A nuclear detonation of the size modeled (0.1-10 kiloton [kT]) in the Scarce Resources for a Nuclear Detonation Project, consistent with the National Planning Scenarios,1 will result in a massive influx of injured victims and concerned citizens to health care facilities, necessitating a rapid, effective, and fair approach to triage.Reference Knebel, Coleman and Cliffer2Reference Caro, DeRenzo and Coleman3 In general, most health care workers have limited knowledge of the specific issues relating to triage and treatment after a nuclear detonation and have not responded to a catastrophic mass casualty event. To address this knowledge gap and provide just-in-time diagnostic and medical management information for planners and health care workers, the Office of the Assistant Secretary for Preparedness and Response4 partnered with the National Library of Medicine to produce the Radiation Emergency Medical Management (REMM) Web site.5 The Scarce Resources for a Nuclear Detonation ProjectReference Knebel, Coleman and Cliffer2Reference Coleman, Knebel and Hick6 described in this special issue of Disaster Medicine and Public Health Preparedness models the consequences of a nuclear detonation in an urban setting and suggests approaches to medical triage in a crisis situation.Reference DiCarlo, Maher and Hick7Reference Hick, Weinstock and Coleman8Reference Casagrande, Wills and Kramer9 The information and assumptions in this article are built on background information in the other articles in the issue,Reference Knebel, Coleman and Cliffer2Reference Caro, DeRenzo and Coleman3Reference DiCarlo, Maher and Hick7Reference Hick, Weinstock and Coleman8Reference Casagrande, Wills and Kramer9Reference Dodgen, Norwood and Becker10Reference Murrain-Hill, Coleman and Hick11Reference Sherman12 which provide the basis for an online interactive tool and a set of triage “cards” (available in this manuscript as Figures 1 through 4 and on the REMM Web site), along with suggestions for application. The focus is on the scarce resource setting expected during the first 4 days after a nuclear detonation. Beyond that time (or sooner if the resource setting improves), there will be a return to contingency and conventional resource settings and “usual care” or “functionally equivalent care,” as defined by the Institute of Medicine (IOM).13
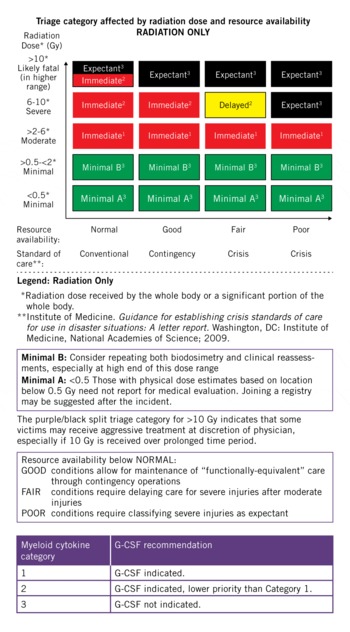
FIGURE 1 Triage card 1: RADIATION ONLY—triage category affected by radiation dose and resource availability

FIGURE 2 Triage card 2: Triage category for TRAUMA and COMBINED INJURY affected by injury severity, radiation dose, and resource availability

FIGURE 3 Triage card 3: Myeloid cytokine (eg, granulocyte colony-stimulating factor) recommendation for casualties with “minimal trauma/radiation only” and “combined injury”

FIGURE 4 Triage card 4: Myeloid cytokine (eg, granulocyte colony-stimulating factor) recommendation for casualties with “minimal trauma/radiation only” and “combined injury”
An overarching goal of the Scarce Resources for a Nuclear Detonation Project was to provide practical information and tools for medical planners and responders that could be used as a starting point for local/regional planning and response, if needed. The key driving forces for this project are the following:
• A well-considered tool that is available both in advance for planning and as just-in-time information for such a large no-notice incident is far better than chaos.
• Few people will have experience with radiation, so guidance will be welcome.
• Data used for triage should be accurate but simple so that triage can be performed with the limited information likely available in the first 4 days.
• To achieve fairness across the response, it is necessary to have a common approach and tools.
