1. Introduction
While health systems across the globe are still struggling with COVID-19, politicians and health policy scholars are already referring to the future, post-pandemic world, and how health systemsFootnote 1 should enhance their pandemic preparedness. Questions are raised about health system resilience; that is, a system's capacity to absorb, adapt and transform in response to crises (Thomas et al., Reference Thomas, Sagan, Larkin, Cylus, Figueras and Karanikolos2020). Particular attention is paid to public health, and its relationship to hospital facilities. In this paper we seek to demystify – that is, describe, contextualize and qualify – the debate on health system resilience by investigating how health systems in Germany, the Netherlands and Sweden have been able to accommodate and, in some ways, also shaped the COVID-19 crisis. By conducting a comparative institutional analysis, we study the ability of the German, Dutch and Swedish health care systems to respond to and learn from a virus outbreak.
In a first step, we critically re-examine the concept of health system resilience and point out its tendency to stress flexibility and coping with risks while ignoring the inertia of national institutional settings. Drawing from institutional theory, we then recapitulate the origins of health system institutions, including the historical (co)evolution of public health and health care (Trein, Reference Trein2018) in each country. This allows us to identify both the path dependencies in health system development (e.g. the dominance of health care over public health; the specific ways in which testing has been organized) and potential inroads to leveraging resilience (e.g. loosely integrated public health agencies). We expect that policy makers' options to foster health system resilience vary due to respective national institutional heritage, for instance, possibilities to steer the system towards collaboration across sectors. Keeping in mind the backdrop of inherited institutional settings, we will, third, present empirical findings about the countries' most characteristic bottlenecks during the COVID-19 crisis to learn how health systems both evoke certain constraints and enable specific solutions (and not others) due to their institutionalized settings. This will lead us, fourth, to country-specific pathways and impasses to stimulate future health system resilience. By analysing bottlenecks in three countries, we aim to develop a conceptual lens to studying health system resilience. The question guiding this research is: What bottlenecks in their national health systems did Germany, Sweden and the Netherlands encounter in combatting the COVID-19 crisis, how have these bottlenecks been managed, and what lessons can we draw from this in terms of health system resilience?
1.1 Examining the concept of health system resilience from an institutional theory lens
Health system resilience, a relatively young research concept that emerged in the aftermath of the Ebola epidemic in 2014 (Fridell et al., Reference Fridell, Edwin, von Schreeb and Saulnier2020), has a strong practical appeal to policymakers. In essence, it is defined by health systems' “ability to prepare for, manage (absorb, adapt and transform) and learn from shocks” (Thomas et al., Reference Thomas, Sagan, Larkin, Cylus, Figueras and Karanikolos2020: 5). In similar vein, others describe health systems resilience by their inbuilt capacity to “bounce back” and “continue to function” (Turenne et al., Reference Turenne, Gautier, Degroote, Guillard, Chabrol and Ridde2019: 177) in reaction to crises. Hence, the concept puts a strong emphasis on systems' coping strategies and assumes that ‘building back better’ is possible if policymakers respond effectively to shortcomings that manifest during times of crisis such as COVID-19. Following the inherited logic of health system resilience, managing a public health crisis requires to productively deal with different stages within a shock cycle: (i) preparedness of health systems to shocks, (ii) shock onset and alert, (iii) shock impact and management and (iv) recovery and learning. Thereby, each stage provides opportunities for enhancing resilience (Thomas et al., Reference Thomas, Sagan, Larkin, Cylus, Figueras and Karanikolos2020: 8) by means of informed interventions and organizational arrangements. As suggested, health systems' actual “capacity to manage resilience” (Blanchet et al., Reference Blanchet, Nam, Ramalingam and Pozo-Martin2017: 432) depends on the extent systems are able to manage key dimensions such as knowledge, uncertainties, interdependence and legitimacy. Accordingly, resilient governance of health systems is characterized by “absorptive, adaptive or transformational capacity in the face of shocks of different intensity” (Blanchet et al., Reference Blanchet, Nam, Ramalingam and Pozo-Martin2017: 434).
The concept of resilience has also been criticized, however, as it assumes a general ‘good’ of how a (health) system can or should respond, instead of a situated and hence contextualized matter – e.g. what might have worked on a system level in the first wave, in which intensive care departments were overflown, might not be effective in the fourth wave when health and societal problems had become more dispersed. Hence, we will also argue in this paper, resilience is contextualized and time specific and is about the ability of health systems to respond to and accommodate emerging crises. Furthermore, we share the criticism that the resilience concept does not sufficiently consider power and structural factors due to its tendency to understand health system resilience as an apolitical outcome (Topp, Reference Topp2020: 3). Therefore, we suggest connecting the notion of resilience to institutional theory to be able to better explain health systems' (in)ability to act in a specific way.
