1. Introduction
The putative association between cannabis use and suicidality has been a matter of debate in the literature. For example, the last report from the Institute for Health Metrics Science and Evaluation (IHME) group on the burden of mental and substance use disorders on deaths by suicide did not include cannabis use as a risk factor for suicide [Reference Ferrari, Norman, Freedman, Baxter, Pirkis and Harris1]. In addition, a recent review and meta-analysis found a lack of consistent evidence for an association between acute cannabis use and imminent suicidality [Reference Borges, Bagge and Orozco2]. Although an association between chronic cannabis use and suicidality was suggested, the credibility of the evidence was limited by heterogeneous definitions of exposure (e.g. any cannabis use, cannabis use disorder, chronic cannabis use, etc.) and outcome (i.e. suicidal ideation, suicide attempts and deaths due to suicide) variables across included studies [Reference Borges, Bagge and Orozco2]. Moreover, the proper controls for potential confounders which are known to be associated with suicide (e.g. environmental risk factors, mood disorders, other substance use disorders) were inconsistent across studies [Reference Borges, Bagge and Orozco2].
Another major gap in the literature is the paucity of studies that have assessed this association in samples derived from low- and middle-income countries (LMICs) [Reference Borges, Bagge and Orozco2]. This association may differ in magnitude in LMICs compared to high-income countries due at least in part to a complex interaction with relevant socio-demographic and environmental risk factors [Reference Breet, Goldstone and Bantjes3]. For example, poverty may comprise a particularly relevant risk factor for suicide across LMICs [Reference Iemmi, Bantjes, Coast, Channer, Leone and McDaid4]. Accordingly, the need to develop specific preventative public health policy interventions for suicide in LMICs is an unmet priority [Reference Jacob5].
Furthermore, a large body of evidence has suggested that cannabis use during adolescence may be particularly detrimental to brain development and to the emergence of psychopathology across the lifespan [Reference Lubman, Cheetham and Yucel6–Reference Chadwick, Miller and Hurd8]. It has also been suggested that cannabis use during adolescence may increase the risk of suicidality during both adolescence [Reference Borges, Bagge and Orozco2, Reference Borges, Benjet, Orozco, Medina-Mora and Menendez9, Reference Kokkevi, Richardson, Olszewski, Matias, Monshouwer and Bjarnason10] and adulthood [Reference Silins, Horwood, Patton, Fergusson, Olsson and Hutchinson11, Reference Clarke, Coughlan, Harley, Connor, Power and Lynch12].
Given these aforementioned gaps and inconsistencies in the literature, we set out to examine the patterns of associations between cannabis use and suicide attempts in a multinational sample of adolescents living in LMICs. We hypothesized that cannabis use could be associated with suicide attempts in this population, and that this association would be robust after multivariable adjustment for potential confounders.
2. Materials and methods
2.1. The survey
Publicly available data from the Global School-Based Student Health Survey (GSHS) were analyzed. Details on this survey can be found at http://www.who.int/chp/gshs and http://www.cdc.gov/gshs. Briefly, the GSHS was jointly developed by the WHO and the US Centers for Disease Control and Prevention (CDC), and other UN allies. The core aim of this survey was to assess and quantify risk and protective factors of major non-communicable diseases. The survey draws content from the CDC Youth Risk Behavior Survey (YRBS) for which test-retest reliability has been established [Reference Brener, Collins, Kann, Warren and Williams13]. The survey used a standardized two-stage probability sampling design for the selection process within each participating country. For the first stage, schools were selected with probability proportional to size sampling. The second stage involved the random selection of classrooms which included students aged 13–15 years within each selected school. All students in the selected classrooms were eligible to participate in the survey regardless of age. Data collection was performed during one regular class period. The questionnaire was translated into the local language in each country and comprised multiple choice response options; students recorded their response on computer scannable sheets. All GSHS surveys were approved, in each country, by both a national government administration (most often the Ministry of Health or Education) and an institutional review board or ethics committee. Student privacy was protected through anonymous and voluntary participation, and informed consent was obtained as appropriate from the students, parents and/or school officials. Data were weighted for non-response and probability selection.
From all publicly available data, we selected all nationally representative datasets that included all the variables included in this study. If there were more than two datasets from the same country, we chose the most recent dataset. Data from 21 countries were included in the current study. The characteristics of each country or survey including the response rates are provided in Table 1. For the included countries, the survey was conducted between 2009 and 2015, and consisted of 4 low-income, 11 lower middle-income, and 6 upper middle-income countries. Low-income countries were defined as those with an annual per capita gross national income (GNI) of 995 USD or less in 2017; lower-middle income countries are those with a GNI per capita between 996 and 3895 USD; and upper-middle income countries were those with an annual per capita GNI between 3896 and 12,055 USD. Those definitions were based on standard parameters from the World Bank.
