Introduction
Healthcare-acquired infections (HAIs) are a worldwide problem that directly affect hospitalized patients and are, in turn, a complication which can directly affects patient safety. Such infections represent a challenge for public health due to potential adverse clinical events and prolongation of hospital stays with a consequent increase in healthcare costs [Reference Barahona, Rodriguez and De Moya1, 2]. According to data provided by the Study of the Prevalence of Nosocomial Infections in Spain (EPINE in its Spanish abbreviation), the prevalence of HAIs in Spain in 2022 was between 5 and 10%, and in turn, the prevalence of HAIs in our centre (the General University Hospital of Alicante or HGUA) in the same year was 8.2% [3]. The most important measure to prevent the transmission of microorganisms and reduce HAIs is hand hygiene (HH) [Reference Boyce and Pittet4] and its proper compliance [Reference Pittet, Hugonnet and Harbarth5–Reference Chico-Sánchez7] according to the ‘5 moments’ for the application of HH as recommended by the World Health Organization (WHO). These are (1) before touching a patient, (2) before performing an aseptic task, (3) after the risk of exposure to body fluids, (4) after patient contact, and (5) after contact with the patient’s environment [Reference Derksen, Keller and Lippke8].
In the context of the COVID pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which is transmitted through close contact and respiratory droplets or aerosols [Reference Moore9], HH, along with the use of personal protective equipment (PPE) and proper respiratory hygiene [Reference Moore9–Reference Aguilar, Hernández and Ibañez13], became an important part of the measures adopted to prevent the transmission of the virus. These measures proved to be highly important due to constant exposure of healthcare staff to infected patients and contaminated surfaces, and consequently posed a risk of both acquiring and transmitting the infection [Reference Lotfinejad, Peters and Pittet12]. Thus, compliance with HH recommendations and its monitoring were key measures to prevent HAIs and reduce the transmission of COVID-19 infection [Reference Boyce and Pittet4, 14].
Numerous studies have surveyed the HH compliance in different hospital areas and generally, compliance levels seldom exceeded 50% [Reference Pittet, Hugonnet and Harbarth5, Reference Chico-Sánchez7]. In this current study, HH compliance was monitored through direct observation (the gold standard method) [Reference Boyce15], and results were communicated healthcare staff to better understand how compliance changed with time, and the factors that may contribute to poor HH practice [11, Reference Sánchez-Payá16, Reference Sánchez-Payá17].
After the start of the COVID-19 pandemic, during the first quarter of 2021, Gras-Valentí et al. [Reference Gras-Valentí18] recorded close to 90% HH compliance in an emergency department. In addition, Wong et al. [Reference Wong19] reported from a study in two paediatric hospital units during the pandemic that full HH compliance by staff was possible. Thus, evaluation of the current situation, post-COVID-19, represents an opportunity to determine the impact of the pandemic on HH compliance on HH and, make healthcare-personnel more aware of its importance in the quality of patient care, and hence promote better adherence to WHO guidelines.
Methods
Population/measures
This was a repeated cross-sectional study in a tertiary-level hospital. The data on the degree of HH compliance, through direct observation, from 2005 to 2022 were obtained through the Epidemiological Surveillance program established by the Center’s Preventive Medicine Service. Observations were carried out of one health professional at a time; without prior notice for 1 h during working hours at a single fixed moment in time. No interventions were made, or follow-up over time of the observations. Observers explained the reason for their presence and requested verbal authorization of the staff to carry out the observation, and completed an anonymous form designed to evaluate HH compliance [Reference Sánchez-Payá17, Reference Wong19], in terms of the measures performed (positive), and those not performed (negative), as well as recording potential explanatory variables (sex, age, type of healthcare-personnel, area of care, WHO activity code, knowledge of the HH leaflet, training session attendance, and availability of pocket-sized hydroalcoholic hand sanitizer – PSAS solution). HH actions that did not correspond to a ‘WHO moment’ were not recorded. The method of choice for hand hygiene at the centre was mainly hydroalcoholic solution; on some occasions, it was substituted with soap and water with subsequent application of hydroalcoholic gel.