Institutional theory traditionally focuses on institutions' ‘stickiness’ or resistance to change and provides explanations for the governance decisions being made by specifying the rules, power structures and procedures of policymaking (Peters, Reference Peters and Bevir2011). Referring to the governance of health systems, the historical development and country-specific layering of institutions must be considered in order to evaluate and assess the implementation of resilience-oriented policies. For example, from a national health system perspective, it makes a difference whether a country pursues a cross-sectorial public health policy (such as Sweden) that distributes public health responsibilities across health system levels and institutions (Burström and Sagan, Reference Burström, Sagan and Rechel2018), or whether public health and health care are delineated by unequally organized (and hence unequally strong and effective) sectors, as is the case in Germany. While the trivial insight according to which ‘institutional frameworks matter’ tends to be side-lined by health system resilience research, resilient governance to a great extend depends on the design of national health system institutions. In fact, the actual meaning of health system resilience is highly related to health systems' institutional heritage and path dependencies (Hall and Taylor, Reference Hall and Taylor1996). Perceived as a form of policy learning, the ability to demonstrate resilience “must be assessed in the context of the interests and intentions of health system actors and the ways in which they mobilize and channel their power” (Topp, Reference Topp2020: 3). Thus, by taking COVID-19 as an example, the strengthening of health systems' public health pillar cannot be seen as an inevitable response to the crisis. Instead, with a view on the distribution of power and decision-making resources among public health and health care stakeholders and “ways in which historical choices have become institutionalized” (Bal et al., Reference Bal, de Graaff, van de Bovenkamp and Wallenburg2020: 672), lessons learnt from the pandemic could take various forms. From an institutional theory lens, resilience-oriented policy action may lead to a stronger role of the hospital sector in the governance of the health system and increased financial support for intensive care units which played a key role in the treatment of COVID-19 patients, rather than strengthening public health policies and organizations. In this scenario, health systems would not fundamentally change but rather ‘bounce back’ in a predictable way that reflects the historically evolved balance of power among institutions and stakeholders. In contrast, the full breadth of the health system resilience concept implies also “significant changes to the system that are a legacy of the shock” (Thomas et al., Reference Thomas, Sagan, Larkin, Cylus, Figueras and Karanikolos2020: 10). In order to implement this far-reaching vision of resilience, no less than health system renewal by means of policy change would be required. In addition, one could argue that it does not necessarily help to prevent or combat future and yet unknown crises that may appear in a totally different form, ensuing other problems. Nevertheless, the COVID-19 crisis might strengthen already existing changes or could be taken up to repair existing weaknesses in health systems.
As argued by political scientists, explanations of policy change have to be based on a nuanced theoretical understanding of the policy process (Knill and Tosun, Reference Knill and Tosun2020). Apparently, the latter is not stimulated by a rather simplistic health system resilience framework that does not perceive policy change as a political, and therefore, contingent process. Policy change emerges due to the interplay between perceived problem structures (e.g. the different interpretations of the COVID-19 crisis) and situational aspects (i.e. constellations of institutions, actors and policy instruments within a given health system). Consequently, it can hardly be explained causally by apolitical terms such as ‘recovery and learning’ but requires a more analytical focus of the policy process and the institutionalized setting in which problems and crises occur. In this paper, we examine the resilience capacity of health systems in Germany, Sweden and the Netherlands by studying the various bottlenecks that these health systems encountered during the first phase of the pandemic (mainly focusing on the year 2020). Bottlenecks are defined here as those situations in which existing institutional structures prevent to respond to or even create systemic problems during a crisis. The ability of health systems to deal with bottlenecks provides an analytical lens on health system resilience. Characteristically, bottlenecks are not ‘policy failures’ but systemic weaknesses or ‘soft spots’ that could be compensated (or even left unnoticed) in times of stability but become problematic in crisis. Importantly, bottlenecks are country- and health system specific as they are not a universal consequence of the pandemic (even if they become highlighted by emerging characteristics of COVID-19) but, first of all, relate to the institutionalized setting of the health system. Furthermore, bottleneck assessment and management may change over time and do not automatically spur health system resilience. During a pandemic some bottlenecks may soften (even if they are still present), while additional ones that are already moored in health systems' institutional setting may show up. In this paper, we shed light on the features and management of bottlenecks within the three health systems as this provides insight in their resilience capacity.
After a short description of methods in the next section, we first briefly explain the institutional contexts of the health systems in Germany, Sweden and the Netherlands. In a second step we provide a brief description of six bottlenecks (two per country), as they emerged during the COVID-19 pandemic. Third, we analyse from a comparative perspective how health systems have managed these bottlenecks and whether we can explain these responses by referring to the institutionalized characteristics of national health systems. Based on this analysis, we also address the question whether the crisis may trigger institutional change in the governance of the German, Dutch and Swedish health system: Are there first signs and indicators towards a focus on (post)pandemic preparedness and resilience?
2. Methods
The empirical findings presented in the three country case studies are based on references to academic and grey literature as well as interviews with regional and national health system experts. Interviews emanated from ongoing projects in the three countries. Interviewees (anonymously referenced in the country sections) were selected by drawing from personal contacts and expert recommendations. In total 15 interviews (i.e. Germany 6; the Netherlands 6; and Sweden 3) were conducted, transcribed and analysed by the authors. All interviews are based on a jointly agreed content guideline including topics such as the institutional setting of the national health system, health system governance, experienced bottlenecks during different waves of the pandemic, lessons learned regarding these bottlenecks and applied actions concerning pandemic preparedness, and resilience. Through joint deliberations, we selected six bottlenecksFootnote 2, two for each country: public health services and nursing home care in Germany; testing and nursing home care in Sweden; and intensive care capacity and testing in the Netherlands. These bottlenecks were repeatedly mentioned by the interviewees and in national policy debates, and widely covered in the media and policy documents. Based on the collected data, ‘thick descriptions’ (Geertz, Reference Geertz1973) were made for each of the bottlenecks that were then discussed between the authors for analysis. It is noteworthy that the identified bottlenecks were not the only ones encountered but very much prominent in the specific countries over longer periods of time. They typically reflect the struggles countries still face in preparing their systems for future/next phase of the pandemic.
2.1 Health systems' institutional backgrounds
Germany, Netherlands and Sweden were chosen because of their different health systems that despite similarities are based on distinct prevalent organizational and financing models (Toth, Reference Toth2021). The three countries have rather high developed health care sectors, and have experienced market-oriented reforms as well as a broader trend of decentralization and managerialization in the past three decades, yet in different manners (Saltman et al., Reference Saltman, Busse and Figueras2006; Pavolini, Reference Pavolini, Klenk and Pavolini2015). They similarly witnessed the outbreak of the pandemic in Italy in February 2020, and had (at least in theory) some preparation time to respond to the domestically unfolding crisis. This occurred in different and path-dependent manners, which can be explained by the institutionalized characteristics of national health systems, ensuing different policy outcomes.
