Introduction
Under-five malnutrition in Bangladesh has decreased over time, but it is still far from meeting the Sustainable Development Goals (SDGs).(Reference Saha, Chattapadhayay and Richardus1) One reason for this malnutrition rate is a lack of adequate dietary diversity among children aged 6–23 months.(Reference Aboagye, Seidu and Ahinkorah2,Reference Borkotoky, Unisa and Gupta3) For the proper development of a child before their fifth birthday, the World Health Organization (WHO) developed an indicator named ‘Minimum Dietary Diversity (MDD)’ for feeding children aged 6–23 months, which is defined as the consumption of five or more food items out of eight food groups.(Reference Solomon, Aderaw and Tegegne4) These eight food groups are: (a) breast milk, (b) grains, roots, and tubers, (c) legumes and nuts, (d) dairy products, (e) flesh food, (f) eggs, (g) vitamin A-rich fruits and vegetables, and (h) other fruits and vegetables. These foods meet a child's daily nutritional needs. If someone received fewer than five of these eight food groups, they were classified as having a minimal dietary diversity deficiency or minimum dietary diversity failure (MDDF).(Reference Borkotoky, Unisa and Gupta3)
It is a matter of concern that few children are receiving a nutritionally adequate diet. Globally, only 29 % of infants and young children aged 6–23 months met the criteria of dietary diversity.(Reference Baek and Chitekwe5) As a result, 149⋅2 million children under the age of five were stunted, 45⋅4 million were wasted, and 38⋅9 million were overweight, which led to a great risk of child death.(6) The past investigations mentioned that less than one quarter of children in Ethiopia practice a minimum level of dietary diversity.(Reference Keno, Bikila, Shibiru and Etafa7,Reference Beyene, Worku and Wassie8) This percentage varies in South Asian countries. For example, 15 % of under-five children received the MDD in India,(Reference Selvaraj, Stephen, Priyadharshini, Radhakrishnan and Ashic9) 47 % in Nepal,(Reference Suresh, Paxton and Pun10) 21 % in Pakistan,(Reference Ali, Arif and Shah11) and so on. According to a 2014 estimate in Bangladesh, only 28⋅8 % of children aged 6–23 months meet the minimum of requirements dietary diversity, and one-third of children under-five do not develop before their fifth birthday, which is not enough to ensure the future of a country's children.(Reference Blackstone and Sanghvi12,Reference Hossain, Haq, Zinnia, Mila and Nayan13) Since nutritional status is perhaps the best indicator of children's well-being,(Reference Haq, Hossain, Parvin, Saleheen, Habib and Chowdhury14) it is therefore important to work towards achieving MDD in the case of Bangladesh.
The reasons for failure in achieving adequate dietary diversity among children aged 6–23 months are numerous and complex. Several studies have been conducted to investigate the determinants of MDD among children in Bangladesh. These studies have highlighted various factors that play a crucial role in determining the MDD, including the residential area,(Reference Blackstone and Sanghvi12) age and sex of the children,(Reference Sheikh, Akram and Ali15) education status of mothers/caregivers,(Reference Ali, Tahsina and Hoque16) wealth index,(Reference Ali, Tahsina and Hoque16) media access,(Reference Blackstone and Sanghvi12) take health facilities during pregnancy and delivery,(Reference Blackstone and Sanghvi12) and working status.(Reference Sheikh, Akram and Ali15) However, despite these efforts, there is still a lack of clear evidence regarding the high prevalence areas of minimal dietary diversity failure, particularly when considering variations between genders. Cultural norms may lead to different food choices for boys and girls, impacting their access to diverse and nutritious diets. The specific risk factors affecting male and female children remain largely undisclosed. To address these gaps in knowledge, the present study aims to comprehensively explore the overall spatial patterns associated with minimal dietary diversity and identify the risk factors influencing dietary inadequacy among boys and girls aged 6–23 months in Bangladesh. By shedding light on gender-specific variations, this research will contribute to a more nuanced understanding of the factors influencing dietary diversity in young children and pave the way for targeted interventions to improve nutrition and overall health outcomes.
