INTRODUCTION
Literature review
An overview of cancer published by the Australian Institute of Health and Welfare (AIHW) projected that cancer rates would increase by 29% for women and 32% for men between 2001 and 2011.1 Cancers of the head and neck region are no exception; the AIHW overview projected a 28% increase in these cancers for women and a 23% increase for men. Consistent with the increase in the incidence of cancer, unpublished data from the Calvary Mater Newcastle (CMN) Radiation Oncology Treatment Centre (ROTC) show a 38% increase in the total number of courses of treatment for all disease sites between 2002 and 2008. The management of head and neck cancer (HNC) often requires a multidisciplinary approach, with surgical, medical and radiation oncology playing significant roles.Reference Rubin and Williams2
According to literature, it has been estimated that 50% of cancer patients should receive radiation therapy, as either a primary modality of treatment or as an adjuvant combined approach, for both palliative and curative treatment intent.Reference Baume3 The increase in HNC places demands on ROTCs to provide timely access to radiation therapy and on the health-care professionals to meet patients’ holistic needs within the existing service capacity and skill base.
It has been identified that patients requiring radiation therapy experience significant levels of anxiety, distress and feelings of powerlessness prior to and at the beginning of radiation therapy.Reference Söllner, DeVries, Steixner, Lukas, Sprinzl, Rumpold and Maislinger4 In reviewing the psychological impact of cancer on growing populations, Baider et al.Reference Baider, Kaufman, Ever-Hadani and Kaplan De-Nour5 noted that studies of cancer patients found 50% to 60% of patients coped well with the impact of the cancer diagnosis and its treatment; however 40% to 50% experienced psychological distress of varying severity. Prevalence studies that have specifically focused on psychological distress have refined this range.
Carlson and BultzReference Carlson and Bultz6 completed a review of studies documenting distress in cancer patients revealing that between 33% and 45% of cancer patients routinely reported significant distress and Zabora et al.Reference Zabora, BrintzenhofeSzoc, Jacobsen, Curbow, Piantadosi, Owens, Hooker, Owens and Derogatis7 reported 25% to 30% of all newly diagnosed and recurrent cancer patients experience significant elevated levels of emotional distress. Zabora et al. also reported that patients diagnosed with cancer struggle with feelings of anxiety, anger, sadness and depression, and that pre-existing psycho-social conditions impact on the patient’s ability to cope during their treatment journey.
It has been reported that patients diagnosed with HNC have an increased incidence of anxiety and depression due to not only the life-threatening nature of the disease but also the morbidity and disfigurement associated with its management.Reference Katz, Irish, Devins, Rodin and Gullane8 Epidemiological risk factors for HNC, such as the use of alcohol and tobacco, may indicate pre-existing anxiety and distress in these patients.Reference Britton9
Graves et al.Reference Graves, Arnold, Love, Kirsh, Moore and Passik10 indicated that if significant levels of distress are not treated, lung cancer patients are more likely to experience lower quality of life, have lower satisfaction with care, comply less with treatment and possibly have a decrease in survival. A study of HNC patients by HumphriesReference Humphries11 concurred and, in addition, found longer hospital stays were associated with an increase in distress.
It has been established that anxiety and distress often goes undetected by oncologists.Reference Fallowfield, Ratcliffe, Jenkins and Saul12 One study found that oncologists’ perceptions of distress were more pronounced in patients with HNC and lung cancer than for other cancer types.Reference Söllner, DeVries, Steixner, Lukas, Sprinzl, Rumpold and Maislinger4 Even though there have been many studies investigating radiation therapy and psychological function, there is a lack of systematic empirical research.Reference Stiegelis, Ranchor and Sanderman13 A further review of literature found no published research on the ability of radiation therapists (RTs) to detect anxiety and distress.