Statistical analysis
During the first phase of the study, compliance with recommendations on HH with confidence intervals (95% CI) was calculated as the ratio between the number of HH actions carried out and the number of WHO HH opportunities: compliance (%) = (actions carried out/opportunities) × 100. To study the evolution over time, a trend analysis based on the degree of compliance was carried out using estimates for 18 periods (from 2005 to 2022) in the different hospital areas. A permutation test for join point regression (JoinPoint®) was used to detect significant percentage changes of the period in the prevalence of degree of compliance. The overall statistical significance level was p = 0.05, allowing a maximum of 7 joining points and 8 line segments.
I year 2018–2019 was taken as the reference period prior to the COVID-19 pandemic, and from June 2020 to end of April 2022 was considered the pandemic period. To study the impact of the pandemic, the degree of HH compliance was compared before and during the pandemic; the odds ratio (OR) and its 95% CI were calculated for each of the subgroups. Associations between HH compliance with the study period and possible explanatory variables were investigated using chi-squared tests. The magnitude of any observed associations was expressed as OR 95% CI. Finally, a multivariate analysis was performed with the variables that showed a statistically significant association in order to estimate the adjusted OR with 95% CIs, using a logistic regression model. The level of statistical significance in all tests was p < 0.05, and SPSS software (version 25.0; IBM Corp., Armonk, NY) was used for the analyses. The study was approved by the Drug Research Ethics Committee at the Department of Health (PI2021/181).
Results
A total of 9,083 activities in which HH had been indicated were observed in the HGUA in the pre-pandemic period (2018 to 2019), compared with 5,821 during the pandemic.
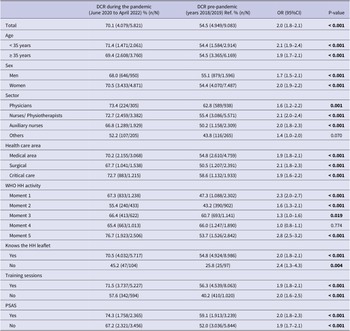
Table 1 shows the trend in the prevalence of degree of compliance from 2005 to 2022. The lowest compliance was in 2005 with 31.0% (95% CI: 29.6%–32.5%) in contrast with 66.5% in 2020 (95% CI: 64.0%–69.0%); 73% in 2021 (95% CI: 71.5%-74.5%) – the highest compliance in the 18 years studied, and 65.3% in 2022 (95%CI:62.3%–68.2%), (Figure 1). Joinpoint regression analysis showed significant inflexion points between the periods from 2005 to 2013, from 2013 to 2014, from 2014 to 2015, from 2016 to 2019 and from 2019 to 2021. Non-significant inflexion points were detected between the period from 2015 to 2016, and from 2021 to 2022.
Table 1. Period percentage change (PPC) in the degree of compliance on hand hygiene recommendations
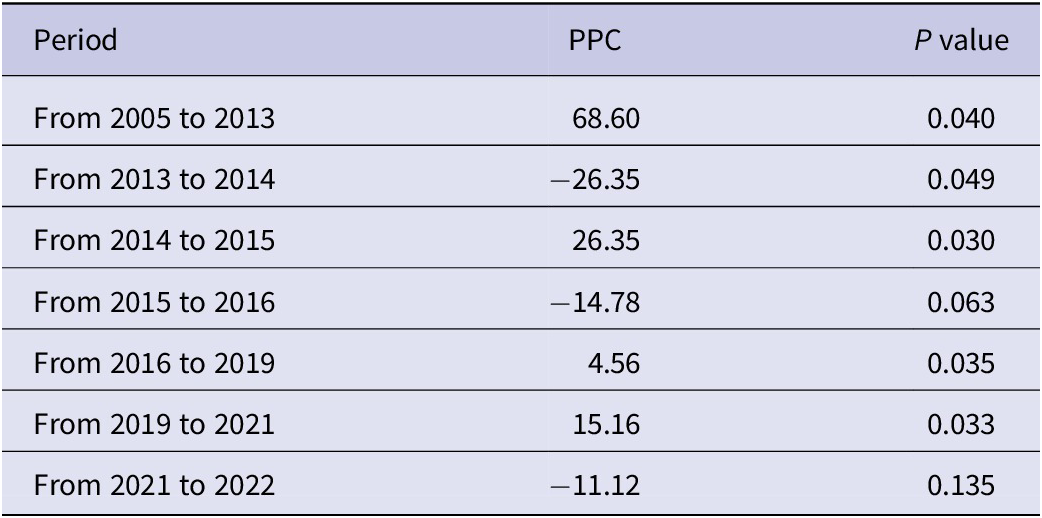

Figure 1. Evolution of the degree of compliance on hand hygiene recommendations pre-pandemic period and during the COVID-19 pandemic period.