The German health system is traditionally characterized by multi-level governance structures providing health policy stakeholders ample leeway for self-organization in the shadow of the state. Both features are key for a corporatist health system which is regulated at arms' length by state authorities (Busse and Blümel, Reference Busse and Blümel2014). The heart of the German health system is the Statutory Health Insurance (SHI) that is financed by employers' and employees' social security contributions. In general, competences to govern the German health system are unevenly distributed among a plethora of actors at the federal, state and regional level. While market- and competition-oriented reforms recalibrated health care providers' incentives in the last two decades, the Bismarckian nature of the German Gesundheitswesen, i.e. its conservative and corporatist features, has been retained. Traditionally, this institutional setting is accompanied with a clear-cut distribution of power according to which the health care sector prevails over other sectors such as social care, long-term care and public health which lack leverages and resources to pursue their interests. In consequence, doctors and hospitals are the main reference point of health policy and policymakers. Thus, the welfare and functioning of the health care sector, that is only loosely coordinated with other health-related sectors, absorb public attention and is often wrongly equated with the German health system at all.
The hallmarks of the Swedish health system are its solidaristic, tax-based financing structure, and the predominantly public provision of care services, typifying a classic social-democratic welfare state. The health system is highly decentralized and administered variously at the national, regional and municipal level. Health care, including public health, is predominantly funded and administered at the regional level by the 21 independent regions, each with their own locally elected political assemblies with the right to levy taxes (Blomqvist and Winblad, Reference Blomqvist, Winblad, Immergut, Andersen, Devitt and Popic2021). While the central government establishes basic principles and legal frameworks for the whole country (most importantly as set forth by the Health and Medical Service Act), hospitals, primary care centres and public health services are funded and operated by the regions. Social care, including nursing homes and in-home care, is provided at the municipal level. Although all nursing homes are publicly financed, approximately 20.5% of nursing homes are run by private actors (Spangler et al., Reference Spangler, Blomqvist, Lindberg and Winblad2019). Due to the largely decentralized character of the health care system governance between the national government and the regions relies on negotiation and collaboration (Fredriksson, Reference Fredriksson2012). At the national level, public health including infection control and protection against communicable diseases is primarily the responsibility of the Public Health Agency (PHA). The more practical public health and health promotion work (i.e. vaccination, child care programmes and preventive measures such as smoking cessation) is largely integrated with the primary health care system at the regional level (Rechel, Reference Rechel2018). Health protection in terms of infection control is however the responsibility of a separate organizational unit within the regions; the regional infectious disease units. Infection control physicians (Smittskyddsläkare) are appointed in each of the 21 regions and have had a central role in determining local restrictions and informing citizens about the disease (Winblad et al., Reference Winblad, Swenning and Spangler2021).
The Netherlands, finally, is usually characterized as a social health insurance system. However, in the past 25 years, the Dutch health system has moved into a layered system of financing, organizing and providing health care (Helderman et al., Reference Helderman, Schut, van der Grinten and van de Ven2005; van de Bovenkamp et al., Reference van de Bovenkamp, de Mul, Quartz, Weggelaar-Jansen and Bal2014). Although the corporatist nature of the Dutch health care system is still highly visible (i.e. professional, provider and patient associations play an important role in health care policymaking), the health system has also gone through some major reforms of decentralization and marketization. The Dutch health system basically consists of three institutionalized components or ‘sub-systems’, regulated by different laws and financed through distinct financial schemes: public health; primary and hospital care; and long-term and social care. Public health is regulated through the Public Health Act and is carried out by regional health care agencies (Gemeentelijke Gezondheids Dienst, GGD) and governed by (collaborating) municipalities. Furthermore, a National Expert Center for Infectious Disease (as part of the National Institute for Public Health and the Environment, Rijksinstituut voor Volksgezondheid & Milieu, RIVM) monitors the spread of infectious diseases and is responsible for the national vaccination programme. Secondly, primary care and hospital care have faced market-oriented reforms since the mid-2000s. Since 2015, municipalities have become responsible for organizing and purchasing care assistance – also seeking to come to a more integrated approach of health and social care. Long-term care, finally, is governed by non-competing health insurers that purchase care (e.g. nursing home care, care for the mentally and physically handicapped) for licensed citizens in their region.
