The healthcare physical environment is a significant reservoir of pathogens. Reference Weber, Anderson, Sexton and Rutala1–Reference Otter, Yezli and French3 Environmental cleaning and disinfection is critical to interrupting the transmission of these pathogens. Reference Donskey4 Despite initiatives that have targeted environmental cleaning, Reference Evans, Kralovic, Simbartl, Jain and Roselle5 cleaning compliance is still low. Reference Evans, Kralovic and Simbartl6 Low practice compliance may partially be explained by practice variation. Reference Atsma, Elwyn and Westert7 In a recent evaluation of infection prevention practices across the Veterans’ Affairs health system, significant variation in cleaning was identified. Reference Keating, Obasi and McKinley8 A recent review of healthcare cleaning strategies highlighted the human factors in the manual cleaning process and the need for work-system evaluation to understand contextual determinants (ie, barriers and facilitators) of environmental cleaning. Reference Doll, Stevens and Bearman9
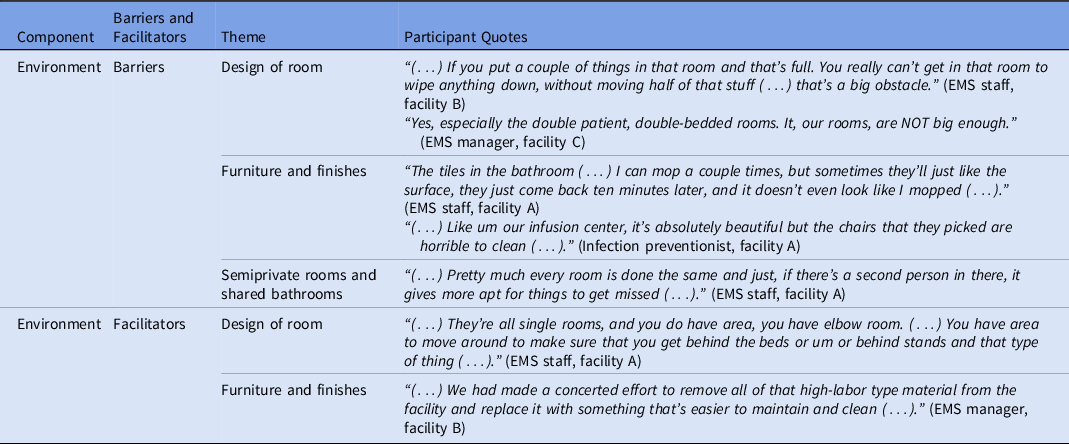
A human-factors engineering (HFE) framework, the Systems Engineering Initiative for Patient Safety (SEIPS) model, Reference Carayon, Schoofs Hundt and Karsh10–Reference Holden, Carayon and Gurses12 has been used extensively in health care as a road map for work system analysis, including its application for understanding processes for infection prevention (Fig. 1). Reference Yanke, Zellmer, Van Hoof, Moriarty, Carayon and Safdar13,Reference Carayon, Wetterneck and Rivera-Rodriguez14
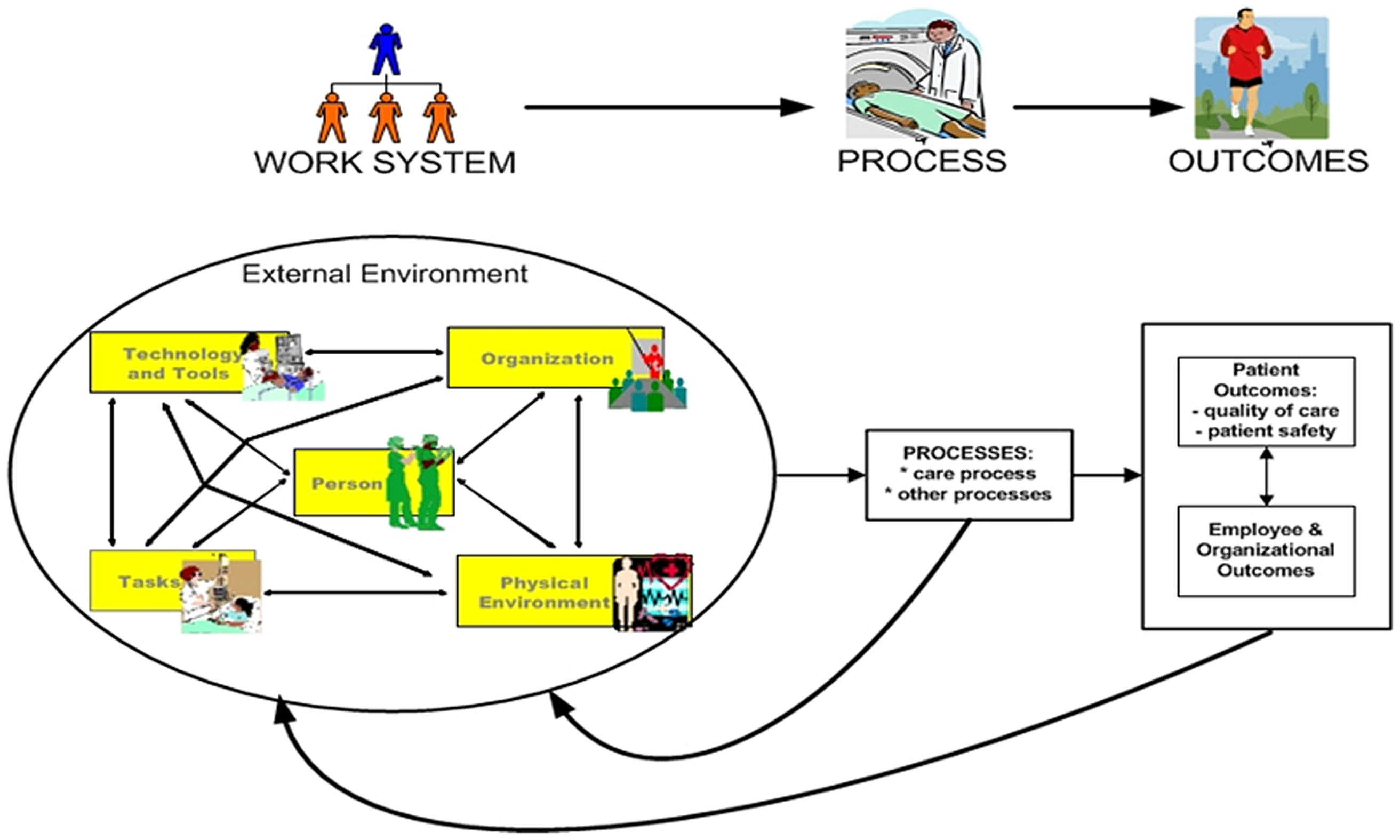
Figure 1. Systems engineering initiative for patient safety model.
