INTRODUCTION
In March 2014, the Guinean Ministry of Health issued an alert about an unidentified disease occurring in the forest region of Guinea that turned out to be Ebola virus disease (EVD) [1]. According to the initial epidemiological investigation results, the suspected index case had died in December 2013 in Meliandou in Guéckédou prefecture [Reference Baize2]. The first Ebola treatment centre was opened in this prefecture by Médecins sans Frontières in March 2014 [3], this outbreak then spread with a sustained transmission in Guinea, Sierra Leone and Liberia [4]. In October 2015, although the outbreak was still ongoing in Guinea, the last case of EVD diagnosed in Guéckédou was on December 2014 [4].
Regarding other morbid conditions, there is increasing evidence that this EVD outbreak has affected the management of infectious diseases in Guinea. From November 2013 to November 2014, a decrease was reported in the numbers of all-cause outpatients visits in the public health facilities in Guinea (11% over the period), cases of fever (15%), and treatment with antimalarial drugs (oral, 24%; injectable, 30%) [Reference Plucinski5]. HIV prevention programmes were affected as well, from April to December 2014, the proportion of patients receiving antiretroviral therapy who did not present to a scheduled visit at Donka hospital increased from 0% to 42%, while a decrease in the number of patients in care was evidenced between June and December 2014 [Reference Ndawinz6]. In Macenta, the EVD outbreak also resulted in a major decrease in the utilization of HIV facilities [Reference Leuenberger7]. Regarding other healthcare services, healthcare centre attendance was halved in N'Zérékoré prefecture during the EVD outbreak [Reference Perron8]. Concerning prevention, disruption of childhood vaccination programmes, especially measles vaccination, might result in severe outbreaks in non-immune populations [Reference Takahashi9]. In Guinea, the measles vaccination coverage rate preceding the Ebola outbreak was estimated to be under the effectiveness threshold, suggesting that additional breakdown of the routine vaccination programme may lead to severe outbreaks [Reference Doumtsop10]. As a consequence of the EVD outbreak, measles vaccination campaigns were not organized in Guinea in the second half of 2014 [11]. Cholera is circulating in this region, especially in Ghana and Côte d'Ivoire, the latter sharing borders with Liberia and Guinea [12, 13]. A spread of this outbreak in the countries affected by EVD could have severe consequences [Reference Azman14].
To quantify the impact of the EVD outbreak on the public healthcare system, we describe the attendance at health centres and health posts, and the main diagnoses reported by these structures in the Guinean prefecture of Guéckédou during the year following Ebola outbreak notification.
METHODS
Data used in this descriptive analysis were provided by the Prefectural Health Direction of Guéckédou. In Guinea, a set of health indicators about public health structures (health centres and health posts) are collected in all prefectures and centralized by the Ministry of Health on a monthly basis through the National System of Health Information and Management (SNIGS) surveillance system. Information is routinely collected, independently of the surveillance specifically implemented in response to the EVD outbreak, through standardized reporting forms in each health centre, including its related health posts. Guéckédou prefecture accounts for 13 health centres and 25 health posts. Data are then computerized at Guéckédou Prefectural Health Direction and communicated to the Ministry of Health. It includes the numbers of visits and diagnosis related to 71 diseases, including 18 with a mandatory notification. Indicators related to maternal and childhood health, prevention of HIV transmission, and financial information about the health structures are also provided [15].
Our study period lasted from January 2012 to March 2015. This period begins 2 years prior the notification of the Ebola outbreak, so as to take into account the influence of seasons on the incidence of a number of infectious diseases such as malaria, which is highly endemic in Guinea [16]. The study ended 3 months after the last EVD case reported by Guéckédou prefecture (December 2014).
