INTRODUCTION
Notification of laboratory-confirmed cases of salmonellosis and notification of clinical cases of salmonellosis with an epidemiological link is mandatory in Germany. In May 2010, 11 cases of Salmonella enterica subsp. enterica, serovar Enteritidis (Salmonella Enteritidis) infections were notified to a district health office in Rhineland-Palatine. All cases were associated with a private barbecue on 1 May attended by 14 people.
Early information indicated that all barbecue guests had developed gastrointestinal symptoms and a cohort study was planned with the aims of describing the outbreak and burden of disease and identifying the outbreak vehicle in order to prevent further cases.
Salmonellosis is one of the most frequent causes of foodborne infections. In 2009, 841 outbreaks with 31 397 cases were notified in Germany [1]. The real number of infections is estimated to be much higher because many Salmonella infections are mild and self-limiting [Reference Angulo, Swerdlow and Saeed2]. Many affected persons do not visit a physician and therefore, these cases are not notified.
In Germany, S. Enteritidis accounted for 58% of all notified and serotyped Salmonella cases in 2009. Of all 665 S. Enteritidis isolates that were phage-typed by the National Reference Centre for Salmonella and other Bacterial Pathogens (NRC), 122 (18·3%) were identified as PT 8/7. This phage type is mainly associated with chicken eggs [Reference Rabsch3] and is not known for particularly high virulence [Reference Pang4] or pathogenicity [Reference Lu5].
Food monitoring in Germany in 2008 found Salmonella in 10·2% of all poultry meat samples and in 0·25% of all analysed eggs. S. Enteritidis accounted for 25% of all positive poultry meat samples and for 93% of all positive eggs [6].
Salmonellosis incubation time depends on the dose ingested as well as host factors and ranges from 6 to 72 h, the majority of cases occur within 12–36 h after ingestion [Reference Heymann7].
The infection results in diarrhoea, abdominal pain, nausea, headache and fever [Reference Hawker8]. Symptoms usually fade within 1–2 days [Reference Angulo, Swerdlow and Saeed2]. It is estimated that only up to 2% of non-typhoidal salmonellosis infections cause extra-intestinal infections [Reference Heymann7].
METHODS
Exploratory interviews
We conducted exploratory interviews via telephone with the hostess, three barbecue guests and one person who had prepared a salad but did not attend the barbecue himself. Information was gathered on the barbecue guests, the menu and the course of events during, before and after the party. Particular attention was given to possible sources of infection during the preparation of the party, food preparation and storage as well as kitchen hygiene.
Case definition
We defined a probable case as diarrhoea within 6–72 h of eating in a person attending the barbecue. A confirmed case was defined as a probable case with microbiological confirmation of S. Enteritidis in a stool sample.
The cohort study
We performed a retrospective cohort study for all persons who attended the barbecue.
A questionnaire was developed based on the exploratory interviews and the party menu. Data were collected on demographics, travel history, time of having the meal at the barbecue, symptom onset and duration, stool sampling and hospital admission. Incubation time was measured in hours, duration of symptoms in days.
Information on onset, type and duration of symptoms (diarrhoea, vomiting, abdominal pain/cramps, fever >38·5 °C) were collected as outcomes for severity of disease. Food dose was taken as level of exposure. For drinks, doses were defined as ‘one bottle/1 × 0·5 l’, ‘two bottles/2 × 0·5 l’, ‘3 or more bottles/ ⩾ 3×0·5 l’. For food, we asked if the barbecue guests had consumed a ‘tasting portion’, ‘a normal portion’, or ‘two or more portions’ of a dish.
The questionnaires and investigation team's contact details were distributed to the barbecue guests by the barbecue hostess via email. Follow-up calls were made until all guests who could be contacted returned their questionnaires.
Statistical analyses
Data were double-entered into an EpiData 3.1 file, cross-checked for inconsistencies and cleaned. Data were analysed using Stata v. 10.0 (StataCorp., USA).
