Introduction
In the last two decades, youth sexual and reproductive health concerns have continuously been on national agendas, especially in sub-Saharan Africa. For many countries in the region, this concern has been motivated by the high prevalence of sexually transmitted infections (STIs), especially HIV/AIDs, among young people. For example, sub-Saharan Africa accounts for about 71% of people living with HIV/AIDS globally and more than half of new infections are among young women aged 15–24 (UNAIDS, 2014; Kharsany & Karim, Reference Kharsany and Karim2016). This high prevalence of HIV/AIDs among youth has been primarily attributed to their risky sexual behaviour. These behaviours include non-condom use, having multiple sexual partners, high life-time number of sexual partners, inter-generational sex, transactional sex and early sexual debut (Homma et al., Reference Homma, Wang, Saewyc and Kishor2012; Uchudi et al., Reference Uchudi, Magadi and Mostazir2012; Namisi et al., Reference Namisi, Aarø, Kaaya, Onya, Wubs and Mathews2013). These behaviours have been found to differ by gender and region (Chatterji et al., Reference Chatterji, Murray, London and Anglewicz2005).
For instance, using Demographic and Health Surveys (DHSs) from sub-Saharan Africa, Doyle et al. (Reference Doyle, Mavedzenge, Plummer and Ross2012) reported gender and regional differences in the age at sexual debut of adolescents aged 15–19, with more females (5% to 26%) reporting having first sex before the age of 15 compared with males (2% to 27%), and higher figures being reported in West Africa compared with other regions. Ringheim and Gribble (Reference Ringheim and Gribble2010) showed that less than half of youth aged 15–19 used condoms at last high-risk sex in sub-Saharan Africa, and males were more likely to use condoms than females. They suggested that this may be the result of poverty, which is more likely to affect younger women and reduces their bargaining power in sexual relationships. These findings are similar to those of a number of studies in sub-Saharan Africa on the gender difference in the use of condoms, where young women are consistently found to be disadvantaged (Calsyn et al., Reference Calsyn, Peavy, Wells, Campbell, Hatch‐Maillette, Greenfield and Tross2013; MacPherson et al., Reference MacPherson, Richards, Namakhoma and Theobald2014; Odimegwu & Somefun, Reference Odimegwu and Somefun2017).
Age has also been identified as a predictor of condom use. For example, a cross-sectional survey of random households conducted in 2011 in the Rufiji, Kilombero and Ulanga districts of Tanzania found that women younger than 20 were more consistent condom users than older women (Exavery et al., Reference Exavery, Kanté, Jackson, Noronha, Sikustahili and Tani2012a). However, another study in South Africa concluded that older women were more likely to use condoms than their younger counterparts (MacPhail & Campbell, Reference MacPhail and Campbell2001).
Men have been demonstrated to be more likely to have multiple sexual partners than women (Odimegwu & Somefun, Reference Odimegwu and Somefun2017), but this may be due to under-reporting by women (Clark, Reference Clark2010). Socioeconomic characteristics have also been linked to multiple sexual partnerships for women (Onoya et al., Reference Onoya, Zuma, Zungu, Shisana and Mehlomakhulu2014; Mlambo et al., Reference Mlambo, Peltzer and Chirinda2016), while younger men aged 15–24 have been documented to be more likely have multiple sexual partners (Onoya et al., Reference Onoya, Zuma, Zungu, Shisana and Mehlomakhulu2014).
However, some young people in sub-Saharan Africa are engaging in positive sexual behaviours, in the same environments as those engaging in risky sexual behaviours. There is a growing body of evidence suggesting that an understanding of the protective factors associated with youth sexual behaviour, alongside the risk factors, may better inform sexual health policy (Blum et al., Reference Blum and Mmari2005). An understanding of these protective factors would help promote positive behaviours, and those adolescents who are taking precautions regarding their sexual health would be encouraged (Wang et al., Reference Wang, Zhang and Zimmerman2015).
By definition, factors are called ‘protective’ if they discourage one or more behaviours that might lead to negative health outcomes (e.g. having sex with many partners) or encourage behaviours that might prevent a negative health outcome (e.g. using condoms and contraception). Knowing what these factors are, and how they operate, will not only help target those youth who are at greatest risk of negative health outcomes, but will also help to design more effective programmes and sustain existing interventions encouraging youth to engage in positive sexual behaviours.
