Introduction
Governance and policy authors have demonstrated renewed interest in policy pilots in recent years (Sanderson Reference Sanderson2002; Heilmann Reference Heilmann2008; Ettelt et al. Reference Ettelt, Mays and Allen2015; Bailey et al. Reference Bailey, Checkland, Hodgson, McBride, Elvey, Parkin, Rothwell and Pierides2017; Hughes et al. Reference Hughes, Yordi and Besco2020). Often, policy piloting has been adopted by governments in the spirit of experimentation, and insights gained from it can inform and refine policymaking. It can be applied to test risky innovations at a confined scale, to delay certain policies, or to advocate innovation (Vreugdenhil Reference Vreugdenhil2010). Many authors agree that it plays a crucially important role in producing policy-relevant knowledge that enables the early evaluation of the potential impacts of new policy initiatives without having major negative impacts societally or professionally (Nair and Howlett Reference Nair and Howlett2016).
China has a long history of policy-pilot use (Heilmann Reference Heilmann2008). In many cases, central government does not issue its policies directly but instead encourages local governments to design and implement their pilot programs to seek the best solutions to resolve societal challenges (Li and Song Reference Li and Song2021). Then it selects the most successful one and upscales it nationwide. This is widely known as proceeding from point to surface (Heilmann et al. Reference Heilmann, Shih and Hofem2013). It has been concluded that policy pilots have hugely facilitated China’s rapid economic development. Authors have even posited that piloting under the hierarchy is a key feature of Chinese government’s adaptive capacity (Heilmann et al. Reference Heilmann, Shih and Hofem2013).
The popularity of policy piloting essentially corresponds with the projectification trend identified by some policy implementation authors; they view policy piloting as a new form of organization for implementing new policies (Hudson Reference Hudson2006; Jensen et al. Reference Jensen, Johansson and Lofstrom2018). A problem with this projectification of public policy implementation is that its use entails some inherent complications that are not sufficiently understood, either by policymakers or in the current research on policy implementation (Jensen et al. Reference Jensen, Johansson and Lofstrom2018, p. 2). To increase our knowledge about this new form of implementation, we must integrate research on project organization with research on policy implementation (Jensen et al. Reference Jensen, Johansson and Lofstrom2018). In policy implementation studies, Matland’s (Reference Matland1995) analytic framework is the most popular and has been widely applied by authors worldwide (Hudson Reference Hudson2006). However, authors have applied it primarily to analyze policy implementation in permanent organization settings. We have little knowledge about its applicability to policy implementation in a temporary organization context (such as a policy pilot). We therefore raise the following research question: how can Matland’s model be adapted to describe the management of policy pilots? To answer this question, we conducted a longitudinal case study on China’s New Rural Cooperative Medical Scheme (NRCMS). The NRCMS is managed by central government and implemented by local governments. This scheme was piloted from 2002 to 2012 and thus provided an opportunity to investigate how it was managed over time. The management of policy pilots refers primarily to the steering and planning approaches adopted by governments to promote policy pilots. Our study contributes to the existing governance and policy literature by adding new building blocks on the management of policy piloting as a temporary form of policy implementation.
Our contribution is structured as follows. We first present our analytic framework, in which the nature of policy pilots and four strategies for managing policy pilots are elaborated. Then, we show the method applied in this study. We apply the single case study approach to examine the management of the NRCMS pilot launched by Chinese Central Government over time. In this section, we elaborate on our case selection reasoning and our data collection and analysis procedures. After that, we show the background regarding Chinese health governance and the operations of the NRCMS. Then, we present our case process regarding the management of the NRCMS. Following this, we elucidate our case analysis and introduce the four strategies for managing the NRCMS pilot over time. The article ends with a discussion section and a conclusion section. The discussion section discusses the implications of the four pilot management strategies identified in this study. The conclusion section summarizes our key findings, key theoretical contributions, and possible limitations.
Analytic framework
Policy pilot
In many countries, policy piloting has become popular in governance processes (Martin and Sanderson Reference Martin and Sanderson1999; Heilmann Reference Heilmann2008; Nair and Howlett Reference Nair and Howlett2016; Hughes et al. Reference Hughes, Yordi and Besco2020). It is a policymaking tool that makes “policy work in accordance with the wishes of their political master” (Bailey et al. Reference Bailey, Hodgson, Checkland, Hodgson, Fred, Bailey and Hall2019, p. 131). Some authors have suggested that policy must be piloted for evidence of its effectiveness to be objectively evaluated (Hodgson et al. Reference Hodgson, Fred, Bailey and Hall2019). Authors define it in terms of many different concepts, such as experiment, social experiment, trial-and-error experiment, demonstration project, and frontrunner project (Vreugdenhil Reference Vreugdenhil2010). Policy piloting represents a form of manipulated emergence, which implies a shift in policy conception from blueprints to broad bright ideas (Harrison and Wood Reference Harrison and Wood1999), or it entails controlled experimentation, which suggests that governments intentionally design and evaluate alternative piloting programs to address uncertainties satisfactorily (Nair and Howlett Reference Nair and Howlett2016). No consensus has yet been reached on the definition of a policy pilot, although many authors agree that it is characterized by five key features: innovation, small scale, field setting, focused on knowledge and learning, and intended to impact policy or society (Vreugdenhil Reference Vreugdenhil2010).
