Introduction
Laryngeal squamous cell carcinoma (SCC) is the second most prevalent malignancy of the upper aerodigestive tract, with an estimated 13 360 new cases and 3660 related deaths in 2017 in the USA.Reference Siegel, Miller and Jemal1 The incidence of laryngeal SCC peaks between the fifth and seventh decades of life. Over the past years, along with prolongation of life expectancy, the proportion of elderly patients with laryngeal SCC is also increasing.
The elderly are usually classified into young-old (65–75 years), old-old (76–85 years), and oldest-old (over 85 years) groups.Reference Balducci2 Elderly patients are underrepresented in clinical trials, and there are few data from phase III studies to guide the treatment decision-making process for these patients. Furthermore, as most clinical trials use the age of 75 years as a cut-off for defining the elderly,Reference Barzan, Veronesi, Caruso, Serraino, Magri and Zagonel3–Reference Muss10 data on optimal treatment delivery in the oldest-old group of elderly patients (over 84 years) are scarce.
The treatment of laryngeal SCC often includes multimodality therapy, which can be associated with some morbidity, especially in older patients who often have significant co-morbidities and impaired functional status. Therefore, elderly patients may be good candidates for definitive radiotherapy.
Current information regarding treatment selection in the elderly is controversial. Several studies found age to be an important factor in decision-making,Reference Derks, de Leeuw, Hordijk and Winnubst6 while others show that standard curative radiotherapy can be safely performed in selected elderly patients.Reference Huang, O'Sullivan, Waldron, Lockwood, Bayley and Kim7 The present study aimed to examine the characteristics of laryngeal SCC in the oldest-old elderly and compare them with those of the young-old and old-old population. We also evaluated the outcome of radiotherapy as a treatment modality for laryngeal SCC in the over 84 years population.
Materials and methods
A retrospective chart review study was conducted of all very elderly patients (aged over 84 years) with laryngeal SCC treated with radiotherapy with or without surgery, in the Davidoff Cancer Center in Israel, from October 1992 to November 2012. Nineteen such patients had sufficient data for analysis, and comprised the study group. Four patients were excluded because of a lack of data regarding radiotherapy dose and disease recurrence.
Demographic and clinical data were collected from the patients’ files. Parameters assessed included patient age and gender, performance status and co-morbidities, histological diagnosis, treatment modalities, fractionation, recurrence, and survival time. Geriatric evaluation findings and performance status scores were also noted. Staging was determined according to the 2017 American Joint Committee on Cancer classification.Reference Amin, Edge, Greene, Compton, Gershenwald and Brookland11
Multi-segmental intensity-modulated radiotherapy was used to plan and deliver treatment. Treatment volume was individualised by extent of disease. In order to ensure adequate irradiation, tumour volume was outlined on the planning computed tomography (CT) scans. To ensure that the isodoses would adequately cover the targets, a CT-based display of the isodoses was recorded. Treatment was given once daily, 5 days per week, as 2 Gy per fraction of gross disease, and as 1.6–2.0 Gy per fraction of subclinical disease.
Data were analysed using SPSS statistical software, version 22.0 (IBM SPSS, Armonk, New York, USA). Survival time was calculated using the Kaplan–Meier product limit estimate method. Variables were compared between groups using the t-test and the chi-square test. A p-value of less than 0.05 was considered to indicate a statistically significant difference.
The study was approved by the Rabin Medical Center Institutional Ethics Committee.
Results
Patients’ demographic and clinical data are presented in Table 1.
Table 1. Demographic and clinical characteristics
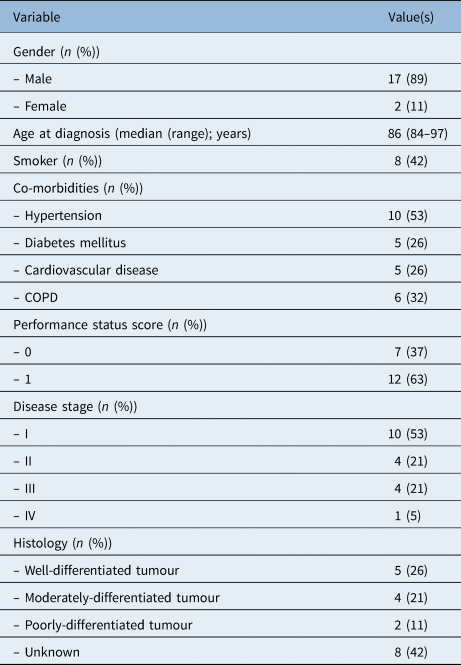
COPD = chronic obstructive pulmonary disease
Nineteen patients (2 females, 17 males) were included in the analysis. Median age at diagnosis was 86 years (range, 84–97 years). Eight patients were reported as smokers. Five patients (26 per cent) had three or more co-morbidities, nine patients (47 per cent) had two, and the rest had one or none. The most common co-morbidity was essential hypertension, with an incidence of 53 per cent. All patients had a good Eastern Cooperative Oncology Group (‘ECOG’) performance status before treatment, with a score of 0–1. Most patients did not receive a specialised oncogeriatric assessment, unless indicated.