2.2. Variables
2.2.1. Suicide attempt (dependent variable)
Suicide attempt was assessed by the question “During the past 12 months, how many times did you actually attempt suicide?” and was defined as at least one suicide attempt in the past 12 months.
2.2.2. Cannabis use (independent variable)
Past 30-day and lifetime cannabis use was assessed with the question “During the past 30 days (or during your life), how many times have you used marijuana?” Country-specific slang terms for marijuana were also included in the question. Marijuana use was defined as having used marijuana on at least one day in the past 30 days (past 30-day cannabis use) or ever having used marijuana (lifetime cannabis use).
2.2.3. Control variables
The selection of control variables was based on past literature [Reference Borges, Bagge and Orozco2] and included age, sex, food insecurity, alcohol consumption, amphetamine use, smoking and anxiety-induced insomnia. Food insecurity was used as a proxy for socioeconomic status as there were no variables on socioeconomic status in the GSHS. Also, anxiety-induced insomnia was considered a proxy of psychiatric disorders as there were no variables on psychiatric disorders including depression in the dataset. Food insecurity was assessed by the question “During the past 30 days, how often did you go hungry because there was not enough food in your home?” Answer options were categorized as ‘never’, ‘rarely/sometimes’, and ‘most of the time/always’. Alcohol consumption was defined as having had one drink containing alcohol for at least one day in the past 30 days. Amphetamine use was defined as having used amphetamines (metamphetamines) at least once in life. Smoking was defined as having smoked at least on one day during the past 30 days. Anxiety-induced insomnia was defined as replying ‘most of the time’ or ‘always’ to the question “During the past 12 months, how often have you been so worried about something that you could not sleep at night?”
2.3. Statistical analysis
Statistical analyses were performed with Stata 14.1 (Stata Corp LP, College station, Texas). The analysis was restricted to those aged 12–15 years. Age-sex adjusted prevalence of cannabis use by country were calculated using the proportions derived from the overall sample as the standard population. We used multivariable logistic regression analysis to estimate the association between past 30-day and lifetime cannabis use (independent variable) and suicide attempt (dependent variable). We constructed six models to assess the influence of the inclusion of different variables on the association between cannabis use and suicide attempts. Specifically, a base model which adjusted only for sociodemographic factors (age, sex, food insecurity, country) was constructed. Subsequently, we added alcohol consumption, amphetamine use, smoking, and anxiety-induced insomnia individually in the base model. Finally, we adjusted for all the above-mentioned variables (fully adjusted model). Adjustment for country was done using fixed effects models as in a previous GSHS study [Reference Vancampfort, Stubbs, Firth, Van Damme and Koyanagi14]. We also tested for interaction by sex in terms of the association between cannabis consumption and suicide attempt by including the product term “sex X cannabis use” in the fully adjusted model. All variables were included in the regression analysis as categorical variables with the exception of age (continuous variable). Sampling weights and the clustered sampling design of the surveys were taken into account to obtain nationally representative estimates. Results from the logistic regression analyses are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The level of statistical significance was set at p<0.05.
3. Results
The final sample consisted of 86,254 adolescents aged 12–15 years with a mean (SD) age of 13.7 (0.9) years and 49.0% were females. The overall age- and sex- adjusted prevalence of past-30 day and lifetime cannabis use were 2.8% [range 0.5% (Laos) to 37.6% (Samoa)] and 3.9% [range 0.5% (Laos) to 44.9% (Samoa)], respectively (Tables 1 and 2, Fig. 1). The overall prevalence of suicide attempts was 10.1%. The association between cannabis use and suicide attempt estimated by multivariable logistic regression is shown in Table 3. In the model adjusted only for sociodemographic factors (i.e., age, sex, food insecurity, country), past 30-day cannabis use was associated with a 9.64 (95% CI = 7.36–12.61) times higher odds for suicide attempts. The inclusion of alcohol consumption, amphetamine use, smoking, and anxiety-induced insomnia in the model attenuated the OR with the largest attenuation observed with amphetamine use followed by smoking. After adjustment for all potential confounders, past 30-day cannabis use was associated with a 2.03 (95% CI = 1.42–2.91) times higher odds for suicide attempts. The results for lifetime cannabis use were similar with the OR (95% CI) of the fully adjusted model being 2.30 (1.73–3.04). There were no significant interactions by sex in the association between cannabis use and suicide attempts.
Table 1 Country and survey characteristics.

Abbreviation: L Low income; LM Lower middle income; UM Upper middle income; H High income.
a Response rate was calculated as school response rate multiplied by student response rate.
b Country income level was based on the World Bank classification at the year of the survey in the respective countries.
c Based on sample aged 12–15 years.
d Age- and sex-adjusted.