Some authors have concluded that policy piloting has an implicit connection with depoliticized and evidence-informed policymaking (Martin and Sanderson Reference Martin and Sanderson1999). Ettelt and Mays (Reference Ettelt, Mays, Hodgson, Fred, Bailey and Hall2019) have argued that governments adopt policy pilots strategically to depoliticize policy processes in three ways: shifting attention away from the question of the desirability of a new policy to the practical problems of implementation, delegating the responsibility for the success and failure of pilots and policy to local actors, and mobilizing claims to objectivity derived from independent evaluation. Regarding its evidence-based policymaking nature, it is often promised that a policy pilot will be rigorously tested before it is widely rolled out (Ettelt and Mays Reference Ettelt, Mays, Hodgson, Fred, Bailey and Hall2019) in an attempt to replace ideologically driven policymaking with a more rationalist approach (Bailey et al. Reference Bailey, Hodgson, Checkland, Hodgson, Fred, Bailey and Hall2019). This means that policy piloting follows a self-evidently rational trajectory, enabling decision-makers to test the validity of policy promises (Ettelt and Mays Reference Ettelt, Mays, Hodgson, Fred, Bailey and Hall2019).
Often, policy piloting creates a state of exception within which it operates (Bailey et al. Reference Bailey, Hodgson, Checkland, Hodgson, Fred, Bailey and Hall2019). It shares many similarities with other public sector projects and temporary project organizations and could be viewed as part of the projectification phenomenon described in public administration (Hodgson et al. Reference Hodgson, Fred, Bailey and Hall2019). Policy piloting promises to accelerate changes and combines controllability and adventure, enabling decision-makers to try new things under conditions with reduced or eliminated risks (Harrison and Wood Reference Harrison and Wood1999). It can bridge the gap between policymaking and policy evaluation, and meet demands from both of them: one for knowledge and the other for evidence (Sanderson Reference Sanderson2002). Moreover, it fosters social learning for involved actors, and experimenting through policy pilots could be viewed as a form of adaptive governance in one way or another, providing information on whether a design works and on best practices (Hughes et al. Reference Hughes, Yordi and Besco2020).
However, policy piloting has its limitations. Some authors have found that it might serve as the catalyst for policy implementation instead of prioritizing the testing of policy initiatives (Ettelt et al. Reference Ettelt, Mays and Allen2015). Also, governments might design policy pilots as smoke screens, behind which hides a lack of intention and willingness to address complex social problems (Ettelt and Mays Reference Ettelt, Mays, Hodgson, Fred, Bailey and Hall2019). Furthermore, some authors have critiqued the “transplant” logic of policy piloting and the neglect of context (that if x works here, x can be transplanted elsewhere, indeed anywhere else) or have argued that it is often the localized learning process that generates value (so x cannot be transplanted, it must be grown from seed in another setting) (Bailey et al. Reference Bailey, Hodgson, Checkland, Hodgson, Fred, Bailey and Hall2019). Other concerns relating to policy pilots include: short-termism, the difficulty of sustaining change beyond the duration of the pilot, and the messy and emergent nature (Checkland et al. Reference Checkland, Hammond, Coleman, Macinnes, Mikelyte, Croke, Billings, Bailey and Allen2021).
The management of policy pilots
As early as 1995, Rogers (Reference Rogers, Stoetzer and Mahler1995) urged authors to treat policy attributes seriously in investigating innovation diffusion. Other authors followed this line of reasoning and examined how different policy attributes, such as relative advantage, ambiguity, salience, and compatibility, relate to policy processes (Matland Reference Matland1995; Clark Reference Clark2000). In this study, we focus primarily on two attributes of policy pilots, namely, ambiguity and compatibility. Matland’s (Reference Matland1995) four types of policy implementation are based on two attributes of policies: ambiguity and conflict. This framework has been widely applied by authors to describe policy implementation in permanent organization settings. Policy piloting is essentially a type of temporary organizing, and we need to adapt Matland’s framework to better describe its implementation. We argue that ambiguity is a key inherent feature of policy implementation in both permanent and temporary settings. Hence, we retain it as our first key dimension. However, we have adopted the attribute of compatibility rather than conflict as our second key dimension, because compatibility is more relevant for implementation in policy piloting settings, compared to permanent organization settings, given its experimenting nature. These two attributes of policy pilots are elaborated in detail below.
-
Ambiguity: Ambiguity is “a state of having many ways of thinking about the same circumstances or phenomena” (Feldman Reference Feldman1989, p. 5). Often, ambiguity is described as leading only to hesitancy, and, when governments face ambiguous means to achieve predefined goals, they are more likely to be hesitant about promoting the policy pilot at a large scale. However, ambiguity can have some positive implications; it allows situational flexibility, which may be necessary where contexts vary, and empowers local decision-makers or democratic bodies (Hodgson et al. Reference Hodgson, Fred, Bailey and Hall2019). Ambiguity relates mainly to two aspects: the ambiguity of goals and the ambiguity of means. The former is connected with the strategy and vision of policies, whereas the latter relates to the instruments and tools to achieve them (Matland Reference Matland1995). Policy piloting is a specific policy implementation approach, which comes well after agenda setting, where those goals are laid out. Thus, goals should not be ambiguous (Ettelt and Mays Reference Ettelt, Mays, Hodgson, Fred, Bailey and Hall2019). In the remainder of this study, ambiguity refers primarily to the ambiguity of means.
-
Compatibility: The compatibility of policy pilots refers primarily to their fit with the beliefs of potential adopters or existing policy systems (Clark Reference Clark2000). Policy pilots always imply newness or uncertainties for potential adopters, and their compatibility with existing governance systems should be treated seriously. When a policy pilot has a low level of compatibility, governments tend to reconsider its promotion or make necessary adjustments before its full rollout. However, a lack of compatibility can be a positive attribute in that it denotes radical ambition, which may be necessary to make major changes (Bailey et al. Reference Bailey, Hodgson, Checkland, Hodgson, Fred, Bailey and Hall2019). Moreover, a low level of compatibility might encourage governments to pay attention to innovative ideas to gain acceptance (Coleman et al. Reference Coleman, Billings, Allen, Mikelyte, Croke, MacInnes and Checkland2020).