Monthly numbers of visits in health centres and health posts reported from January 2012 to March 2015 were provided to describe the trend in attendance at these structures. We used non-parametric methods (Loess regression) to obtain a smooth evolution of the number of visits before and after the first confirmed case of Ebola in Guéckédou (March 2014). The five most frequent diagnoses reported monthly by these public health structures in the surveillance system were also described. This included: malaria, acute respiratory infections, intestinal helminthiasis, vaginal discharge, and gastritis or ulcer. In addition, among infectious diseases requiring a mandatory notification, the six most frequent were described: schistosomiasis, onchocerciasis, bloody diarrhoea, tuberculosis, typhoid fever and measles. Data relating to diseases requiring a mandatory notification were available from January 2012 to December 2014, except for bloody diarrhoea and measles; for these two diseases data collection covered the whole study period.
Information regarding attendance or the number of diagnoses was missing for October 2012, August 2012, and December 2014. In these instances, the mean of the values reported for the preceding and following months was imputed to the missing value.
RESULTS
Attendance at healthcare structures
From January 2012 to March 2015, the median number of visits reported each month in Guéckédou prefecture was 15 724 [interquartile range (IQR) 14 448–16 930].
In 2012 and 2013, the season appears to have influenced attendance, with two peaks observed in March–April and October–November in the numbers of visits reported (Fig. 1). Following the Ebola outbreak notification in March 2014, the seasonal peak was evidenced as during the preceding years, and seemed to be in the same range (18 615 visits in May 2012, 19 175 visits in April 2013, 19 579 visits in March 2014). However, the second peak expected in October–November 2014 was not observed, in contrast the attendance was still falling after July. In 2014, the lowest attendance was observed during September with 12 152 visits, compared to 13 808 visits in July 2013, which represented the lowest attendance observed in the study period preceding the Ebola outbreak notification.

Fig. 1. Attendance at health centres and health posts in the Guinean prefecture of Guéckédou, January 2012–March 2015.
From April to September, 98 225 and 95 567 visits were reported in 2012 and 2013, respectively. During the same period in 2014, corresponding to the EVD outbreak peak in Guéckédou, 90 947 visits were reported. This represented decreases of 4·8% and 7·4%, respectively, compared to 2013 and 2012.
Of note, following the last EVD notification in Guéckédou, the number of visits increased between January and March 2015 (from 12 540 to 16 032 visits). This was lower than in March 2014 (19 579 visits), but was in the same range as in March 2012 (17 578 visits) and 2013 (16 870 visits).
Trends of the main diagnoses
Of 591 751 diagnoses reported during the study period, malaria accounted for 214 155 (36%), acute respiratory infections for 127 022 (21%), intestinal helminthiasis for 69 744 (12%), vaginal discharge for 26 946 (5%), and gastritis or ulcer for 18 481 (3%).
Regarding malaria, the monthly median number of diagnoses reported over the study period was 5370 (IQR 4821–6052). The expected seasonality was observed during the study period, including the EVD outbreak, with 27 890, 25 827 and 22 519 malaria cases reported from April to July in 2012, 2013 and 2014, respectively (Fig. 2).

Fig. 2. Main diagnoses reported by health centres and health posts in the Guinean prefecture of Guéckédou, January 2012–March 2015.
Concerning acute respiratory infections, a higher number of diagnoses was noted during the periods of April–June (median: ~3500 diagnoses/month) and September–December (median: ~3300 diagnoses/month) in 2012 and 2013, respectively. However, in 2014, for the latter period, fewer diagnoses were recorded (median: ~2837 diagnoses/month; Fig. 2).
We did not observe major changes in the other diagnoses (helminthiasis, vaginal discharge, ulcer) reported between March and December 2014 compared to 2012 and 2013 for (Fig. 2).
Evolution of the number of notifiable diseases
Intestinal schistosomiasis was the most frequent mandatory notifiable disease, a median total of 485 cases were reported monthly (IQR 299–589). Seasonality was not observed during the study period, but the number of cases seemed to decrease after June 2013, and an unexpected peak was observed in March 2014 (824 cases). In 2013 and 2012 the highest values were observed in April with 604 and 662 cases, respectively (Fig. 3). The number of urinary schistosomiasis diagnoses reported monthly was much lower (median: five cases) but a peak was observed between April and August 2014 with in median of 52 cases per month and a peak of 89 cases in June.

