincani, Della Corte and Sesana70,Reference Lynn, Gurr and Memon74,Reference Currie and Heslop77,Reference Allen, Parrillo and Will80–Reference Baker82,Reference Brandenburg and Arneson98,Reference Burke, Iverson and Goodhue99,Reference Aliyu105,Reference Cocco and Thomas-Boaz110,Reference Collignon111,Reference Seifman, Ek and Menezes124,Reference Janati, Sadeghi-Bazargani and Hasanpoor126,Reference Shahrestanaki, Khankeh and Masoumi129,Reference Esbitt139,Reference Hendrickx, D’Hoker and Michiels143–Reference Thomas, Hsu and Kim149
Command, Control, and Coordination
A central body or lead agency maintains hierarchy, inter-agency response coordination, and mobilizes resources. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adini, Bodas and Nilsson21,Reference Alexander22,Reference Biddinger, Cadigan and Auerbach28,Reference Bradt31,Reference Cha, Kim and Kim36,Reference Hardy, Fattah and Wisborg45,Reference Holgersson47,Reference Juffermans and Bierens50,Reference Moser, Connelly and Baker55–Reference Savoia, Biddinger and Burstein58,Reference Wurmb, Schorscher and Justice61,Reference Zafar, Jawad and Shamim62,Reference Ganz, Schafer and Yang64–Reference Wachira, Abdalla and Wallis66,Reference Jenckes, Catlett and Hsu73,Reference Baker82,Reference Gryth, Rådestad and Nilsson88,Reference Higgins, Wainright and Lu89,Reference Burke, Iverson and Goodhue99,Reference Chim, Yew and Song100,Reference Cocco and Thomas-Boaz110,Reference Collignon111,Reference Catlett, Jenkins and Millin118,Reference Chang, Vacanti and Michaud119,Reference Shahrestanaki, Khankeh and Masoumi129,135,Reference Adini, Aharonson-Daniel and Israeli138,Reference Cone142,Reference Bacis145,Reference Thomas, Hsu and Kim149–Reference Xu and Li155 At the local level, a physical emergency operations center (EOC) with well-defined jurisdictional responsibility is mandated for MCI management. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adini, Bodas and Nilsson21,Reference Alexander22,Reference Biddinger, Cadigan and Auerbach28,Reference Bradt31,Reference Bukowski34,Reference Cha, Kim and Kim36,Reference Holgersson47,Reference Juffermans and Bierens50,Reference Moser, Connelly and Baker55–Reference Stander, Wallis and Smith59,Reference Wurmb, Schorscher and Justice61,Reference Zafar, Jawad and Shamim62,Reference Ganz, Schafer and Yang64–Reference Wachira, Abdalla and Wallis66,Reference Jenckes, Catlett and Hsu73,Reference Baker82,Reference Gryth, Rådestad and Nilsson88,Reference Higgins, Wainright and Lu89,Reference Burke, Iverson and Goodhue99,Reference Cocco and Thomas-Boaz110,Reference Collignon111,Reference Catlett, Jenkins and Millin118,Reference Chang, Vacanti and Michaud119,Reference Shahrestanaki, Khankeh and Masoumi129,135,Reference Cone142,Reference Bacis145,Reference Thomas, Hsu and Kim149,Reference Born, Briggs and Ciraulo151–Reference Shah, Rehman and Sayyed158 EOCs play an important role by coordinating amongst organizations that need medical resources with those that can provide medical resources and delegating various emergent tasks among different entities. Reference El Sayed, Chami and Hitti39,Reference Juffermans and Bierens50,Reference Little, Cooper and Gope54,Reference Catlett, Jenkins and Millin118,Reference Born, Briggs and Ciraulo151,Reference Comfort, Dunn and Johnson152,Reference Xu and Li155,Reference Fletcher, Knight and Pockrus157,Reference Abbasi and Kapucu159,Reference Christian, Sprung and King160 EOCs follow the framework of a centralized and hierarchical incident command system (ICS) in directing all response activities. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Adini, Bodas and Nilsson21,Reference Alexander22,Reference Biddinger, Cadigan and Auerbach28,Reference Cha, Kim and Kim36,Reference Holgersson47,Reference Juffermans and Bierens50,Reference O’Neill56–Reference Stander, Wallis and Smith59,Reference Wurmb, Schorscher and Justice61,Reference Zafar, Jawad and Shamim62,Reference Ganz, Schafer and Yang64–Reference Wachira, Abdalla and Wallis66,Reference Jenckes, Catlett and Hsu73,Reference Baker82,Reference Gryth, Rådestad and Nilsson88,Reference Higgins, Wainright and Lu89,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Burke, Iverson and Goodhue99,Reference Cocco and Thomas-Boaz110,Reference Catlett, Jenkins and Millin118,Reference Chang, Vacanti and Michaud119,Reference Shahrestanaki, Khankeh and Masoumi129,135,Reference Cone142,Reference Thomas, Hsu and Kim149,Reference Born, Briggs and Ciraulo151–Reference Xu and Li155,Reference Fletcher, Knight and Pockrus157,Reference Shah, Rehman and Sayyed158,Reference Hoffner, Keck and Hemphill161–Reference Zane and Prestipino163 Based on the extent and duration of the MCI, the ICS system can be lean or more expansive, requiring additional command and support roles to facilitate the operations of care delivery for at least 10 days without external assistance. Reference Adini, Bodas and Nilsson21,Reference Biddinger, Reisman and Seger29,Reference Bukowski34,Reference Gabbe, Veitch and Curtis40,Reference Gomez, Haas and Ahmed43,Reference Juffermans and Bierens50,Reference Berger, Körner and Bernstein69,Reference Albanese, Burich and Smith75,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Catlett, Jenkins and Millin118,Reference Devereaux, Christian and Dichter120,Reference Rubinson, Hick and Hanfling140,Reference Cone142,Reference Bacis145,Reference Born, Briggs and Ciraulo151–Reference Filmer and Ranse153,Reference Zane and Prestipino163,Reference Kearns, Marcozzi and Barry164 Incident command should be established at the scene of the MCI, within each responding agency, as well as at each health facility that receives victims, and should include clinical and nonclinical representatives to ensure a multidisciplinary approach to disaster management. Reference Biddinger, Reisman and Seger29,Reference Bradt31,Reference Bukowski34,Reference Holgersson47,Reference Rimstad and Braut57,Reference Avidan, Hersch and Spira67,Reference Lynn, Gurr and Memon74,Reference Albanese, Burich and Smith75,Reference Halpern, Tsai and Arnold102,Reference Avitzour, Libergal and Assaf128–Reference Shartar, Moore and Wood130,Reference Hendrickx, D’Hoker and Michiels143,Reference Assa, Landau and Barenboim150,Reference Comfort, Dunn and Johnson152,Reference Filmer and Ranse153,Reference Fletcher, Knight and Pockrus157,Reference Shah, Rehman and Sayyed158,Reference Hoffner, Keck and Hemphill161–Reference Zane and Prestipino163,Reference Born, Briggs and Ciraulo165
Care Delivery
Care delivery is an umbrella term that covers a variety of operational and logistical activities. Approximately two-thirds of the articles, or 67%, covered clinical medical response for MCIs in the pre-hospital and hospital setting, discussing rational use of resources, triage, decontamination, surge capacity, stockpiles of medical supplies and equipment, bottlenecks in providing critical services, care of pediatric patients and other special populations, specialized management of burn injuries, and the unique considerations of chemical, biological, radiological and nuclear (CBRN)-related MCIs.