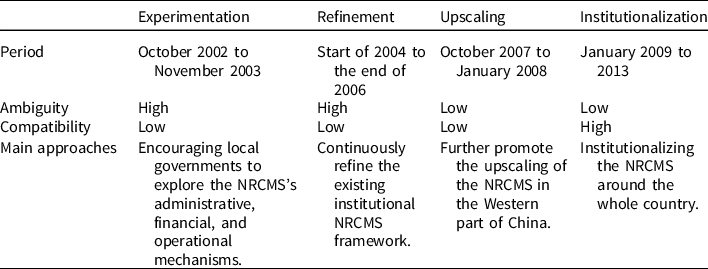
Based on the differences between these two attributes of policy pilots, four strategies for managing policy piloting can be identified: experimentation, refinement, upscaling, and institutionalization (see Table 1). Our implicit assumption is that policymaking about policy pilots essentially takes place in a highly depoliticized context that has experienced relatively small impacts from politics. Hence, investigating policy-pilot management is appropriate from this perspective. These four strategies are elaborated in detail, as follows:
-
1. Experimentation: When governments have no idea about the means to achieve policy goals and recognize that a policy pilot has low compatibility with existing policy systems, they are more likely to adopt an experimentation strategy. This means that they use the policy pilot to promote variation, which entails intentionally crafting various policy alternatives to facilitate the emergence of a successful policy design and solution (Swanson and Bhadwal Reference Swanson and Bhadwal2009). This strategy emphasizes the explorative nature of policy piloting, and governments purposely apply it to gain general insights into the policy’s characteristics, nature, and functions. One example is the Chinese Central Government’s selection of Shenzhen as the experimental zone to accumulate Shenzhen’s experiences in economic development since its inception in 1992 (Heilmann Reference Heilmann2008).
-
2. Refinement: In the face of high ambiguities and high compatibilities, governments tend to look for more evidence to establish causality (Vreugdenhil Reference Vreugdenhil2010). To some degree, this strategy shares many similarities with the concept of controlled experiment, which aims to establish causality to improve effectiveness (Van der Heijden Reference Van der Heijden2014). In governance processes, this strategy implies that governments refine the tools of policy pilots to improve their effectiveness. For instance, central government adjusted the institutional arrangements of the administrative licensing pilot after years of experimentation in several Chinese cities.Footnote 1
-
3. Upscaling: Upscaling implies that the policy means to achieve predefined goals are clear for governments, although the policy pilot’s compatibility with existing policy systems is low. Then, governments are more likely to promote its rollout or to upscale it nationwide (Hughes et al. Reference Hughes, Yordi and Besco2020). Upscaling implies the government’s deliberate efforts to magnify the impacts of its pilots to extend their benefits to more people and develop them sustainably. One example relates to the upscaling of the Sanming healthcare pilot. After its successful piloting in Sanming city, the Fujian provincial government decided to upscale it around the whole province (Li and Song Reference Li and Song2021).
-
4. Institutionalization: Institutionalization implies that when governments know the means to achieve policy goals and the pilot is compatible with existing policy systems, they tend to institutionalize the policy pilot (Sanderson Reference Sanderson2002). Institutionalization implies that a policy pilot has become a formal public policy. Moreover, it has entered the field of policy implementation (Hughes et al. Reference Hughes, Yordi and Besco2020). An example is the institutionalization of the administrative filling procedures around China after a one-year pilot in some pilot cities.Footnote 2
Table 1. Four strategies for managing policy piloting

Our new model, adapted from Matland’s model introduced above, is applied in this study to describe how a policy pilot, the NRCMS, unfolded in the Chinese context. In one way or another, the combination of the four strategies seems an ideal type of sequence of policy adjustment, representing stages in a process with the purpose of piloting policy to reduce ambiguity and increase compatibility.
Method
Rationale for methodology selection
In this instance, a case study is the chosen approach, as it is appropriate for answering how-oriented research questions (Yin Reference Yin2008). The rationale for choosing this approach is that our case is critical and therefore allows us to test how a significant theory – our adapted version of Matland’s (Reference Matland1995) model – is applied. We have two main reasons for choosing the NRCMS case. First, this case is appropriate for answering our research question. The pilot lasted from 2003 to 2013, and it is thus a good option for us to investigate the management of policy pilots over time. Second, we collected sufficient data on the NRCMS pilot to enable us to conduct an in-depth analysis. As one of the best-known policy pilots in Chinese healthcare, the NRCMS has received substantial media attention and scholarly interest, which enabled us to understand its piloting process comprehensively. This study aims to elucidate how a refined model is applied in a single case; and we attempt to test the applicability of this model in a Chinese context, thereby gaining new insights into the management of policy pilots. Regarding the transferability of the conclusions drawn from this study, we follow a naturalistic generalization, implying a process where readers can gain insights by reflecting on the details and descriptions presented in our case study (Stake and Trumbull Reference Stake and Deborah1982). We contend that when readers find that our case descriptions resonate with their experience, they will be prompted to reflect on whether their situations are sufficiently similar to warrant generalization of our findings to their own case.
Data sources
Case study inquiry often relies on multiple sources of evidence to triangulate data. In this study, two sources of evidence have been collected to improve the validity of our case analysis. We first gathered ample secondary data, totaling about 200 news reports, academic papers, and government documents. We used the key search term, NRCMS pilot, to collect media reports from leading mainstream media, including China Central Television, Xinhua News Agency, Renmin Daily, and Guangming Daily, and the official website of the National Health Commission. We also applied the key search term, NRCMS pilot, to collect academic studies from the best-known academic dataset, China National Knowledge Infrastructure, and Web of Science. Furthermore, we conducted semi-structured interviews with 16 respondents through a purposive and snowball sampling approach. Among the respondents, 13 were government officials: seven from the National Health Commission, two from the Health Reform Office of the State Council, and four from local governments’ Health Reform Office. Three were experts familiar with Chinese health governance. Each interview lasted about one hour on average. The affiliations of the 16 interviewees are shown in Appendix 1.