At the individual level, religion and HIV knowledge have been documented to be protective factors against early sexual debut among young women in Nigeria (Asubiaro & Fatusi, Reference Asubiaro and Fatusi2014). The literature on the role religion plays in the sexual behaviour of young people has been contradictory and inconclusive (Olivier & Wodon, Reference Olivier and Wodon2015). Using data from slums in Nairobi, Muindi et al. (Reference Muindi, Mudege, Beguy and Mberu2014) found religion to be a protective factor for single sexual partnerships, with the exception of young people of the Islamic faith, which they attributed to Islam’s stance on polygamy. Another study in Nigeria found no association between religion and youth sexual behaviour (Omoteso, Reference Omoteso2006), implying that this association may be dependent on the particular context.
Also at the individual level, gender, self-efficacy and academic achievement have been found to be protective factors for positive sexual behaviour among youth (Marteleto et al., Reference Marteleto, Lam and Ranchhod2008; Clark & Mathur, Reference Clark and Mathur2012). At the family level, family structure, socioeconomic characteristics and parent–child relationship have been found to be associated with positive sexual behaviours among youth. For instance, in a meta-analysis, Widman et al. (Reference Widman, Choukas-Bradley, Noar, Nesi and Garrett2016) established the protective effect of parent–adolescent communication on sexual health for safer sexual behaviour among youth, and this association was stronger for girls. These associations are similar to those of a longitudinal data analysis of unmarried adolescents aged 12–19 in Nairobi, where gender differences were also found (Okigbo et al., Reference Okigbo, Kabiru, Mumah, Mojola and Beguy2015).
Theoretical framework
Studies in developed settings have explored positive sexual behaviour among youth using sociological theories such as resilience theory. The seminal work of Sorokin (Reference Sorokin1950) was the first to draw attention to the need to study positive behaviours of youth. Youth displaying such behaviours can be referred to as ‘outliers’ or young people who ‘beat the odds’. Criticizing the constant focus on negative outcome in the West, Sorokin highlighted the importance of examining the positive to understand the negative. Nevertheless, studies on positive outcomes have been scarce because its viability as a concept has been questioned (Babalola et al., Reference Babalola, Ouedraogo and Vondrasek2007). However, several studies have started exploring positive behaviour among children and youth in the face of adversity in an attempt to shift emphasis from a problem-based approach to one that enhances strengths. Resiliency theory has been identified as a suitable framework for this strength-based approach (Zimmerman, Reference Zimmerman2013). Resilience is the realization of positive outcomes despite adverse circumstances – youth’s capacity to adapt to negative environments. Resilience is multifaceted and context specific.
Using the compensatory model of resilience theory, this study hypothesized that socioeconomic status, as measured by educational attainment and individual-level demographic variables such as age, act as protective factors for youth positive sexual behaviour. It also hypothesized that the results would vary by gender. Finally, it was expected that the factors would differ by region due to different cultural values and norms.
Methods
Data
For the purpose of this study, ‘youth’ are defined as males and females aged 15–24 years, in line with the World Health Organization (WHO) definition (Prata et al., Reference Prata, Weidert and Sreenivas2013), and the term is used interchangeably with ‘adolescents’ and ‘young people’.
The study used data from the most recent Demographic and Health Surveys (DHSs) from sixteen sub-Saharan African countries selected on the basis of data availability and geographical differences: Cameroon (2011), Congo DRC (2013–14), Congo Brazzaville (2011–12) and Gabon (2012) representing Central Africa; Burundi (2010), Kenya (2014), Rwanda (2014–15) and Uganda (2011) representing East Africa; Liberia (2013), Nigeria (2013), Sierra Leone (2013) and Togo (2013) representing West Africa; and Namibia (2013), Malawi (2015/16), Zambia (2014) and Zimbabwe (2015) representing Southern Africa. Data pooling was done to increase statistical power (sample size) and enhance generalizability to sub-Saharan Africa. This was also motivated by the fact that a number of organizations (e.g. WHO) usually present data of this type using a regional perspective, which has been beneficial for programme planning at the regional level.