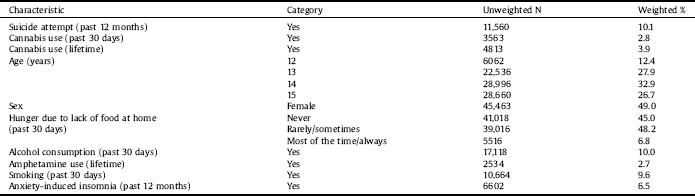
Table 2 Sample characteristics.

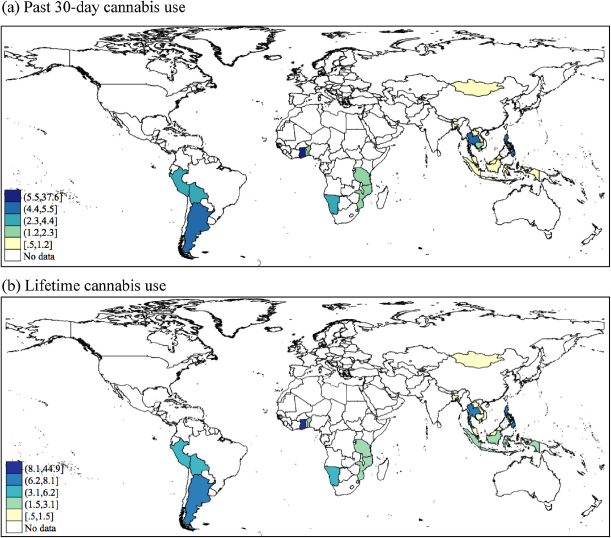
Fig. 1. Age and sex-adjusted prevalence of (a) past 30-day and (b) lifetime cannabis use.
Table 3 Association between cannabis use and suicide attempts estimated by multivariable logistic regression.

Data are odds ratio [95% confidence interval].
a Base model is adjusted for sociodemographic factors (i.e., age, sex, food insecurity, country).
b Fully adjusted model is adjusted for age, sex, food insecurity, country, alcohol consumption, amphetamine use, smoking, and anxiety-induced insomnia.
* P < 0.001.
4. Discussion
Although both cannabis use and suicide attempts are highly prevalent among adolescents in our samples, some geographical variations are worth mentioning. This is consistent with evidence that points to the high burden attributed to suicide and substance use disorders in youths living both in upper-income countries and in LMICs [Reference Erskine, Moffitt, Copeland, Costello, Ferrari and Patton15]. Our findings also suggest that any cannabis use during the past 30 days or during lifetime are associated with a greater likelihood of suicide attempts. Furthermore, these associations remained robust and significant after adjustment for relevant confounders including the use of other substances and socio-demographic variables. Those results are in accordance to previous school-based reports [Reference Borges, Benjet, Orozco, Medina-Mora and Menendez9, Reference Kokkevi, Richardson, Olszewski, Matias, Monshouwer and Bjarnason10, Reference Zarrouq, Bendaou, Elkinany, Rammouz, Aalouane and Lyoussi16]. However, previous studies were predominantly conducted in high-income countries and there is a lack of multinational studies of this kind [Reference Borges, Bagge and Orozco2], with the exception of the survey conducted by Kokkevi et al. [Reference Kokkevi, Richardson, Olszewski, Matias, Monshouwer and Bjarnason10] which included a school-based sample derived from 16 European countries, and found that any cannabis use in the past 30 days was significantly associated with suicide attempts among adolescents. However, after adjusting to potential confounding variables the magnitude of the association (OR = 1.47; 95%CI: 1.18–1.58) [Reference Kokkevi, Richardson, Olszewski, Matias, Monshouwer and Bjarnason10] appeared somewhat smaller than the one observed in this study (OR = 2.03; 95%CI: 1.42–2.91). The current study fills a gap in the literature as it examines the association of cannabis use and suicide attempts in a multinational sample of adolescents attending schools across 21 LMICs.
The associations between cannabis use and suicide attempts were attenuated after adjustment to alcohol use and particularly after multivariable adjustment to smoking and amphetamine consumption. Those findings are consistent with previous studies and reviews that indicate that the use of alcohol or other drugs may decrease the magnitude of the association between cannabis use and suicidality [Reference Borges, Bagge and Orozco2, Reference Kokkevi, Richardson, Olszewski, Matias, Monshouwer and Bjarnason10, Reference Degenhardt, Ferrari, Calabria, Hall, Norman and McGrath17, Reference Degenhardt and Hall18].