Disease stage at diagnosis was I, II, III and IVA in 53 per cent, 21 per cent, 21 per cent and 5 per cent of cases, respectively. After imaging investigation, two patients (11 per cent) were found to have positive nodal disease. All patients presented with SCC. Tumour grade was reported in 11 patients. Twenty-six per cent of patients presented with well-differentiated SCC tumours and 21 per cent presented with moderately-differentiated tumours.
The initial treatment modality was radiotherapy in 14 patients, surgery in 2, chemoradiotherapy in 2, and a multimodality treatment combining surgery and chemoradiotherapy in 1 patient. Of those patients who underwent chemotherapy, two received weekly cisplatin and one was treated with cetuximab. All three completed this treatment.
The median radiotherapy dose was 60 Gy (range, 50–72 Gy) given in 25 fractions (range, 25–35 fractions), over a time period of 5.7 weeks (range, 1.3–8 weeks). In most patients, the radiation field was restricted to the larynx; in two patients with stage III disease, the nodes were treated prophylactically.
Patient outcomes and survival data are presented in Table 2. Three patients had recurrence of disease: one patient had recurrence 16 months after the end of radiotherapy, one patient after 38 months and another patient 10 months following radiotherapy. In all patients, the recurrence was within the gross tumour volume field that had been previously treated. No patient discontinued treatment because of toxicity and there was no radiotherapy-related mortality. Two patients underwent a temporary protective tracheostomy. No other grade 3–4 acute toxicity was reported.
Table 2. Treatment characteristics and outcomes
CRT = chemoradiotherapy
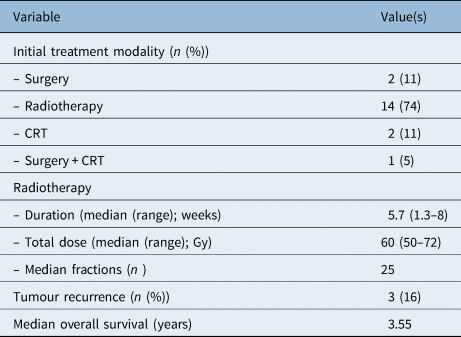
The median overall survival was 3.6 years (range, 0–10 years) (Figure 1), and the median disease-free survival was 2.52 years (range, 0–10 years). Histology, disease stage and radiotherapy dose did not significantly affect survival. Only two patients died from disease recurrence; most patients died of non-cancer-related causes. A cause-specific survival rate curve is presented in Figure 2.
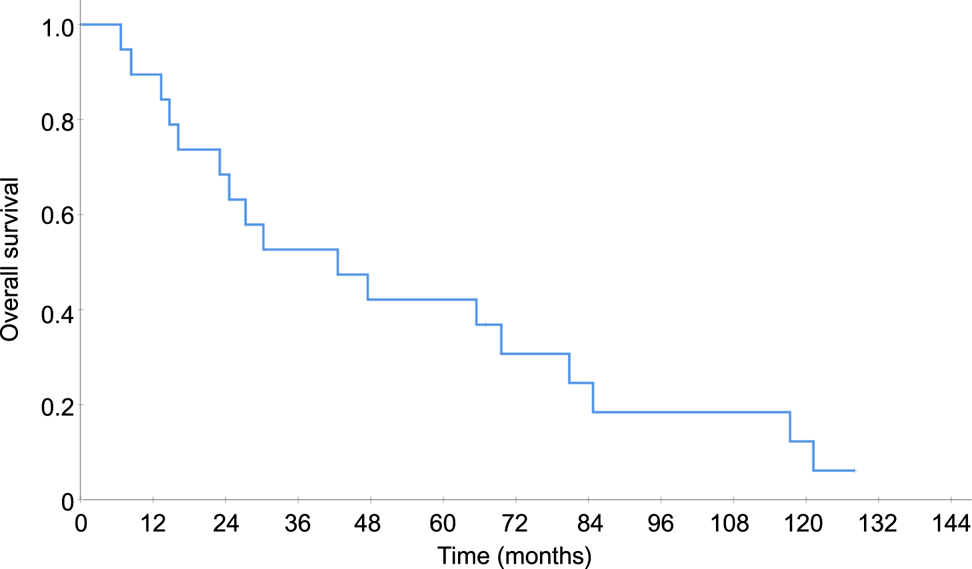
Figure 1. Overall survival.