Rationale
Screening for pre-existing conditions, which are associated with anxiety, can assist in identifying patients with a propensity for elevated levels of distress.Reference Zabora, BrintzenhofeSzoc, Jacobsen, Curbow, Piantadosi, Owens, Hooker, Owens and Derogatis7 In the United States, the Distress Management Panel of the National Comprehensive Cancer Network established guidelines that suggested that all patients with cancer, regardless of stage, should be screened for distress from the first visit and then subsequently at regular intervals.Reference Graves, Arnold, Love, Kirsh, Moore and Passik10 Literature that focused on screening radiation therapy patients for psychological functioning indicates that screening has commenced up to 4 weeks before treatment, first day of treatment, during treatment and the last day of treatment.Reference Stiegelis, Ranchor and Sanderman13
A unique aspect of radiation therapy for HNC is the use of an immobilization device or mask. Radiation therapy for HNC or brain tumour patients requires a number of steps prior to treatment commencing. To deliver treatment accurately, it is acknowledged professional practice to use a firmly fitted mask to secure the patient to the treatment couch.Reference Washington and Leaver14 The photo below shows a patient in position with well- fitted mask and how the mask is secured to the treatment couch (Photograph 1).
The immobilization process is very intimidating for many patients. At times, it may be necessary to suspend a treatment procedure and remove the mask to relieve a patient’s anxiety; then recommence the procedure after a period of time. In some cases this form of intervention is not successful and other strategies may be required. A referral to psycho-oncology may be necessary to manage this level of anxiety, but for more severe cases, medical support for administration of medication may be necessary to recommence the procedure. A study by Rose and YatesReference Rose and Yates15 revealed that patients identified the use of immobilization devices to have a profound negative impact on their radiation therapy experience.
Anxiety and distress experienced by the patient and the subsequent disruption to the procedure may have a flow-on effect that may result in distress for the treatment RTs. An increase in waiting times for the subsequent patients on the treatment schedule may also occur, thus possibly affecting their levels of anxiety.
There appears to be scope for improving the management of patients with HNC experiencing anxiety and distress during radiation therapy. One suggestion is to screen patients for the propensity to experience anxiety and distress, thus preempting a situation where there is a negative impact on the patient and radiation therapy service. However, this suggestion leads to questions that include the following:
• What is a suitable method for screening patients?
• Are RTs able to identify anxiety and distress in these patients?
• What process and procedures are in place to best manage anxiety and distress in these patients?
Aim
This study aimed to
1. Document the prevalence of self-reported anxiety amongst patients requiring an immobilization mask for radiation therapy to the head and neck region.
2. Document the prevalence of anxiety and distress, and associated disruption to the procedures, within this group as reported by RTs
3. Compare the self-reported levels of anxiety amongst this group of patients and the RTs reported levels.
METHOD
Patient sample
Patients eligible to participate in this study were those presenting for radical or palliative radiation therapy with newly diagnosed or recurring HNC requiring an immobilization mask (also included were brain tumour patients requiring immobilization). Patients were excluded if they were unable to comprehend written or spoken English, if they were under 18 years of age or if they were incapable of informed consent (due to illness or neurological impairment).
Ethics
The study received ethics approval from the Hunter New England Human Research Committee (05/09/14/3.14) in November 2005. Accrual commenced in January 2006 and closed in February 2007. The data were de-identified; however, a study number was assigned to ensure it was traceable within the ROTC.
Consent was obtained prior to the patient commencing the radiation therapy process.
Data collection
Data collection time points
Data collection was undertaken at two time points, prior to CT-Simulation (CT-Sim) and prior to fraction 1 of treatment (Fx1).