Materials and methods
Data source
This study utilised the data and variables from the Bangladesh Multiple Indicator Cluster Survey (MICS), 2019, which is a nationally representative cross-sectional survey. The Bangladesh MICS, 2019 was administered by the Bangladesh Bureau of Statistics (BBS) and funded by UNICEF in Bangladesh.
Sample design and sample size
The Bangladesh MICS, 2019 used a two-stage stratified cluster sampling design, where 3220 enumeration areas were selected in the first stage, and subsequently selected 20 households from each enumeration area in the second stage. The survey covered a total of 64 400 households, and 24 686 mothers/caregivers with children under-five were eligible for the interview. For this study, data were specifically limited to children aged 6–23 months who were currently breastfeeding. Based on this criterion, the weighted sample size for this study was 6092 mothers/caregivers with children aged 6–23 months (comprising 3158 male children and 2934 female children).
Dependent variable
The MDD score for children aged 6–23 months is defined as the proportion of children aged 6–23 months who consumed foods from at least five of the eight food groups within 24 h.(Reference Adubra, Savy and Fortin17) These eight food groups are:
1. breast milk
2. grains, roots, and tubers
3. legumes and nuts
4. dairy products
5. flesh food
6. eggs
7. vitamin A-rich fruits and vegetables
8. other fruits and vegetables
Children who received less than five food groups are categorised as having MDDF, which was the main outcome variable in this study. For pointing out food received for each child i, aged of 6–23 months old in Bangladesh for the food group r,
Then, to analyse the MDDF compliance for each child i, aged 6–23 months, in Bangladesh, we assess whether they received fewer than five food groups out of eight food groups.
That is,
Independent variables
After the literature review, various socio-demographic and economic variables were included as independent/explanatory characteristics of this study, such as children's age group (in months) (6–14 months, 15–23 months), child sex (Male, Female), maternal education (No/Primary, Secondary, Higher+), wealth status (Poor, Middle, Rich), mass media access (Yes, No), institutional delivery (Yes, No), antenatal care (ANC) visit (None, 1–3, 4+), residence (Urban, Rural), and division (Barisal, Chattogram, Dhaka, Khulna, Mymensingh, Rajshahi, Rangpur, Sylhet).
Analytical procedure
A simple descriptive analysis, bivariate analysis, and multivariate analysis were conducted in this study. Descriptive analysis describes the percentage distribution of the variables. In bivariate analysis, this study examines the association between MDDF among currently breastfed children aged 6–23 months and selected independent variables. In this case, the Chi-square test statistic is performed, which can be defined as
where O i and E i are the observed and expected frequency, respectively. The χ 2 statistic asymptotically follows the χ 2 distribution with the degrees of freedom (a − 1) × (b − 1), where a is the number of categories for the independent variable and b is the number of categories for the dependent variable.
In a multivariate set-up, the effect of an independent variable on the MDDF among currently breastfed children aged 6–23 months can be determined using the binary logistic regression model. Let Y i denote the binary dependent variable for the ith observation, where
X i1, …, X ip be a set of independent variables which can be quantitative or indicator variables referring to the level of categorical variables. Since M i is a binary variable, it has a Bernoulli distribution with parameter π i. The dependent of the probability of success on independent variables is assumed to be respectively as
The above relation also can be expressed as
The likelihood is maximised by finding estimates of the parameters that are most likely to give us the data. The maximum likelihood estimator (MLE) of β 0 and β 1 can be obtained by maximising:
The odds ratio with a 95 % confidence interval was usually used to explain predictor variables’ impact.
Software
Data wrangling was conducted using Statistical Package for the Social Sciences (SPSS) version 25, while both analysis and geographical mapping were performed using R-programming version 4.0.0.
Ethical statement
The study utilised publicly available data from the MICS (https://mics.unicef.org/) and downloaded the shape file from the Humanitarian data exchange (https://data.humdata.org/), which was accessible to everyone. Hence, no additional ethical approval was required for this investigation.