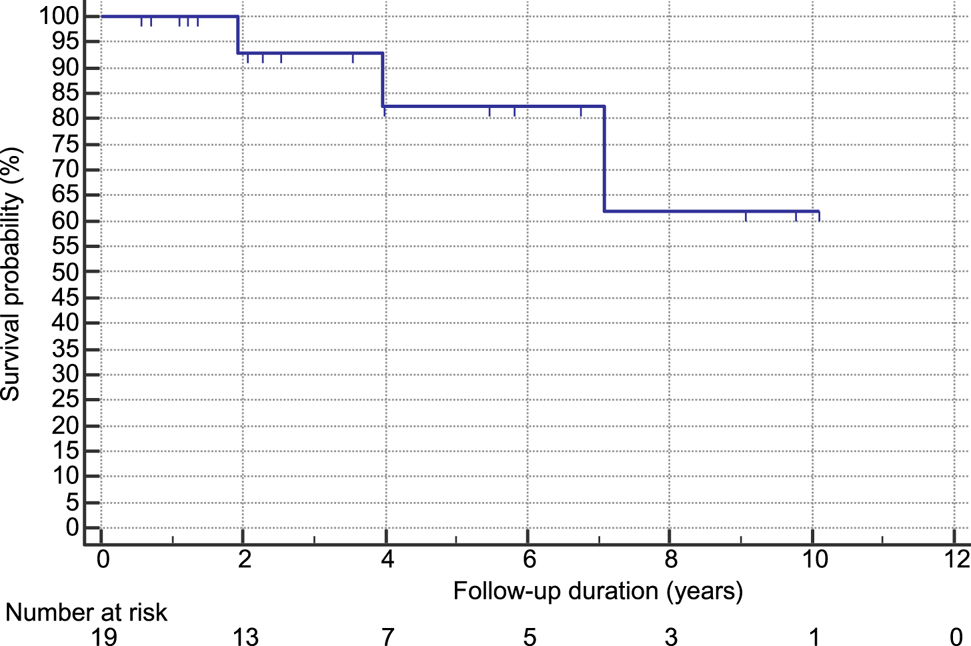
Figure 2. Cause-specific survival curve.
We compared our findings with a similar study performed in our department on 250 young-old elderly patients (mean age, 64 years) with laryngeal cancer (data not yet published). We noted that smoking rates were 76 per cent in the young-old population compared to 42 per cent in the present study. The very elderly patients from the present study tended to have lower rates of advanced disease (stages III–IV) than the young-old patients (26 per cent vs 41 per cent). Similar rates of radiotherapy were noted in both studies (89 per cent), while the chemotherapy rate was lower in the present study (16 per cent vs 43 per cent). Lower rates of recurrence were demonstrated in the very elderly patients (16 per cent, vs 22 per cent in the young-old group). However, median overall survival in the present study was less than the 7.7 years in the young-old patients.
Discussion
In the past few years, along with prolongation of life expectancy in the general population, the incidence of laryngeal SCC in the elderly population has been rising. In the past year, median age at diagnosis of laryngeal cancer was 65 years. More than 22 per cent of new cases of laryngeal SCC occurred in patients aged over 75 years, and 5.5 per cent were over the age of 84 years. The incidence of laryngeal cancer deaths among patients aged over 75 years and over 84 years was 32.2 per cent and 9.9 per cent, respectively.12 With an ongoing ageing of the population, we will likely face increasing numbers of very elderly laryngeal cancer patients in the coming years.
The majority of patients with laryngeal SCC will present with advanced disease (stages III and IV) requiring multimodality therapy.Reference Argiris and Eng13 This often results in significant acute toxicity and long-term morbidity, which can be profound in older patients, along with their co-morbidities and impaired functional status. Subsequently, older patients are often less likely to receive optimal treatment than younger patients.Reference de Rijke, Schouten, Schouten, Jager, Kopperjan and van den Brandt14–Reference Jones19 As long as there is a paucity of clinical trial data available to determine standard management for elderly patients, many may continue to receive non-standard or suboptimal treatment.