The operational components of pre-hospital MCI care delivery include evacuation, triage, and safe transport of the victims. Reference Rimstad and Braut57,Reference Zafar, Jawad and Shamim62,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Zoraster, Chidester and Koenig134,Reference Lowe154 Several different triage methodologies have been used and tested in disasters, such as the START, JumpSTART, SALT, or SORT algorithms, among others, which quickly prioritize victims and assist in casualty distribution and setting up treatment areas where patients can be separated into cohorts based on triage categories. Reference Biddinger, Baggish and Harrington27,Reference Bloch, Schwartz and Pinkert30,Reference Bradt31,Reference Crawford, Mackway-Jones and Russell37,Reference El Sayed, Chami and Hitti39,Reference Gabbe, Veitch and Curtis40,Reference Hardy, Fattah and Wisborg45–Reference Holgersson47,Reference Knotts, Etengoff and Barber52,Reference Leahy, Yurt and Lazar53,Reference Moser, Connelly and Baker55,Reference Wild, Maher and Frazee60,Reference Zafar, Jawad and Shamim62,Reference Berger, Körner and Bernstein69,Reference Albanese, Burich and Smith75,Reference Baker82,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Burke, Iverson and Goodhue99,Reference Corcoran, Niven and Reese101–Reference Hick, Hanfling and Cantrill103,Reference Aliyu105,Reference Ablah, Tinius and Konda107,Reference Abraham108,Reference Cocco and Thomas-Boaz110,Reference Catlett, Jenkins and Millin118,Reference Devereaux, Christian and Dichter120,Reference Veenema and Toke125,Reference Jenkins, McCarthy and Sauer127,Reference Zoraster, Chidester and Koenig134,Reference Bacis145,Reference Roccaforte and Cushman148,Reference Born, Briggs and Ciraulo151,Reference Lowe154,Reference Christian, Sprung and King160,Reference Adini, Cohen and Glassberg166–Reference Silvestri, Field and Mangalat184 However, triage is a dynamic process, and patients may need to be reevaluated and reassigned to a different category. Reference Almogy and Rivkind23,Reference Biddinger, Baggish and Harrington27,Reference Broeze, Falder and Rea33,Reference Cha, Kim and Kim36,Reference El Sayed, Chami and Hitti39,Reference Gabbe, Veitch and Curtis40,Reference Hick, Koenig and Barbisch46,Reference Holgersson47,Reference Hsu, Jenckes and Catlett49,Reference Juffermans and Bierens50,Reference Leahy, Yurt and Lazar53,Reference Wild, Maher and Frazee60–Reference Zafar, Jawad and Shamim62,Reference Ganz, Schafer and Yang64,Reference Wachira, Abdalla and Wallis66,Reference Avidan, Hersch and Spira67,Reference Baker82,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Jacobs95,Reference Jacobs and Burns96,Reference Corcoran, Niven and Reese101–Reference Hick, Hanfling and Cantrill103,Reference Aliyu105,Reference Jenkins, McCarthy and Sauer127,Reference Avitzour, Libergal and Assaf128,Reference Zhong, Clark and Hou133,Reference Zoraster, Chidester and Koenig134,Reference Ashkenazi, Olsha and Schecter144,Reference Bond, Subbarao and Kimmel146,Reference Roccaforte and Cushman148,Reference Assa, Landau and Barenboim150,Reference Born, Briggs and Ciraulo151,Reference Lowe154,Reference Christian, Sprung and King160,Reference Adini, Cohen and Glassberg166,Reference Challen and Walter168–Reference Field and Norton174,Reference Gebhart and Pence176–Reference Hirshberg, Frykberg and Mattox189 In such instances, emphasis is placed upon directing scarce resources to those who have the best chance of survival. Reference Almogy and Rivkind23,Reference Albanese, Burich and Smith75,Reference Baker82,Reference Chim, Yew and Song100,Reference Corcoran, Niven and Reese101,Reference Hick, Hanfling and Cantrill103,Reference Aliyu105,Reference Abraham108,Reference Cordner and Ellingham112,Reference Devereaux, Christian and Dichter120,Reference Veenema and Toke125,Reference