• Preparation and response will be facilitated for planners and responders with resources such as medical triage guidance (this article), information on REMM,5 and a state and local planner's playbook.Reference Murrain-Hill, Coleman and Hick11
METHODS
Scarce Resources for a Nuclear Detonation Project Process
The participants in this projectReference Coleman, Knebel and Hick6 are subject matter experts in a range of areas relevant to medical planning and response to a major public health incident, including ethics and legal issues. Some participants are actively involved in nuclear/radiological preparedness. As detailed in the Project Summary in the article by Coleman et al,Reference Coleman, Knebel and Hick6 the lead authors in the Scarce Resources for a Nuclear Detonation Project prepared 10 manuscripts addressing key topics. The manuscripts were reviewed, discussed, and revised by the coauthors, and then by a group of experts who had attended the initial meetings. These manuscripts were then submitted to Disaster Medicine and Public Health Preparedness for full peer review and revised accordingly. The authors recognize that these recommendations represent expert opinion, and that there are limited human and animal data describing the diagnosis and treatment of whole-body radiation injury with or without the kind of severe trauma and/or burns that may be seen after a nuclear detonation. The guidance represents neither formal US government guidelines nor mandated practice standards of care. Over time, it is anticipated that this guidance will be reviewed, analyzed, and improved.
The background information and references can be found in the other articles.Reference Knebel, Coleman and Cliffer2Reference Caro, DeRenzo and Coleman3Reference Coleman, Knebel and Hick6Reference DiCarlo, Maher and Hick7Reference Hick, Weinstock and Coleman8Reference Casagrande, Wills and Kramer9Reference Dodgen, Norwood and Becker10Reference Murrain-Hill, Coleman and Hick11Reference Sherman12 The present article includes key background points used for developing the triage guidance.
Overarching Principles of Fairness in TriageReference Caro, DeRenzo and Coleman3
Triaging victims requires selecting some to receive treatment before others.Reference Caro, DeRenzo and Coleman3 To maximize fairness, each person in the same triage category (ie, the same predicted outcome) should have an equal opportunity of receiving treatment based on the availability of resources. For example, everyone within the same triage category who could benefit from a ventilator should have an equal chance of obtaining one until they are no longer available. Selection could be made by a lottery, first-come, first-served, or by other predetermined criteria. Preference should not be based on nonmedical factors, as discussed by Caro and coauthors.Reference Caro, DeRenzo and Coleman3
Although saving lives is a primary goal, equally important goals are providing compassionate, palliative (symptomatic) care and fairly apportioning available resources for both lifesaving and palliative interventions, as discussed by Caro et al.Reference Caro, DeRenzo and Coleman3 In the aggregate, these goals support provision of the “greatest good for the greatest number.” Thus, it is medically and ethically acceptable to allocate some portion of available resources that could be used as part of lifesaving treatment to alleviate pain and suffering in individuals who are not expected to survive.
Need for Reassessment and Repeat Triage
Reassessment and repeat triage are key features of the nuclear detonation medical response, as resource availability improves over time and casualties are moved to locations distant from the epicenter of the blast. For example, during this process of reassessment and repeat triage, some could have their status changed from “expectant” to “immediate” or “delayed.”
“Triage tools” in this article are meant to assist the medical decision makers. Certainly, medical judgment and experience are also key factors. Tools cannot account for all of the variables, and thus cannot be used to provide a binary answer, only to assist in clinical decision making. Gaining familiarity with this triage tool in advance will help provide some order in the initial chaos.
Radiation Dose Rate: Prompt and Protracted
Radiation dose from a nuclear detonation can be instantaneous from exposure to the prompt (instantaneous from explosion) radiation released with the blast wave or protracted (from fallout) for hours to days from the fallout as contaminated materials fall back to earth. Most significant fallout exposure occurs in the first few hours.Reference Knebel, Coleman and Cliffer2 Protracted exposure generally produces less biological injury than an equivalent instantaneous exposure.Reference DiCarlo, Maher and Hick7 The numerical casualty risk models discussed in other articles consider protracted exposure and the dose-rate effect. However, for simplicity purposes, the dose-related triage tools proposed in this article for the few days of the response ignore the effects of protracted dose. This simplification will be needed for management and is sufficiently accurate for initial triage purposes, given the various other uncertainties: the likelihood that whole-body dose will be nonuniform (or even just partial body), uncertainties about the duration of exposure, effects of sheltering, and likelihood that for most victims, exposure protraction will occur during only a few hours. Subsequent detailed medical management will depend on the patient's medical course and on refinement of dose estimates, including laboratory data that will be available at later times.