The SEIPS model focuses on 5 interacting components of the work system: organization, person, tools and technology, tasks, and environment. Interactions of these components can affect care processes such as environmental cleaning practices in healthcare as well as subsequent outcomes such as poor cleaning compliance, pathogen transmission and healthcare-associated infections (HAIs).
An HFE-focused work-system analysis provides a means to understanding the contextual determinants of environmental cleaning processes, which could improve the fidelity of the processes through identifying key entry points for interventions. We conducted a comprehensive work-system analysis using the SEIPS model to identify determinants of cleaning practices within the VA.
Methods
We conducted a qualitative study Reference Elo and Kyngas15,Reference Elo, Kääriäinen, Kanste, Pölkki, Utriainen and Kyngäs16 using semistructured interviews with key stakeholders including environmental management service (EMS), nursing, and infection preventionists (IPs) at VA facilities across 3 acute-care settings and 2 long-term care settings between January and June 2019. We interviewed 18 participants using interview guides developed by the research team. The interview questions focused around the 5 work-system components of the SEIPS model within the context of cleaning processes (eg, healthcare worker’s knowledge; knowledge as an element within the ‘person’ component of cleaning) was assessed by asking “How is cleaning important for infection prevention?” (see the Interview Guide in the Supplementary Material online).
Interviews were conducted by trained research staff at each site who received ∼10 hours of didactic training on qualitative interviewing. Interviews lasted 45 minutes on average and were audiorecorded using encrypted recorders and were transcribed verbatim. The qualitative team used MAXQDA software (VERBI Software, Berlin, Germany) to manage and analyze electronic transcripts.