Biddison, Berkowitz and Courtney131,Reference Born, Briggs and Ciraulo151,Reference Christian, Sprung and King160,Reference Field and Norton174,Reference Hirshberg, Holcomb and Mattox180,Reference Hogan and Brown181,Reference Castle187 When determining appropriate and timely patient distribution, the distance to the nearest facility, type of injuries sustained, special patient needs (eg, pediatrics, burns), and the capabilities of the receiving hospital should be considered, as well as an emphasis of managing families as best as possible. Reference Adini, Bodas and Nilsson21,Reference Almogy and Rivkind23,Reference Biddinger, Baggish and Harrington27,Reference Biddinger, Reisman and Seger29,Reference Bloch, Schwartz and Pinkert30,Reference Broeze, Falder and Rea33,Reference Cha, Kim and Kim36,Reference Crawford, Mackway-Jones and Russell37,Reference El Sayed, Chami and Hitti39,Reference Holgersson47,Reference Leahy, Yurt and Lazar53–Reference Moser, Connelly and Baker55,Reference Wild, Maher and Frazee60,Reference Avidan, Hersch and Spira67,Reference Jenckes, Catlett and Hsu73,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Jacobs95,Reference Brandenburg and Arneson98,Reference Chim, Yew and Song100,Reference Halpern, Tsai and Arnold102,Reference Hick, Hanfling and Cantrill103,Reference Collignon111,Reference Carley, Mackway-Jones and Randic117,Reference Devereaux, Christian and Dichter120,Reference Joho, Lozano and Pagella123,Reference Seifman, Ek and Menezes124,Reference Avitzour, Libergal and Assaf128,Reference Al-Shamsi, Moitinho de Almeida and Nyanchoka132,Reference Zoraster, Chidester and Koenig134,Reference Adini, Aharonson-Daniel and Israeli138,Reference Hendrickx, D’Hoker and Michiels143–Reference Bacis145,Reference Branas, Sing and Perron147,Reference Assa, Landau and Barenboim150,Reference Lowe154,Reference Kearns, Marcozzi and Barry164,Reference Adini, Cohen and Glassberg166,Reference Cryer, Hiatt and Eckstein173,Reference Castle187,Reference Conlon and Martin188,Reference Kanter190 When indicated, mass decontamination procedures are initiated at the scene of injury and repeated or continued at a health facility. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Crawford, Mackway-Jones and Russell37,Reference Albanese, Burich and Smith75,Reference Currie and Heslop77–Reference Allen, Parrillo and Will80,Reference Baker82–Reference Chilcott, Larner and Durrant86,Reference Higgins, Wainright and Lu89,Reference Hood, Fernandes-Flack and Larrañaga90,Reference Abraham108,Reference Collignon111,Reference Ashkenazi, Olsha and Schecter144,Reference Bacis145,Reference Lowe154,Reference Born, Briggs and Ciraulo165,Reference Burgess, Kovalchick and Harter191
Hospital response must integrate vertical and horizontal response capabilities, tiered surge capacity (conventional, contingency, crisis), maintenance of supply chain, personal protective equipment (PPE) requirements, secondary patient transfers, and the handling of dead bodies. Reference Almogy and Rivkind23,Reference Biddinger, Baggish and Harrington27,Reference Biddinger, Cadigan and Auerbach28,Reference Broeze, Falder and Rea33,Reference Crawford, Mackway-Jones and Russell37,Reference El Sayed, Chami and Hitti39,Reference Gabbe, Veitch and Curtis40,Reference Holgersson47,Reference Little, Cooper and Gope54,Reference Moser, Connelly and Baker55,Reference Albanese, Burich and Smith75,Reference Baker82,Reference Brown, Beatty and O’keefe83,Reference Higgins, Wainright and Lu89,Reference Jacobs and Burns96,Reference Corcoran, Niven and Reese101–Reference Hick, Hanfling and Cantrill103,Reference Aliyu105,Reference Cocco and Thomas-Boaz110–Reference Deelen, Costermans and Moss113,Reference Carley, Mackway-Jones and Randic117,Reference Devereaux, Christian and Dichter120,Reference Zhong, Clark and Hou133,Reference