Data analysis
Regarding our data analysis, different strategies were applied to analyze the two types of data sources. The secondary data were analyzed by document analysis, which is particularly applicable to qualitative case studies for providing descriptions of a single phenomenon, event, or program. We followed the step-by-step procedures provided by Miles and Huberman (Reference Miles and Michael Huberman1994) to construct our case process: putting information into different arrays, creating data displays, tabulating the frequency of different events, and ordering information chronologically. Regarding our interview data, content analysis was applied to systematically identify the common themes and categories in our interview transcripts (Miles and Huberman Reference Miles and Michael Huberman1994). An open coding approach was applied to identify emerging themes and categories. We have cited these comments and themes in our case analysis to legitimate our arguments and conclusions (Mele et al. Reference Mele, Esteve, Lee, Bel, Cappellaro, Petrovsky and Ospina2020).
Ethical consideration
To minimize the risk of readers identifying our respondents, our respondents’ names have all been anonymized (Mele et al. Reference Mele, Esteve, Lee, Bel, Cappellaro, Petrovsky and Ospina2020). Furthermore, we encouraged all our participants to openly present their opinions, we confirmed that our study would be used only for academic research, and we assured them that they were free to refuse to answer our questions.
Background
In China, the Health System Reform Leading Group of the State Council plays a leading role in health governance, and it has the highest authority to develop directions and strategies for managing various healthcare issues (Li and Song Reference Li and Song2021). The National Health Commission is responsible for making specific policies and designing frameworks for healthcare at national level, whereas local health commissions are responsible for delivering healthcare services and supervising the delivery of healthcare services (Chen and Zhang Reference Chen and Zhang.2013).
The national healthcare system in China is essentially a multilevel system, with basic medical insurance (BMI) as the pillar and medical aid as the backup, commercial health insurance, charitable donations, and mutual medical aid as supplements (Yi Reference Yi2021). The BMI covers primarily three programs: the Urban Employees’ Basic Medical Insurance (UEBMI), the NRCMS, and the Urban Residents’ Basic Medical Insurance (URBMI). In 1998, central government launched the UEBMI, and all employees in urban regions must participate in this program (Ramesh et al. Reference Ramesh, Wu and Jingwei He2014). In 2003, it launched the NRCMS for rural residents, and the URBMI for urban migrant workers and the unemployed (including the elderly, disabled people, and students) in 2007. Participation is voluntary in both programs (Chen and Zhang Reference Chen and Zhang.2013). At the end of September 2020, over 95% of China’s population was covered by one of the BMI programs (Yi Reference Yi2021). Moreover, the state introduced medical aid to support the low-income population’s participation in BMI by subsidizing their medical costs. Furthermore, many social forces, including the private sector, nonprofit organizations, and donations, have also been allowed to deliver healthcare services to the public.Footnote 3
In this contribution, our main interest lies in the NRCMS pilot. In 1949, China established a rural cooperative medical scheme (CMS). This scheme was developed in rural areas, organized at village level, and managed by the cooperative medical scheme management committee. The village administration provided the premium subsidy to the management committee, which consisted of representatives of the village administration and the village clinic. The villagers paid premiums to the management committee and received reimbursement from it. From 1949 to 1955, the Chinese state emphasized the development of rural health organizations, and villagers mostly did not pay out-of-pocket for medical services (Wang and Liang Reference Wang and Liang2017). In 1955, the first CMS was established in Henan province. After that, many CMSs emerged in rural areas of China. It has been estimated that about one-fifth of the population in rural China belonged to a CMS at the end of 1958. In the 1960s and 1970s, the CMS was promoted around the whole country, and the rate of coverage reached 90% in 1979. The CMS is widely regarded as having one of the best records among all developing countries for safeguarding rural residents’ access to health services for good health and is recognized by the World Health Organization as a template for developing countries to resolve their healthcare problems (Wang and Liang Reference Wang and Liang2017).
However, the CMS coverage rate dropped sharply between 1980 and 1985 with the collapse of the collective economy. Some reports have shown that it dropped from 90% to 5% during this period. Gradually, villagers started paying for their healthcare themselves and transferred to fee-for-service. It was found that villagers had less access to medical services (Muller Reference Muller2017). Even worse, high treatment costs were likely to impoverish rural dwellers. By the late 1990s, over 90% of rural residents did not have medical insurance coverage (Chen and Zhang Reference Chen and Zhang.2013). In the 2003 National Survey on Health Services, it was reported that nearly 85% of rural residents in China stated that they did not seek medical treatment because of their inability to afford it. The problem of illness-induced poverty became an urgent issue on the Chinese political agenda. Consequently, establishing a new medical insurance scheme for rural residents increasingly became a top priority for Chinese Central Government (Muller Reference Muller2017).