Results
Geographical conception of MDDF in Bangladesh
The map presented in Fig. 1 illustrates the percentage of children experiencing MDDF in Bangladesh, categorised by district. The legend represents a gradient from high percentage (red colour) to low percentage (green colour) of MDDF in children aged 6–23 months.
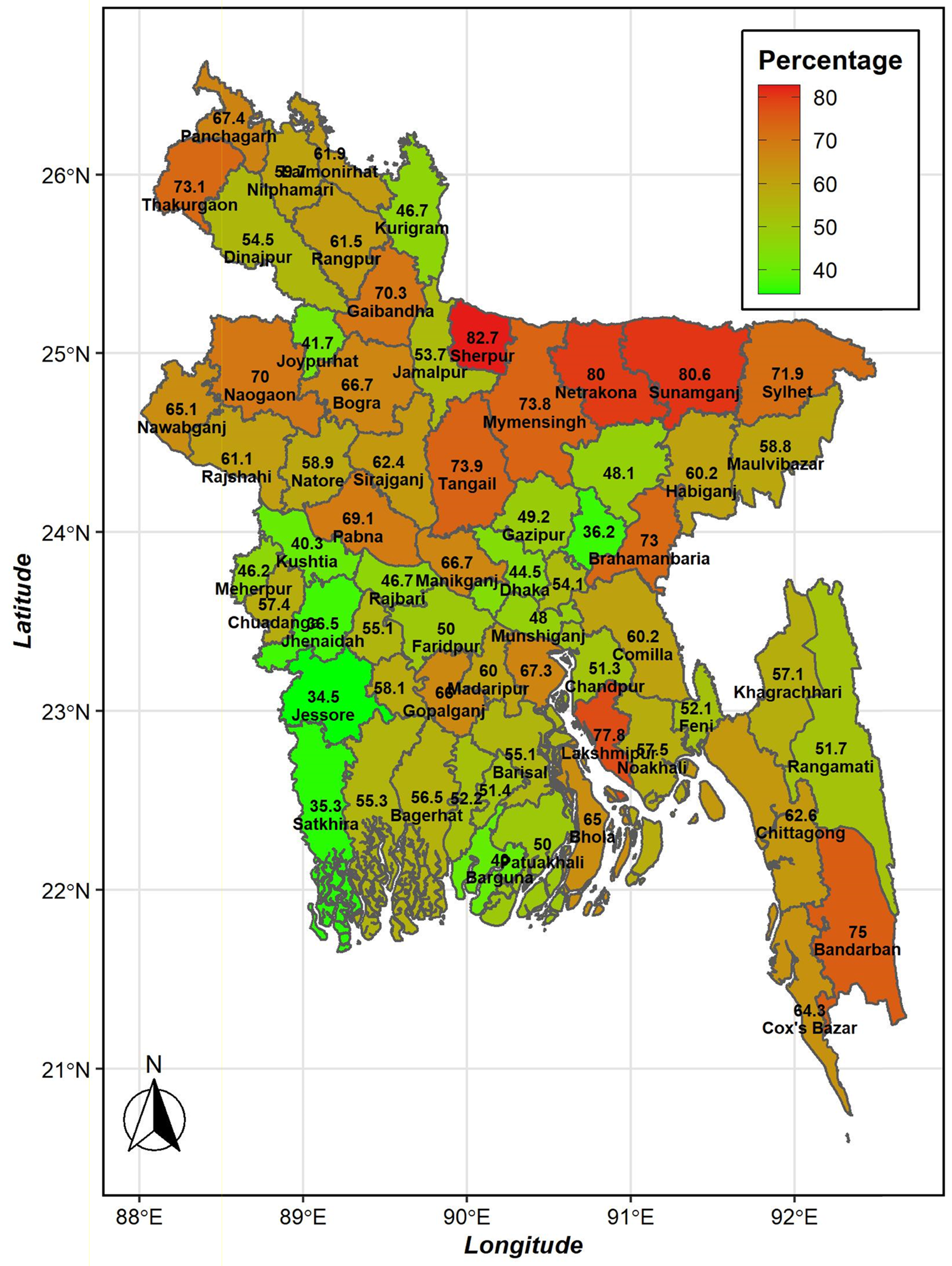
Fig. 1. The proportion of minimum dietary diversity failure found for the 64 districts of Bangladesh from the Multiple Indicator Cluster Survey, 2019.