3. Findings
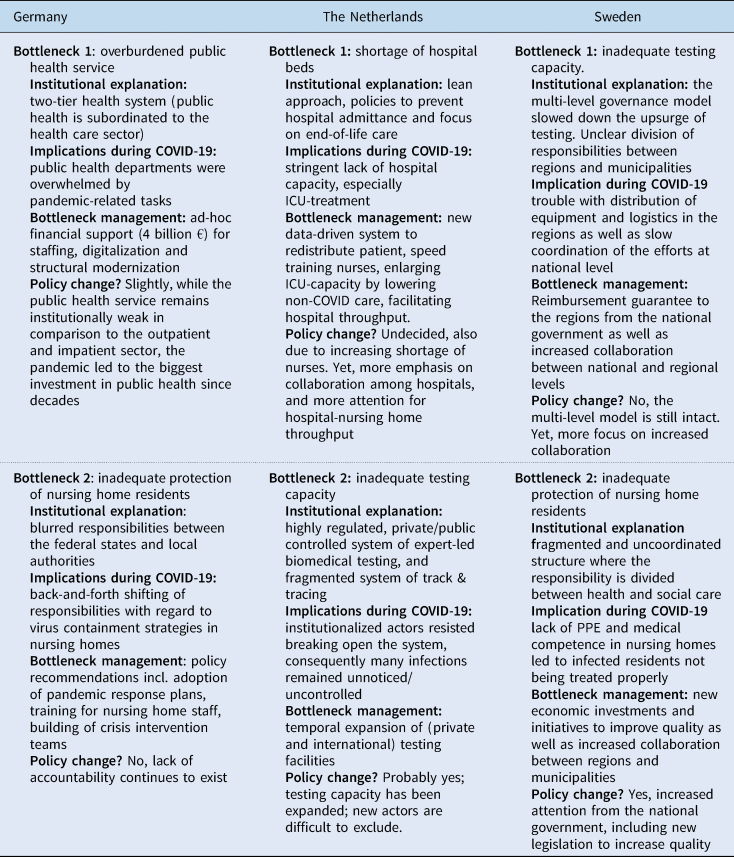
In this section, the bottlenecks and the specific governance responses are presented (Table 1). We will subsequently develop a more integrated analysis and discussion of (future) health system resilience; relating to the pandemic and beyond
Table 1. Health systems' bottlenecks and their management in Germany, the Netherlands and Sweden
3.1 Germany
3.1.1 A neglected and overburdened public health system
Due to the inherited health care gaze of the German health system the role of one of its other institutional pillars is often overlooked: the public health service (Öffentlicher Gesundheitsdienst, or ÖGD). Unsurprisingly, the public health service turned out to be a major bottleneck when the crisis began, revealing institutional failure rather than pandemic preparedness and rapid crisis response. Operating at the fringes of the health system, the ÖGD “is comprised of state and local health departments, certain institutions of veterinary and food inspection, and health authorities at the national, state and municipality levels” (Plümer, Reference Plümer and Rechel2018: 35). In general, the public health service is responsible for a broad set of tasks ranging from communicable disease prevention, hygiene and food control administration, animal disease control to obligatory medical check-ups for civil servants and pupils and social psychiatric counselling, though there are considerable differences among federal states. In pre-pandemic times the public health service largely operated beyond the radar of public attention. Most citizens were rarely aware of local health departments (Gesundheitsämter). Public health service's institutional ‘decoupling and subordination’ (Trein, Reference Trein2018: 152) has historic reasons: the murderous public health policy during the Nazi regime delegitimized any population-based health interventions from the outset – at least in West Germany; in the German Democratic Republic there have been some failed efforts to ideologize issues of public health. As a result, the ÖGD has remained a weak institution in post-war Germany lacking resources (in terms of both personnel and budget) but also political clout to influence health policy significantly.
The pandemic has revealed public health service's bottleneck status overnight. In spring 2020, the ÖGD abruptly became a key institution of the German health system since the tracing and tracking of persons infected with the virus fall under its legal remits. Out of the sudden, ‘dusty offices’, traditionally underfunded and understaffed, involuntarily turned into operational hubs which had to respond effectively to an accelerating global pandemic. Public health service staff did a tremendous job by monitoring infections, quarantining infected persons and identifying contact persons. Especially during the first wave of the pandemic, local public health departments demonstrated resilience in the absence of federal support. Hardworking, dutiful yet overburdened, and exhausted civil servants, euphemistically called ‘containment scouts’, that depend on pen, paper, phone and fax machines to fight a deadly virus (Intw-GER-1, see Appendix). In order to keep pace with the spread of the virus, public health departments had to recruit untrained staff from other public departments but also students and soldiers. In many cases public health service staff numbers increased 10-fold in a few months, requiring, above all, leadership and organizational development skills (Klenk et al., Reference Klenk, Cacace and Ettelt2021). Likewise, smooth cooperation (e.g. through the use of a standard trace-and-track software) among ÖGD units across local, state and federal levels was deemed necessary to join forces. While internal workflows have been efficiently streamlined during the second and third wave of the pandemic, public health departments experienced incremental institutional change by turning into permanent crisis response centres. To meet COVID-19 requirements, public health departments completely neglected their other tasks and duties. For example, there were no capacities left to address people's mounting social psychiatric needs caused by social distancing and lockdowns, neither was it possible to maintain preventive services such as addiction counselling (Intw-GER-2).
In August 2020, calls for a prompt infrastructural boost of the ÖGD gained political momentum. Pushed by daily evidence that highlighted the bottleneck function of the public health service in the day-to-day management of the pandemic, the federal government passed an ad-hoc policy in order to modernize the ÖGD. The so-called pact for the ÖGD includes four billion Euro for staffing, digitalization and structural modernization. It also refers, although rather vaguely, to the proliferation of the ‘Health in All Policies (HiAP)’ approach to revitalize future public health policymaking in Germany (Arnold and Teichert, Reference Arnold and Teichert2021). What seems to be a historic chance for an institutional upgrade of public health in the German health system must still be put to the test in practice. Implementing the pact turned out to be difficult due to fierce political infighting between the federal state and the Federation of German Cities and Municipalities over funding particularities (Intw-GER-3). Moreover, although the law mirrors the increased political attention towards the ÖGD, it has not resulted in a gain of institutional power (yet). The public health service still remains an underdog of the German health system. However, the pact has been re-established the public health service and its pandemic preparedness back on the political agenda.
3.1.2 Inadequate protection of older persons in nursing homes
The second bottleneck revealed another inherited weakness in the German health system; that of the long-term sector. Especially the situation in nursing homes has been largely neglected by health policymakers despite increasing care needs at the backdrop of demographic change. In consequence, authorities failed to protect nursing home residents from COVID-19 to the extent the general public has been protected. Death numbers among this most vulnerable group amount to 29,000 people (as of March 2021), making up more than one third of all COVID-19 deaths (approximately 82,600, 29 April 2021). In some federal states the situation was even more sincere, for example, in Hesse 1045 out of the 1447 people (i.e. 73%) that died in January 2021 because of the virus were nursing homes residents. However, public outcry has been surprisingly limited, underscoring the subordinated attention for long-term care.