In 2002, Chinese Central Government initiated a local voluntary medical scheme at county level, NRCMS. The NRCMS is a government-organized mutual assistance program among voluntary rural residents against serious illness (Gu et al. Reference Gu, Yang, Li, Liang, Zhong and Feng2018). It has three main features. First, it is managed at local government level and subsidized directly from central government’s budget. Previous medical insurance for rural residents was organized at village or township level. County governments initially managed the NRCMS, and now city-level governments do so. Central government’s subsidies are based on the number of enrolled rural residents as well as the financial contributions by county/city and provincial governments (Klotzbucher et al. Reference Klotzbücher, Lässig, Jiangmei and Weigelin-Schwiedrzik2010). Second, Chinese Central Government established NRCMS as a key measure to mitigate high medical costs resulting from illness (Gu et al. Reference Gu, Yang, Li, Liang, Zhong and Feng2018). The scheme focuses on cost reimbursement for serious illnesses and provides financial support for hospitalization only (Chen and Zhang Reference Chen and Zhang.2013). Third, rural residents participate voluntarily in the scheme. Rural residents can enroll or withdraw from the scheme and pay their premiums voluntarily (Chen and Zhang Reference Chen and Zhang.2013). In China, the participation of medical insurance for public employees in public institutions and for employees in state-owned and private enterprises is compulsory. The voluntary nature of of the NRCMS is uncommon; indeed, its voluntary nature has created ambiguities and compatibility issues that have influenced its piloting process.
The operation of the NRCMS involves four main actors: county government, health service providers, New Cooperative Management Scheme (NCMS) fund managers, and rural residents (Mao Reference Mao2005). Among them, county government plays an important role in designing rules for managing the NCMS fund and is responsible for regulating and monitoring the behaviors of all the involved actors (Chen and Zhang Reference Chen and Zhang.2013). It also partially assumes financial responsibilities (for the NCMS fund) and provides subsidies to the participants in the scheme. Rural residents participate voluntarily in the NCMS scheme, and, after paying their premium, they have the right to enjoy the scheme’s benefits (Muller Reference Muller2017). County governments’ health departments often manage the NRCMS fund, and they reimburse rural residents’ healthcare treatment through banks.Footnote 4 The health service providers include public and private hospitals responsible for providing health services to rural residents. The relationship among the four main actors involved in the NRCMS is presented in Figure 1.Footnote 5

Figure 1. The main actors involved and their relationships in NRCMS in local context.
Case process
Four stages can be distinguished in the case, and each stage is characterized by one of the management strategies identified in the analytic framework. In the following, the four stages of the case are elaborated in detail.
Stage 1: Crossing the river by feeling the stones (from October 2002 to November 2003)
At the start of 2002, Chinese Central Government organized the National Rural Health Work Conference, during which it declared that rural residents’ medical insurance problems must be resolved. In October 2002, the Central Committee of the Communist Party of China and the State Council released the Decision on Further Promoting Rural Health Work; this implies that rural residents’ medical insurance entered the Chinese political agenda.Footnote 6 This document publicly emphasized the relevance of establishing a new rural cooperative medical and medical aid system. Moreover, it developed the goal that this system would be formally established nationwide by 2010. The Severe Acute Respiratory Syndrome (SARS) crisis in 2003 further convinced central government to promote the establishment of the NRCMS nationwide (Muller Reference Muller2017). Chinese Central Government officially required every province to select at least two or three counties or cities by the end of May 2003 as a site to pilot the NRCMS. The pilots were expected to explore the NRCMS’s administrative, financial, and operational mechanisms.Footnote 7 In general, the chosen counties had good fiscal and administrative capacities for experimenting with this pilot. The pilot was started formally in July 2003, during which 256Footnote 8 counties piloted the NRCMS, which received support from central government but was based on residents’ voluntary engagement. Individuals, collectives, and the government jointly financed it. Specifically, individual rural residents paid no less than 10 RMB per person annually, rural collectives offered some sponsorship to residents, and local government provided subsidies to residents of no less than 10 RMB per person. Up to October 2003, over 295 counties had piloted the NRCMS in their jurisdictions (Chen and Zhang Reference Chen and Zhang.2013).
Stage 2: Establishing best practices for NRCMS (from the start of 2004 to the end of 2006)
From the start of 2004, the NRCMS was further piloted, but central government publicly announced a stop to the quick extension of NRCMS piloting sites. One key reason for this was that central government was worried that a quick extension might cause unintended and unwanted consequences (respondent 14; respondent 15). After that, the number of piloting sites expanded relatively slowly. In 2004, 333 counties started piloting the NRCMS in their jurisdictions.Footnote 9 On October 22, 2004, the Second NRCMS Conference was organized in Beijing, during which government officials and experts intensively exchanged their ideas about the piloting of the NRCMS. By the end of 2005, 678 counties had experimented with the NRCMS, and its coverage rate reached 75.66%.Footnote 10 By the end of March 2006, over 1369 counties had experimented with the NRCMS. Footnote 11 From March to July 2006, the State Council dispatched a group consisting of experts from Beijing University, the Academy of Social Sciences, and the Economic Research Center of the Agricultural and Rural Ministry of China. It evaluated the performance of 257 counties that had experimented with the NRMCS (Chen and Zhang Reference Chen and Zhang.2013). The expert group chose these counties from the first cohort of 333 pilot counties and concluded that the NRCMS experimentation generally had progressed well.Footnote 12
Stage 3: Upscaling the NRCMS pilot (from October 2007 to January 2008)
In 2007, the Fourth NRCMS Conference was organized in Xi’an city, and central government started promoting the NRCMS upscaling nationwide.Footnote 13 By the end of 2007, about 2451 counties in China had piloted the NRCMS, accounting for 83.54% of rural residents, and the coverage rate reached 86.20%. At this stage, the main concern was that some rural regions in China were in a rather bad financial situation and were still relatively unmotivated to adopt the NRCMS pilot (respondent 13). To cope with this, central government increased its financial subsidies to county governments in those regions to promote the upscaling of the NRCMS. By the end of June 2008, over 95.32% of counties around China had piloted the NRCMS in their jurisdictions.