Prevalence of MDDF in Bangladesh
Fig. 2 presents the gender differences in the prevalence of MDDF among 6–23-month-old children who were currently breastfeeding in Bangladesh. The figure reveals that 59⋅3 % of the children in this age group received less than five food groups. Specifically, 57⋅8 % of these children were male, while 61 % were female. The bar chart clearly demonstrates that the prevalence of MDD among females aged 6–23 was higher compared to males. Furthermore, the proportion test shows a significant difference between male and female children (χ 2 = 6⋅58, P < 0⋅01).
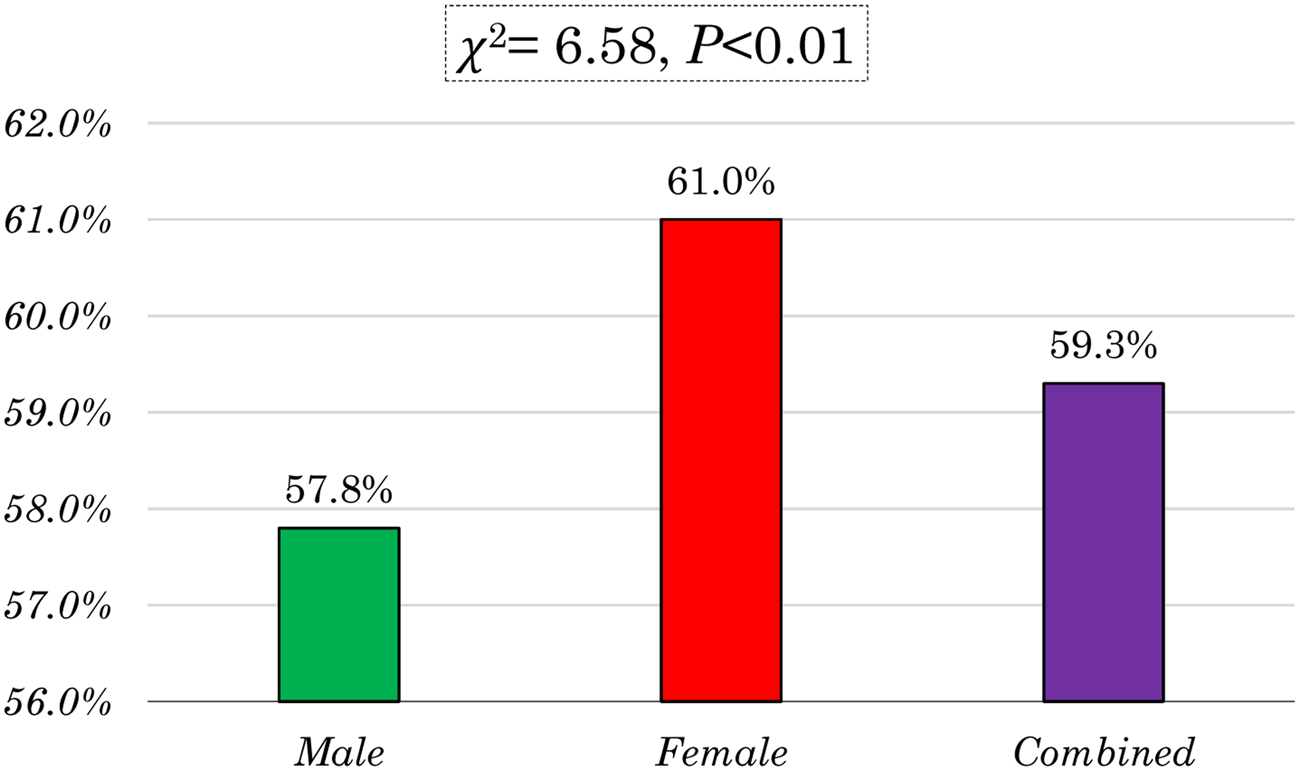
Fig. 2. Gender differences of minimum dietary diversity failure in Bangladesh.