In Germany, approximately 730,000 people receive care in more than 15,000 nursing homes which are run by public, private or non-profit providers. Responsibilities to regulate inpatient nursing homes are shared between the federal government and federal states. The federal level mainly controls the legality of care contracts between home residents and nursing home providers. The Länder (federal states) are responsible – together with the Medical Service of the SHIs – for the supervision of nursing homes in terms of adherence to legal conditions, care quality and on-time elimination of possible shortcomings. However, the devil is in the detail since many federal states have delegated supervision responsibilities to local and municipal administrations. Recently, there have been modest attempts to strengthen the overall status of the care profession in relation to physicians (e.g. by an academization of educational training and the establishment of Care Chambers in some federal states) and to improve the poor image of care by putting care concerns at the centre stage of the German health system. One important thread in this debate has been the question to what extent nursing homes can become more community-oriented (Hämel, Reference Hämel2016), i.e. the sheer opposite to sealed facilities in which people are bound to spend the final stages of their life in isolation. With regard to this mission, the pandemic has proved to be a bitter setback.
Experts publicly denounced major policy failures caused by ‘organized non-responsibility’ that was able to emerge due to the strong health care orientation of the German health system (Intw-GER-4). While the public has been recurrently reminded that an overload of intensive care bed units needs to be avoided at all cost, concepts to effectively protect nursing home residents have not debated to the same extent. While the federal government is not in charge (and, hence, blames the federal states for their mismanagement), federal states and local authorities have been shifting responsibilities back-and-forth instead of developing a workable approach that lasts throughout the pandemic. Shortcomings include the unavailability of protection equipment for nursing home staff and chaotic situations in facilities that turned into Corona hotspots (Roth et al., Reference Roth, Feller, Ruhnau, Plamp, Viereck, Weber and Savaskan2021). Partly, similar to public health departments, ad-hoc recruited soldiers assisted the overburdened nursing home staff.
Most problematically, the crisis resulted in fewer inspections of nursing homes. There is a lack of monitoring and collective learning whether and how nursing homes providers accomplished the protection and welfare of residents. Furthermore, informal social control of carers and nursing home providers by relatives has become difficult despite an increase of videocalls since residents were not allowed to receive visitors. Consequently, the causes for COVID-19 outbreaks and deaths in nursing homes are still unclear, making targeted interventions difficult. Policymakers, perceiving nursing homes as black-boxes, have little knowledge about providers' internal decision-making processes. Facing nursing homes' tragedy, commentators felt reminded to Goffman's (Reference Goffman1961) dystopian concept of the ‘total institution’. Despite recommendations by the Robert-Koch-Institute (RKI) for a potential re-opening, most nursing homes remained closed during the second wave of the pandemic. Proposals for the development of intelligent pandemic response plans, including prevention training for nursing home staff, crisis intervention teams (for acute virus outbreaks), care emergency services (in case of staff shortage due to quarantines) and context-specific test strategies (Schrappe et al., Reference Schrappe, François-Kettner, Gruhl, Hart, Knieps, Manow, Pfaff, Püschel and Glaeske2020), have not been adopted widely.
All this confirms nursing homes' bottleneck character in the German health system that had already been neglected in pre-pandemic times and suffered from policymakers' lack of accountability during the crisis. So far, meaningful policy change, for example, an integration of long-term care ‘into health service delivery and public health functions’ (Haldane et al., Reference Haldane, De Foo, SM, AS, Tan, Wu, Chua, Verma, Shrestha, Singh, Perez, Tan, Bartos, Mabuchi, Bonk, McNab, GK, Panjabi, Nordström and Legido-Quigley2021: 15) seems out of reach.
3.2 Sweden
3.2.1 Quality failures within nursing home care
Similar to Germany, the inability of nursing homes to protect frail older people from being infected was a clear bottleneck in the Swedish health care system during the pandemic. The COVID-19 pandemic has affected nursing homes particularly hard, with half of all mortalities thus far occurring among nursing home residents (Corona Commission, 2020). A particular problem has been the lack of medical competence in nursing homes, which among other things has necessitated medical decision-making by inadequately trained staff (Intw-SWE-1). Evaluations have suggested that many infected residents did not get individual medical assessments by a physician, and many residents were not referred to a hospital when necessary but rather died from COVID-19 at nursing homes (IVO 2020). The fragmented and uncoordinated care structure can be attributed to a previous reform (ÄDEL), implemented in the early 1990s, which attempted to de-institutionalize long-term care to curb costs. As a result of the reform, the responsibility for long-term care up to the level of nursing care was assigned to the municipalities, while physicians remained employed by the regions. Subsequently, the collaboration between social and medical care deteriorated (Blomqvist and Winblad, Reference Blomqvist, Winblad, Immergut, Andersen, Devitt and Popic2021).
It has been concluded that a lack of medical competence at the nursing homes, in combination with low compliance with hygiene recommendations and lack of sufficient personal protective equipment (PPE) for staff, has contributed to the difficulties in limiting the spread of the disease (Winblad et al., Reference Winblad, Swenning and Spangler2021). The lack of PPE and the prioritization of equipment for regional-level care providers (i.e. acute and intensive care treatment) often left staff in the municipal care sector without adequate equipment (Intw-SWE-1). The municipalities thus often had to find their own ways of obtaining PPE through independent purchases and procurements (Corona Commission, 2020).
Inadequate collaboration between hospitals and nursing homes (i.e. between regions and municipalities), too low medical competence and the lack of PPE, along with vague national guidelines of how and when to use PPE, hampered effective mitigation efforts particularly in care, likely contributing to the spread of the virus (Corona Commission, 2020). These quality issues led to increased attention to the care sector from government actors, including economical investments by the national government, initiatives to improve quality at municipal level and increased collaboration between regions and municipalities (Intw-SWE-2). Thus, the COVID-19 pandemic could be driving improvements across the organizational boundaries between care and health care, potentially leading to more integrated services in the long run. Furthermore, in light of the pandemic, it has become clear that the care sector has been neglected and not politically prioritized during the last decades.