The DHS programme is a nationally representative, cross-sectional survey conducted in participating countries, typically every five years. The DHS uses a stratified random sampling approach, with clusters providing the primary sampling unit. Within each selected cluster, the DHS randomly samples households. This analysis was based on data from a subsample of never-married young males and females aged 15–24 interviewed in the four sub-Saharan African regions: Central Africa, East Africa, West Africa and Southern Africa. A breakdown of the final sample of never-married youth (40,400 males and 59,464 females) by country and gender is presented in Table 1.
Table 1 Distribution of never-married young people aged 15–24 by country and gender, DHS
Variables
Dependent variable
The dependent variables were ‘positive behaviours’: ‘condom use at last sex’ and ‘single sexual partnership’. Protective factors are those that discourage youth from engaging in behaviours that might lead to pregnancy or STD infection, or encourage behaviours that might prevent them. According to Chin et al. (Reference Chin, Sipe, Elder, Mercer, Chattopadhyay and Jacob2012), positive sexual behaviours include abstinence, contraceptive use and attitude change towards risky sexual behaviours.
In the study, a youth was said to engage in a positive behaviour if she/he reported using a condom at last sexual intercourse and only had a single sexual partner in the 12 months preceding the survey. Condom use was deduced from the question ‘Did you use a condom during last sex with most recent partner?’ The 12-month reference period was useful for capturing most recent behaviours and minimizing recall errors. Youth were coded ‘1’ if they reported use of a condom at last sexual intercourse and ‘0’ otherwise.
Single sexual partnership in the year preceding the survey was derived from the question ‘In the past year, how many people, excluding spouse, have you had sexual intercourse with?’ This was coded ‘0’ if a respondent reported having multiple sexual partners in the 12 months prior to the survey and ‘1’ otherwise. The focus was on number of sexual partners because single sexual partnership constitutes the key mechanism through which young adults can be protected from STIs and HIV infections, which are rapidly spreading across sub-Saharan Africa.
Independent variables
The independent variables considered were socio-demographic characteristics selected based on the study hypotheses and those previous studies have shown to influence sexual behaviours. These included: age, place of residence, wealth status, educational attainment, work status, exposure to mass media, HIV knowledge, delayed sexual debut (first sex after the age 15) and family structure as measured by sex of the household head. Protective behaviours have been documented to be more common among older persons than younger persons in the general population (Stephenson, Reference Stephenson2009; Exavery et al., Reference Exavery, Lutambi, Mubyazi, Kweka, Mbaruku and Masanja2012b), thus age was categorized as 15–17 and 18–24 years.
Place of residence was categorized as ‘urban’ and ‘rural’. This was included because studies in sub-Saharan Africa have shown that youth in urban areas show higher levels of positive sexual behaviour due to the intensity of HIV campaigns, access to HIV/AIDS awareness through the mass media, easy access to condoms, including their availability in public washrooms, and easy access to reproductive health services, including treatment for STDs. Residing in rural areas may therefore be associated with little or no access to condoms.
Previous study results on the effect of wealth status on youth sexual behaviours have been mixed. Wealth sometimes acts as an enabler or compensatory factor and these effects have been found to differ by gender. Wealth was categorized as ‘poor’, ‘middle’ and ‘rich’. Educational attainment has been shown to be associated with young people’s sexual behaviours. Educated youth are more likely to be knowledgeable about reproductive health services, which may translate into positive health behaviours. Educational level was coded as ‘no education’, ‘primary education’ and ‘secondary/higher education’. Work status was measured as a dichotomous variable coded as ‘not working’ and ‘working’. The association between work status and protective behaviours may be difficult to predict for two reasons. On the one hand, being employed can promote protective behaviour by making it possible for a man or a woman to develop life aspirations that make it difficult to have multiple sexual partners. On the other hand, being employed may also increase the inclination to engage in risky behaviour by increasing exposure to opportunities that can be used to address occasional emotional and/or economic needs.
Media exposure was measured from whether respondents reported hearing family planning messages on the radio or TV or reading them in magazines in the last few months. A dichotomous variable was created and coded ‘1’ if respondent responded ‘yes’ to at least two of the forms of media and ‘0’ if otherwise. Knowledge of HIV was measured using questions that captured local misconceptions about HIV (that it is transmitted through mosquito bites and sharing food), comprehensive knowledge of HIV (that having just one uninfected faithful partner can reduce the chances of getting AIDS) and basic knowledge of HIV (knowing that a healthy looking person can have HIV). Youth who answered all these questions correctly were regarded as having ‘high HIV knowledge’; those that did not were classed as having ‘low HIV knowledge’.