Frequency of consumed food groups
Fig. 3 illustrates the dietary consumption patterns of children within 24 h preceding the survey. Grains, tubers, and roots were the most commonly consumed food group, according to 86⋅2 % of the children's diets. In contrast, the consumption of legumes and nuts was relatively low, with only 19 % of children having included them in their diet.

Fig. 3. Food groups consumed among 6–23 months children in the last 24 h.
Association of socio-demographic and economic factors on MDDF
Table 1 presents the background characteristics of mothers/caretakers and their children included in the study. The largest proportion of mothers resided in Dhaka (23 %) and lived in rural areas (79⋅3 %) of Bangladesh. Nearly half of the respondents had male children (51⋅8 %) and children aged between 6 and 14 months (51⋅6 %). Approximately 41 % of the participants belonged to poor households. Exactly half of the respondents (50 %) had attained a secondary education level. Around two-thirds of the respondents had access to media (60 %), and 45⋅5 % had received 1–3 ANC visits during their pregnancy.
Table 1. Exploring the relationship between minimum dietary diversity failure and selected variables (stratified by gender of child)
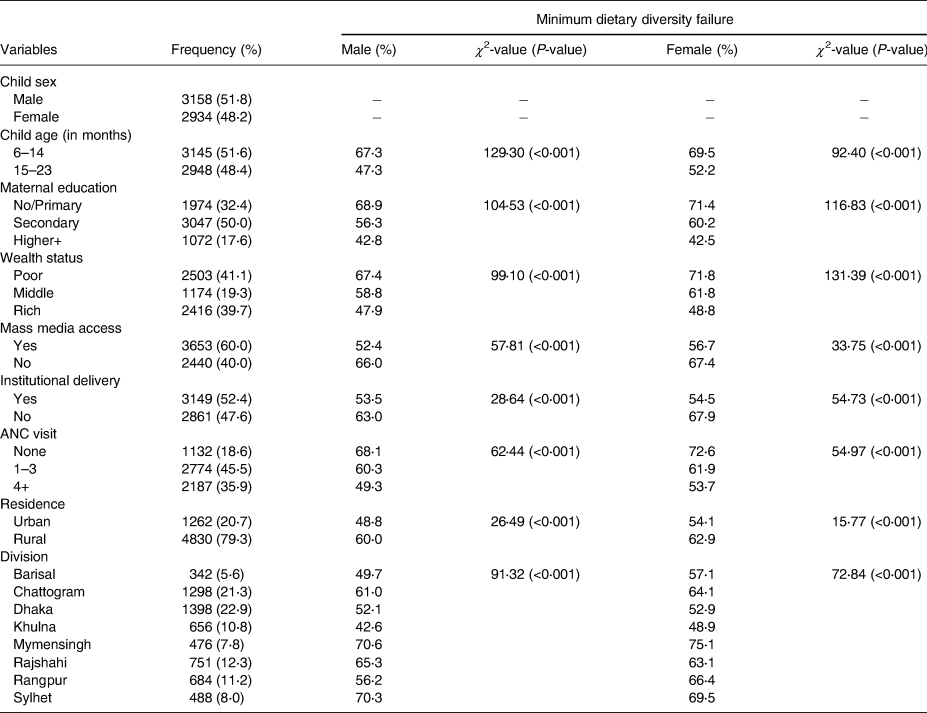
Table 1 also presents the relationship between socio-demographic and economic characteristics and the MDDF among 6–23 months male and female children in Bangladesh. Our analysis revealed significant relationships (P < 0⋅001) between various variables, including child age (in months), maternal educational status, mass media exposure, wealth status, institutional delivery, antenatal visits, residence, and division of both male and female children in Bangladesh.