Transcripts were analyzed for thematic content and were then mapped to the SEIPS work-system components. Analysis was conducted by an interdisciplinary team including trained social scientists with backgrounds in anthropology, public health, nursing, and infection control. The initial inductive coding 56% of the transcripts occurred via group consensus. This process involved individuals reading and coding transcripts independently with final coding assigned after group consensus. Reference Elo, Kääriäinen, Kanste, Pölkki, Utriainen and Kyngäs16 Through an iterative process of discussion and code definition refinement, a comprehensive codebook was developed. The remaining transcripts (44%) were coded by pairs following a similar method of initial independent coding followed by paired consensus. Reference Elo, Kääriäinen, Kanste, Pölkki, Utriainen and Kyngäs16 Discrepancies continued to be discussed within the larger group to reach agreement and consensus. The team first focused on inductive codes, which were later mapped onto domains of the SEIPS framework. This unconstrained coding process allowed the team to later align themes congruent with the SEIPS constructs and allowed for the emergence of themes that may have been disparate from the framework. The team found that the codes aligned well with the SEIPS domains; however, there was overlap between domains (ie, codes could be mapped to >1 domain). The mapping of inductive codes within the SEIPS domains is provided in the Results section along with exemplar quotes.
Human-subject review
Human-subject review and approvals were sought from the VA Central Institutional Review Board (CIRB 18-10) and local site research and development committees. We received a waiver of documentation of informed consent for the interviews.
Results
All 18 interviews were conducted with 11 EMS managers and staff, 4 nurse managers and staff, and 3 IPs. Reference Bengtsson17 Several themes were identified as determinants of environmental cleaning.
Organization
Most of the emergent themes centered within the organization component of the SEIPS framework, which are outlined in Table 1. Primarily, stakeholders reported challenges to EMS staff recruitment and retention that greatly affected assignment consistency, cleaning practices, teamwork, and training. Other important organization themes were communication, professional value and organizational culture, and leadership.
Table 1. Themes and Exemplar Quotes within the Organization Component
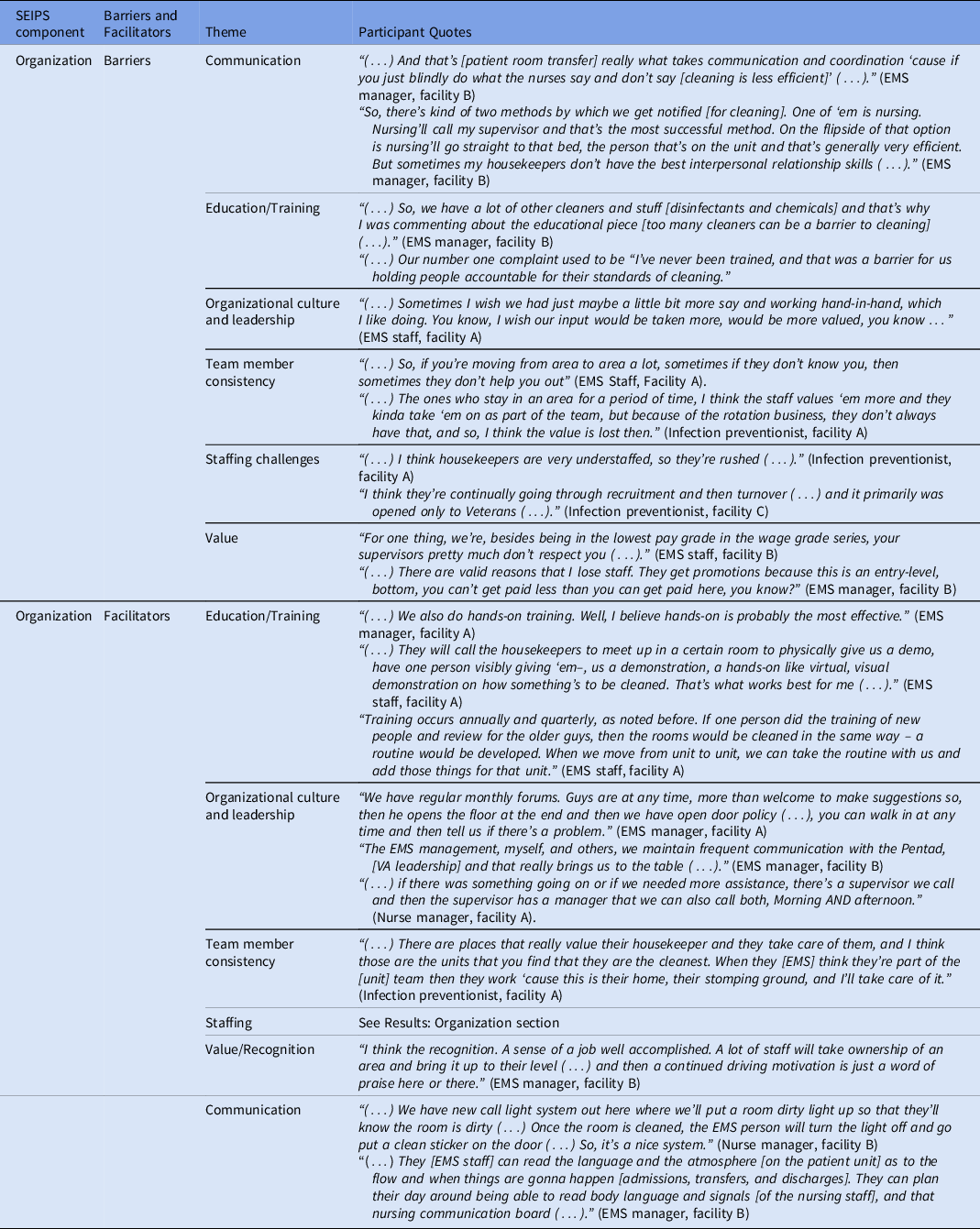
The staffing challenges occurred across the continuum from recruitment to retention. Respondents noted that regulatory and restrictive hiring processes within the VA for hiring EMS staff led to staffing challenges. Specifically, laws governing specific positions (eg, housekeeping aids) of government employees restrict hiring to veterans, which have limited the applicant pool. According to 5 US Code 3310, a 2013 law that governs Title 5 government employees, housekeeping aid positions are restricted to veteran hires. Reference McKinley, Baubie, Bartel, Flower, Keating and Safdar18 In 2022, 5 US Code 3310 was amended to allow nonveteran hires when veteran eligibles are not available.