Tool 1: Patient self-reported anxiety assessment
The Brief Symptom Inventory-18 (BSI-18) was used to assess the patient’s self-reported anxiety levels.Reference Zabora16 It is a standardized assessment with proven validity and reliability in oncology settings.Reference Zabora16 The 18-item questionnaire, which takes approximately 4 minutes to complete, asks patients to rate, on a 5-point scale (0 to 4), how much a problem has distressed or bothered them during the past 7 days. The inventory produces three scale scores (somatization, depression and anxiety) and an overall score, the Global Severity Index (GSI). Somatization is the process where physical symptoms are manifested as a result of psychological distress, and depression focuses on abnormal feelings of sadness and melancholy.Reference Glanze17 Somatization and depression are not the focus of this research. Only the anxiety scores are reported in this analysis. Caseness for anxiety was defined using established community norms on the anxiety sub-scale score (a raw score of 7 or more for males and 8 or more for females).Reference Derogatis18
Tool 2: RT rating of patient anxiety
Overall, RTs provided four ratings for each patient, two ratings at each time point. The first rating at each time point concerned patient anxiety and the second related to the level of disruption to the session due to patient anxiety. Figure 1: Each rating was on a one-item, 5-point Likert-type scale. The first question posed was, ‘How anxious was this patient?’; the end points of this scale were not anxious to very anxious. The second question posed pertained to whether there was a disruption to the procedure due to patient anxiety and the magnitude of the disruption; the endpoints were from no disruption to major disruption. Finally if disruption had occurred, RTs were asked to record any intervention undertaken for the procedure to be completed. Examples of interventions included removing the mask and allowing the patient to rest or have a drink of water, to medical intervention (administration of drug therapy for anxiety) or psychological intervention (progressive relaxation).
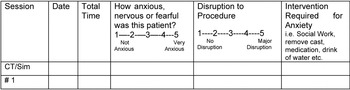
Figure 1. RT Rating Scale for Patient Anxiety
Data analysis
Statistical Package for Social Sciences (SPSS) Version 14 data analysis software was used to calculate frequencies, percentages, cross-tabulations and the correlation (Spearman’s ρ for non-normally distributed data) between the BSI-18 anxiety score and the RT rating of patient anxiety to determine how well the continuous measures were related overall.
The DAGStat program19 was used to examine sensitivity, specificity and Cohen’s κ. Sensitivity is the proportion of patients classified as cases by the test that are cases according to a gold standard. Specificity is the proportion of patients classified as non-cases by the test who are non-cases according to a gold standard.Reference McKinnon20 For this test the patient’s self-report, as measured by the BSI-18, was designated the gold standard, since emotions such as anxiety can be deemed subjective.
κ Values were interpreted according to the classification suggested by Landis and KochReference Landis and Koch21 as follows: 0 = Poor; 0–0.20 = Slight; 0.21–0.40 = Fair; 0.41–0.60 = Moderate; 0.61–0.80 = Substantial; 0.81–1.00 = Almost perfect.
RESULTS
Sample
From January 2006 to February 2007, a total of 147 HNC and brain tumour patients requiring immobilization masks were identified, six did not meet the eligibility criteria and 21 were missed due to issues, such as appointment scheduling. Fifteen (12%) of the remaining 120 patients declined to participate leaving 105 patients who consented to participate in the study (88% of 120)
Seventy patients had complete anxiety data at both time points (58% of 120) by completion of the study. Data from 35 out of the original 105 patients consented was deemed incomplete; this was due to patient schedule and department workload constraints. Participant characteristics are shown in Table 1. The sample was 69% (n = 48) male and the mean age was 67 years, with a standard deviation (SD) of 13. The category is included as an indicator of the impact of radiation therapy on the disease and thus prioritizes the need for access to radiation therapy. Patients categorized as B1 must commence radiation therapy within 21 days of their optimal date for commencing treatment; B2, C and D categories follow.
Table 1. Participant characteristic of patient sample
Missing data for category (n = 2); site (n = 1) and stage (n = 9).
Patient self-reported anxiety
At CT-Sim, 16% (n = 11) of patients were self-reported cases of anxiety on the BSI-18. At Fx1, 14% (n = 10) of patients were self-reported cases of anxiety on the BSI-18
RT rating of patient anxiety and disruption
The participating RTs' experience ranged from 1 year post-qualification to over 25 years post-qualification. The RTs ranged in age from 20 to 55 years of age and the majority (89%) was female. Participating RTs were rostered through all areas of the department at various times and for various durations throughout the data collection period. No record was kept that linked staff members to ratings they provided. This was done with the intention of encouraging staff to feel they would not be judged on their performance. However, it meant that the relationship between staff characteristics, such as experience and accuracy of the ratings could not be examined. In addition, no specific staff member would have been consistently rostered to one area for the entire duration of the study’s data collection period.