Children aged 6–14 months exhibited a higher rate of MDDF, with 67⋅3 % for males and 69⋅5 % for females, compared to those aged 15–23 months, where the rates were 47⋅3 % for males and 52⋅2 % for females. Notably, maternal education showed a significant association with MDDF. Children born to mothers with no or primary education experienced higher failure rates, reaching 68⋅9 % for males and 71⋅4 % for females.
Furthermore, wealth status played a crucial role in MDDF, as children from poor households had elevated failure rates, namely 67⋅4 % for males and 71⋅8 % for females. Access to mass media also exhibited a significant association with failure rates, as children from households without mass media access demonstrated higher rates of failure, reaching 66⋅0 % for males and 67⋅4 % for females.
The mode of delivery emerged as another factor, with institutional delivery associated with lower failure rates (53⋅5 % for males and 54⋅5 % for females). Moreover, children whose mothers had no ANC visits exhibited higher rates of failure, reaching 68⋅1 % for males and 72⋅6 % for females.
Residence played a vital role, as children residing in rural areas displayed higher failure rates compared to their urban counterparts, with rates of 60⋅0 % for males and 62⋅9 % for females. Division also demonstrated a significant association, with considerable variation between males and females across different divisions in terms of failure rates.
These findings underscore the importance of considering factors such as age, maternal education, wealth status, mass media access, delivery mode, ANC visits, residence, and division when addressing MDDF. By targeting these factors, interventions can be tailored to reduce the prevalence of malnutrition and improve dietary diversity among children in Bangladesh.
Factors associated with MDD among male and female children
Table 2 presents the outcomes of a binary logistic regression analysis exploring the influence of MDDF among male and female children aged 6–23 months based on various background characteristics.
Table 2. Binary logistic regression analysis showing the effect of minimum dietary diversity failure among male and female children (6–23 months) by background characteristics

Statistical Significance: * P < 0.05, ** P < 0.01, *** P < 0.001.
Table 2 reveals that children aged 15–23 months exhibit significantly lower odds of experiencing MDDF in comparison to their younger counterparts (aged 6–14 months) for both male (OR = 0⋅43) and female (OR = 0⋅45) children.
Furthermore, maternal education plays a noteworthy role in MDD outcomes. Male children whose mothers have attained secondary education demonstrate reduced odds (OR = 0⋅78, 95 % CI 0⋅65–0⋅94) of MDDF in contrast to those with no or primary education. Moreover, the effect is even more pronounced among children with mothers having higher educational attainment (OR = 0⋅56, 95 % CI 0⋅43–0⋅72). Similarly, female children also benefit from their mother's education, with those whose mothers have secondary education exhibiting lower odds (OR = 0⋅82, 95 % CI 0⋅67–0⋅99) of MDDF, and even lower odds for those with higher educated mothers (OR = 0⋅45, 95 % CI 0⋅35–0⋅59).
Economic status, as measured by wealth status, is found to be associated with dietary diversity outcomes. Male children from middle households have reduced odds (OR = 0⋅77, 95 % CI 0⋅62–0⋅95) of MDDF compared to those from poor households. The odds are even lower for male children from rich households (OR = 0⋅62, 95 % CI 0⋅49–0⋅77). Among female children, similar patterns emerge, with those from middle households exhibiting decreased odds (OR = 0⋅84, 95 % CI 0⋅67–1⋅05) of MDDF and those from rich households having even lower odds (OR = 0⋅58, 95 % CI 0⋅46–0⋅73). For male children, those without mass media access have 25 % higher odds (OR = 1⋅25, 95 % CI 1⋅05–1⋅49) of MDDF compared to those with access. However, this association was not statistically significant for female children.
Regarding healthcare factors, institutional delivery has no significant association with MDDF among male children. However, for female children, those born outside of institutional delivery have 21 % higher odds (OR = 1⋅21, 95 % CI 1⋅01–1⋅44) of experiencing MDDF. Likewise, the number of ANC visits by mothers appears to be linked to MDDF outcomes for female children. Children whose mothers had 1–3 or 4+ ANC visits exhibit lower odds of MDDF in comparison to those whose mothers had no ANC visits. For instance, those whose mothers had 1–3 ANC visits exhibit lower odds (OR = 0⋅75, 95 % CI 0⋅59–0⋅95) of MDDF, and the odds are even lower for those with 4+ ANC visits (OR = 0⋅74, 95 % CI 0⋅57–0⋅96).