HH compliance increased significantly (p < 0.001) to 70.1% (95%CI: 68.9–71.2) during the COVID-19 pandemic compared to 54.5% (95%CI: 53.5–55.5) in the prior reference period (Table 2). As shown in Table 1, compliance during the pandemic was higher in healthcare-personnel aged under 35 years at 71.4% (1,471), in 70.5% (3433) of women, 73.4% (224) of physicians, and 74.3% (1758) of staff carrying pocket-sized alcohol hand sanitizers. There was a significant increase in the degree of HH compliance at each of the WHO moments during the pandemic period (p < 0.05), with the exception of moment 4. Compliance with the latter was 66.0% (95%CI: 63.8–68.1in the period prior to the pandemic, and no significant differences were observed between the first and second periods (p = 0.774). Compliance with WHO moment 2 was lowest in both periods (43.2% and 55.4%, respectively). (Table 2). The highest degrees of compliance (72.7%; 95%CI: 70.1–75.2) were observed in the critical care unit in medical areas (72.7%; 95%CI: 68.6–71.9) in the 2020–2022 period (Table 2).
Table 2. Hand hygiene compliance during the COVID-19 pandemic and in the pre-pandemic period

Note: Boldface indicates statistical significance (P < 0.05).
CI, 95% confidence interval; DCR, degree of compliance with the recommendations; HH, hand hygiene; Moment 1, before contact with the patient; Moment 2, before carrying out an aseptic technique; Moment 3, after contact with biological fluids; Moment 4, after contact with the patient; Moment 5, after contact with the patient’s environment; N, number of opportunities to perform hand hygiene; n, number of times hand hygiene was performed; OR, odds ratio; PSAS, pocket-sized hydroalcoholic solution; 95% P, level of statistical significance; Ref., reference category for calculating the magnitude of the association.
As shown in Table 3, the factors that were significantly and independently associated with HH compliance were the time period (before or during the COVID-19 pandemic), with an ORa of 2.0 (95%CI: 1.8–2.1), knowledge of the HH leaflet (ORa = 1.8; 95%CI: 1.3–2.5), training session attendance (ORa = 1.6; 95%CI: 1.4–1.8), and availability of PSAS (ORa = 1.4; 95%CI: 1.3–1.5), as well as medical care areas (ORa = 1.2; 95%CI: 1.1–1.3) and critical care units (ORa = 1.4; 95%CI:1.3–1.5), and attention to the WHO moments 1,3,4, and 5.