“(…) [Hiring is] a time-consuming, complicated quagmire of regulations (…).” (EMS manager, facility B)
These hiring difficulties led to low staffing and assignment inconsistencies that affect teamwork within the area where cleaning occurs. Without consistent staff assignment, EMS staff felt unable to integrate into the healthcare team. Stakeholders also noted the power of staffing consistency.
“(…) We try to keep people in the same area, you know, instead of switching people (…) When they’re in an area longer, they build up the lines of communication with the staff in there. They build up their ownership of that area (…).” (EMS manager, facility A)
Stakeholders reported that understaffing had practice implications, such as rushing through cleaning processes, and that perceptions, including quality of cleaning practices, may be compromised:
“Things are gonna get missed. Quality control is gonna go down and something bad’s gonna happen. But staffing is ALWAYS an issue.” (EMS staff, facility A)
Inadequate staffing levels can also create training issues, and training is critical for EMS staff performance, as one EMS manager (facility B) noted:
“So, staffing issues create training issues because if I don’t have enough staff to go around and that shortchanges a new employee on the amount of time that they get trained without being put out on the floor independently.”
EMS staff education and training lacked standardization. Interviews revealed various training methods such as online training, training during staff meetings, peer shadowing, train-the-trainer activities, and hands-on training. Facilitators reported by interviewees largely centered around preferred training methods and best practices to improve training. Simulation (or hands-on) methods and train-the-trainer methods were preferred approaches to training:
“In training (…) new ones [EMS staff], I like to pair ‘em up with a real good housekeeper that’s been here for quite a while and work side by side with ‘em. That hands-on training is probably your best. (…).” (EMS manager, facility B)
The interviews highlighted several best practices for optimizing standardized training:
“(…) We converted a housekeeping aide position to a GSI [VA pay scale] training specialist, and she solely dedicated to training for housekeeping personnel.” (EMS manager, facility B)
Person
Multiple people are involved in the work process for environmental cleaning. Overlap of these processes has been described in other SEIPS components such as the communication (ie, organization component) required for room cleaning. Table 2 outlines key themes identified within the person component. Many EMS staff were veterans who were highly motivated to serve fellow veterans, especially to prevent them from acquiring infections. Although cleaning was perceived to be important for patient safety, there was also a perception that cleaning may be disruptive to patients.