Residence, whether urban or rural, does not seem to have a significant effect on dietary diversity outcomes for both male and female children, significant variations in odds of MDDF are observed across different divisions for both male and female children.
Discussion
The main objective of this study was to identify risk factors associated with the failure of minimal dietary diversity among boys and girls aged 6–23 months in Bangladesh. Our findings emphasise the urgent need to address the concerning failure rate of achieving MDD. However, approximately two-thirds of 6–23-month-old children do not meet the MDD score in Bangladesh, which was approximately equal to the prevalence observed in Nepal.(Reference Thorne-Lyman, Bevis and Kuo18)
Through bivariate and multivariate analyses, we identified several significant factors associated with inadequate dietary diversity among children. From bivariate analysis, it was found that child age, maternal education, wealth status, access to media, institutional delivery, prenatal care, place of residence, and divisions were significantly associated with inadequate dietary diversity among children. Subsequently, we used the binary logistic regression model to estimate the adjusted effects of these selected covariates.
The present study's finding revealed that the MDDF rate for female children was 3⋅2 % higher than that of male children. The proportion test indicates there was a significant difference between male and female children aged between 6 and 23 months in Bangladesh. This study was consistent with studies conducted in Ethiopia.(Reference Sema, Belay and Solomon19,Reference Bedada Damtie, Benti Tefera and Tegegne Haile20) To gain better understanding of this difference, it is crucial to consider various socio-demographic and economic factors that may contribute to the observed disparity.
The results from binary logistic regression indicate that children aged 15–23 months are less likely to experience a lack of minimal dietary diversity compared to children aged 6–14 months. As children grow older, the risk of not reaching the MDD decreases significantly, as they need a more diverse range of nutrients to support their physical and cognitive development, and failure to meet this changing nutritional need could result in a higher risk of dietary diversity issues. This finding aligns closely with the outcomes of independent studies conducted in Bangladesh and Ethiopia.(Reference Sheikh, Akram and Ali15,Reference Belew, Ali, Abebe and Dachew21)
Maternal education is an important indicator influencing children's health and well-being.(Reference Paul, Paul, Gupta and James22) This study revealed a significant negative association between maternal education and the failure of minimal dietary diversity in both male and female children in Bangladesh. Children with mothers having secondary or higher education faced approximately 18–55 % lower risk of MDDF compared to those born to illiterate mothers. These findings align with another prior study.(Reference Blackstone and Sanghvi12) It is plausible that better-educated mothers tend to have a greater understanding of their children's health needs.(Reference Vikram and Vanneman23)
There was a notable association between wealth status and inadequate dietary diversity in children. The prevalence of insufficient minimal dietary diversity was relatively lower among children in the rich category of the wealth index compared to their counterparts. However, it is essential to highlight that another prior study has demonstrated that children from poor families face a significantly higher risk of MDDF.(Reference Senarath, Godakandage, Jayawickrama, Siriwardena and Dibley24) Hence, policymakers should take initiatives to not only increase education levels but also raise awareness of child health among economically disadvantaged populations.