Fig. 3. Schistosomiasis reported by health centres and health posts in the Guinean prefecture of Guéckédou, January 2012–March 2015.
Over the study period, a median of 42 bloody diarrhoea diagnoses were reported monthly (IQR 28–67). Peaks were observed each year in March (Fig. 4). Following March 2014, the number of bloody diarrhoea cases declined to <30 cases/month [a median number of 20 cases were reported monthly from April 2014 to March 2015 (IQR 12–27)]. From January to March 2014, a total of 261 bloody diarrhoea cases was reported in Guéckédou, 152 (58%) of these being notified by Guendembou and Tékoulo sub-prefectures; both sub-prefectures had notified probable and confirmed EVD cases in the first months of the outbreak. In the preceding year from January to March 2013, of 178 cases of bloody diarrhoea notified in Guéckédou, 75 (42%) were notified from these sub-prefectures.
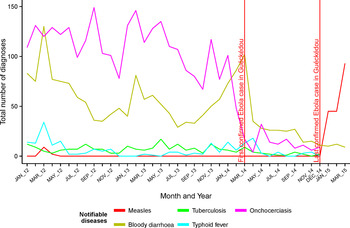
Fig. 4. Notifiable diseases reported by health centres and health posts in the Guinean prefecture of Guéckédou, January 2012–March 2015.
No measles cases were notified between April 2012 and December 2014 (Fig. 4). A total of 183 cases was notified during the first trimester of 2015 in Guéckédou (January: 45 cases; February: 45 cases, March: 93 cases), confirming the measles outbreak reported in N'Zérékoré prefecture at that time [11].
Finally, the number of onchocerciasis diagnoses reported has markedly reduced during the Ebola outbreak, while no important trend was observed regarding typhoid fever and tuberculosis (Fig. 4).
DISCUSSION
This study shows that, in Guéckédou prefecture, attendance in non-hospital public health structures decreased by 5–7% during the first 6 months of the EVD outbreak, compared to the same period in the preceding years.
This reduction might be considered as modest; however, important changes were observed regarding specific diagnoses (bloody diarrhoea, schistosomiasis), while for some high-incidence diseases, such as malaria, no major changes were observed.
During the EVD outbreak in Guéckédou, no health centres or health posts were closed due to medical staff contamination by Ebola virus. Thus, the population had access to all health structures over the study period in Guéckédou, especially during the EVD outbreak.
In N'Zérékoré prefecture, healthcare attendance decreased by around half during the EVD outbreak, which occurred there between September 2014 and February 2015 [Reference Perron8]. Thus, in Guéckédou no major changes were observed in healthcare attendance while in N'Zérékoré, another prefecture located in the Guinean forest region, healthcare attendance was halved during the EVD outbreak. A cross-sectional survey performed in Guinean health facilities has evidenced that decline in healthcare attendance might be driven by the population's fear [Reference Plucinski5]. We can speculate that in N'Zérékoré the population's fear has preceded the occurrence of the EVD outbreak, possibly worsening the fall in healthcare attendance. In Guéckédou, the epicentre of the outbreak, the population's fear might have occurred at the same time as the outbreak, perhaps leading to a lower decrease in healthcare attendance. However, we were not able to fully describe the social characteristics of these prefectures to completely understand this difference.
In a study assessing the effect of the EVD outbreak on malaria case management in Guinea, a cross-sectional survey of health facilities was conducted in eight Guinean prefectures (the four most affected by the EVD outbreak, and four without any reported EVD cases). The most common explanation provided by healthcare workers for the decrease in healthcare attendance were: patient's fear of healthcare workers, contracting EVD during a visit to a health facility, and being sent to an Ebola treatment centre. These results suggest that the EVD outbreak has affected trust in the public health system and led to the population's fear in accessing it [Reference Plucinski5].