“So, the environmental management department is the first line of defense between organisms that are found in the environment and the staff and visitors and patients that use the environment.” (EMS manager, facility B)
And
“(…) sometimes you can do that [clean] and sometimes you can’t because some patients don’t want you in there.” (EMS staff, facility C)
Table 2. Themes and Exemplar Quotes within the Person Component
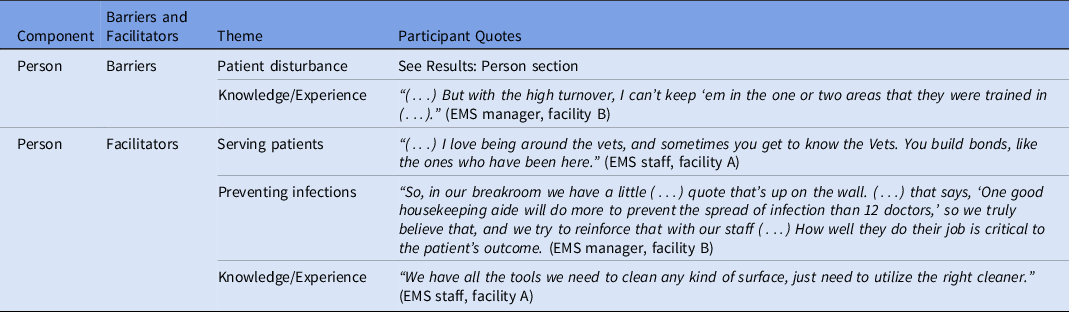
EMS staff understood the technical knowledge required for the position, especially understanding the multitude of chemicals used. There was also acknowledgement of the need to understand the intricacy of patients they serve:
“(…) But you know, you can have the fastest cart in the world, it’s about how you use what’s on that cart.” (Facility C)
And
“(…) When I started working in the hospice unit, I was SCARED, you know, and now you know, I’ve gotten more comfortable with it, but I think that would be a nice training that they could have.” (Facility B)
Tools and technology
Themes identified within the tools and technology SEIPS component (Table 3) included having effective cleaning products, but sometimes these products and/or equipment were in limited supply. Staff noted on several occasions that the introduction of new products, supplies, and/or equipment improved the cleaning process.
“(…) The rag issue [limited supplies], which they try and try and try to solve and that just seems to be one of those things that is the same with the staffing (…).” (EMS staff, facility B)
And
“He’s [EMS] using a microfiber system for cleaning floors. I find that to be much more clean than when they used the old mops and they’re more attuned to changing heads than they did with their mop heads (…).” (Infection preventionist, facility A)
Table 3. Themes and Exemplar Quotes within the Tools/Technology Component
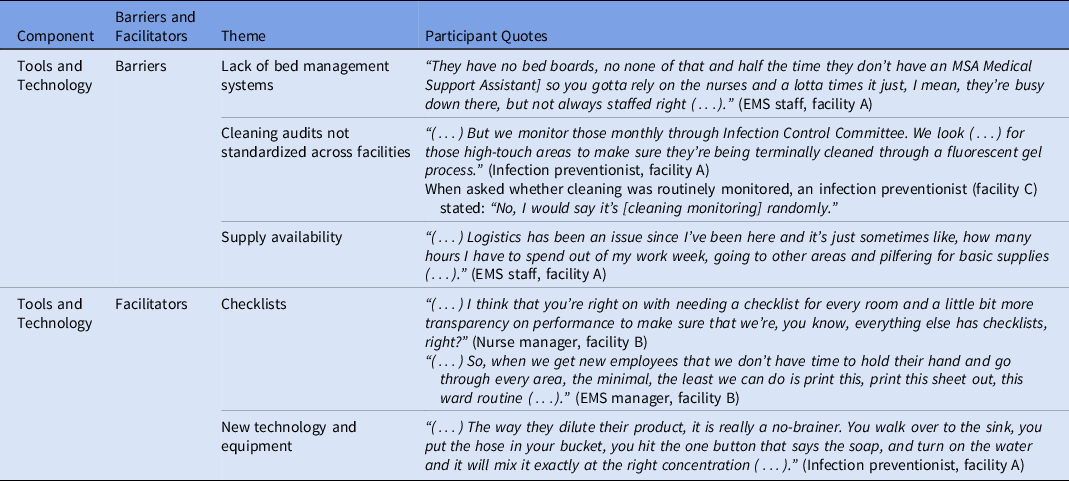
Interviewees at most sites reported some form of monitoring (ie, audits and/or checklists) of their cleaning process, however, there was variation in type and frequency. Audits and checklists were generally felt to be important and to provide useful information.
“I think that it [audits] should be mandated across the country that environmental management reports data (…).” (EMS manager, facility B)
Several staff mentioned that automated bed management systems (BMSs) could facilitate communication required for efficient notification and management of room cleaning, but some facilities lacked this technology:
“Other facilities have a fully functioning bed management system, meaning the ED knows when rooms are open (…).” (Nurse manager, facility B)
Tasks
Several important themes were identified within the task component of the SEIPS framework (Table 4). Stakeholders reported that moving patients from one room to another occurred frequently for various reasons (eg, isolation or patient acuity) which greatly affected workload.