Based on the findings of this study, media usage emerged as one of the most important and significant predictors of children's health improvement in Bangladesh, applicable to both boys and girls. The mechanism behind this association can be attributed to the role of media in disseminating health-related information and influencing behaviour. In Bangladesh, media, including television, radio, and digital platforms, often serve as vital channels for health education, including proper child nutrition, breastfeeding practices, and awareness campaigns. Children whose mothers had no access to any type of media were more susceptible to MDDF, consistent with another study conducted in Bangladesh.(Reference Blackstone and Sanghvi12)
Mothers who received ANC during pregnancy were less likely to remain in the worst childhood dietary diversity status than mothers who did not use the service. Approximately the same outcome was found in another study conducted in Ethiopia.(Reference Bedada Damtie, Benti Tefera and Tegegne Haile20,Reference Dangura and Gebremedhin25) Obviously, ANC plays a crucial role in children's nutrition status and overall health outcomes.(Reference Kuhnt and Vollmer26) For instance, ANC includes nutrition counselling, supplementations, education on breastfeeding, and so on.(Reference Torlesse, Benedict, Craig and Stoltzfus27) Moreover, the place of birth had a significant impact on the failure of MDD among children, indicating that mothers who did not have institutional deliveries were at higher risk of MDDF in Bangladeshi children. This result is consistent with several previous studies.(Reference Sema, Belay and Solomon19) Both findings suggest that maternal access to health facilities should be ensured during pregnancy to reduce the failure rate in minimal dietary diversity among children. Additionally, the division also showed a significant impact in this study, revealing that dietary diversity failure was significantly higher among children in all regions of Bangladesh.
This study includes an analysis of dietary diversity failure prevalence across various districts of Bangladesh, identifying districts with high rates, including Sherpur, Netrokona, Sunamganj, and Sylhet. Notably, all these districts are flood-affected areas, which probably contributes to the high prevalence. Floods can disrupt food availability and diversity, leading to rapid changes in dietary patterns within these regions.(28)
Strengths and limitations of the study
The strengths of this study lie in its use of nationally representative data, which provides robustness and applicability to the entire population of interest in Bangladesh. Additionally, the study's focus on gender differences offers valuable insights into potential variations in MDDF between male and female children, contributing to a comprehensive understanding of gender-related factors influencing the outcome. Moreover, the study's calculation of prevalence based on district allows for a detailed assessment of geographical disparities in MDDF, enabling targeted interventions and resources allocation in high prevalence districts like Sherpur, Netrokona, Sunamganj, and Sylhet.
While our study provides valuable insights into MDDF risk factors in Bangladesh, it is important to acknowledge its limitations. First of all, due to data limitations, this study is unable to utilise several important factors that are major contributors to MDD among under-five children. Secondly, the cross-sectional characteristics of the data do not allow us to establish causal relationships. On the other hand, it is also crucial to acknowledge the non-significant findings in our study. For example, while certain factors showed significant associations with inadequate dietary diversity in the bivariate analysis, they may not have retained significance in the multivariate analysis after adjusting for other factors. This suggests that the observed associations might be confounded or influenced by other variables included in the model.
Conclusion
Based on the findings of this study, it is evident that the rate of MDD among children aged 6–23 months in Bangladesh is low, especially at the district level. Consequently, there is a crucial need for Bangladesh to prioritise efforts in the district areas to enhance the minimum level of dietary diversity among children aged 6–23 months. Additionally, this study highlights that male children have a lower proportion of experiencing MDDF compared to female children. Therefore, it is essential to address the issue of MDD among girls from low socio-economic backgrounds and mothers with limited or no formal education. In conclusion, the insights obtained from this research can serve as valuable guidance for health policymakers in making informed decisions regarding healthcare in district areas of Bangladesh. Our study provides important policy implications for improving dietary diversity among children in Bangladesh. These include addressing gender disparities, enhancing maternal education, targeting poverty reduction, utilising media platforms for education, and strengthening maternal health services. Implementing these policies can contribute to reducing the prevalence of minimal dietary diversity failure and improving the overall nutritional status and well-being of children in Bangladesh.
Acknowledgements
We express our gratitude to UNICEF for granting us permission to utilise data from the Bangladesh Multiple Indicator Cluster Survey for our research.
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
M. I. H. contributed to the concept and data collection tool; conducted data collection, analysis, and interpretation of data; and wrote the first draft of the manuscript and revised it. S. K. and F. A. Z. contributed to the concept, participated in protocol development, reviewed the assessment tool, and reviewed analysis findings, and revised the draft and final manuscript. All authors read and approved the final manuscript.
The authors declare that they have no competing interests relevant to this manuscript.
In this study, we used data from the Bangladesh Multiple Indicator Cluster Survey, 2019, which is available from https://mics.unicef.org/.