Acute Radiation Syndrome and LatencyReference Knebel, Coleman and Cliffer2Reference DiCarlo, Maher and Hick7
Acute radiation syndrome (ARS) typically involves 3 phases. The duration of each depends on the total radiation dose and the rate at which it is delivered. After initial radiation exposure there may be a prodromal phase, with symptoms such as nausea, vomiting, and lethargy. Symptoms may occur at doses as low as 0.75 Gy. The prodromal phase is followed by a latent phase, during which a person feels relatively well before developing the manifest phase of organ system dysfunction. Of the various ARS organ system subsyndromes, the hematological system is the most sensitive (>1-2 Gy), followed by the gastrointestinal tract (approximately 4-6 Gy), skin (approximately 6 Gy depending on radiation type), and cerebrovascular system (approximately 10 Gy). Other organ systems such as the lungs (approximately 8 Gy) can also be involved, although typically after multiple weeks. The latent phase of hematological ARS at the lower dose range (approximately 2-4 Gy) may be 1 to 3 weeks. Higher doses may shorten or eliminate the latent phase. The time phases of ARS are illustrated on the REMM Web site.14 Patients receiving higher levels of exposure may be a low priority for therapeutic interventions because of their poor prognosis and limited resources, as discussed below.
Diagnostics and Licensed Therapeutics for ARS
The diagnostic laboratory tools available include hematologic assays (complete blood count and lymphocyte-depletion kinetics) and the dicentric chromosome assay.Reference Knebel, Coleman and Cliffer2Reference DiCarlo, Maher and Hick7 Research and development by the National Institutes of Allergy and Infectious Diseases and the Biomedical Advanced Research and Development Authority of point of care and high throughput diagnostics is ongoing.
There are no US Food and Drug Administration (FDA) products licensed for ARS treatment. Recommendations in this issue (eg, for cytokines) are based on hematology, oncology, and transplantation experience. There will be off-label use of products currently licensed and/or emergency use authorization for products currently licensed and possibly under development.
Good medical practice and the best interests of the patient require that physicians use legally available drugs, biologics, and devices according to their best knowledge and judgment. If physicians use a product for an indication not in the approved labeling, then they have the responsibility to be well informed about the product, to base its use on firm scientific rationale and on sound medical evidence, and to maintain records of the product's use and effects. Use of a marketed product in this manner when the intent is the “practice of medicine” does not require the submission of an Investigational New Drug Application, Investigational Device Exemption, or review by an institutional review board. See also http://www.fda.gov/RegulatoryInformation/Guidances/ucm126486.htm.)
Standards of Care and Resource Situations13
Table 1 illustrates the relation between resource availability as used in this project to the definitions of conventional, contingency, and crisis situations and related standards of care as proposed by the IOM (eFigure). Note that “crisis standards” pertain to settings in which the functional equivalent of normal care cannot be maintained.
TABLE 1 Relation Between Resource Availability as Used in This Project and the IOM's Crisis Situation13

There are 4 resource-availability states used in the modeling for this project: normal, good, fair, and poor. Conventional is “normal” and contingency is “good.” For crisis situations there will be insufficient resources for all of the people who need lifesaving intervention. In both the “fair” and “poor” resource settings, the highest priority for immediate treatment is people with moderate life-threatening injury rather than those with severe injury. The distinction between “fair” and “poor” is that in “fair” there are still sufficient resources for treating the moderate life-threatening injury group (but not severe), whereas in “poor” resources to even treat people with moderate life-threatening injuries are insufficient.
The injury modeling for this project, illustrated in Figure 4 in the article by Casagrande et al,Reference Casagrande, Wills and Kramer9 indicates that prioritization of victims with “moderate” life-threatening injury over victims with “severe” life-threatening injury saves lives and uses resources more effectively under crisis conditions.
Triage Categories That Include Radiation Injury
Triage begins with the assessment of physical trauma (and/or burn) and continues with the assessment of possible radiation exposure and whole-body dose. Table 2 describes the Scarce Resources for a Nuclear Detonation Project triage categories for injuries from radiation only and also from radiation plus trauma and/or burns.