Rebmann, McPhee and Osborne136,Reference Esbitt139–Reference Brunner, Rocha and Chudgar141,Reference Roccaforte and Cushman148,Reference Kearns, Marcozzi and Barry164,Reference Born, Briggs and Ciraulo165,Reference Garner175,Reference Bayram, Zuabi and Subbarao186,Reference Castle187,Reference Caramello, Camerini and Ricceri192–Reference Davis, Poste and Hicks194 In-hospital clinical care can be facilitated by unidirectional patient flow, keeping triage cohorts together, implementing a disaster patient tracking system, pre-positioning pre-stocked medicines and supplies with adjacent quick-reference or action cards, directing skilled staff to pre-allocated areas to provide care, delegating unskilled volunteers to perform menial tasks (transportation of patients, blood, equipment), enacting an early discharge pathway for non-critically ill patients present within the ED and/or hospital, and using a mobile health-based data entry system. Reference Nekoie-Moghadam, Kurland and Moosazadeh13,Reference Almogy and Rivkind23,Reference Einav, Schecter and Matot38,Reference El Sayed, Chami and Hitti39,Reference Hick, Koenig and Barbisch46,Reference Hsu, Jenckes and Catlett49,Reference Juffermans and Bierens50,Reference Knotts, Etengoff and Barber52–Reference O’Neill56,Reference Zafar, Jawad and Shamim62,Reference Wachira, Abdalla and Wallis66,Reference Avidan, Hersch and Spira67,Reference Jenckes, Catlett and Hsu73,Reference Lynn, Gurr and Memon74,Reference Baker82,Reference Liebergall, Braverman and Shapira93,Reference Seaton, Maier and Sachdeva94,Reference Jacobs and Burns96,Reference Halpern, Tsai and Arnold102,Reference Hick, Hanfling and Cantrill103,Reference Abraham108,Reference Cocco and Thomas-Boaz110,Reference Cordner and Ellingham112,Reference Carley, Mackway-Jones and Randic117,Reference Veenema and Toke125,Reference Al-Shamsi, Moitinho de Almeida and Nyanchoka132,Reference Brunner, Rocha and Chudgar141,Reference Born, Briggs and Ciraulo151,Reference Feizolahzadeh, Vaezi and Taheriniya156,Reference Born, Briggs and Ciraulo165,Reference Garner175,Reference Ashkenazi, Kessel and Olsha185,Reference Bayram, Zuabi and Subbarao186,Reference Caramello, Camerini and Ricceri192,Reference Dann, Bonstein and Arbov193,Reference Haverkort, Bouman and Wind195–Reference Soffer, Klausner and Bar-Zohar197 Radiology services, primarily x-ray, and CT scans, are relevant diagnostic modalities in traumatic injuries and guide management decisions, particularly with the assumption that 50% of injured patients will require operative management. Reference Almogy and Rivkind23,Reference Avidan, Hersch and Spira67,Reference Berger, Körner and Bernstein69,Reference Lynn, Gurr and Memon74,Reference Avitzour, Libergal and Assaf128,Reference Ashkenazi, Kessel and Olsha185,Reference Bookman and Zane198 However, radiology has been recognized as a bottleneck for patient care. Reference Bloch, Schwartz and Pinkert30,Reference Kearns, Skarote and Peterson51,Reference Berger, Körner and Bernstein69,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Halpern, Tsai and Arnold102,Reference Veenema and Toke125,Reference Brunner, Rocha and Chudgar141,Reference Bookman and Zane198 Lean strategies are recommended, such as limiting radiologic capabilities to only high priority patients, using bedside ultrasound to facilitate rapid identification of operative pathology, stationing a radiologist with the radiology tech in the patient care area to aid in prompt diagnosis, and facilitating paper-charting or use of a simplified computerized electronic order entry to order a diagnostic study. Reference Almogy and Rivkind23,Reference Bernardo and Veenema26,Reference Bloch, Schwartz and Pinkert30,Reference Brands, Hernandez and Stenberg32,Reference El Sayed, Chami and Hitti39,Reference Hick, Koenig and Barbisch46,Reference Kearns, Skarote and Peterson51,Reference Avidan, Hersch and Spira67,Reference Berger, Körner and Bernstein69,Reference Baker82,Reference Brooke Lerner, O’Connor and Schwartz91,Reference Halpern, Tsai and Arnold102,Reference Hick, Hanfling and Cantrill103,Reference Veenema and Toke125,Reference Biddison, Berkowitz and Courtney131,Reference Brunner, Rocha and Chudgar141,Reference Bookman and Zane198