3.2.2 Failing upsurge of test facilities
A second bottleneck in the Swedish health care system was the relatively slow increase in testing capacity, at least during the first wave of the pandemic, stemming from trouble with equipment and logistics in the regions, and initially unclear communication and lackluster coordination of the effort at the national level. When community transmission was identified in the beginning of March 2020, the regions began establishing testing based on a prioritization scheme developed by the Public Health Authority (PHA) which focused on testing prioritized groups of individuals. Priority groups 1 and 2 were defined as hospitalized patients and health- and eldercare staff, followed by priority group 3, people with important societal functions (the latter was not included in the PHA prioritization scheme until May 27). The initial Swedish testing strategy was thus not to test the general public, but even given the strategy of only testing prioritized groups, the establishment of sufficient testing capacity in the regions was found to be a complicated task. While the reasons for these complications differed from region to region, it appears that a lack of the materials necessary to conduct testing, as well as limited analytical capacity in regional laboratories were two main factors. Another important factor for the slow upsurge has been an unclear division of responsibilities between the national and regional levels (Hallberg et al., ongoing study). Eventually, when large-scale and population-wide testing became a national goal, it took time to finalize reimbursement guarantees by the national government for testing costs, and the regions only accepted to begin large-scale public testing when they were granted money from the national government to do so in June 2020 (Fredriksson and Hallberg, Reference Fredriksson and Hallberg2021).
There were also intense discussions regarding the interpretation of priority group 3 (that is employees being considered ‘societally important’) exemplifying the unclear guidance and insufficient communication from the national agencies involved. Furthermore, while the prioritization scheme from the PHA about testing prioritized groups remained until June 2020, the national government simultaneously communicated that testing needed to increase on a broader basis. This double message seemed to create both confusion and frustration among the regions, and is most likely a result of the Swedish governance model, which prohibits interference from the government in day-to-day activities of the national agencies, such as the PHA.
Since the reimbursement guarantees were implemented in June 2020, Sweden has had a rather well-functioning large-scale testing programme as a result of improvements in the testing apparatus by the regions, partly with help from national actors (e.g. the procurement of analytical capacity through the PHA), and through economic steering by the national government (Fredriksson and Hallberg, Reference Fredriksson and Hallberg2021).
3.3 Netherlands
3.3.1 Searching for hospital beds
From early in the crisis onwards, the Netherlands has faced a shortage of hospital beds and nursing capacity. The number of COVID-19 patients, especially during the first wave of the pandemic (March–May 2021) outweighed the number of (especially) intensive care beds and specialized nurses (Boin et al., Reference Boin, Overdijk, van der Ham, Hendriks and Sloof2020). Prior to the COVID-19 crisis, the number of beds had been reduced as part of the shift to a system of regulated competition (encouraging hospitals to be ‘lean’), as well as an overall reduction of hospital stay (Jeurissen and Maarse, Reference Jeurissen and Maarse2021). This lean approach however did not result in shortages before the crisis; hospitals often had ‘empty beds’ (up to 30%) and waiting lists were usually short.
In the first phase of the crisis, hospitals were overwhelmed with severely ill patients; one out of five needing intensive care treatment. It was calculated that 2400 ICU beds would be necessary at the height of the first wave of the pandemic, whilst only 1150 were available (de Graaff et al., Reference de Graaff, Bal and Bal2021). To upsurge capacity, several strategies were employed: scaling up intensive care capacity (i.e. speed-training ward nurses, enlarging the number of beds by turning operation facilities into intensive care beds and purchasing ventilators), scaling down non-COVID-19 care and redistributing COVID-19 patients among hospitals. This redistribution of patients has become a cornerstone of collective action (de Graaff et al., Reference de Graaff, Rahmawan-Huizenga, Bal, Kuijper, Felder, Zwart, Kalthoff, Van de Bovenkamp, Wallenburg and Bal2022). In the first two weeks, the redistribution of patients mainly happened based on peer contact (physicians helping out their colleagues in other hospitals). Yet when the number of patients further increased, the national network of acute care regions (in Dutch, the LNAZFootnote 3, until then, more or less a ‘sleeping agency’) installed a special centre for the redistribution of patients, coordinated with the help of the Dutch army (Landelijk Centrum Patiënten Spreiding, LCPS). Hospitals were required to report their number of patients to a regional agency (RCPS, connected to the regional acute care networks) that monitored the number of patients in the region. Data systems were built to monitor bed capacity and patient flows.
In the first wave, redistribution was mainly focused on COVID-19 patients only. During the second and third wave focus (and related calculating mechanisms) shifted to a ‘fair share’ of COVID-19 patients in order to keep regular care provision going as much as possible. In case of an unequal distribution – that is, not in accordance with the ‘fair share norm’ – patients were redistributed among hospitals in or outside the region, or even to other countries (particularly Germany). This newly invented system has to protect the availability of non-COVID-19 care, as well as hospitals' competitive position (e.g. compensating hospitals for the loss of non-COVID-19 care). It is supported by the Dutch Health care Authority that has developed an imbursement scheme, and monitors the scaling down of regular care (NZa 2021). Although the LCPS works quite well, it has been also heavily criticized as its data models are not fully trusted among hospitals that are afraid (amongst others) of waiting lists and losing non-COVID-19 patients to other hospitals (authors' observations during LNAZ meetings).