TABLE 2 Triage Categories for Injuries From Radiation Only and Radiation Plus Trauma and/or Burns

Although the names of the 4 standard categories are retained, the definition of minimal also includes parameters for radiation dose without physical injury or burn. Minimal (green) assignments due to minor trauma, minimal burn, and low-dose radiation (eg, <2 Gy) may require medical care, but are not deemed to be life threatening in the initial 4-day time period. Minimal in this setting is also different from the traditional trauma triage category “minor,” because some minimal patients may require substantial intervention within the next few days as resources become available (eg, a fracture that is initially splinted because of resource scarcity will require a subsequent orthopedic procedure). Immediate (red), delayed (yellow), or expectant (black) triage category assignments after a nuclear detonation may be applied to trauma, burn, radiation, or a combination of injuries.
A unique aspect of a nuclear detonation is that large numbers of people will need to be evaluated for radiation exposure, even those who may have minimal or no physical injury. Dose from exposure will be a key clinical triage parameter. Dose estimation can be performed by knowing a victim's physical location(s) after the detonation and matching that location to radiation levels that were estimated or measured in the environment, assessing the onset and severity of signs and symptoms of ARS and matching those to dose ranges previously described, and/or evaluating blood counts or other laboratory techniques such as cytogenetics. Using the combination of laboratory and clinical factors to estimate dose is called biodosimetry.
Victims exposed to 0.5 to 2 Gy (Minimal B triage category) may require an initial assessment followed by multiple biodosimetry assessments, but they are unlikely to require clinical intervention for ARS. There are some victims who, by virtue of their location, have a minimal risk of having received a radiation dose of ≥0.5 Gy (Minimal A). It is suggested that these individuals not receive formal evaluation for radiation exposure, certainly not in the first few days. (The break point at 0.5 Gy is somewhat arbitrary. It was chosen because the lowest dose at which symptoms of exposure [eg, nausea, vomiting] are usually seen is approximately 0.7 Gy.)15
RESULTS
Clinical Considerations for Triage
Initial medical triage will consider 4 factors. The first 3 should be reassessed iteratively over time as more data become available.
Factor 1: Physical Trauma and/or Burns
The categories used for assessment of trauma severity are outlined in Table 3 and were the categories used by Casagrande et alReference Casagrande, Wills and Kramer9 in modeling the outcomes from different triage approaches. The initial assessment will be for life-threatening injury, which includes severe trauma, moderate trauma, or combined injury. Minimal trauma may require medical care, but it is not immediately life threatening. The trauma triage system used will be that in routine use. Effects will be visible from physical examination or inferred from history. Traumatic injuries are the primary consideration in initial triage and treatment. Once a patient is triaged immediate (red) or delayed (yellow) by traumatic injuries, the radiation dose (factor 2) and comorbid conditions (factor 4) should be used to modify triage priority.
TABLE 3 Trauma Categories Used in the Scarce Resources for a Nuclear Detonation ProjectReference Casagrande, Wills and Kramer9

For victims with second-degree burns (superficial partial thickness and deep partial thickness) or third-degree burns (full thickness), 20% of total body surface area (TBSA) is used as the threshold that worsens clinical prognosis and triage category. The choice is somewhat arbitrary and judgment will be required because prognosis worsens with increasing area. Of note, a recent radiation biology article on combined injuryReference Ledney and Elliott16 used 15% as a marker of worse prognosis, and the American Burn Association referral recommendation is 10% TBSA. We selected 20% because the mortality from burn alone is increased at >20% TBSA.Reference Osler, Glance and Hosmer17Reference Ryan, Schoenfeld, Thorpe, Sheridan, Cassem and Tompkins18 Patients with extensive burn injuries consume substantially more resources.Reference Ryan, Schoenfeld, Thorpe, Sheridan, Cassem and Tompkins18 Burn is one injury for which age matters for triage because burns in elderly adults have a much worse prognosis.Reference Osler, Glance and Hosmer17Reference Ryan, Schoenfeld, Thorpe, Sheridan, Cassem and Tompkins18
Factor 2: Radiation Dose
Radiation dose will be assessed initially from simple parameters: history of the victim's location(s), victim's sheltering actions after the detonation, and signs and symptoms from exposure to prompt radiation or early particulate fallout. Effects may include skin redness (related to radiation effects but unrelated to thermal trauma), nausea, vomiting, and lethargy. Although common after whole- or significant partial-body radiation exposure, vomiting is not a specific predictor of radiation doseReference Demidenko, Williams and Swartz19 and could also reflect head trauma, anxiety, or other pathology. Thus, the presence of vomiting should be considered in the context of all of the other factors, including physical location, other signs and symptoms, and likelihood of radiation exposure. When laboratory tests become available, particularly the absolute lymphocyte count (ALC), a more accurate assessment of radiation dose will be possible.20
Factor 3: Combined Injury
Combined injury is defined as estimated whole-body/significant partial-body radiation dose of ≥2 Gy in combination with moderate or severe life-threatening trauma (Table 3) or burns >20% TBSA. Those with minimal trauma are triaged according to the radiation only card (Figure 1). Superficial partial-thickness and deep partial-thickness (second degree) or full-thickness (third degree) burns >20% of TBSA worsens the triage category (ie, puts victims lower on the priority list) 1 level or more, for example, immediate to delayed or expectant and delayed to expectant.
