No CrossRef data available.
Article contents
Resistance or pseudo-resistance?
Published online by Cambridge University Press: 01 September 2022
Abstract
Treatment-Resistant Depression continues to represent a great challenge for clinicians.
We investigated patients with history of resistance, assessing prognostic factors, response to treatments, and remission over time.
We recruited 202 unipolar and bipolar depressed inpatients. According to anamnestic backgrounds, patients were assigned to: A) Non-resistant: responders, with no characteristics of resistance in the current episode. B) Resistant: resistant to two antidepressant trials of adequate doses and duration. C) Pseudo-resistant: non-responders, not classifiable as Resistant because of inadequate trials. During hospitalization, patients were treated by clinical judgment, following a rehabilitation program.
| Table 1 | ||||
|---|---|---|---|---|
| Non-resistant (111) | Resistant (54) | Pseudo-resistant (35) | p-value | |
| Age | 59.1±11.9 | 63.0±12.6 | 57.0±11.3 | 0.036* |
| Episodes of illness | 3.8±2.1 | 4.0±1.9 | 3.0±1.8 | 0.036* |
| Personality disorders | 27.0% | 18.9% | 48.6% | 0.009** |
| Therapies: | 0.014** | |||
| SSRI | 62.4% | 40.4% | 69.7% | |
| SNRI | 19.8% | 42.3% | 15.1% | |
| TCA | 17.8% | 17.3% | 15.1% | |
| Augmentation | 24.3% | 38.9% | 17.1% | 0.05** |