Head of household was used as a proxy for family structure and was categorized as ‘male headed’ and ‘female headed’.
Statistical analysis
Univariate analysis was done to show the frequency distribution of youth engaging in positive sexual behaviours. Bivariate analysis was done to examine the independent effect of each protective factor with outcomes. Multivariate analysis was used to model the combined effect of the independent and outcome variables. The results are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The odds ratios provide estimates of the relative hazards for various categories of each covariate, relative to the reference category. Analysis was conducted using STATA (version 14.2). To account for under-sampling and over-sampling in the selected countries, weighing factors were applied at the various levels of analysis with the svy (survey) command in STATA. The DHS documentation for sampling recommends that when pooling DHS datasets, the weights need to be ‘de-normalized’ (ICF International, 2012). This was done by multiplying the weight by the target sample and dividing this by the number of completed cases (sum of the weights), for each survey, because the given sampling weights were country-time specific (Pacifico, Reference Pacifico2014). Also, the study variables of interest were re-named to common names across all the country DHS survey datasets to facilitate comparability and pooling. After pooling the DHS datasets, a new weight variable was created by dividing the DHS supplied weight variable by 1,000,000, as recommended.
Results
Descriptive statistics
Female youth’s rate of condom use at last sex ranged from 26% in West Africa to 55% in both East and Southern Africa (Fig. 1). For males, rate of condom use at last sex ranged from 43% in West Africa to 72% in East Africa (Fig. 2). The incidence of single sexual partnership was highest in East Africa (84% among females and 73% among males) and lowest in Central Africa (54% among females and 46% among males). Tables showing the distribution of respondents by positive sexual behaviours and by selected independent variables for the sub-Saharan African countries considered in the study are available from the corresponding author on request.
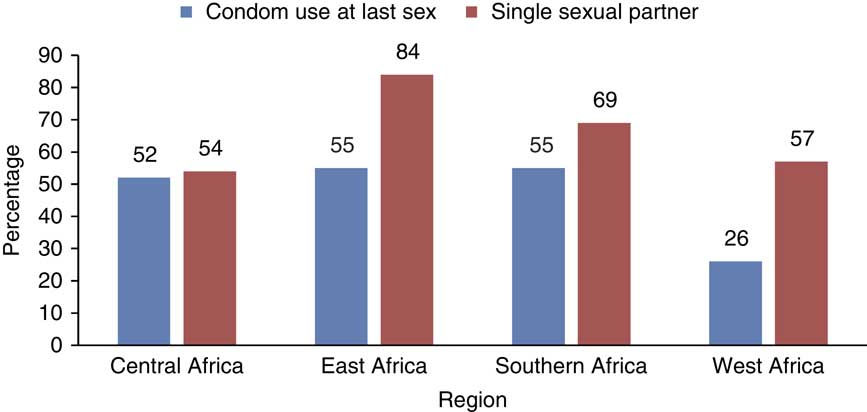
Fig. 1 Positive sexual behaviours of never-married females aged 15–24 by sub-Saharan African region.
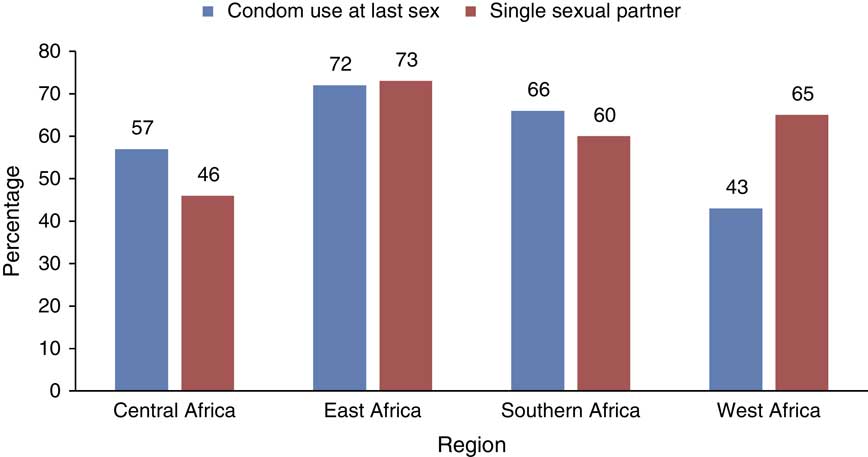
Fig. 2 Positive sexual behaviours of never-married males aged 15–24 by sub-Saharan African region.