“That [patient movement] takes away from their regular daily cleaning on everybody else on that unit because my person spent 90 minutes to make sure that one patient got closer to the nurse.” (EMS manager, facility B)
Table 4. Themes and Exemplar Quotes within the Task Component

EMS staff were reportedly motivated to clean high-touch surfaces but also found that cleaning the room with the patient present in the room was difficult:
“(…) But day shift, their primary task is doing daily cleanings and (…) they’re supposed to hit the bathroom, high-touch areas.” (EMS staff, facility A)
And
“But, as far as the patient bed, you know, it’s, while they’re in it, it’s hard [cleaning]. You know?” (EMS manager, facility C)
Another theme included challenges with cleaning reusable medical equipment (RME) such as ambiguity regarding who was responsible for cleaning (ie, EMS or the end user) and cleaning complex or delicate equipment:
“It depends on the equipment. There’s certain things we clean and there’s certain things that are assigned to certain people (…).” (EMS staff, facility A)
Environment
Table 5 lists the themes identified within the SEIPS environment component. Room design was important when semiprivate rooms were reported to be harder to clean than private rooms. However, small private rooms with multiple medical equipment were also challenging:
“I mean you get two patient beds (…) big chairs (…) trying to get in there and work around everything, it’s challenging (…).” (EMS manager, facility C)
And
“They’re [patient room] too small (…) when they pack that room full of IV poles, monitoring equipment and other equipment, it just makes it next to impossible to get into that room, clean it in an efficient manner.” (EMS manager, facility B)
Table 5. Themes and Exemplar Quotes within the Environment Component
Furniture and surface finishes were important and could be considered a barrier to or facilitator of cleaning:
“(…) I think our bathrooms have tile and grout, which makes [cleaning] it tough (…).” (Nurse manager, facility B)
And
“(…) We need to have high quality, easy to clean, easy to maintain equipment. (…) you cannot skimp on cost (…).” (EMS manager, facility B)
Adapted SEIPS model for environmental cleaning
Our study identified important components of the work system that could be barriers or facilitators to environmental cleaning. Based on these findings, we developed a SEIPS model outlining essential work-system components for cleaning (Fig. 2). The adapted SEIPS model can be used when evaluating the status of facility or unit-level cleaning program or processes to elicit comprehensive feedback from stakeholders and to provide specific actionable entry points for improvement efforts.
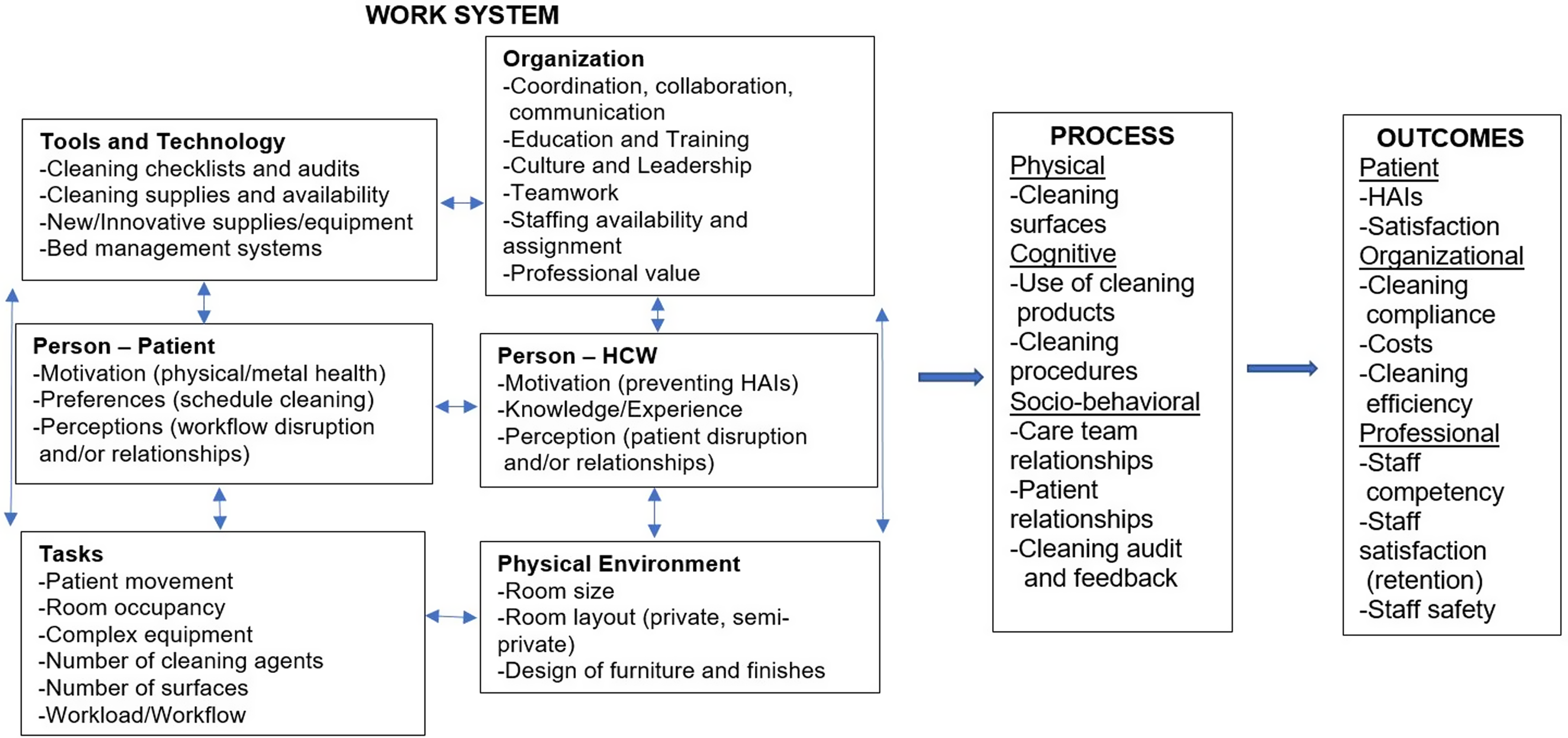
Figure 2. SEIPS 2.0 model adapted for environmental cleaning.
Discussion
In this study, we identified several work-system facilitators of and barriers to environmental cleaning. One notable finding was that EMS staff, many of whom are veterans, were especially motivated to serve the veteran population. We previously reported findings from interviews with hospitalized veterans, and many reported enjoying having fellow veterans EMS staff to converse with and even had feelings of bonding and camaraderie, which may promote a healing environment. Reference McKinley, Baubie, Bartel, Flower, Keating and Safdar18 Our team also identified the need create a work environment for EMS staff to be viewed as a valued member of the healthcare team and potential ways for healthcare organizations to improve EMS work climate. Reference Goedken, McKinley and Balkenende19