Descriptive statistics were used to characterize the study population and to characterize the outbreak. Median with range and interquartile range (IQR) was calculated for the age of cohort members, incubation time and duration of symptoms.
The dose–response relationship of suspected food items was tested according to scale levels of exposure and outcome measures. Fisher's exact test was used to analyse the relationship between food item and hospital admission [Reference Kirkwood and Sterne9]. Wilcoxon rank sum tests were conducted to compare incubation times and durations of symptoms of individuals exposed to different doses of the suspected food item [Reference Kirkwood and Sterne9]. A P value of <0·05 was considered as significant.
Food traceback
As no food of the barbecue party was left over for testing, pasta of the same type and brand as the dried pasta used for preparing the salad incriminated by the epidemiological investigations was purchased from the same local shop for testing.
Laboratory investigations
The stool samples of barbecue guests, and of one person who had prepared a salad but did not attend the barbecue himself, as well as the pasta sample were investigated for Salmonella subspecies. They were cultured on standardized media and serotyped according to the guidelines for the detection of Salmonella species, issued by the German Institute for Standardization.
Isolates of a subset of patients were stored and phage-typed by the NRC according to the typing systems of Ward/Lalko & Laszlo, e.g. PT8/7, phage type 8 according to Ward et al. [Reference Ward, de Sa and Rowe10] and phage type 7 according to Laszlo et al. [Reference Laszlo, Csorian and Paszti11].
RESULTS
Exploratory interviews
The barbecue lasted from about 15:00 hours until well after midnight. According to the hostess, 14 persons attended the barbecue and all of them became ill with gastroenteric symptoms that night or the day after the party.
Guests started to eat between 15:00 and 22:00 hours. The food and drinks were brought by the guests and were laid on the buffet table without cooling.
A person who was supposed to attend the barbecue party had fallen ill the day before (30 April). He had prepared a vegetable pasta salad in the morning and developed gastroenteric symptoms within 3 h after salad preparation. He was hospitalized the next morning (1 May) and therefore did not attend the barbecue (Fig. 1).

Fig. 1. Course of events in an outbreak of Salmonella Enteritidis PT8/7 linked to a private barbecue in Rhineland-Palatinate, Germany, May 2010.
Nevertheless, his salad was served at the party. It was stored unrefrigerated for 23 h at approximately 20 °C before being served. The stored salad contained only pasta, tomatoes, peppers and cucumbers and was dressed with basic vinaigrette from oil and vinegar just shortly before consumption.
The cohort study
Cohort properties, attack rate
Information was available for 11 (five males, six females) of the 14 barbecue attendants. Ten guests returned cohort study questionnaires. Information on demographics, symptoms and hospitalization could be drawn from the notification data on one further guest. Median age was 27 years (range 21–28, IQR 23–28 years). All 11 cohort members met the case definition, nine were confirmed and two were probable cases, implying an overall attack rate of 100%.
Exposure measures: food and drinks consumed
Food consumption
Ten barbecue guests had provided information on food consumption.
Three different salads and various types of meat, bratwurst and drinks were served at the barbecue. Consumption patterns varied greatly because most guests enjoyed mainly their own food and drinks. Amounts of food and drink items that were consumed by three or more guests are given in Table 1.
Table 1. Amounts of food and drink items consumed by three or more barbecue guests in an outbreak of Salmonella Enteritidis PT8/7 linked to a private barbecue in Rhineland-Palatinate, Germany, May 2010
The vegetable pasta salad and another salad were the only food items eaten by all barbecue guests who returned the cohort questionnaire. Only the vegetable pasta salad was additionally linked to the non-participating person who was infected with the outbreak pathogen.
Outcome measures
Incubation times and symptoms
First symptoms occurred within 6–28 h (median 18, IQR 13–21 h) after starting to eat. All 11 cases had diarrhoea, four (36%) cases vomited, eight (73%) suffered abdominal pain/cramps and seven (64%) had fever >38·5 °C.