Stage 4: Shifting the NRCMS from a policy pilot to public policy (from January 2009 to 2013)
In 2009, Chinese Central Government released the Opinion on Deepening Medical and Healthcare System Reforms, which indicated that a high-quality healthcare scheme covering residents in both rural and urban areas would be formally established.Footnote 14 By 2013, the NRCMS, as universal medical insurance, covered over 98.9% of rural residents in China, implying that the NRCMS was formally established as the basic medical insurance system (Ministry of Health of the People’s Republic of China 2014). The NRCMS, piloted by different counties, combines the best practices from different counties. All these counties follow more or less similar institutional frameworks, but their detailed regulations have some differences. For instance, different counties have their own reimbursement regulations, although central government established the general principles and guidelines for these local regulations.
Case analysis
In this section, the four management strategies adopted by Chinese Central Government in managing the NRCMS are elaborated in detail.
Experimentation at Stage 1 is characterized by high ambiguities and low compatibilities
Regarding the ambiguities of the NRCMS pilot, central government was still unclear about how to achieve the predefined goals established by the NRCMS, the overall goal of which is to improve rural residents’ access to healthcare services and help them mitigate the financial risks involved in catastrophic illness (respondent 15). However, achieving this was still a puzzle for central government. Central government had already experimented with two pilots to resolve rural residents’ medical insurance issue in 1991 and 1997, respectively (Muller Reference Muller2016). Both pilots failed, and did not provide useful insights for piloting the NRCMS. Central government hence left the details of the NRCMS program to county governments, and each county was responsible for designing its benefit packages (respondent 7). The coverage and generosity of the NRCMS differed by county. The subsidies received by the counties from central government also differed; they were allocated based on participation rates and financial subsidies from the county and the provincial government (Muller Reference Muller2017). Moreover, central government still had no specific agencies to manage the design and development of the NRCMS pilot. “At the beginning, the NRCMS pilot was managed by a national government agency, primarily in charge of the hygiene issue in rural regions” (respondent 12). Against this background, no unified institutional framework was developed to pilot the NRCMS. Central government at this stage established the principle of rural residents’ voluntary participation in this new scheme. However, it was uncertain whether this voluntary enrollment premium-collection approach would work in practice. As respondent 14 argued, “traditionally, rural residents faced heavy tax burdens, and they had low trust in governments.” Furthermore, several of our respondents had differing viewpoints on the voluntary nature of enrollment premium collection. Some of them, for instance, argued that it should be collected compulsorily to safeguard the sustainability of this program (respondent 13). This further increased the ambiguities of the system.
Regarding compatibility, the NRCMS pilot’s compatibility with the existing healthcare system was low. As mentioned above, the NRCMS pilot was a new institution. Although the earlier CMS system might have provided some lessons for it, it had been terminated many years previously. The NRCMS system was still not well embedded in the existing healthcare system. Moreover, rural residents had rather low confidence in this system and were generally unwilling to participate. As suggested by respondent 15, “initially, many residents thought the NRCMS was a fraud program developed by the government.” Also, local governments sometimes used pressure, force, and coercive approaches in premium collection. This led to conflicts between governments and rural residents that illustrated the low compatibility of the NRCMS nationwide (Muller Reference Muller2017). Moreover, the premium collection was time-consuming, psychologically difficult, and conflict-prone (Muller Reference Muller2016). “For some time, the NRCMS has become a core task for local government, which has taken substantial time and energy for them” (respondent 16). All of this reduced county governments’ interest in piloting the NRCMS in their jurisdictions (Chen and Zhang Reference Chen and Zhang.2013).
In this situation of high ambiguity and low compatibility, central government at this stage did not develop a blueprint for piloting the NRCMS. Instead, it encouraged local governments to find innovative solutions. For instance, it allowed Hubei province to establish a commercial bank as the agency bank – chosen via a bidding procedure – to operate an income-expenditure two-line management system to manage the pilot.Footnote 15 Moreover, central government played mostly a meta-governor role in steering local governments’ piloting. For instance, at the end of 2003, central government organized the First NRCMS (pilot) Conference in Yichang city, Hubei province, during which four provinces piloted the NRCMS in their jurisdictions.Footnote 16 After the conference, central government released Guiding Opinions on the Further Piloting of the NRCMS. These guiding opinions provided concrete requirements for NRCMS piloting, such as site selection, rural residents’ participation, fundraising, and funding management and use (Chen and Zhang Reference Chen and Zhang.2013).
Refinement at Stage 2 is characterized by high ambiguities and high compatibilities
Regarding ambiguity, central government still did not develop a consistent institutional framework for the NRCMS, although it had made many efforts to achieve this. Different counties designed their own pilot programs. Most of them did not establish unified premium-collection mechanisms, and their time schedules for premium collection differed. Also, different county governments adopted different approaches to establishing accounts for rural residents. For instance, there were three options: separate accounts for in- and outpatient treatment; one single account, with different reimbursement ratios for in- and outpatient treatment; or coverage only for inpatient treatment (Chen and Zhang Reference Chen and Zhang.2013). Counties could choose their approaches, leading to different institutional designs in different counties. In short, for central government, the ambiguities of the NRCMS were still high at this stage.
NRCMS compatibility started becoming increasingly high. At this stage, the first cohort of pilot counties increasingly accepted it in their jurisdictions. In particular, after its first round of experimentation, an increase in NRCMS transfers raised the reimbursement rate, making it attractive for rural residents, who increasingly accepted it (Muller Reference Muller2016). “Increasingly, rural residents have found that the NRCMS could reimburse their medical costs, and they saw benefits, which increased their acceptance to this program” (respondent 14). At the end of 2006, about 0.41 billion peasants in rural areas participated in the NRCMS, and its coverage rate reached 80.66% (Chen and Zhang Reference Chen and Zhang.2013).