Health Finance
Seven of the included articles directly addressed the financing of MCI response. Financial resources, largely determined by the fiscal budget of the city government, determine the extent at which MCI response activities can be operationalized in an effective and timely manner. Reference Adelaine, Shoaf and Harvey20,Reference Biddinger, Baggish and Harrington27,Reference Biddinger, Reisman and Seger29,Reference Gotham, Sottolano and Hennessy44,Reference Golabek-Goldman87,Reference Higgins, Wainright and Lu89,Reference Jacobs and Burns96,Reference Smith, Paturas and Tomassoni104,Reference Seifman, Ek and Menezes124,Reference Janati, Sadeghi-Bazargani and Hasanpoor126,Reference Shartar, Moore and Wood130,Reference Al-Shamsi, Moitinho de Almeida and Nyanchoka132,Reference Born, Briggs and Ciraulo151 Recognizing that there are many competing priorities for municipal funds, local government officials should perform annual hazard analyses to allocate resources corresponding to level of risk. Reference Adelaine, Shoaf and Harvey20,Reference Biddinger, Baggish and Harrington27,Reference Brands, Hernandez and Stenberg32,Reference Gotham, Sottolano and Hennessy44,Reference Moser, Connelly and Baker55,Reference Chim, Yew and Song100,Reference Smith, Paturas and Tomassoni104,Reference Cocco and Thomas-Boaz110,Reference Seifman, Ek and Menezes124,Reference Janati, Sadeghi-Bazargani and Hasanpoor126,Reference Shartar, Moore and Wood130,Reference Al-Shamsi, Moitinho de Almeida and Nyanchoka132,Reference Hendrickx, D’Hoker and Michiels143,Reference Branas, Sing and Perron147,Reference Born, Briggs and Ciraulo165
Discussion
With the premise that an effective and timely response saves lives, the immediate aftermath of an MCI deserves special attention. An effective MCI response minimizes chaos, misinformation, and delays in care. However, defining effectiveness is met with considerable variability. Here, we sought to characterize the essential domains and components of an emergency medical response, specifically pertaining to MCIs. The observed heterogeneity and complexity of emergency medical response system components during an MCI are by and large a function of the scope of the event on the affected population. System-level tools and assessments exist to improve disaster readiness but fall short of comprehensively capturing crucial activities in an MCI emergency medical response framework. 1,Reference Rentschler199–203 The World Health Organization’s (WHO) Emergency Response Framework (ERF) is geared toward emergencies with public health consequences that are outside of the definition of this study’s defined MCI (eg, natural disasters, bioterrorism events, or pandemics) and limits its framework to the activities of the WHO. 201 Other frameworks such as the mass casualty management systems framework summarize comprehensive strategies and guidelines for building health sector capacity at the national level, provincial/state level, community and local government level, and health-care facility level. 203 Using the thematic analysis in this study, an Integrated Framework of MCI Response with the essential domains and components is presented in Figure 3. The framework highlights the connections and interrelatedness of different components, which is sometimes overlooked when studying one aspect of the MCI response. It is, therefore, imperative to remember how each of these component influences and shapes the other.