Bivariate analysis
Condom use at last sex
The unadjusted associations between selected characteristics and condom use at last sex using bivariate analysis are presented in Table 2. Age was significantly associated with condom use at last sex for both females and males in Central and West Africa. Also, being older (18–24) was associated with increased condom use at last sex for males in East Africa. Rural place of residence was associated with lower odds of using condoms at last sex for females and males in all regions. Education and wealth status were significantly associated with condom use at last sex for both females and males in all regions. Females who were working, in all regions except Central Africa, had lower odds of using condoms at last sex compared with their counterparts who were not working, while males who were working had lower odds of using condoms at last sex in all regions apart from East Africa. Females in female-headed households in Southern Africa were more likely to use condoms at last sex than those in male-headed households. Similar results were seen for males and in West and Southern Africa. Being exposed to mass media was positively associated with condom use for females in all regions except Central Africa, where a negative association was evident. For males, a positive association between mass media exposure and condom use at last sex was evident in all regions. Delayed sexual debut was a strong predictor of condom use for both males and females in all the regions studied.
Table 2 Unadjusted bivariate analysis of condom use at last sexual activity among never-married young people aged 15–24 by region and gender
Ref., reference category.
*p<0.1; **p<0.05; ***p<0.01.
Single sexual partnership
The unadjusted associations between selected characteristics and single sexual partnership are presented in Table 3. Age was significantly associated with single sexual partnership for females and males in all regions. Older females aged 18–24 had lower odds of having single sexual partners compared with females aged 15–17. Rural place of residence was associated with higher odds of having single sexual partners for females and males in all regions except West Africa for males. Females and males who were working, in all regions, had lower odds of having single sexual partners compared with their counterparts who were not working. Similar associations were seen for education, with females and males with higher levels of education having lower odds of having single sexual partners, except for males in West Africa where there was no difference. Females and males in the rich wealth quintile in Central and East Africa had lower odds of having single sexual partners, while in Southern Africa, females in the rich quintile had higher odds of having single sexual partners, and in West African males in the rich quintile had higher odds of having single sexual partners compared with youth in the poor quintile. Females from female-headed household in all regions had lower odds of having single sexual partners compared with their counterparts in male-headed households, while this was the case for males in Central and Southern Africa only. Being exposed to mass media was also associated with lower odds of having single sexual partners among females and males in all regions.
Table 3 Unadjusted bivariate analysis of single sexual partners among never-married young people aged 15–24 by region and gender
Ref., reference category.
*p<0.1; **p<0.05; ***p<0.01.
Multivariate analysis
Condom use at last sex
The adjusted associations between selected characteristics and condom use at last sex using multivariate analysis are presented in Table 4. Age was only statistically significant for positive sexual behaviour among females in Southern Africa (OR=0.66, CI=0.56–0.77). Older females aged 18–24 had lower odds of using condoms compared with their counterparts aged 15–17. On the other hand, males in the East (OR=2.28, CI=1.75–2.97), Southern (OR=1.34, CI=1.41–1.66) and West African regions (OR=1.55, CI=1.24–1.92) had higher likelihoods of using condoms at last sex than females aged 15–17.
Table 4 Adjusted multivariate analysis of condom use at last sex for never-married young people aged 15–24 by region and gender
*p<0.1; **p<0.05; ***p<0.01.
Ref., reference category.
Living in a rural area was not found to be a protective factor for condom use at last sex for females in Central (OR=0.57, CI=0.49–0.66), Southern (OR=0.79, CI=0.68–0.92) and West Africa (OR=0.79, CI=0.68–0.91). Similar results were seen for males in Central (OR=0.69, CI=0.50–0.96) and West Africa (OR=0.74, CI=0.62–0.88). However, males living in rural areas of Southern Africa were significantly more likely to use condoms at last sex than males in urban areas (OR=1.22, CI=1.03–1.44).