A central theme was the staffing challenges reported by stakeholders, which affected assignment consistency, cleaning practices, teamwork, and training. Hiring policies within the VA, particularly when hiring EMS staff, are legislated and thus are beyond the scope of this manuscript. However, investing in EMS staff once employed may be a viable solution and has been previously proposed by providing or incentivizing specialized certification. Reference Tyan and Cohen20,Reference Peters, Otter, Moldovan, Parneix, Voss and Pittet21 The nursing profession has identified the role of specialty certification and improved patient outcomes, including reducing HAIs. Reference Coelho22 Evidence shows that certification of healthcare professionals who infection prevention and control (ie, CIC) results in improved care processes and HAI outcomes. Reference Pogorzelska, Stone and Larson23,Reference Saint, Greene and Olmsted24 Certification requirements can be used to reclassify VA positions to higher pay grades, which may, in turn, address professional value and retention and ultimately improve care and outcomes.
Stakeholders reported that consistent staffing assignments improved many aspects of the work system including communication, accountability, performance, and teamwork. Consistent assignment is a staffing model used in nursing homes to improve resident outcomes and although the evidence varies, further study is warrented. Reference Rahman, Straker and Manning25 Education and training of EMS staff was a key facilitator identified by stakeholders. Various methods were implemented to address staff training needs including interactive hands-on (or simulation) training, on-the-job training (eg, peer coaching and train-the-trainer activities), and online computerized courses. Many respondents believed that simulation training was extremely effective, and we have reported these findings separately. Reference Goedken, McKinley, Balkenende, Hockett, Reisinger and Safdar26
Communication emerged as a challenge within the work system. Notification of EMS for room cleaning during admissions, transfers, and discharges (ie, patient throughput) was especially challenging. Although various communication methods were used (eg, nursing boards, light systems, phone calls or pagers, signs, etc), many staff agreed that implementation of an automated BMS could facilitate this process. Delays in patient flow can lead to poor patient outcomes, and automated BMS have improved patient throughput. Reference Tortorella, Ukanowicz, Douglas-Ntagha, Ray and Triller27
Audit and feedback of environmental cleaning is a mainstay recommendation for infection prevention and control programs. Reference Guh and Carling28 Most stakeholders reported some type of audit and feedback in place, but it was highly variable in method and consistency. Audit and feedback of healthcare processes is associated with improvements in practice, Reference Ivers, Jamtvedt and Flottorp29 and efforts to standardize this practice are critical.