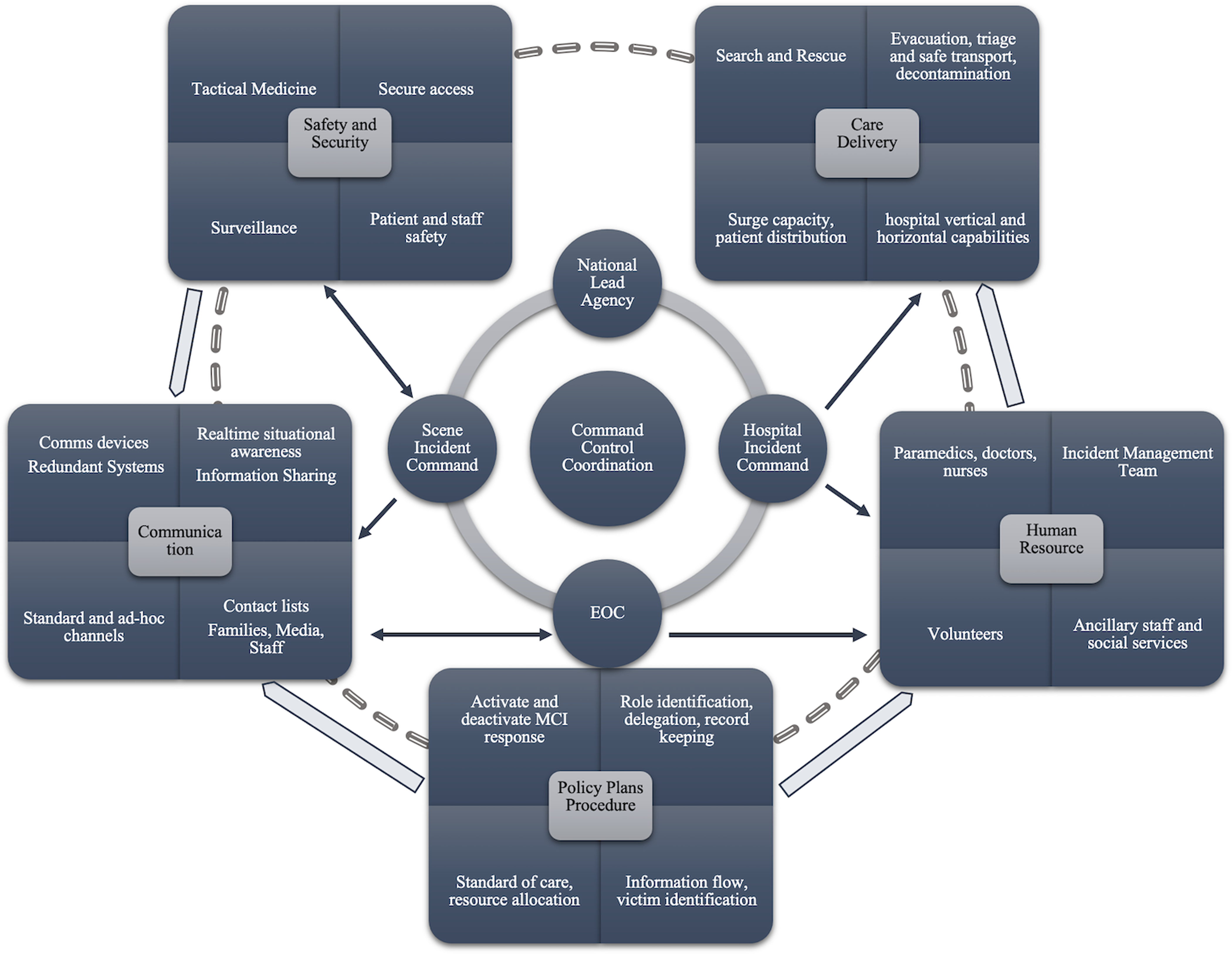
Figure 3. Integrated framework of MCI response.