Factor 4: Comorbid Conditions
Some prior comorbid conditions may affect the outcome of treating trauma, burns, or radiation injury (Table 4).Reference DiCarlo, Maher and Hick7 These conditions reduce the efficacy and effectiveness of medical intervention or prompt the need for unsustainable resource expenditures in a crisis setting, which could compromise the effectiveness of treatment for many others. Thus, in appropriate circumstances, preexisting conditions are factors to be considered in assigning triage category.
TABLE 4 Suggested Medical Evaluation During First 4 Days After a Nuclear Detonation

Medical Evaluation
Despite the complexity and uniqueness of a nuclear detonation, much of medical management follows standard medical practice. Table 4 provides examples of expected injury types, medical evaluation approaches, and other diagnostic considerations as they relate to triage. The fourth column includes medical conditions that may be confused with effects from a high dose of radiation. For example, deafness or blindness could be mistaken for neurovascular ARS. The eTable provides examples of mild, moderate, and severe trauma that may be seen in a nuclear detonation. A detailed table is included in the article by Casagrande and colleagues.Reference Casagrande, Wills and Kramer9
It is not possible to fully define all of the medical evaluation and triage criteria because the subtleties of medical judgment are essential in both patient assessment and assignment of category. The tables provide examples of what issues may be considered. Standard trauma triage techniques generally apply (eg, use of trauma scores) to initial assessment.
Triage Cards as Clinical Tools for Use During Response to a Nuclear Detonation
To assist responders and planners, this article provides tools to guide diagnosis and management tasks during the initial 4 days of the response. These are offered as recommendations for triage categories and cytokine use, and are not to be inferred as official guidance. Figures 1 through 4 are “cards” for assigning triage categories based on how injury severity changes in progressively worsening resource settings, as was noted in Table 1. (Cards can be downloaded and printed from the REMM Web site, which also has an interactive tool linked to them.5 Each has a front “side” with recommendations and a reverse “side” with a legend including explanations and definitions. Usability testing and feedback from receivers and health care providers may lead to modification of the cards over time. Therefore, it is suggested that if the reader wants to download and/or print the cards, they should visit the REMM Web site, where updated versions will be available.)
The superscripts appended to triage categories suggest guidance on how to prioritize the use of myeloid cytokines (eg, granulocyte colony-stimulating factor [G-CSF]) to mitigate ARS (Table 5). Myeloid cytokines may shorten or prevent neutropenia in some victims exposed to ≥2 Gy (discussed further by DiCarlo et alReference DiCarlo, Maher and Hick7). Other myeloid cytokines, such as pegylated G-CSF or granulocyte monocyte colony-stimulating factor may also be considered.
TABLE 5 Myeloid Cytokine Category (for G-CSF or Equivalent) for Mitigation of ARS

To be usable in emergencies, cards for use in triage categorization have limitations to the amount of information they can contain. The complex issues in a nuclear detonation required specialized information relating to the following:
• Change in triage status as the resource situation changes
• Standards of care and resource setting
• Categories of trauma
• Definition of combined injury
• Isolated radiation injury
• Biodosimetry, including use of the ALC
• Guidance for the use of myeloid cytokines (G-CSF and related cytokines)
Although the triage cards are designed to be self-explanatory, the discussion below summarizes what is on each card and some of the background behind it.