In this situation of high ambiguity and high compatibility, central government’s primary task was to continuously refine the existing institutional NRCMS framework. Initially, it asked all pilot counties to report their statistics every three months, including the number of people hospitalized, outpatient expenditures, and inpatient expenditures. It analyzed and compared statistics from eastern, middle, and western China, based on which adjustments were made (respondent 16). Generally, central government made key adjustments in three areas at this stage: the organization structure, the premium-collection approach, and the engagement of commercial insurance companies. First, regarding organization structure, it established specific institutions to manage the operation of the NRCMS. Second, as for premium collection, it formally established persuasion and a government subsidy as two key strategies for collecting premiums. Third, it allowed commercial insurance companies to provide medical insurance for rural residents. To safeguard the continuous refinement of the NRCMS pilot, central government set up a technical guidance group that guided and assisted NRCMS implementation around the country. It conducted inspections for at least two weeks every three months and submitted a report to central government about NRCMS promotion countrywide.Footnote 17
Upscaling at Stage 3 is characterized by low compatibilities and low ambiguities
Regarding compatibility, the NRCMS was still incompatible with the existing healthcare system, especially for some counties in the economically underdeveloped western part of China, although it became increasingly popular and accepted in the economically well-developed eastern part of China. The NRCMS was formally piloted in 20 out of 31 Chinese provinces, and it was reported that rural residents’ satisfaction with the NRCMS in Zhejiang province reached 85% at the end of 2007, and in Hubei 93.4%, for instance. However, about 14% of counties, mostly in the western part of China, did not pilot the NRCMS in their jurisdictions (Chen and Zhang Reference Chen and Zhang.2013). Residents in economically underdeveloped regions often had a low acceptance of it. “You could not understand what we have experienced in piloting the NRCMS in some western counties. [Residents there] could not understand what you were talking about, and they did not know relevant regulations. Governments there demanded us to develop proposals for them in piloting the NRCMS” (respondent 14). Hence, central government saw their NRCMS compatibility as still low (Wang Reference Wang2007).
In terms of ambiguity, the NRCMS pilot’s institutional framework was formally established after rounds of refinements. Its institutional framework generally relates to four key dimensions: organization system, financing mechanism, fund supervision and administration, and medical service management (Wang Reference Wang2007). First, for the organization system, local governments established specific institutions for managing the NRCMS, including medical service coordination teams, rural cooperative management commissions, and rural cooperative medical supervision commissions (Chen and Zhang Reference Chen and Zhang.2013). Second, regarding the financing mechanism, it was formally established that the NRCMS fund should come primarily from individual payments of fees, collective sponsorship, and government subsidies (Wang Reference Wang2007). Third, in terms of fund supervision and administration, it was regulated that rural cooperative medical supervision commissions and audit departments would regularly monitor the use of the medical funds; and rural cooperative medical service administrative institutions regularly released information about the NRCMS fund’s revenue and expenditure. Fourth, concerning medical service management, competition was established as the primary approach to select rural cooperative medical service providers.
In situations of low ambiguity and low compatibility, central government adopted different approaches to promote further the upscaling of the NRCMS in the western part of China, where its key strategy was to increase its subsidies to residents there from 10 RMB to 40 RMB to speed up the nationwide upscaling of the NRCMS (Chen and Zhang Reference Chen and Zhang.2013). Furthermore, it applied a hierarchical approach to promote NRCMS upscaling. For instance, it officially demanded provincial governments in the western parts of China, such as Jiangxi province, Guizhou province, Qinghai province, and others, to increase their financial support to safeguard the upscaling of the NRCMS pilot.Footnote 18 Moreover, central government developed training programs specifically for government officials in the western part of China that allowed them to learn best practices in other parts of China (respondent 10).
Institutionalization at Stage 4 is characterized by high compatibilities and low ambiguities
By Stage 4, the ambiguity of the NRCMS was low. As mentioned above, Chinese Central Government had already institutionalized this scheme nationwide. The scheme’s institutional framework had been formally established, and central government knew clearly how the whole system worked and the best practices.
Furthermore, the NRCMS was highly compatible with the existing health governance system in China. Its coverage rate reached 98% by 2013, implying its high popularity and acceptance among rural residents around the country (Chen and Zhang Reference Chen and Zhang.2013). The NRCMS has been found to have played a key role in safeguarding rural residents’ healthcare. Central government’s subsidization has mitigated rural residents’ high healthcare costs by decreasing their out-of-pocket payments (Gu et al. Reference Gu, Yang, Li, Liang, Zhong and Feng2018). As argued by respondent 13, “nowadays, when I conducted interviews with farmers in rural regions, they still talked of the NRCMS. In fact, there was no NRCMS anymore, and it is called the Urban-Rural Residents Medical Insurance. You can see that the NRCMS has been imprinted in the heart of the farmers.” In short, after its institutionalization, the NRCMS had already become a public policy, implying its embeddedness in the existing healthcare system (Muller Reference Muller2016).
In situations of low ambiguity and low compatibility, central government primarily adopted two approaches in further institutionalizing the NRCMS around the country. First, central government improved the NRCMS funding-pool level. Initially, the NRCMS funds were pooled at county level. By Stage 4, they were pooled at city level, thereby offering better risk protection (Muller Reference Muller2016). Second, the NRCMS was further institutionalized by connecting it with another key medical insurance scheme, the URBMI. The NRCMS served primarily residents in rural China, whereas the URBMI served residents in urban China. Two government agencies managed them, and their regulations on payment modes, government subsidies, and reimbursement rates differed. The partition of the two insurance schemes led to much criticism, notably regarding social justice. Ultimately, central government promoted the integration of the two schemes (Chen and Zhang Reference Chen and Zhang.2013). Therefore, residents in rural and urban areas increasingly could access equally high-quality healthcare services (Muller Reference Muller2017).
Discussion
In the above section, we have elaborated on how Chinese Central Government applied four strategies to manage the NRCMS. The relationship between the two policy-pilot attributes and management strategies at four different stages is presented in Table 2.