At CT-Sim, RTs rated 24% (n = 15) of patients as experiencing some level of anxiety and 13% (n = 8) of patients as having some level of disruption to the session due to anxiety. At Fx1, RTs rated 44% (n = 31) of patients as having some level of anxiety and 24% (n = 17) of patients as having some level of disruption to treatment due to anxiety.
Interventions for anxiety were recorded for 6 of the 8 patients where CT-Sim sessions were considered to be disrupted due to patient anxiety. Verbal reassurance alone was offered to 3 patients, and 3 patients had the mask removed. At Fx1, interventions were recorded for 8 of the 17 patients where there was disruption due to patient anxiety. Three patients received verbal reassurance alone, 3 had mask removal alone and 1 had both of these interventions. Two patients could not complete treatment at Fx1 and were scheduled to receive medication for future treatments. One patient who received mask removal alone refused further radiation therapy after Fx1; at the time, the patient stated anxiety was the reason for ceasing treatment.
Comparison of patient self-reported anxiety with RT ratings
The correlation between BSI-18 anxiety scores and RT rating of patient anxiety at CT-Sim was not statistically significant (ρ = –0.17, p = 0.893), nor at Fx1 (ρ = 0.188, p = 0.119).
At CT-Sim, sensitivity was 0.37 (0.06 to 0.61) indicating that RTs detected 27% of patient self-reported cases of anxiety. Specificity was 0.90 (0.79 to 0.98) indicating that RTs correctly identified 90% of non-cases of anxiety as not anxious. The κ coefficient was 0.20 ((–0.10 to 0.50), p = 0.12); which indicated slight agreement between patient self-report and RT rating of patient anxiety.
Sensitivity at Fx1 was 0.50 (0.19 to 0.81) indicating that RTs detected 50% of patient self-reported cases of anxiety. Specificity was 0.57 (0.43 to 0.69). The κ coefficient indicated slight agreement between patient self-report and RT rating of patient anxiety (κ = 0.04 (–0.14 to 0.21), p = 0.69).
DISCUSSION
Incidence of Anxiety
In this study, 16% of patients self-reported clinically significant symptoms of anxiety at CT-Sim and 14% at Fx1. A review of 45 studies investigating radiation therapy patients, with various types of cancer, also found that anxiety was common prior to treatment, with 10% to 20% of patients feeling anxious prior to radiation therapy, followed by a decline over the course of treatment.Reference Stiegelis, Ranchor and Sanderman13 In studies with HNC patients, data indicate a prevalence of distress in 20% to 32% of patients prior to treatment, and in some studies anxiety increased over the course of treatment.Reference Stiegelis, Ranchor and Sanderman13,Reference Washington and Leaver14,Reference Chen, Jennell, Grady, Tovar, Bowen, Simonin, Tracy, McCrudden, Stella and Vijayakumar22–Reference Kohda, Otsubo, Kuwakado, Tanaka, Kitahara, Yoshivura and Mimura24 The reason for this increase has only been postulated.
According to Haman,Reference Haman25 many HNC patients have pre-existing psychological issues that affect levels of anxiety and distress, and these can be exacerbated as treatment progresses. In particular the effect of pain on distress is documented in the literature.Reference Haman25 Other side-effects related to treatment and associated with distress include disfigurement and dysfunction and problems communicating with caregivers, which in turn affects social support mechanisms.
One factor that may explain the variation in anxiety rates between studies is the use of different screening tools for anxiety. Another factor may be the differing time points at which anxiety was measured. A review of literature by StiegelisReference Stiegelis, Ranchor and Sanderman13 found the time of screening varied and it showed no other studies measured anxiety immediately prior to CT-Sim; however, as previously mentioned, screening was undertaken up to 4 weeks before radiation therapy and before Fx 1. This study included the two fixed time points in an attempt to capture the anxiety associated with the procedure.