Another important theme was the concern that having a patient in the room during cleaning may be interpreted by staff as disruptive to patients. EMS staff may feel unnecessarily rushed or may avoid cleaning all together, leading to less thorough cleaning or low compliance. Previous qualitative studies have reported this barrier to cleaning, as staff report circumventing cleaning near patients to avoid disturbing them. Reference Bernstein, Salsgiver and Simon30 EMS staff also felt that it was more difficult to do daily cleaning when someone was in the bed. We have previously reported that surfaces were less likely to be cleaned when the patient was in the room during daily cleaning. Reference McKinley, Goedken and Balkenende32 Although the VA has national guidance for environmental cleaning procedures, which includes a procedure for daily cleaning for occupied rooms, 31 detail is lacking on how to optimize cleaning around patient care articles and belongings (ie, clutter) that can prevent easy access to environmental surfaces. We previously reported the presence of clutter in both acute-care and LTC settings; the presence of clutter was particularly prevalent in LTC settings. Reference McKinley, Goedken and Balkenende32 These findings may represent opportunities for interventions such as simulation-based competency assessments. Reference Keddington and Moore33
EMS staff were acutely aware of the determinants of environmental cleaning within the context of the physical environment. EMS staff should be involved in the selection of healthcare furniture and finishings as well as healthcare design (or redesign) of patient care areas to ensure that cleaning is optimized. EMS involvement in healthcare design has been recommended previously. Reference Van Tiem, Friberg and Cunningham Goedken34
This human-factors analysis (ie, HFE) of environmental cleaning provides multiple opportunities for interventions. The use of HFE has long been recommended Reference Kohn, Corrigan and Donaldson35 to advance patient safety because it uses the understanding of human performance in complex systems to target and develop interventions. The SEIPS model, which integrates HFE principles and has been adapted for environmental cleaning by another group, Reference Rock, Cosgrove and Keller36 highlights multiple intervention entry points to consider. There is recent interest in collaborative efforts of HFE (understanding of human performance in complex systems) and quality improvement (knowledge of complex systems to make changes) to address sustainability of patient safety interventions. Reference Hignett, Jones and Miller37 Findings from these studies can be used to evaluate interventions in real-world settings such as future quality improvement or implementation science initiatives that address staffing issues through professional recognition and staff training.
The study is the first multisite human-centered work-system analysis of environmental cleaning within VA acute and long-term care. The study findings are limited to a descriptive analysis, but identification of multiple points of entry for intervention have been identified for future study. And although the results are not generalizable to non-VA settings, the VA is the largest healthcare system in the United States, and many of the themes identified will resonate in non-VA healthcare settings.
In conclusion, a work-system analysis using SEIPS identified common determinants of environmental cleaning processes, which provide multiple entry points for interventions. Incorporating cleaning practices that address the determinants identified here may facilitate more standardized cleaning of environmental surfaces. Interdisciplinary collaboration between researchers, especially those with HFE, quality improvement and/or implementation science expertise and healthcare clinical and ancillary staff is needed to develop and test interventions that are systems oriented, person centered, and design driven to standardize environmental cleaning work-system processes. A recent report by our group demonstrated the use of SEIPS to evaluate an antimicrobial stewardship intervention to reduce fluoroquinolone prescriptions in intensive care units. Reference Carayon, Thuemling and Parmasad38 Successful implementation strategies utilized in this project mirrored those identified to be important in our study: leadership, communication, education, and feedback. Future research should evaluate similar implementation or quality initiatives utilizing these strategies when targeting individual work-system components of cleaning, especially those designed to standardize processes that overcome barriers and incorporate best practices.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2023.226
Acknowledgments
We thank the patient and veteran members of the UW–Madison and the Madison VA Patient Engagement in Education and Research (PEER) Group for their partnership in our HAI prevention research. We thank the VA employees and veterans who participated in the interviews for their time and willingness to share their experiences. We thank Ms. Trina Zabarsky, MSN, RN, CIC, FAPIC, Chair of VHA Environmental Programs Service Director’s Advisory Board, for their review of this manuscript.
Financial support
This work was supported by the VA-CDC Practice-Based Research Network, which was funded collaboratively by the VA Health Services Research & Development Service (HSR&D) service, the Centers for Disease Control & Prevention (CDC), and the Collaborative Research to Enhance and Advance Transformation and Excellence (CREATE) program (CRE 12-289, HSR) from the VA HSR&D.
Competing interests
All authors report no conflicts of interest relevant to this article.