Higher education was a protective factor for positive sexual behaviour among youth in all regions for both males and females. Females who were working in Central Africa had reduced odds of using condoms at last sex (OR=0.76, CI=0.68–0.86) compared with females with no education. For males, being employed in East Africa increased the odds of using condoms at last sex (OR=1.27, CI=1.02–1.59) compared with being unemployed. Similarly, residing in a rich household increased the likelihood of condom use at last sex for males and females in all regions studied, except for males in East Africa where the association was not significant.
Exposure to mass media was found to be a protective factor for youth sexual behaviour in all regions for males and females, except for males in East and West Africa. Comprehensive knowledge of HIV increased the odds of condom use at last sex for females in Central (OR=1.21, CI=1.08–1.36), East (OR=1.39, CI=1.15–1.69) and West Africa (OR=1.20, CI=1.07–1.35). For males, this positive association was seen in Central (OR=1.46, CI=1.10–1.93), Southern (OR=1.26, CI=1.11–1.44) and West Africa 1.29 (1.12–1.49). Delayed sexual debut was also a protective factor for youth positive sexual behaviour in Central (OR=1.28, CI=1.13–1.45), Southern (OR=1.37, CI=1.17–1.59) and West Africa (OR=1.46, CI=1.28–1.67) for females; and in Southern (OR=1.51, CI=1.32–1.71) and West Africa (OR=1.51, CI=1.28–1.77) for males.
Coming from a female-headed household in East Africa (OR=1.22, CI=1.01–1.47) was a protective factor for condom use at last sex for females. Males residing in female-headed households in Southern Africa (OR=1.27, CI=1.11–1.45) had higher odds of using condoms at last sex than females in male-headed households while males in female-headed households in West Africa (OR=0.84, CI=0.72–0.98) had lower odds of using condoms at last sex than their counterparts in male-headed households.
Single sexual partnership
The adjusted associations between selected characteristics and single sexual partnership are presented in Table 5. Compared with youth aged 15–17, older youth aged 18–24 had lower odds of having single sexual partners in all regions for males and females. Regional differences were observed in the association between place of residence and positive sexual behaviours. Females residing in rural areas in Central (OR=1.55, CI=1.37–1.74), East (OR=1.76, CI=1.54–2.01) and Southern Africa (OR=1.26, CI=1.13–1.40) had higher odds of having single sexual partners, while their counterparts in West Africa (OR=0.82, CI=0.74–0.90) had lower odds of having single sexual partners compared with females in urban areas. For males, living in rural areas was a protective factor for single sexual partnership in East Africa (OR=1.93, CI=1.69–2.21); conversely, males living in rural areas in West Africa had lower odds of engaging single sexual partnership than males in urban areas (OR=0.79, CI=0.70–0.90).
Table 5 Adjusted multivariate analysis of single sexual partnership for never-married young people aged 15–24 by region and gender
*p<0.1; **p<0.05; ***p<0.01.
Ref., reference category.
Having higher education reduced the odds of males and females engaging in single sexual partnership in all the regions except Southern Africa compared with their counterparts with no education. Similar results were seen for youth who were also employed. Residing in a rich household increased the odds of females having single sexual partners in Central (OR=1.71, CI=1.50–1.9) and Southern Africa (OR=1.61, CI=1.42–1.82). Similar results were seen for males in East (OR=1.18, CI=1.02–1.37) and Southern Africa (OR=1.15, CI=1.02–1.31), but males from rich households in West Africa (OR=0.64, CI=0.55–0.74) had lower odds of engaging in single sexual partnerships compared with males from poor households.
Being exposed to mass media reduced the odds of engaging in single sexual partnerships for males and females in all the regions except in Central Africa.
Comprehensive knowledge of HIV reduced the odds of having single sexual partners among females in Central (OR=0.62, CI=0.57–0.69), Southern (OR=0.75, CI=0.69–0.81) and West Africa (OR=0.67, CI=0.62–0.73). These associations were similar for males in Southern Africa (OR=0.89, CI=0.81–0.97). Delayed sexual debut was associated with increased odds of having single sexual partners among males and females in all the regions studied. Females in female-headed households in all regions had lower odds of engaging in single sexual partnerships than females in male-headed households but this association was only found for males in West Africa.