Delta-9-tetrahidrocannabinol (THC) and cannabidiol (CBD) are the two main ingredients in cannabis [Reference Boggs, Nguyen, Morgenson and Taffe19]. THC is thought to be the main responsible for the addictive properties of cannabis and the resulting subjective euphoria, anxiety/dysphoria, and cognitive effects. On the other hand, CBD has anxiolytic effects and may also mitigate some psychoactive effects related to THC although there are some discrepancies across studies [Reference Boggs, Nguyen, Morgenson and Taffe19, Reference Rong, Lee, Carmona, Cha, Ragguett and Rosenblat20]. Nevertheless, differences in the relative concentrations of THC and CBD in different strains of cannabis may contribute to the associations herein reported, and hence may also partly explain differences observed across geographic regions.
4.1. Strengths and limitations
The main strengths of the current study include the enrollment of the largest sample of adolescents (86,254) to date on this topic and its multi-national scope. Most research that had previously examined this association derives from Western countries [Reference Borges, Bagge and Orozco2, Reference Breet, Goldstone and Bantjes3], while this study provides data from many LMICs. However, our findings should be interpreted in light of some limitations. First, as with many other school-based surveys, this is a cross-sectional study, and hence the direction of causality cannot be established. Second, evidence indicates that chronic cannabis use may be associated with the development of depressive disorders [Reference Lev-Ran, Roerecke, Le Foll, George, McKenzie and Rehm21]. Evidence suggests that anxiety and insomnia are strongly related to depression in adolescents [Reference Roberts and Duong22, Reference Johnson, Roth and Breslau23]. We adjusted our findings for the presence of anxiety-induced insomnia, which to a certain degree may thus proxy the presence of depression. Consistently, anxiety-induced insomnia was also associated with suicide attempts across samples from all examined geographical regions. This finding is consistent with previous evidence which suggests that sleep disturbances and particularly insomnia could be associated with suicidal behaviors [Reference Pigeon, Pinquart and Conner24, Reference Pompili, Innamorati, Forte, Longo, Mazzetta and Erbuto25]. However, the lack of control for the presence of depression is a main limitation of the current work. Third, we controlled our findings to the use of other substances (e.g. alcohol). However, the use of alcohol in the past 30 days may not necessarily reflect the presence of problematic drinking or an alcohol use disorder. Fourth, although food insecurity is closely related to socioeconomic status [Reference Cook, Black, Chilton, Cutts, Ettinger de Cuba and Heeren26, Reference Pai, Kandasamy, Uleryk and Maguire27], a more comprehensive measure of socioeconomic status could have been more appropriate. Finally, our findings are based on self-reported data. Nevertheless, it has been demonstrated that anonymous self-report questionnaires may elicit more valid data on sensitive issues compared to other methods in this age group [Reference Safer28].
4.2. Implications
The strong and independent associations between cannabis use and suicide attempts in a large sample of adolescents from 21 LMICs herein reported open relevant research and clinical implications. First, the causality of this association warrant confirmation in subsequent prospective and Mendelian Randomization studies [Reference Katikireddi, Green and Taylor29]. Our findings suggest that cannabis use should be taken into consideration when assessing suicide risk in adolescents particularly those living in LMICs. In addition, the current findings may inform preventative public health interventions targeted at adolescents at-risk for suicide residing in LMICs.
4.3. Conclusions
In conclusion, our findings point to a significant association between cannabis use and suicidal attempts among adolescents attending schools in disparate world regions. Cannabis use should be taken into account in the prevention and assessment of suicidal behaviors in adolescence. For example, universal, school-based interventions may be effective for the prevention of risk behaviors including cannabis use among the youth [Reference MacArthur, Caldwell, Redmore, Watkins, Kipping and White30]. Furthermore, these potential risks should be taken into account during the ongoing international debates around legalization of recreational cannabis use. However, the causality of the association herein reported warrants confirmation in large-scale prospective and Mendelian randomization studies.
Funding
AK’s work was supported by the Miguel Servet contract financed by the CP13/00150 and PI15/00862 projects, integrated into the National R + D + I and funded by the ISCIII - General Branch Evaluation and Promotion of Health Research - and the European Regional Development Fund (ERDF-FEDER). BS is supported by Health Education England and the National Institute for Health Research ICA Programme Clinical Lectureship (ICA-CL-2017-03-001). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available in the Global school-based Student Health Survey repository, available at: http://www.who.int/ncds/surveillance/gshs/country/en/.
Authors’ contributions
AFC and AK wrote the first draft of the manuscript. AK conducted data analysis. All authors have contributed to the interpretation of the data and have provided meaningful intellectual contribution. All authors read and approved the manuscript prior to submission.
Ethics approval and consent to participate
Ethical approval was obtained from ethical boards at each study site. Participants give written informed consent. Details are available at: http://www.who.int/ncds/surveillance/gshs/country/en/.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.eurpsy.2018.10.006.






Comments
No Comments have been published for this article.