Comparing patient self-report and RT-rated incidence of anxiety
This study of HNC patients undergoing radiation therapy found slight agreement between the patients’ self-reported anxiety and the RTs’ rating of the patients’ anxiety. Further, the percentage of patients classified as anxious based on self-report did not significantly change between CT-Sim and Fx1, yet the number of patients considered by RTs to be experiencing anxiety, and session disruption due to anxiety, doubled from CT-Sim to Fx1.
The increase in RT ratings could reflect the RT attention to patient anxiety, perhaps as a result of the study. The higher level of identification of anxiety resulted in increased sensitivity at Fx1 compared to CT-Sim (0.50 compared with 0.37), but still about half of the self-reported cases were missed.
The increase in disruption from CT-Sim to Fx 1 (13% to 24%) may reflect the patients being sensitized to the discomforts of the procedure or the patient’s realization that at Fx 1 their radiation therapy would be actually delivered.
The main question that arises from this data is which best represents patient anxiety levels, patient self-report or RT ratings. Even though patient self-reporting with the BSI-18 ideally is the most accurate measure, the disruptions to procedures due to anxiety appear to indicate that possibly the patients have under-reported their levels of anxiety and that RTs have over-rated patients’ anxiety levels.
Strengths and limitations
The strengths in this study are limited. The original sample was intended to be an accurate representation of patients requiring immobilization masks; however, due to the issues regarding incomplete data, the significance was reduced. A proposed strength is that the measurement of anxiety ratings immediately preceding CT-Sim and Fx1 provided two fixed time points. This ensured both patient self-report and RT ratings were completed within a short amount of time of each other.
In terms of limitations, the adequacy of the measurement tools chosen for this study must also be considered. Even though the BSI-18 is validated for use in cancer patients, it may be too general to identify anxiety relevant to the disruption of CT-Sim and treatment procedures. It would be prudent to compare the BSI-18 with other validate tools. With regard to the RTs’ rating of the level of disruption due to anxiety, there was no validated questionnaire available, and it was not possible to examine inter-rater reliability. Even though the percentage of cases of disruption was clinically significant, the overall number of cases was small and limited the statistical power of the study to find associations.
Implications for clinical practice
It is acknowledged in this study that patient self-report is the best option available for the formal screening of patient anxiety. However in the absence of formal screening and a validated RT-rating assessment tool, it would be of benefit in the short term for RTs to improve their ability to identify patient anxiety. Second, the low rate of recorded intervention in cases where patients were significantly distressed, such that the treatment session was disrupted, suggests that RTs may need to improve skills in the management of patient anxiety.
One possible method for improving RT knowledge and skills in the identification and management of patient anxiety is in-service education and training. It is recommended that these be provided by experts in psycho-oncology. This is not to suggest that the RTs become experts in the screening and management of these conditions. However, it can be considered prudent for RTs to have the knowledge and ability to identify at-risk patients and assist in the management of mild cases.
A further recommendation is that RTs form part of a proposed two-tier strategy in the management of anxiety and distress. The first tier could involve RTs intervening when low levels of these conditions are detected, thus reducing the need for immediate referral to psycho-oncology or medical services. When higher levels of anxiety and distress are identified, then the second tier of intervention would be initiated. This would involve appropriate referral to psycho-oncology or medical services.
Ideally, the combination of routine screening of patients prior to CT-Sim, using validated assessment tools and training RTs in identification, management and referral for anxiety could result in an increased level of care for these patients.
CONCLUSION
There were only slight levels of agreement between patient self-reported levels of anxiety and RTs’ ratings of patient anxiety prior to radiation therapy for HNC patients requiring immobilization masks. Since untreated anxiety is unpleasant for patients and can have serious consequences, further investigation into the development of routine screening with appropriate assessment tools and RT education and training in assessment and management of anxiety and distress is recommended.
Acknowledgements
This study was funded by a grant from Associate Professor Anthony Proietto, Gynaecological Oncologist, Hunter New England Area Health Service. Appreciation is also extended to Karen Jovanovic, Chief Radiation Therapist, and Radiation Oncology Staff and patients at the Calvary Mater Newcastle.