Discussion
This study documented the prevalence of positive sexual behaviours, i.e. by condom use at last sex and single sexual partnership, among youth in sub-Saharan Africa. The analysis of nationally representative survey data from sixteen countries in sub-Saharan Africa found that a high number (more than half) of young people were engaging in these positive sexual behaviours. The results support the study hypothesis that positive behaviours are strengthened in the presence of individual-level protective factors such as age and educational attainment. The results also support the second hypothesis – that the positive behaviours differ by gender.
Reported levels of condom use among young people have increased over time, but not in all countries, and this study has confirmed this. The study found that reported condom use among young females and males was highest in the Southern Africa region, where HIV prevalence is also highest, and lowest in East and West Africa. Namibia, Gabon and Kenya were the only countries in which female condom use at last sex reached 60%, whereas males in most countries had a rate of condom use at last sex of 60% or more. This corroborates the findings of previous studies of the sexual behaviour of adolescents in sub-Saharan Africa (Doyle et al., Reference Doyle, Mavedzenge, Plummer and Ross2012). Consistent with other findings (Black et al., Reference Black2011; Zembe et al., Reference Zembe, Townsend, Thorson and Ekström2012; Namisi et al., Reference Namisi, Aarø, Kaaya, Onya, Wubs and Mathews2013), condom use was higher among males than in females and this has been attributed to male condom negotiation being mainly controlled by males.
The regional difference in condom use is due to differences in social norms regarding youth sexual behaviour. This could be attributed to changing traditional norms as a result of globalization, which brings about changes in socio-demographic variables such as religion, exposure to mass media, education and the socioeconomic status of young people. The rates at which these changes occur differ by region, which ultimately influences youths’ sexual behaviours. For instance, youth in Southern Africa may be liberal compared with their counterparts in West Africa. This could be the result of policies at the national level of programmes that have been put in place to educate young people on sexual health.
South Africa is one the few countries in the region that have made attempts to introduce sexual and HIV/AIDS education in secondary schools (Thaver & Leao, Reference Thaver and Leao2012). Also, the constitution in South Africa allows young adults to engage in sexual activity without incurring criminal sanctions (Bhamjee et al., Reference Bhamjee, Essack and Strode2016). The practice in South Africa may influence countries like Namibia and Zimbabwe due to their geographical proximity. This is in contrast to countries in West Africa, like Nigeria, where young adults are less likely to express themselves sexually, coupled with the influence of religions like Christianity and Islam, which frown on the implementation of sex education in schools. This limits the information young people have about healthy sexual practices as they get most of their sexual education from friends or social media, which may be misleading.
The results on young people’s HIV knowledge are similar to those of other studies in sub-Saharan Africa, which have shown that, although awareness of AIDS and risk reduction measures like condom use is high, this knowledge is not transformed into positive attitudes and behaviours like consistent condom use. These results correlate with other findings in sub-Saharan Africa, where men are more likely to report multiple sexual partnerships (Onoya et al., Reference Onoya, Zuma, Zungu, Shisana and Mehlomakhulu2014). According to Clark (Reference Clark2010), while both husbands and wives may have extramarital sexual partnerships, men report having sexual relationships outside of marriage far more openly than women. This may be the result of females not reporting their number of sexual partners due to the social stigma associated with female promiscuity. In addition, most African societies may tolerate male promiscuity more than female promiscuity. In some cultures they say ‘male promiscuity does not destroy a home compared to that of a female’.
Gender and regional differences in the association between age and condom use at last sex were evident. There was no difference in the condom use behaviour of younger and older female youth in all regions studied, except Southern Africa where older youth were less likely to use condoms at last sex. This is an unexpected result, especially in the context of Southern Africa where condom use is high compared with other regions. This could be the result of the low stigma attached to unwanted pregnancy in Southern Africa compared with other regions. The results for males are consistent with those documented in the literature. Older males aged 18–24 had higher odds of using condoms compared with their counterparts aged 15–17. This could be because they were more aware of the benefits of using condoms.
At the individual level, education was a protective factor for condom use among females in all regions. This is similar to the findings of other studies. The increase in condom use with secondary or higher education level may be due to the role education plays in societal transformation, and also that education enhances women’s self-esteem, self-confidence, ability to make decisions and freedom of expression. The negative association between condom use and education in Central Africa may be as a result of the instability of some of the countries in the region.