Table 3. Factors associated with HH compliance according to the characteristics of the health professionals and activity
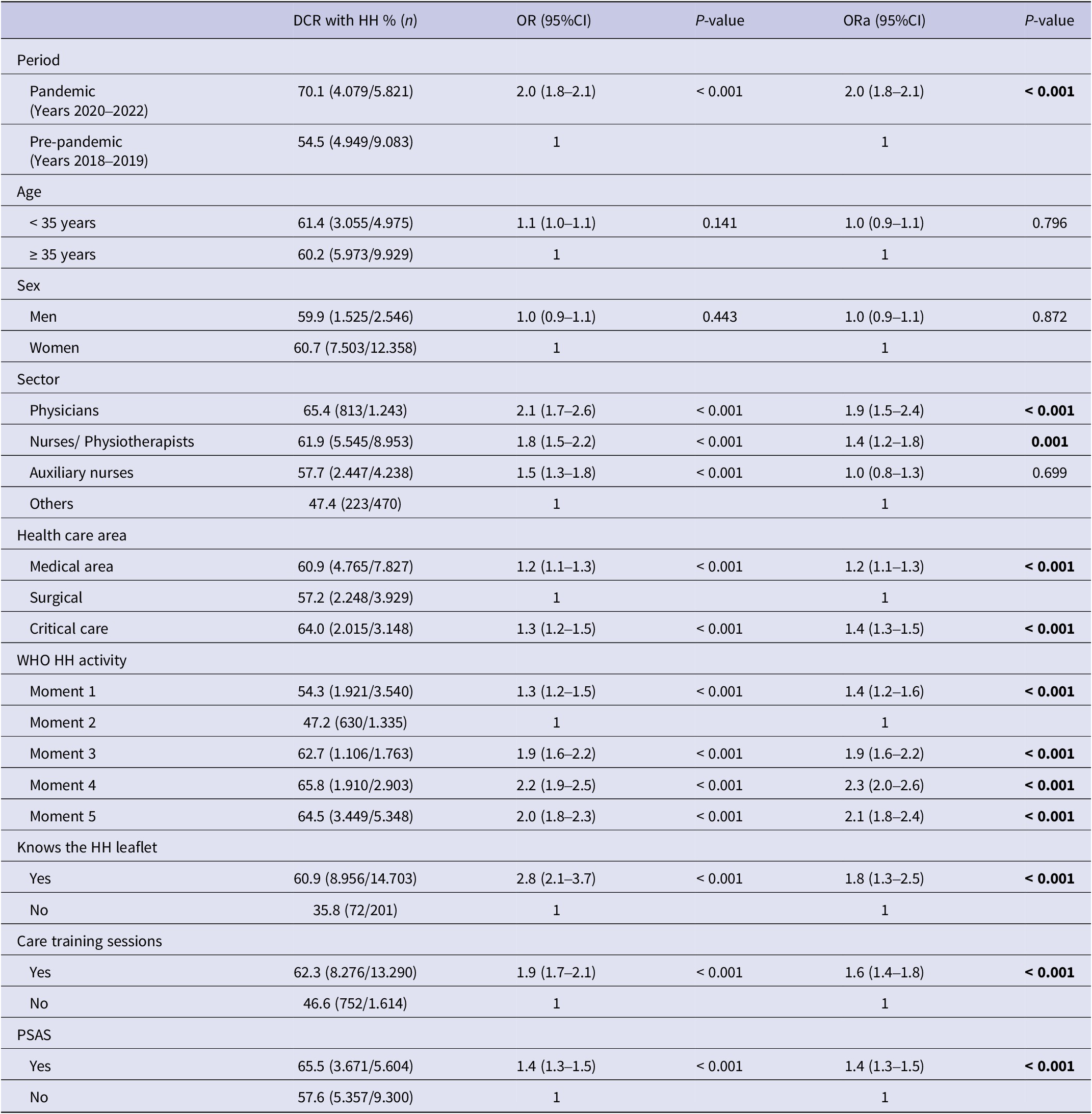
Note: Boldface indicates statistical significance (P < 0.05).
DCR, degree of compliance with the recommendations; HH, hand hygiene; Moment 1, before contact with the patient; Moment 2, before carrying out an aseptic technique; Moment 3, after contact with biological fluids; Moment 4, after contact with the patient; Moment 5, after contact with the patient’s environment; OR, odds ratio; ORa, adjusted odds ratio; P, level of statistical significance; pa, adjusted level of statistical significance; PSAS, pocket-sized hydroalcoholic solution; 95% CI, 95% confidence interval.