Triage Card 1 (Figure 1): Radiation Only—Triage Category Affected By Radiation Dose and Resource Availability
The radiation dose categories refer to doses absorbed by the whole body or a significant portion of the whole body. Dose can be estimated using the following:
• Victim's location and sheltering actions at the time of the detonation and during the fallout
• Time of onset and severity of the signs and symptoms of ARS
• Biodosimetry (dose calculation tools are available on REMM)20
– Laboratory tests, especially ALC; a single ALC can be helpful, but serial analyses are more accurate
– Cytogenetic analysis, if available, particularly as confirmation for ALC when needed; this assay requires 3 to 4 days to process and is not available in usual clinical laboratories
To simplify triage, this article uses 5 radiation dose ranges:
• >10 Gy: Fatal—Almost universally fatal, even with intensive management in normal resource environment.
• >6-10 Gy: Severe radiation injury—Initial symptoms are severe. After short or no latent period, hematological and gastrointestinal ARS will predominate.
• >2-6 Gy: Moderate radiation injury—Initial symptoms will range from mild to severe. After a latency period of days to weeks, hematologic ARS will be the primary manifestation, with gastrointestinal ARS at the higher end of the dose range.
• >0.5-2 Gy: Minimal B radiation injury—May produce mild prodromal signs and symptoms, especially at the higher end of the dose range. Unlikely to develop significant hematologic, gastrointestinal, or other manifest ARS. Multiple biodosimetry measurements may be warranted in the upper dose range to ensure that initial dose was not an underestimate.
• <0.5 Gy: Minimal A radiation injury—Biodosimetry is not indicated if physical dose estimate is below 0.5 Gy. Epidemiologic studies may be conducted later.
Under normal conditions with conventional standards of care, those with an estimated dose between 2 and 10 Gy would be triaged to receive immediate (red) care. Although doses above 10 Gy are likely to be fatal within 24 to 48 hours, there may be a limited number of scenarios with few casualties, protracted exposure, and possible dose inhomogeneity over the whole body in which physicians elect to aggressively treat patients using cytokines and supportive care rather than expectant triage and comfort care. Thus, under normal conditions, clinicians may choose to triage some patients with likely fatal (>10 Gy) exposures as immediate (red) and not as expectant (black), particularly for patients with exposures at the lower end of this range. However, as the resource situation and standards of care change from normal to contingency or crisis, those with >10 Gy are triaged as expectant.
Working under fair resource availability conditions, there are still sufficient resources to treat those exposed to a moderate (>2-6 Gy) dose. Those exposed to a severe (>6-10 Gy) dose would be triaged as delayed. As resources diminish further (poor resource availability), patients estimated to have received exposures >6 Gy may be triaged to expectant.
The priority for administration of cytokine (G-CSF or related drug) is indicated by the superscripts:
• Category 1: Cytokine (eg, G-CSF) is indicated and it is a first priority.
• Category 2: Cytokine (eg, G-CSF) is indicated, but this group is a lower priority than category 1.
• Category 3: Cytokine is not indicated.
Triage Card 2 (Figure 2): Triage Category for Trauma and Combined Injury Affected By Injury Severity, Radiation Dose, and Resource Availability
After a nuclear detonation, triage assignments will be based initially on the severity of trauma, with further refinements based on observed clinical radiation effects and estimated dose using the best techniques available at the venue. Because significant radiation dose worsens outcome after trauma and burns,Reference DiCarlo, Maher and Hick7 combined injury is included in the trauma triage scheme.
Triage category is determined by 4 factors:
1. Injury severity: degree of trauma and extent/degree of burns
• Injury severity is defined according to Table 3 with examples from a nuclear detonation in the eFigure. Standard trauma triage techniques and systems that are routinely employed are used.
• Trauma severity should be assessed before assessing radiation dose.
• Partial-thickness (second degree) or full-thickness (third degree) burns to >20% TBSA worsens the triage priority by at least 1 level (eg, immediate (red) to delayed or expectant and delayed (yellow) to expectant).
2. Radiation dose
• Non–life-threatening or minimal trauma or burns to <20% TBSA plus radiation injury is triaged as radiation only (Figure 1).