Best practices pertaining to MCI response commonly emerge from real-world contexts and are often anecdotal. Real-world experience could better inform practices through more systematic collation and rigorous analysis. Few studies based on experimental design pertaining to MCI response were found in this review, likely attributable to the largely unpredictable nature of MCIs. Another notable observation was the predominant focus of literature on process outcomes, such as early MCI activation, EMS response time, shortened transit from scene to facility time, early injury identification, and efficient injury management. In contrast, only a few included articles presented data linking process improvements to improved health outcomes. Reference Einav, Schecter and Matot38,Reference Ablah, Tinius and Konda107,Reference Feizolahzadeh, Vaezi and Taheriniya156,Reference Gebhart and Pence176,Reference Kanter190 This suggests that further research is needed to explore how health and other impact outcomes are affected by improvements in process indicators.
Furthermore, despite LMICs carrying the global burden of death and disability from MCIs, evidence concerning emergency response from these settings remain sparse. 204 The majority of the studies in this review are from high-income countries, potentially limiting generalizability to LMICs. The essential domains and components of an organized approach to MCIs can be adapted to LMICs but is not representative of the unique challenges facing low-resourced environments and, therefore, should be applied with caution. For instance, very limited information is available on the key responders representing institutions not typically involved in response in HICs. Additionally, many identified components of the emergency medical response were found to hinge upon the preparedness of regional medical centers and the presence of health-care infrastructure capable of providing emergency care services, which often is not as developed in LMICs. Reference Murray, Elmes and Fly205,Reference Cosgrove, Jenckes and Kohri206 More research taking into consideration the perspective of MCI response in LMIC settings is warranted. The predominance of descriptive, observational, and case studies provides low-quality of evidence related to education, training, clinical care, and in some instances, policy recommendations.
Limitations
Although this review focuses on the response phase of the disaster management cycle, it is recognized that effective emergency response cannot be separated from preparedness, mitigation, and recovery. Studies pertaining to these other phases were designated as outside of the scope of this review. The selected focus of this review centered on the subset of manmade MCIs due to their increasing frequency and high relevance to understanding emergency medical response capacity and may not necessarily be applicable to other events that are subacute or of a protracted nature. As stated in our findings, the literature on MCI is largely from high-resource settings, despite a relatively higher burden in LMICs. We believe the basic characteristics of a response system would remain the same irrespective of the setting and the specific roles of the individual institutions. Finally, MCIs of catastrophic proportions that resulted in complete disruption of health systems were not examined, and accordingly, findings may have limited generalizability outside of the scope of this review.
Conclusions
This study identified significant gaps in the available evidence on emergency health system response for MCIs, with much of the literature characterized as anecdotal. Most existing literature is also from high income countries, with far less evidence from low resource, particularly LMIC, settings. We identify 7 essential domains, 40 sub-components of an emergency medical response system, and introduce an Integrated Framework of MCI Response to highlight the interconnectedness of an MCI emergency response. The framework for MCI response is limited if it is not evaluated and implemented by key stakeholders in the immediate aftermath of an MCI. Further research on emergency response capacity for MCIs tailored to the LMIC context is greatly needed.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/dmp.2022.235
Acknowledgments
We acknowledge the support of Ms. Katie Lobner, Dr. Rodney Omron, Ms. Chelsea Ducille, and Mr. Julio DeJesus for providing their technical manuscript assistance.
Author contributions
J.R. conceived and designed the study, and obtained research funding. A.U., A.M., S.R., A.E., A.A., O.A., J.D. acquired, analyzed and interpreted the data. A.U., A.M., and E.H. drafted the manuscript, and all authors contributed substantially to its revision. A.U., A.M., C.T., and J.R. supervised and provided final approval of the manuscript version for publication. A.U. and J.R. take responsibility for the manuscript as a whole.
Funding
Angelica K. Ezeigwe BS MPH was supported by the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by Grant Number TL1 TR003100 from the National Center for Advancing Translational Sciences (NCATS). Junaid Razzak MBBS PhD FACEP was supported by the Enhancing Learning and Research for Humanitarian Assistance (ELRHA) 2016 Research Grant for Health in Humanitarian Crisis (R2HC). He is also supported by the National Institutes of Health in the United States and Aga Khan University in Pakistan.