Discussion
In recent years, many efforts have been made to monitor the on HH practice in different healthcare areas around the world, and several have showed a high level of non-compliance with the recommendations [Reference Pittet, Hugonnet and Harbarth5, Reference Derksen, Keller and Lippke8, Reference Lotfinejad, Peters and Pittet12, Reference Sánchez-Payá17]. Infection prevention and control measures, especially HH, have gained vital importance worldwide in the current context of the COVID-19 pandemic. Indeed, several studies, including a meta-analysis by Ying et al. [Reference Wang20], have shown, among others, a significant increase in HH practice at the beginning of the pandemic (years 2020–2021) [Reference Gras-Valentí18, Reference Wong19]. Nonetheless, relatively little research has continuously monitored over time to determine if compliance was maintained throughout, or varied during the pandemic. Thus, this current work provides pertinent data that show a significant improvement in HH compliance which was sustained during the COVID-19 pandemic. In fact, the highest levels of compliance recorded in recent years (70.1%) were reached during the pandemic, with figures similar to those published by Qian Zhou et al. [Reference Zhou21]. In contrast, other studies reported a lack of increase [Reference Casaroto22, Reference Sandbøl23], or even a decline [Reference Huang24, Reference Stangerup25], in HH compliance over the period. These results differ from our own observations, perhaps due to differences in the methodology used to document this metric. Indeed, to our knowledge, all of the previous studies monitored the HH compliance through an electronic system, which may have led to certain differences in the observed trend. Current evidence supports such systems as a complement to direct observation for monitoring HH, but the latter continues to be the gold standard method.
In addition, we found that the WHO moment was independently and significantly associated with the degree of compliance on HH, as evidenced by the observed improvement in practice in the 2020–2022 period for all, but ‘moment’ 4 which nonetheless, did not reflect a significant increase in compliance during the pandemic compared with the period beforehand, which stayed constant at around 65%. This finding might suggest that performing HH ‘after’ direct contact with patients is a deep-rooted behaviour among healthcare-personnel. Moreover, although there was an improvement in compliance for all WHO moments, there was a higher degree of conformance for moments 3, 4, and 5 which all occur ‘after’ contact or exposure to patients, their fluids, or environment. This view is supported by the lower compliance with moments 1 and 2, which occur ‘before’ the contact or care procedure [Reference Derksen, Keller and Lippke8]. Specifically, moment 2 had the lowest degree of compliance in both periods, even though it increased by almost 15 percentage points during the pandemic period. This finding may be of concern considering that the purpose of HH at moments 1 and 2 is to prevent the transmission of infectious agents to patients, while at moments 3, 4, and 5, its primary purpose is prevention of the risk of transmission to healthcare-personnel and contamination of the care area [26].
These results coincide with previously published studies [Reference Chico-Sánchez7, Reference Sánchez-Payá16, Reference Sánchez-Payá17, Reference Zhou21, Reference Sodré da Costa27] and could possibly reflect a behaviour guided by healthcare-personnel being concerned for their self-protection after coming into contact with patients, thus making them potential dispersers of microbes to patients. As a consequence, these data indicate that successive training interventions focused on the importance of preventing cross-infections through HH performed at WHO moments 1 and 2 (those that constitute a greater risk of infection to patients) should be emphasized [Reference Derksen, Keller and Lippke8]. In general, the increase in HH during the COVID-19 pandemic had a positive impact on the reduction of HAIs and infection resistance rates, as seen in other studies [Reference Wee28–Reference Luangasanatip30]. This justifies the implementation of strategies aimed at markedly improving HH compliance to levels ranging from 89.8–97.1% [Reference Pittet, Hugonnet and Harbarth5, Reference Chico-Sánchez7, Reference Sánchez-Payá16, Reference Sánchez-Payá17, Reference Banks and Phillips31]. From this perspective, it is of interest to define accurately the key factors which influence the compliance in the healthcare setting so that strategies which coincide with the most critical moments for patient safety can be implemented.