Eight (73%) cases suffered diarrhoea for ⩾6 days. In total, diarrhoea lasted from 2 to 14 days (Fig. 2) with a median of 6 (IQR 4–8) days and vomiting was suffered for 1–6 days with a median of 3 (IQR 1·5–5) days. Abdominal pain/cramps lasted for 2–14 days (median 6, IQR 4–11·5 days) and fever >38·5 °C lasted for 2–5 days (median 3, IQR 2–3 days). The maximum duration of overall symptoms for individuals was 2–14 days (median 7, IQR 4–9 days).
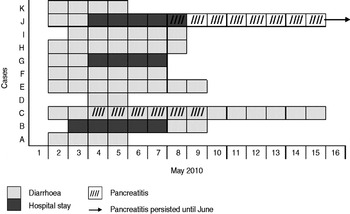
Fig. 2. Onset and duration of diarrhoea, hospital stay and pancreatitis in barbecue guests in an outbreak of Salmonella Enteritidis PT8/7 linked to a private barbecue in Rhineland-Palatinate, Germany, May 2010.
Hospital admission and complications (Fig. 2)
Three (27%) cases were hospitalized for 4–5 days (median 5, IQR 4–5 days). Two (18%) cases developed acute pancreatitis with epigastric pain and pancreatic enlargement. They recovered after 6 and 45 days, respectively.
Dose–response relationship
Dose–response relationship was calculated for the vegetable pasta salad, because it was the only food item that was linked to the non-participating person who was infected with the outbreak pathogen (Table 1).
All barbecue guests were cases and all of them had been exposed to the vegetable pasta salad. Therefore, relative risks or odds ratios could not be calculated.
Five barbecue guests had consumed a tasting portion and five had consumed a normal portion. One of the former and two of the latter were hospitalized (P = 1·00). Pancreatitis occurred in one guest who had eaten a tasting portion and one who had eaten a normal portion (P = 1·00). Median incubation times of both groups were similar (P = 0·81), but consuming higher doses was associated with a longer median symptom duration (7 days vs. 4 days, P = 0·11) (Table 2).
Table 2. Dose–response relationship for vegetable pasta salad in an outbreak of Salmonella Enteritidis PT8/7 linked to a private barbecue in Rhineland-Palatinate, Germany, May 2010
IQR, Interquartile range.
* Fisher's exact test.
† Wilcoxon rank sum test.
Laboratory results
Stool cultures, serotyping and phage-typing
S. Enteritidis was found in the stools of 9/11 barbecue guests and of the salad preparer. Two isolates were phage-typed and S. Enteritidis PT8/7 was identified in the stools of the preparer of the vegetable pasta salad and one barbecue guest.
Besides the barbecue outbreak cases, the Federal State Public Health Services and the NRC did not identify any other cases of S. Enteritidis PT8/7 in 2010 in the whole of Rhineland-Palatinate.
Food sample
There were no pathogens found in the pasta of the same brand purchased after the barbecue. The vegetables could not be traced back.
DISCUSSION
In this barbecue-associated, self-limited point-source outbreak we found a high attack rate and a high proportion of severe infections, hospitalizations and complications in young and otherwise healthy adults. The high attack rate in this outbreak is remarkable. Like incubation time, attack rates vary depending on inoculum size and host factors. In general, high infectious doses are required for a Salmonella infection. Risk assessment models suggest a 10–20% probability for infection with a dose of 102 organisms and a 60–80% probability for infection with a dose of 106 organisms [Reference Heymann7]. Considering that nobody in the barbecue cohort belonged to a particular risk group with increased susceptibility to Salmonella infection, the attack rate of 100% indicates a very high bacterial load of the vehicle of infection.