Next to patient redistribution and modelling, new care arrangements have been introduced to lower the pressure on hospitals, and to intensify the relationship with primary care and nursing home care. Patients who are in need of oxygen therapy but who are clinically stable are sent home with oxygen treated by their own general practitioner. Also, hospitals have set up care pathways with nursing homes for older persons to fasten discharge (Intw-NL-1). It is expected that these newly arranged technical and integrated care systems and care routines will remain, and may be expanded after the crisis. In terms of the institutional structure of the Dutch health care system we can thus see on the one had that the layered system still is of influence – i.e. central coordination next to professional negotiations and competition between providers – but has also altered, mainly through the data-intensified national and local acute care networks. Moreover, links between acute, primary and long-term care have been strengthened in the ‘heighdays’ of the crisis yet have fallen apart when the number of hospitals admissions decreased, revealing the emphasis on hospital throughput.
3.4 Institutional working rounds for testing capacity
Similar to Sweden, testing capacity in the Netherlands has lagged behind, especially during the first wave of the pandemic. Reasons are fivefold: (1) the Netherlands has a distributed testing system mainly connected to hospitals and GP practices; (2) and related, the testing infrastructure is highly expert-based and mainly controlled by microbiologists that have developed entry-rules legitimized by safety regulations and nationally oriented public health standards; (3) the testing infrastructure was highly reliant on one company (Roche – controlling 70% of the market), which had trouble keeping up with production during the pandemic; (4) testing for public health was controlled through the regional public health organizations (GGDs) which meant a lack of national coordination, suggesting that testing capacity was not optimally used; (5) contact tracing was poorly organized meaning that large-scale testing and tracing failed. Dealing with these bottlenecks has proven to be hard and controversial (Stokmans et al., Reference Stokmans, Lievisse and Adriaansen2020).
During the first wave, coordination of testing was taken over by the Ministry of Health in close coordination with the national association of GGDs, the RIVM – which was responsible for guidelines determining who needed to be tested – and the association of microbiologists. Due to scarcity, guidelines for testing were very restrictive at start: only people with complaints (fever above 38.2, coughing and stuffiness) could be tested. An exception was hospital employees and patients as hospitals had enough capacity to test their personnel and patients. Also, one university hospital deviated from the national guidelines and tested as many citizens as possible in their region (Intw-NL-2). Many reports in the media indicate that lacking test-capacity has led to the quick spread of the virus as many positive but not ill people went unnoticed. Furthermore, lack of expertise and capacity for contact tracing hampered the tracing of (possibly) infected citizens.
The controversy over testing capacity has a long history as traditionally the Dutch system has worked with small, highly expert-driven laboratories, which stands in contrast to for example Germany and France that use large-scale, fully automated labs (Intw-NL-3). Whilst these large labs are generally cheaper and are able to do much more tests, the Dutch system has been highly successful in for example preventing MRSA infections and in decreasing ‘unnecessary’ tests and use of antibiotics, mainly because of the tight connection between microbiology labs and care practices. For years already, mainly German companies have been active to enter the Dutch market and have some labs functioning. During the early stages of the pandemic, this controversy was further played out. Only towards the summer of 2020, after the first wave had ended and testing became more and more politicized, deals were made to expand testing capacity by opening up to international and for-profit providers (Intw-NL-4). Circumventing the ‘monopoly’ of microbiologists, but with their temporary consent, these deals have been made through the Ministry of Health. New labs are supposed to live up to the standards as set by the association of microbiologists and the Health care Inspectorate monitors this. Whilst the new structure is expected to end after the COVID-19 crisis, some argue that it is here to stay and will restructure the testing market, allowing for large commercial and fully automated labs to take over the largely expert-led testing infrastructure of before the pandemic. Some signs of this are already there, as commercial labs are moving into the area of testing for sexually transmitted diseases (Baltesen, Reference Baltesen2021). The case of testing on the one hand shows the possibilities – and accompanying problems – of upsurging capacity. On the other had it also shows the institutional work as performed by the Ministry of Health, in this case mainly by ‘working around’ existing institutional arrangements of testing. Whether this will influence testing infrastructures in the future remains to be seen.
4. Discussion
4.1 From bottlenecks to resilience?
In this paper, we have described six bottlenecks and their management in the German, Swedish and Dutch health systems, exemplifying how policy responses are affected by the institutional contexts of health care systems, and what this may teach us about the (in)abilities to deal with a sudden health crisis as well as the opportunities to foster health system resilience. Two different types of bottlenecks could be distinguished: First, systemic weaknesses (e.g. the negligence of nursing homes) to be conceived as inherent defects of health systems' institutional settings. Second, unforeseen, new and partly episodic challenges with regard to certain subfields and functioning of health systems (e.g. testing, number of ICU-beds). Our cross-country comparison shows that countries have faced both sorts of bottlenecks in the course of the pandemic, although they applied different strategies to cope and deal with them. As a general lesson, our findings confirm our initial assumption that bottleneck management could be explained by country-specific institutional contexts and path dependencies. Moreover, whilst such responses have been at least partly successful, we suggest that ad-hoc and quick-fixes solutions to bottlenecks are insufficient to reach health system resilience.
Concerning the first category of bottlenecks, the dramatic situation in nursing homes turned out to be most severe. While sluggishness and incompetence exacerbated the problem, reasons for the failures could be traced back to nursing homes' weak position within the institutional setting of the German and Swedish health systems – i.e. a specific bottleneck that has become exposed due to COVID-19. As the pandemic evolved, nursing homes' disadvantageous condition, coordination problems and unbearable burdens of responsibility were brought into attention. For example, uncoordinated and fragmented long-term care system in Sweden hampered the provision of adequate medical care in nursing homes. In Germany, federal government blamed the federal states for their mismanagement of nursing homes, whilst federal states and local authorities shifted responsibilities back-and-forth instead of developing and implementing a protection scheme that lasted throughout the pandemic. Germany and Sweden managed the nursing home bottleneck differently, revealing varying degrees of flexibility and adaptability in health system governance. The German federal government has been paralyzed by the situation in the nursing homes, buttressing the assumption that protecting nursing home residents do not belong to the key priorities of Germany's health care-oriented health system. In contrast, in the Swedish case, the same problems forced at least ad-hoc investments and policy initiatives to improve cross-sectorial collaborations by the national government.