Factors such as training session attendance, knowledge of the HH leaflet, and carrying pocket-sized hand sanitizer were also independently and significantly associated with HH compliance. These results corroborate the data obtained in a previous study [Reference Pittet and Boyce32] which recorded compliance rates of 66% after carrying out educational and awareness-raising interventions for professionals. Of note, in general, it is difficult to compare the results between studies due to differences in the methodology employed or the specific study period. Thus, the results reported here should be considered with caution as it is too early to know if they will be maintained over time once the COVID-19 pandemic has ended.
The outcomes seen in the data we report here can have an impact on infection prevention and control strategies for COVID-19 and inform practice in future microbial epidemics. Indeed, increased information in the media about the importance of HH, and the greater perception of risk by staff following after the COVID-19 pandemic was declared led to greater awareness of the value of these measures [Reference Neuwirth, Mattner and Otchwemah33]. Even so, some authors, including Wong et al. [Reference Wong19] and Ragusa et al. [Reference Ragusa34], observed maximum compliance with HH prior to the pandemic, which may suggest a prior awareness of its importance by healthcare-personnel – a very encouraging finding when considering how to continue promoting these measures. There was a marked improvement in hand hygiene practice in our hospital which indicates that the strategies implemented were effective. In future work, the main objective will be to maintain the improvement over time and focus on factors that can potentially be improved, such as enhancing the hand hygiene knowledge, awareness, and motivation of health care personnel.
The limitations of this study were inherent in its design and objective. For example, the decrease in patients seen in surgical areas during the COVID-19 pandemic (because of the suspension of non-urgent operations) may have impacted on the number of observation opportunities in these areas. In addition, the Hawthorne effect – modification of behaviour due to awareness of observation – and the possible resulting overestimation of compliance must also be considered. Nonetheless, this effect remained constant in all the study observations. Another possible limitation was that of selection, but as recorded in a previous study on HH compliance [Reference Sánchez-Payá17], the rate of non-participation by staff did not exceed 1.2%. The use of multiple observers may have led to increasing variability in recording and collection of data. To minimize this effect, all observers were trained using the same methodology and were all members of the Preventive Medicine Service.
Conclusion
The COVID-19 pandemic promoted an increase in the HH compliance reflecting a very positive change in this practice by healthcare-personnel. Monitoring and evaluation of compliance allowed us to communicate results to staff, thereby generating active feedback for the development of strategies to improve the quality of patient care and HH compliance. Considering the role that healthcare-personnel play as health agents both in centres and the community, we must take advantage of this momentum and direct our efforts towards new continuous improvement objectives. These include (i) achieving the same or higher HH compliance in WHO moments 1 and 2 as already recorded for moments 3, 4, and 5; and (ii) maintaining the outcomes from the study to ensure that the healthcare environment is a safe place for both staff and patients.
Data availability statement
Data that are not presented in the article are available upon reasonable request from the corresponding author.
Author contribution
M.G-S., P.G-V., P.C-S. and J.S-P. involved in conceptualization; J.S-P., P.G-V., P.C-S. and I.L.G-S. contributed to methodology; P.C-S. contributed to design of software; J.S-P. involved in validation; J.S-P., P.G-V., P.C-S., M.G-S. and I.L.G-S. involved in formal analysis; G.P-A. and R.F.S.A. contributed to investigation; C.M.B.M., L.C.L., and M.S.V. contributed to resources; G.P-A. and R.d.F.S-A. participated in data curation; J.S-P., P.G-V., M.G-S. participated in writing original draft; P.G-V., J.S-P. and M.G-S. involved in writing review and editing; C.M.B.M. contributed to visualization.; M.F-P. supervised the study; P.G-V. involved in project administration. All authors have read and agreed to the published version of the manuscript.
Funding statement
We received funding through the Alicante Institute for Health and Biomedical Research (ISABIAL) plan for scientific and technical research and innovation project number 2021–0392.
Competing interest
The authors declare none.
Ethical standard
The study was conducted in accordance with the Declaration of Helsinki and approved by the Drug Research Ethics Committee at the Department of Health (PI2021/181).