Some outbreaks due to non-typhoidal Salmonella subspecies with high attack rates (ARs) are described in the literature. In Spain, S. Enteritis (not phage-typed) caused gastrointestinal symptoms in 101/140 (AR 71%) children who had consumed a school canteen lunch [Reference Godoy12]. S. Enteritidis PT6 was the infectious agent in an outbreak linked to a children's birthday party in UK where 30/37 guests fell ill (AR 81%) [Reference Dodhia, Kearney and Warburton13]. In Australia, an outbreak of S. Typhimurium PTI35 affected 53/98 (AR 54%) guests at a local community dinner [14]. In Singapore, 55/94 (AR 59%) consumers of a canteen dinner were infected with Salmonella group E in a military camp [Reference Lee, Ong and Auw15]. S. Enteritidis PT21 caused gastrointestinal symptoms in 85/115 visitors (AR 74%) to a small fair in Austria [Reference Schmid16]. Like the barbecue outbreak, the last three outbreaks affected adults not belonging to specific risk groups and suggest high inoculum sizes.
In our barbecue outbreak, the most likely vehicle was the vegetable pasta salad, as all cases had eaten it and the person who had prepared it was infected with the same strain. He developed gastroenteric symptoms within only 3 hours after preparing the salad. Shedding of Salmonella in the prodromal phase of infection [17, Reference Todd18] and high infectious doses in food originally contaminated with low pathogen doses [Reference Frank19] has been reported.
The lack of other S. Enteritidis PT8/7 cases in the region during the outbreak period strengthens the evidence that the salad was contaminated during preparation and not by one of the ingredients contaminated further back in the farm-to-table chain.
Storing the salad at room temperature for 23 h allowed a substantial increase of bacterial load, which can explain the severe infections of all barbecue guests, none of whom belonged to a risk group for severe infections. Proliferation is inhibited or can be reduced by acidic pH values [Reference Entis20] but vinegar was only added to the salad shortly before serving.
The prolonged symptom duration of guests who had consumed normal portions compared to those who only tasted the salad may serve as an additional evidence for the vegetable pasta salad as the vehicle of the outbreak. The lack of statistical significance could be explained by the small cohort.
When interpreting the dose–response analysis, it should be considered that Salmonella usually multiply in clusters. Therefore, tasting portions may have contained high doses of bacteria, although the salad had been mixed thoroughly before serving.
We found a high proportion of cases with pancreatitis. Only a few case reports mention this complication of Salmonella infection. In a prospective study conducted in 1991, 22/31 hospitalized patients with S. Enteritidis infections had raised serum lipase activities (70%), abdominal ultrasound found pancreatic enlargement in 11 (35%) of these patients [Reference Renner, Nimeth and Demmelbauer21]. On the other hand, a prospective study from 2003 found only five (20%) of 25 hospitalized patients with S. Enteritidis infections to have raised serum lipase activities; ultrasound did not show morphological abnormalities of their pancreatic glands [Reference Pezzilli22].
Our study has several limitations. First, the lack of non-cases precludes the calculation of relative risks. We accounted for this constraint by testing associations between food exposure dose and hospitalizations as well as duration of diarrhoea and incubation times as alternative measures of association. Second, the small cohort size hindered any statistical test from reaching significance. Finally, no samples of consumed food were left over, and it was not possible to confirm the outbreak pathogen in the vegetable pasta salad directly.
CONCLUSIONS
Epidemiological and laboratory investigations provided consistent evidence that the vehicle for S. Enteritis PT8/7 was the vegetable pasta salad.
This outbreak shows that lack of basic food hygiene can cause serious infections in individuals not belonging to common risk groups. As a consequence of this outbreak, we will publish a press release with food hygiene recommendations for the general public for the beginning of the next barbecue season. The recommendations will include the discarding of food if the person who prepared it falls ill shortly afterwards.
Recommendations
This outbreak underscores the importance of proper kitchen hygiene and food storage in private settings. Food hygiene recommendations should be reiterated to the public at the beginning of the barbecue season by public health actors. Additionally, it should be emphasized that if a person develops gastroenteric symptoms shortly after preparing a meal, the food should be considered as potentially infectious and discarded.
ACKNOWLEDGEMENTS
We thank the barbecue guests and the salad preparer for their kindness in answering our questions and the staff of the local health authorities for their generous cooperation. Our thanks are also due to Manuel Dehnert, who supported the investigation with statistical advice.
DECLARATION OF INTEREST
None.