At present, recommendations for the management of elderly patients with laryngeal SCC are based on retrospective studies or subset analyses of prospective trials. In primary non-metastatic tumours, surgery and radiotherapy have remained the cornerstones of care.Reference Barzan, Veronesi, Caruso, Serraino, Magri and Zagonel3
The main dilemma in the treatment of this age group concerns the costs versus the benefits of treatment. Curative treatment can include either adequate surgery or radiation with dosage over 60 Gy. However, these treatments may cause temporary side effects, and the question is whether patients will benefit from this attempt or die as a result of it. Another issue is life expectancy at this age regardless of the treatment, and how the treatment or disease will affect this expectancy.
The controversy regarding age as an important factor for treatment selection already existed two decades ago, when Pignon et al.Reference Pignon, Horiot, Van den Bogaert, Van Glabbeke and Scalliet16 published a meta-analysis that pooled data from 1589 patients (26 per cent were over 65 years) enrolled in five European Organisation for Research and Treatment of Cancer (‘EORTC’) trials. Survival and toxicity were examined after splitting the database into seven age categories, three of which belonged to the elderly population (65–69 years, 70–75 years and over 75 years). No differences were observed in overall survival, locoregional control, acute objective mucosal reactions, weight loss or late effects. However, functional mucosal reactions, corresponding to symptoms experienced by the patients, were more common in older adults. Although this age dependency disappeared after adjustment for performance status, it was suggested that elderly people might tolerate acute toxicity less well than their younger counterparts.Reference Pignon, Horiot, Van den Bogaert, Van Glabbeke and Scalliet16 Several subsequent studies noted higher mortality rates among older patients, but concluded this was due to higher co-morbidity status rather than chronological age.Reference Mell, Dignam, Salama, Cohen, Polite and Dandekar20,Reference Ildstad, Tollerud, Bigelow and Remensnyder21
Many studies have shown that older patients receive suboptimal, less aggressive treatment,Reference Olmi and Ausili-Cefaro22–Reference Syrigos, Karachalios, Karapanagiotou, Nutting, Manolopoulos and Harrington24 resulting in lower rates of survival,Reference Sesterhenn, Teymoortash, Folz and Werner23,Reference Syrigos, Karachalios, Karapanagiotou, Nutting, Manolopoulos and Harrington24 while others have noted that elderly patients may achieve comparable outcomes when treated with similar therapies as their younger counterparts.Reference Bernardi, Barzan, Franchin, Cinelli, Balestreri and Tirelli25–Reference Maggiore, Curran, Witt, Haraf, Vokes and Cohen31
Derks et al.Reference Derks, de Leeuw, Hordijk and Winnubst6 divided elderly patients into two groups (aged 70–79 years, and 80 years or more). The proportions of patients receiving standard treatment in the 45–60 years, 70–79 years, and 80 years or more populations were 89 per cent, 75 per cent and 36 per cent, respectively, whereas no treatment was given to 4 per cent, 13 per cent and 18 per cent of cases from the respective groups.
According to Ortholan et al.,Reference Ortholan, Lusinchi, Italiano, Bensadoun, Auperin and Poissonnet32 59 per cent of 200 patients aged 80 years or more and treated with curative intent including surgery and/or radiation therapy received age-adapted treatment. Other studies have shown that standard treatment with curative intent can be performed safely in elderly patients with a good performance status and without severe co-morbidities.Reference Metges, Eschwege, de Crevoisier, Lusinchi, Bourhis and Wibault33,Reference Schofield, Sykes, Slevin and Rashid34
Other retrospective studies found radiotherapy to be feasible for patients aged 85 years and above, although only some of them (approximately 40 per cent) were able to receive standard treatment according to institution policy, being age-adapted in most patients.Reference Zachariah, Balducci, Venkattaramanabalaji, Casey, Greenberg and DelRegato35–Reference Wasil, Lichtman, Gupta and Rush38
Several studies have shown that radiotherapy is effective and well tolerated in the elderly patient population, and advanced age alone should not be considered a contraindicator for radiation therapy.Reference Zachariah, Balducci, Venkattaramanabalaji, Casey, Greenberg and DelRegato35,Reference Yamakawa, Shiojima, Takahashi, Saito, Matsumoto and Mitsuhashi39,Reference Hishikawa, Kurisu, Taniguchi, Kamikonya and Miura40
Geinitz et al.Reference Geinitz, Zimmermann and Molls41 demonstrated a benefit in definitive treatment, even in patients aged over 85 years, with expected survival of more than 4 years, with cure and disease-specific survival rates comparable to those observed in younger patients. The authors highlight the biological and molecular data, which could indicate an increase of ionising radiation sensitivity in the elderly due to a decreased ability to repair DNA damage. They conclude that age itself does not constitute a contraindication for radiotherapy, nor is it an indication for dose reduction.