Table 2. The use of the four management strategies in the New Rural Cooperative Medical Scheme case
As already mentioned, policy piloting is a popular approach adopted by the Chinese Central Government to test new ideas in the healthcare field (Li and Song Reference Li and Song2021). Our study has illustrated how the NRCMS as a pilot was managed in the Chinese context. We have found that in China – a big country with huge regional economic and social differences – policy piloting enables it to design tailor-made policies. We have seen some general routines regarding the management of policy pilots in China, first encouraging local governments to experiment with new ideas to find new ways to achieve policy goals; then allowing some regions (especially economically well-developed regions) to develop their institutional frameworks after iterative refinements and adjustments; then upscaling the refined policy pilots to other regions of China (mostly economically underdeveloped regions); and finally institutionalizing the policy pilots nationwide. This step-by-step policy piloting has its advantages. It allows central government to reconcile the relationship between controllability and adventure; it tries new ideas under limited risks (Harrison and Wood Reference Harrison and Wood1999). Also, it leaves sufficient time for central government to learn and develop tailor-made policies. Central government can continuously accumulate new knowledge, allow involved key stakeholders to develop consensus, and design the most appropriate and effective policies. Moreover, policy piloting produces a positive profile for central government, showing its intention to treat public interests seriously and thereby helping to improve public trust in government. However, this piloting process has its limitations. Because this pilot grants sufficient autonomy to local governments to design their pilots, an unintended consequence is that they might engage in fraud. For instance, they might manipulate the premium-collection process in piloting the NRCMS, potentially decreasing its effectiveness (Muller Reference Muller2016).
Moreover, it is noted that governments might not always adopt the four strategies in a clear linear fashion. As our case is exploratory, it functions as a heuristic tool that enables us to gain preliminary insights into the dynamics of dominant management strategies adopted by central government over time. In practice, these four management strategies might combine with one another. For instance, central government might simultaneously adopt the institutionalization and the refinement strategy. Even when central government had institutionalized the NRCMS pilot, it still attempted to refine it by making minor adjustments. This shows the combined use of the institutionalization strategy and the refinement strategy. We must bear this in mind to better understand our analytic framework. Also, the historical timing of the piloting experience is dynamic and shaped partially by intergovernmental relationships. Before 1994, central government had limited control over local governments. We could see that central government often did not engage in policy pilots in the very early stages. One revealing example is the Household Responsibility System in 1978, during which local governments in Anhui province actively piloted this system, after which central government institutionalized it nationwide. However, after 1994, central government strengthened its control of local governments through the tax-sharing reform. Then, it started to dominate most policy piloting processes, and local governments’ autonomy to make decisions was reduced.
Our study contributes to the existing literature in two ways. First, it contributes to mainstream policy implementation theories by offering a project perspective on policy implementation. As mentioned earlier, many previous implementation studies relate to permanent organization settings (Hudson Reference Hudson2006). Our knowledge of policy implementation through a temporary organization – in this case, a policy pilot – is rather limited, although an increasing number of public policies have been implemented through piloting (Jensen et al. Reference Jensen, Johansson and Lofstrom2018). This study has attempted to link project organization research to policy implementation research, allowing us to understand policy implementation from a project or temporary organization perspective (Jensen et al. Reference Jensen, Johansson and Lofstrom2018). This combination is a key step toward revitalizing the discussion on policy implementation and contributes to our understanding of policy implementation.
Second, this study has further expanded the applicability of Matland’s (Reference Matland1995) policy implementation model to a temporary organization setting. As already mentioned, Matland’s analytic framework is relevant in the policy implementation field and has been widely applied by authors to describe policy implementation in permanent organization settings. Our study has addressed the permanent/temporary gap by adapting Matland’s analytic framework to investigate policy-pilot management. This adapted model has been successfully applied in our study to analyze policy implementation in a temporary organization setting, thereby further extending the applicability of Matland’s model.
Conclusion
Policy piloting has become a new form of organization for implementing public policies. However, it often entails a different institutional context, characterized by limited time/timing, de-politicization, and task orientation (Hudson Reference Hudson2006). The current literature still discusses little about the management of policy piloting as a form of temporary organization for implementing public policies. In this contribution, we have reported an in-depth case study, introducing an analytic framework consisting of four strategies to manage policy pilots: experimentation, refinement, upscaling, and institutionalization. Moreover, the NRCMS case has been elaborated to exemplify the application of these four management strategies. Our study has shown the applicability of the adapted Matland (Reference Matland1995) model for describing policy implementation in temporary project settings, thereby enriching our understanding of general public policy processes.
Last but not least, this contribution has examined how two different policy-pilot attributes influence its management. It is possible that some other policy-pilot attributes, such as relative advantage, salience, or easy installation, may also shape the management of policy pilots. It is expected that authors will conduct more studies in the future to examine this topic. Also, our study focuses on four management strategies adopted by Chinese Central Government for policy piloting. Some issues related to them, such as rules, incentive schemes, hierarchical forms of authority, policy intentions, design, local roles and responsibilities, and evaluative mechanisms, should be comprehensively investigated by future studies. Furthermore, our study fails to provide a systematic explanation of the selection of strategies for governing policy pilots. Qualitative comparative analysis or large-N studies would help to provide a satisfactory answer to this.
Data Availability Statement
This study does not employ statistical methods and no replication materials are available.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0143814X23000338.
Acknowledgements
We are appreciate for the constructive comments of three reviewers and kind sugestions from the editors of Journal of Public Policy.
Funding statement
This research is funded by the National Social Sciences Foundation of China (grant No.: 18BSH170).
Competing interests
The authors have no conflicts of interests.
Appendix 1. Interviewee list