• A patient with life-threatening trauma (moderate or severe) plus a radiation dose ≥2 Gy will be considered to have experienced a combined injury.
3. Resource availability
4. Comorbid diseases—May be appropriate modifiers of triage category if they directly affect survival as related to immediate injury and intervention.Reference Caro, DeRenzo and Coleman3
In normal resource settings, conventional triage prioritizes the most severely injured people as immediate.
In contingency settings, severe life-threatening trauma alone is still triaged as immediate; however, combined injury may be triaged as immediate or delayed, or even expectant, especially in the higher radiation dose ranges, which are likely to be rapidly fatal (Figure 2).
In crisis situations with fair resource availability, moderate life-threatening trauma is treated before severe trauma because that saves more lives.Reference Caro, DeRenzo and Coleman3 Combined injury would be triaged as delayed or expectant, as indicated by the split box. Under crisis situations with poor resource availability, moderate trauma would be triaged as immediate and severe trauma and combined injury as expectant.
Triage Cards 3 and 4: Myeloid Cytokine (eg, G-CSF) Recommendation for Casualties with “Radiation Only/Minimal Trauma” and “Combined Injury”
These are based on “normal or good” resource availability or “fair or poor” resource availability (Figure 3 and Figure 4). Triage category and cytokine prioritization are a function of injury/burn severity and radiation dose. Prioritization to receive cytokines should occur after conducting a trauma-based severity assessment, and is dependent on resource availability. Included here are recommendations for delivery of myeloid cytokines under “normal to good” resource availability and “fair to poor” resource availability. Victims with minimal trauma and radiation should be triaged according to the radiation only triage scheme. The use of cytokines will depend ultimately on availability at each venue, so even those triaged to immediate care may be further subdivided based on priority for cytokines (superscripts in Figure 3 and Figure 4).
G-CSF, granulocyte monocyte colony-stimulating factor, and pegylated G-CSF are licensed by the FDA and commonly prescribed for treatment of neutropenia from chemotherapy and other clinical situations. These agents are not licensed by the FDA for acute or chronic radiation injury. Nonetheless, it is likely that these countermeasures will provide clinical benefit in treating radiation injury after a nuclear detonation.Reference DiCarlo, Maher and Hick7 At present, myeloid cytokine administration to victims after a nuclear detonation before the onset of leukopenia would be either an off-label use (discussed above) or require an emergency use authorization from the Department of Health and Human Services Secretary when drugs from the Strategic National Stockpile or other federal resources are used.
Although myeloid cytokine use is likely to provide benefit after significant acute radiation injury, data on timing after radiation injury have not been validated in humans. Recent nonhuman primate animal data suggest that the maximal effect may require administration of the first dose within 24 hours after exposure.Reference DiCarlo, Maher and Hick7Reference Dainiak21Reference Hérodin and Drouet22 A first dose within 24 hours after exposure is the current goal of the optimal nuclear detonation response. Additional animal studies in progress are evaluating the efficacy of drug administration beginning at later time points. Because G-CSF and other agents are likely to be in short supply after a nuclear detonation, this is a key resource that will need to be prioritized, as outlined in Figure 3 and Figure 4.
DISCUSSION
The variables to consider in triage and myeloid cytokine administration after a nuclear detonation are complex. Medical triage and treatment decision making must account for trauma, burn, and radiation injuries as well as comorbid conditions. An individual's predicted outcome must then be weighed against the current level of available resources in each venue and region. There will be substantial resource heterogeneity based on distance from the epicenter and the resources available will change over time so that adaptability to the changing resource setting is critical to optimizing the response.
A key goal of the Scarce Resources for a Nuclear Detonation Project was to assist medical planners and receivers faced with making these challenging decisions by developing useable triage guidance and tools based on the best available evidence, expert opinion, and ethical principles. The overarching ethical principle is fairness; priorities include saving the greatest number of lives, maximizing the efficacy of scarce resource use, and providing palliative care to the greatest extent possible.Reference Caro, DeRenzo and Coleman3 The tools we have developed can be applied to response activities when demand exceeds available resources, primarily during the first 4 days after a nuclear detonation or for a shorter period of time if resource availability improves and standards of care return to normal.