Another matter of importance concerns fractionation schedules and radiation fields. A large meta-analysis of 15 trials enrolling 6515 SCC head and neck patients, showed that altered radiotherapy, especially hyper-fractionation, improved locoregional control and survival. However, the beneficial effect decreased with advancing age and poor performance status. This was explained by an increased proportion of non-cancer-related deaths in the elderly.Reference Geinitz, Zimmermann and Molls41 Therefore, conventional fractionation (1.8–2 Gy per fraction for five to seven weeks) remains the standard of care for these patients.
Transoral laser microsurgery is another treatment strategy for early laryngeal cancer, although, to our knowledge, randomised, prospective trials comparing transoral laser microsurgery with standard external beam radiotherapy are scarce. Feng et al. Reference Feng, Wang and Wen42 conducted a large meta-analysis comparing outcomes associated with the treatment of T1–T2 glottic cancer. Their analysis demonstrated no significant difference in cure rates between transoral laser microsurgery and external beam radiotherapy. In the setting of recurrent laryngeal cancer, transoral laser microsurgery provides a useful means of surgical salvage.
The present study describes the patient and tumour characteristics, treatment, and outcome of patients aged over 84 years who received radiotherapy for laryngeal SCC. Most patients received a standard and full radiotherapy regimen. Only three patients had disease recurrence 1–3 years following the end of radiotherapy; two of these patients had survival of 3 years and 7 years, and the median overall survival was 3.55 years, suggesting that fit elderly patients may benefit from standard radiotherapy.
Comparison of the results with those from a younger cohort of patients demonstrates lower rates of tobacco use among elderly patients, as previously reported in literature.Reference Koch, Patel, Brennan, Boyle and Sidransky18,Reference Gugić and Strojan43 The very elderly patients with laryngeal cancer in our study tended to be diagnosed with early-stage disease, which differs from findings in other studies.Reference Pignon, Horiot, Van den Bogaert, Van Glabbeke and Scalliet16,Reference Mountzios44 Our patients were treated with less chemotherapy, but had similar rates of radiotherapy, implicating less aggressive treatment. The lower rates of recurrence and median overall survival noted in our study may be explained by the older age of our population.
There are several possible strategies for outcome improvement associated with decreasing treatment toxicity in elderly patients, including omitting chemotherapy, and reducing the radiotherapy dose or field. Whether the neck should be prophylactically treated as in younger patients remains unclear. We treated all but two patients without prophylactic radiation to the neck, while all recurrences occurred within the initial gross tumour volume field, suggesting that a better outcome and less toxicity may be achieved by minimising the radiation field in these patients.
The role of chemotherapy given concomitantly to radiation in the elderly population is controversial in the literature.Reference Tsukuda, Ishitoya, Mikami, Matsuda, Horiuchi and Taguchi45–Reference Merlano, Monteverde, Colantonio, Denaro, Lo Nigro and Natoli48 In our study, only 3 of 19 patients received chemotherapy, with no significant toxicity. These findings for this small number of patients may be hypothesis-generating, but could not be used to draw a general conclusion.
The present study has certain limitations. Firstly, the small cohort makes it difficult to reach statistical significance. However, to our knowledge, no large-scale randomised clinical trials have examined the outcome of radiotherapy in patients aged over 84 years, and the experience with this population is lacking. Secondly, the long follow-up period of the study may lead to certain ambiguities. Nevertheless, treatment modality, age at diagnosis and mortality should not be affected by this.
• Elderly patients are underrepresented in clinical trials, and there are few data from phase III studies to guide treatment decision-making for these patients
• A retrospective chart review was conducted of very elderly (over 85 years) laryngeal squamous cell carcinoma (SCC) patients treated with radiotherapy; all 19 patients had a good performance status
• Multi-segmental intensity-modulated radiotherapy was used to plan and deliver treatment; median dose was 60 Gy
• Three patients had disease recurrence; no patient discontinued treatment because of toxicity and there was no radiotherapy-related mortality
• Very elderly laryngeal SCC patients may derive a similar survival advantage as younger counterparts
• Modern radiotherapy is effective and safe for treating laryngeal SCC in this population
In conclusion, fit very elderly patients with laryngeal cancer, who have few co-morbidities and good geriatric performance status scores, may derive a similar survival advantage as their younger counterparts and should be treated irrespective of their age. Radiotherapy with standard regimens in smaller fields should be strongly considered in this patient population. Nevertheless, more large-scale prospective studies are needed.
Competing interests
None declared