| Remission | 76.5% | 59.5% | 81.2% | CvsB:0.045** CvsA:0.587** |
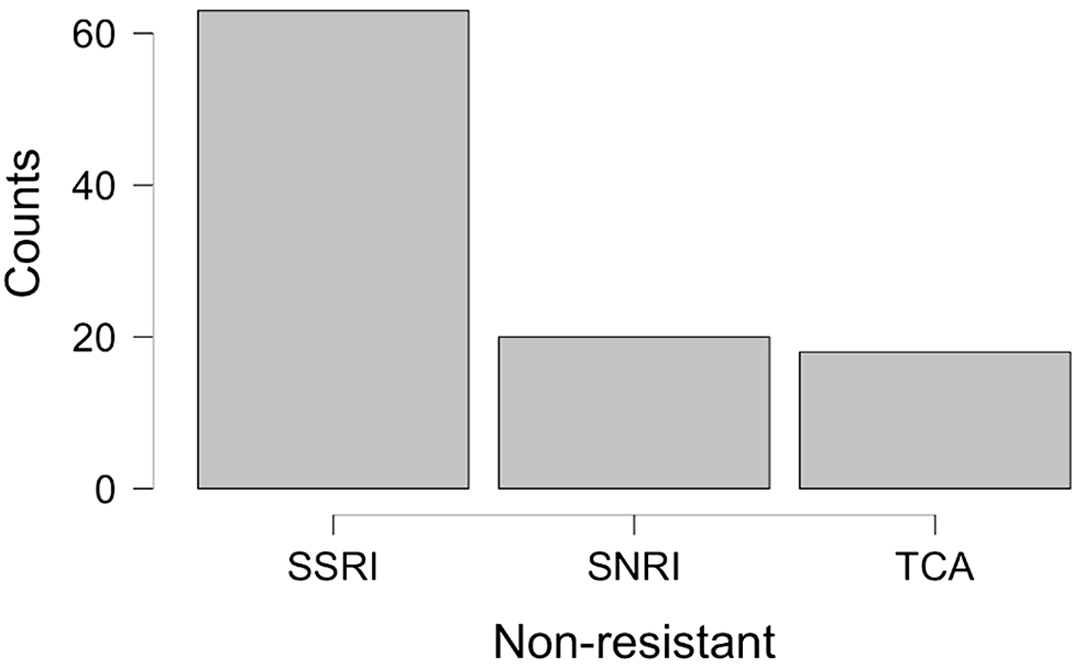
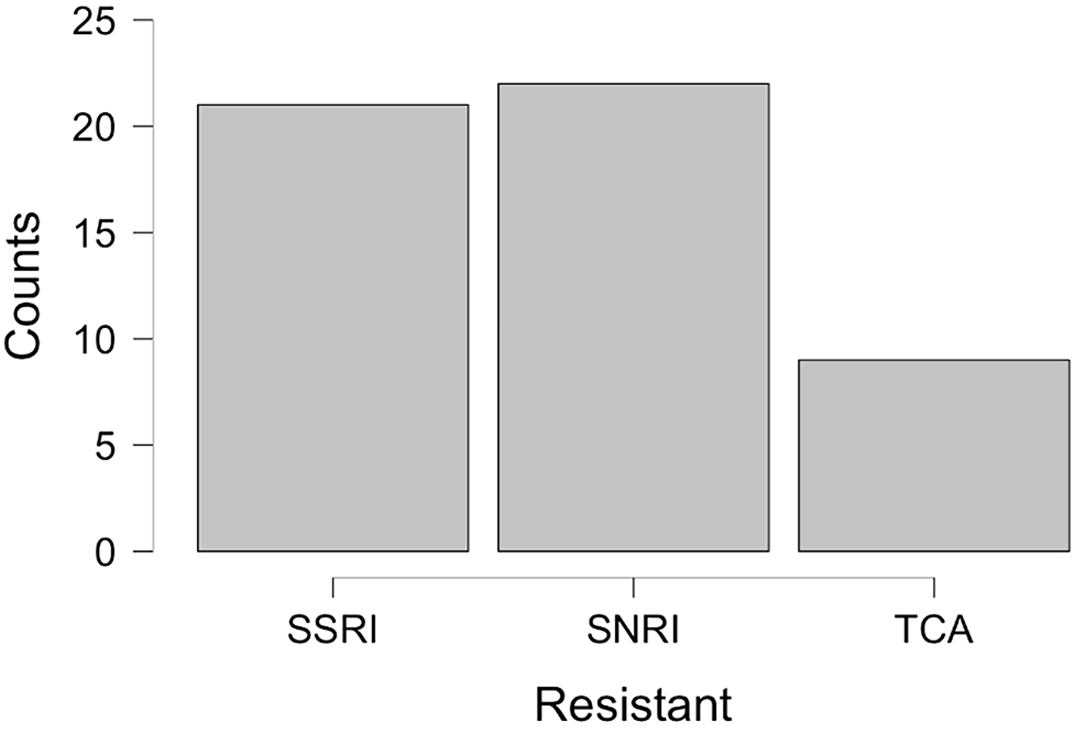
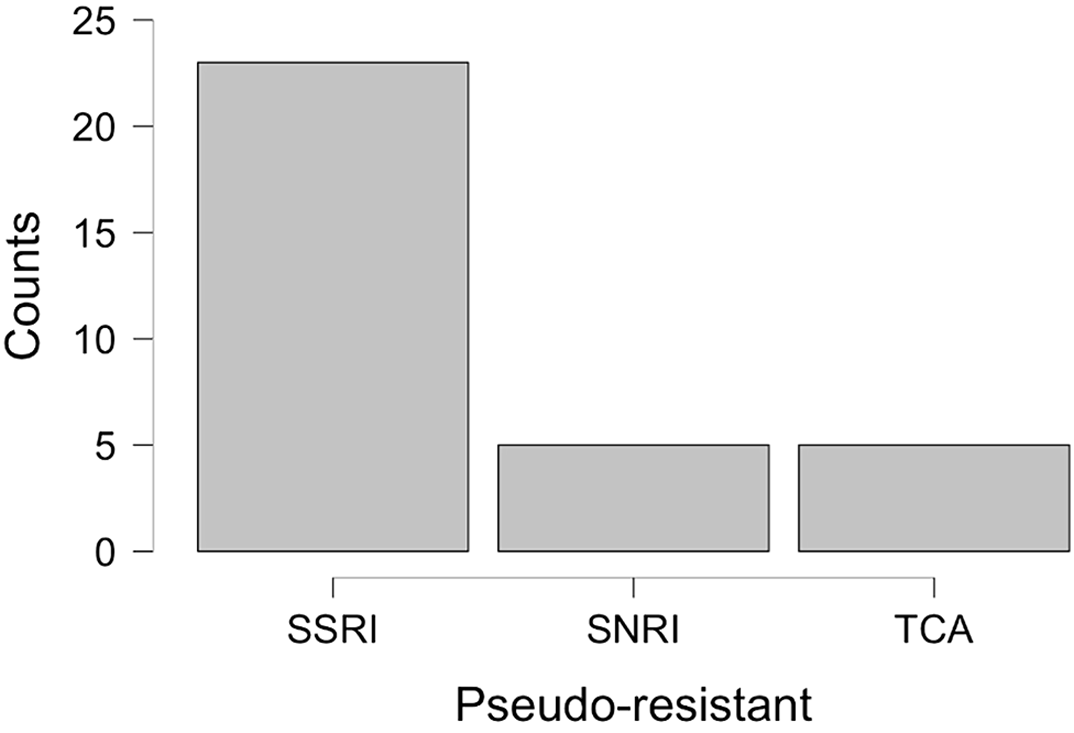
On the day of admission, non-responders were 44.5% of the sample, but 39.3% of them did not meet the Resistant criteria, defining the Pseudo-resistant group. Pseudo-resistant differed from others by younger age, fewer illness episodes, higher rate of personality disorders, and different therapies during hospitalization [Fig.1,2,3]. Pseudo-resistant remission rate, significantly greater than Resistant one, was comparable to Non-resistant [Tab.1]. *Kruskal-Wallis Test **Chi-Squared Test
This study outlines a new group of depressed patients that, apparently drug-resistant, displays the same outcome as responders when treated with first-line drugs during hospitalization, certainly taking benefit from the psychoeducational program. Quick recognition of these patients could be crucial to giving optimal care.
No significant relationships.
- Type
- Abstract
- Information
- European Psychiatry , Volume 65 , Special Issue S1: Abstracts of the 30th European Congress of Psychiatry , June 2022 , pp. S370 - S371
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2022. Published by Cambridge University Press on behalf of the European Psychiatric Association



Comments
No Comments have been published for this article.