Delayed sexual debut was the strongest predictor of positive sexual behaviour for females in all the regions studied. This shows the importance of existing programmes that support abstinence and delayed sexual debut in sub-Saharan Africa. These include the African Youth Alliance programme in Ghana, Tanzania and Uganda. This aims to improve adolescent sexual and reproductive health (ASRH) in three African countries and reduce the incidence of HIV/AIDS and other STIs. An evaluation of the programme concluded that there was a significant positive impact on behaviours such as condom use and partner reduction (Williams et al., Reference Williams, Mullen, Karim and Posner2007). Because ‘abstinence-only-until-marriage’ programmes have been criticized, programmes and policies sponsored by UNFPA, USAID and other international organizations have sponsored the ABC approach: Abstain, Be faithful and use Condoms. Changes in these sexual behaviours have contributed to a reduction in HIV/AIDS rates in countries like Uganda and Zambia (Green et al., Reference Green, Halperin, Nantulya and Hogle2006; Murphy et al., Reference Murphy, Greene, Mihailovic and Olupot-Olupot2006). Sustaining this progress is important for achieving the sustainable development goals, which have highlighted lack of access to sexual and reproductive health services as a major challenge facing female youth in sub-Saharan Africa.
At the family level, wealth status was seen to be a protective factor for youth condom use at last sex in all regions except Central Africa. Household wealth usually determines individual educational attainment and work status. This may also translate into autonomy for young females, which enables them to negotiate condom use with partners.
This study revealed regional and gendered differences in youth sexual behaviour in sub-Saharan Africa. The sexual behaviours of the youth studied may have been shaped by socio-cultural and gender norms that model different standards of behaviours for females and males. Protective factors such as socioeconomic status must also be strengthened. In addition, programmes must target countries in West Africa where sex education is not as common as it is in Southern Africa. Parents must also be encouraged to discuss with young adults the benefits of engaging in positive sexual behaviours. Public health experts in all sub-Saharan African regions must engage in strategies that are open and more informed, which will help youth sustain positive behaviours and encourage their counterparts who are not doing so already.
This study has several limitations. First, the data came from a cross-sectional survey design so no causal conclusions could be drawn about whether factors associated with positive behaviours can predict behaviours longitudinally. Secondly, data collected on self-reported sexual behaviours may be biased or inaccurate as females may tend to under-report number of sexual partners for cultural reasons, while males may over-report as they think it reinforces their masculinity. Although the data weighting was re-normalized, some countries still had larger samples: for example, Nigeria in West Africa, which may have influenced the results.
Policy implications
These results suggest that programmes aimed at youth should foster a sense of hope and possibility about the future and the development of goals and aspirations to sustain positive sexual behaviours. Family planning providers must look beyond socio-demographic determinants of youth sexual behaviour and provide interventions that consider cultural norms in the region. Parents and religious leaders must help youth make positive decisions that will influence their sexual and reproductive health. These findings provide evidence that youth are engaging in positive sexual behaviours and it is important that programme planners give them the information they need. In order for the sustainable development goals to have the best impact on youth, unbiased comprehensive sexual education should be strengthened as prevention has been proven to be better than cure. Existing programmes should be reviewed to examine how condom use promotion messages have been communicated to youth, and how such messages could be more effectively communicated in the future.
Acknowledgment
The authors acknowledge Kirk Allen of AuthorAid for his editorial input.
Ethical approval. The DHS can be downloaded from the website and is free to use by researchers for further analysis. In order to access the data from DHS MEASURE a written request was submitted to the DHS MACRO and permission was granted to use the data for this survey.
Conflicts of Interest. The authors have no conflicts of interest to declare.
Funding. This research was supported by the Consortium for Advanced Research Training in Africa (CARTA), which is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No. B 8606.R02), Sida (Grant No. 54100029) and the DELTAS Africa Initiative (Grant No: 107768/Z/15/Z). The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS) Alliance for Accelerating Excellence in Science in Africa (AESA) and is supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (UK) (Grant No: 107768/Z/15/Z) and the UK government. The statements made and views expressed in this paper are solely those of the authors.