The weak, and even neglected, position of public health in all three countries has been another systemic bottleneck that has been resistant against rapid solutions. This is perhaps most prominent in Germany, where public health agencies suffer from a troubled history and have more or less become an appendix to the health care system. Viewed in this context, the agreed pact for the public health service to improve health departments' situation in terms of budget, equipment and staff, is a rather unusual step forward. However, as argued, within a multi-level health system institutional bottleneck remedy cannot be ordered top-down but depends on a painstaking and lengthy implementation process. While in the Netherlands and Sweden public health's institutional position is traditionally stronger, likewise, insufficient coordination and cooperation between policy levels, governance levels and policy sectors complicated the implementation of tracing and testing strategies. Moreover, even where political will might be present, other health system-specific issues might stand in the way of long-term solutions. For example, whilst in the Netherlands there is a large support for increasing intensive care treatment capacity, there is also a structural capacity problem, especially in nursing.
In general, the misalignment between different sectors within the health system, being the outcome of purposeful policy making in the past, appeared a real barrier to flexibly respond to the crisis. In the Netherlands, for instance, decentralization aimed to enhance community care and welfare in the light of an ageing population (e.g. Schuurmans et al., Reference Schuurmans, van Pijkeren, Bal and Wallenburg2020) but becomes problematic in relation to a national crisis. This fragmentation is further exemplified by the testing bottlenecks in both Sweden and the Netherlands, where microbiologists protected institutionalized and monopolized testing arrangements (Netherlands) and a decentralized system which led to uncoordinated policies in 21 different testing organizations (Sweden), leading to delays in the testing for a large portion of the population. Once again, attempts of country-specific bottleneck management have merely been temporarily coping strategies that do not lead to a straight removal of the bottleneck: In the Netherlands, this meant to bypass existing institutional arrangements for testing; in Sweden, the national government took responsibility for funding the testing rather late, causing further coordination problems.
Regardless of the bottleneck type, it must be stated that bottleneck management under stress is a complex and difficult endeavour. While flexibility and pragmatism certainly helped to prevent the worst, swift structural changes are hard to reach. Even if established policymaking procedures can temporarily circumvented by ad-hoc policies, they may cause new problems in the future. Moreover, public health and long-term care stakeholders often lack the capacities to fully engage themselves in the conflictual process of policy implementation while, at the same time, being fully absorbed by crisis management. Likewise, structural divisions of the health system, like the one between social care and health care in Sweden, cannot be instantly bridged. The same holds true with regard to claims for more regional cooperation and sector integration (as in the Netherlands and Sweden) or the proliferation of health-in-all-policy approaches (as in Germany).
What do we learn from bottleneck management regarding health system resilience? Above all, there is no causal mechanism linking the one to the other. Instead, policy makers' responses are marked by uncertainty and temporal limitations. Taken measures might be inadequate or even counterproductive in order to contain creeping health crises related to, for instance, an ageing population, non-communicable diseases or climate change. There is ample reason to believe that future disasters will be accompanied with other or additional bottlenecks than those we witnessed since March 2020. In terms of health system resilience, the ‘art of dealing with bottlenecks’ – whatever their specific origin or object – seems to be more important than removing them. Particularly questions concerning system integration improvement, perceived as attempts to strengthen so far neglected sectors such as public health and long-term care, are very likely to become a cross-cutting issue of health system resilience. Hence, resilience could be demonstrated by the specific manner policy makers respond to and actively manage bottlenecks. As shown, in the health systems we looked at, resilient action has been limited to the identification and recognition of bottlenecks. Secondly, bottlenecks caused, at best, quick policy adaptions, leaving “the broader social, economic and political factors in society” (Haldane et al., 2021: 15) and health systems (e.g. the imbalance of power between hospitals and public health agencies) untouched. Thus, the acute management of bottlenecks during the pandemic closely resembles ‘the science of muddling through’ (Lindblom, Reference Lindblom1959). That is, no permanent solutions were found nor implemented for the sake of health system resilience, but bottlenecks were pragmatically dealt with within the boundaries of health systems' institutional settings.
While muddling through is by all means a virtuous approach to maintain the basic functioning of health systems when under attack, it is no substitute for broader reforms. Bottleneck recovery requires no less than sectoral reorganization, shifting of institutional responsibilities and a change of stakeholders' mindsets. Measured against these indicators, meaningful health system resilience remains unavailable until further notice.
Conflict of interest
None.
Appendix
Overview of conducted interviews
Germany
Interview with a head of local health department A (Intw-GER-1)
Interview with a head of local health department B (Intw-GER-2)
Interview with a national public health service representative (Intw-GER-3)
Interview with a health system expert (Intw-GER-4)
Interview with a regional public health service representative (Intw-GER-5)
Interview with a public health service physician (Intw-GER-6)
Netherlands
Interview with an acute care coordinator (Intw-NL-1)
Interview with a regional director of public health (Intw-NL-2)
Interview with a public health expert (Intw-NL-3)
Interview with a national public health coordinator (Intw-NL-4)
Interview with a national acute care coordinator (Intw-NL-5)
Interview with a intensive care specialist (Intw-NL-6)
Sweden
Interview with a medically responsible nurse (Intw-SWE-1)
Interview with a regional health care director (Intw-SWE-2)
Interview with a regional area manager (Intw-SWE-3)