We noted an increase in reported bloody diarrhoea and intestinal schistosomiasis in the weeks preceding the EVD outbreak notification, especially in Tékoulo and Guendembou sub-prefectures; two sub-prefectures where EVD cases were diagnosed at the beginning of the outbreak. Reported schistosomiasis diagnoses are clinically based, as biological confirmation is not routinely available, and diarrhoea is a common symptom of this disease. However, it is of note that in all the diseases reported, those for which a peak was observed in the weeks preceding the EVD outbreak notification share common symptoms with EVD: diarrhoea and bloody diarrhoea, even if bleeding is not among the most frequent symptoms reported during the current EVD outbreak [Reference Bah17, Reference Barry18]. Except for malaria, biological confirmation is not routinely available for the diagnoses reported here, and lethality rates are not reported. Thus, we were not able to further describe the aetiology of these peaks of diarrhoea diagnoses.
The absence of measles diagnosis reported during a 32-month period strongly suggests an underreporting of this disease in Guéckédou, as of 28 March 2014 the measles outbreak notified in January 2014 in Guinea has resulted in 4689 cases and 11 deaths [19]. However, despite this limitation, this surveillance system detected the measles outbreak occurring in 2015. The reasons of this underreporting are unclear and should be further explored, as measles diagnosis is clinically based on the occurrence of typical symptoms.
Surveillance systems in Guinea need to be implemented according to international standards in a resilient health system able to respond both to routine and unexpected challenges [Reference Kieny and Dovlo20]. However, it should be acknowledged that data collected through current routine surveillance in Guinea were available to perform this descriptive analysis despite the limitations of these systems. This suggests that the implementation of an efficient surveillance system in Guinea might rely on existing structures.
This study also presents a number of limitations. Rapid diagnosis and malaria treatment are free and widely available in public health structures in Guinea; however, the other diagnoses reported by these health structures are mainly clinically based, even for infectious diseases. Thus, misdiagnosis issues cannot be excluded and the influence of this potential bias could not be assessed. Data are collected on a monthly basis, leading to a poor reactivity of this system, and numerous contributors are involved (health posts, health centres, Guéckédou Prefectural Health Direction, and Ministry of Health). This can lead to potential mistakes in this system, or a lack of reactivity.
This study does not include data related to care provided in hospitals and the private sector, especially traditional healers. The lack of hospital-based information is not expected to be a major issue, as hospital attendance may be quite low compared to all other public health structures. In contrast, the overall health system attendance is underestimated due to the absence of information regarding traditional healers' activity, and information bias cannot be excluded if patients with specific conditions were more likely to visit to traditional healers. In Guinea, prior to the EVD outbreak, it was estimated that 57% of children presenting febrile illness were treated in the public sector, and 13% by traditional healers, which accounts for the most frequent alternative to public sector [16]. This highlights the important role of traditional healers in Guinea.
To fully understand the evolution of healthcare attendance during the EVD outbreak in each prefecture, a detailed social structure should be considered, including health system acceptance.
Observed numbers of patients attending healthcare centres and numbers of specific diagnoses were reported rather than incidence estimates. This is due to the lack of reliable estimations of the Guéckédou population size.
CONCLUSION
Active transmission of Ebola virus was still ongoing in Guinea in October 2015, at that time the last case in Guéckédou was in December 2014. Data observed in this context appear to show that lower attendance at public health structures observed during the EVD outbreak was not persistent in this Guinean prefecture. The emergence of measles recalls the marked consequences of an EVD outbreak, related to the higher risk of occurrence of other infectious diseases outbreaks. This highlights the necessity of implementing efficient surveillance and outbreak response in resilient health systems, in implementing these measures social specificities should be considered.
ACKNOWLEDGMENTS
The authors acknowledge Dr Henriette De Valk (French Institute for Public Health Surveillance) and Dr Josep Jansa (European Centre for Disease Prevention and Control) for their input in this manuscript.
DECLARATION OF INTEREST
None.