The impact of radiation on triage category should include laboratory (biodosimetry) confirmation of radiation dose whenever possible. The absolute lymphocyte count, particularly using serial assessments (ie, lymphocyte-depletion kinetics), is the most useful measure of dose, although other techniques are in development.Reference Rea, Gougelet, Nicolalde, Geiling and Swartz23 The triage categories used by the Scarce Resources for a Nuclear Detonation Project for normal and contingency conditions are compatible with the recent proposed triage categories by Rea et al,Reference Rea, Gougelet, Nicolalde, Geiling and Swartz23 in which 2 Gy is “unaffected” or “minimal,” 2 to 6 Gy is “variable” or “urgent,” 6 to 10 Gy is “immediate,” and >10 Gy is “expectant.”
The Scarce Resources for a Nuclear Detonation Project developed triage cards and an interactive online tool with which triage officers may make rapid, consistent, and informed decisions based on each individual's medical condition and the current resource setting. This tool is derived from the Model of Resource and Time-Based TriageReference Casagrande, Wills and Kramer9 described elsewhere in this issue and located on the REMM Web site.5 The triage cards can be printed from REMM and made available as hard copy in emergency departments and distributed among first responders, receivers, and health care workers who are responsible for triage decisions. The triage tool can be used either online or downloaded.
The triage tools and guidance presented here are based on available, albeit limited, data, as discussed in the other articles in this issue. The known effects of whole-body radiation on humans (in the absence of trauma) derive primarily from descriptions of industrial accidents, clinical medicine, and historical data from atomic bomb events. Data from animal models of radiation injury support the use and efficacy of supportive care (fluid, nutrition, antibiotics, and myeloid cytokines) and reinforce the observation that combined injury usually produces a worse outcome than single injury alone.Reference DiCarlo, Maher and Hick7 In the modeling data,Reference Casagrande, Wills and Kramer9 a shortage of medical personnel was identified as the key limiting resource in trauma care, although supply shortages will also constrain the delivery of an effective response.
Despite the limitations, the Scarce Resources for a Nuclear Detonation Project modeling demonstratesReference Casagrande, Wills and Kramer9 that in severely resource-constrained settings, prioritizing moderately injured victims for care over those with severe life-threatening injuries enhances the effectiveness of the medical response and saves more lives than other triage schemes. This approach supports the ethical principle of fairness. Under normal circumstances, fair allocation of resources is based on a first come, first served triage scheme that is preempted by the arrival of more severely injured patients. Caro and colleaguesReference Caro, DeRenzo and Coleman3 make the point that this prioritization order can be modified if there is reason to believe that a different prioritization will enhance the effective utilization of available resources.
The opportunity for usability or field testing for this tool is limited, but this will be done when possible during response exercises. The information presented in this article is a new paradigm for civilian medical care after a nuclear detonation and this approach may be explored further for other resource-scarce settings.
CONCLUSIONS
The set of triage cards provides triage and prioritization tools for victims of a nuclear detonation who have radiation exposure only, trauma and combined injury, and a demonstrated need for myeloid cytokines. An online tool is available on the REMM Web site, along with background information and a state and local planner's playbook.Reference Murrain-Hill, Coleman and Hick11 These are new approaches to a complex situation that will provide guidance should an incident occur and provide a framework for further refinements.
This guidance was developed by Scarce Resources for a Nuclear Detonation Project subject matter experts.Reference Coleman, Knebel and Hick6 It is meant to assist responders and planners in the aftermath of a nuclear incident. It is not intended as definitive guidelines or official policy. Other clinical factors must be considered as appropriate. Further refinement will be ongoing and suggestions are welcome. The approaches and models, including Model of Resource and Time-Based TriageReference Casagrande, Wills and Kramer9 and REMM,5 serve as examples for how the Office of the Assistant Secretary for Preparedness and Response, US Department of Health and Human Services and subject matter experts are working together to meet the goal of “a nation prepared.”4
Author Disclosures: The author reports no conflicts of interest.
Acknowledgments: The authors acknowledge the contribution of Alicia Livinski, biomedical librarian, National Institutes of Health Library, and Paula Murrain-Hill, program analyst, Office of the Assistant Secretary for Preparedness and Response, DHHS, for their assistance with the preparation of this article.











