Introduction
Within radiotherapy, there have been many improvements in technology over the past 20 years with rapid changes from 3-dimensional (3D) conformal radiotherapy (3D-CRT) to intensity modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT). It has been noted in the National Radiotherapy Advisory Group (NRAG) report that 80% of patients with head and neck cancer would benefit from IMRT treatment in comparison to 3D-CRT.Reference Williams1 Currently, radical radiotherapy treatments utilise IMRT or VMAT techniques due to the high levels of coverage and conformity to target volumes, while sparing healthy surrounding tissues as much as possible, as well as being more efficient with increased survival rates.Reference Hunted, Clark and Zyuzikov2,Reference Osborn3
In education, it has been difficult to implement the training of IMRT/VMAT for radiotherapy students due to time constraints as well as the financial implications of running a fully clinical system along with payment of additional user licenses. Feedback has been received over several years from students that treatment planning sessions felt outdated in comparison to the practices students see when on clinical placements. Moreover, by combining sessions of VMAT and IMRT with the previous teaching, which demonstrates how different beam arrangements, energies, weightings, multi-leaf collimator and wedges will change a plan, and how these basic principles are necessary for a Therapy Radiographer’s understanding of how plans are created and why certain aspects have been changed for each patient.
Gamification
Gamification or serious play is the application of game attributes in a non-gaming contextReference van Gaalen, Brouwer and Schönrock-Adema4,Reference Christopoulos and Mystakidis5 or as described by Gentry et al.,Reference Gentry, Gauthier and L’Estrade Ehrstrom6 ‘the application of the characteristics and benefits of games to real-world processes or problems’. With aspects of problem-solving mixed with digital platforms, this has been shown to improve engagement and motivation as well as increased perceived autonomy when used in education.Reference Gentry, Gauthier and L’Estrade Ehrstrom6 Studies have shown highly positive satisfaction rates.Reference van Gaalen, Brouwer and Schönrock-Adema4
The focus of this study is each student optimising their own performance of VMAT planning, which can later be compared to others.Reference Flinton, Khine and Mannion7 Game-based learning, gamification or serious play are active learning styles that align with both local and national guidance.8,9 The aim of gamification is to make learning more interesting and/or inspiring with game-related mechanisms, gamification’s capacity to empower learners to navigate complex systems through gaming processes can provide students with unique learning possibilities.Reference Awan, Dey and Salts10 It has been shown that learning-related functional changes within the brain happen best when someone is actively engaged; one way to improve engagement in the classroom can be done by making teaching ‘fun’. Fun can be defined in three ways: achievement, discovery and bonding; to maximise enjoyment in gamification, it is required to appeal to each of these three sources of fun.Reference Awan, Dey and Salts10–Reference Rudolphi-Solero, Jimenez-Zayas and Lorenzo-Alvarez12 A review by Krishnamurhty et al.Reference Krishnamurthy, Selvaraj and Gupta13 found that participants should be motivated by gamification; motivation simply means that an individual is driven to achieve their goal. Motivation can be divided into both intrinsic and extrinsic; extrinsic motivation refers to doing something because it leads to a specific tangible result, while intrinsic motivation refers to doing something because it is pleasant or captivating.Reference Cerasoli, Nicklin and Ford14,Reference Wu, Li and Zheng15 There is no clear conclusion in the research as to whether gamification has a greater effect on intrinsically driven or extrinsically motivated learners. The use of computer software in treatment planning, along with the ability to add clinical goals which can be used as a scoring system, lends treatment planning sessions to benefit from the use of gamification, the added motivation of a ‘goal’ for the extrinsic motivation, but also the intrinsic motivation of the enjoyment of manipulating plans and problem-solving to achieve their end goal of a clinically deliverable treatment plan; something they may need to do once fully qualified.
Volumetric modulated arc therapy
Instead of teaching VMAT in a similar manner to 3D-CRT techniques, which build on basic principles and how to manipulate the plan and the complex software over the course of weekly sessions, when looking at how to maximise outcomes in limited teaching time; gamification could give students the ability to ‘play’ within the software and see how they can manipulate the plan, without being given excessive guidance, linking to more of an active learning style. VMAT treatment planning can be semi-automated with the use of planning templates, which can automate the creation of VMAT planning structures, adding objectives into the optimiser and even estimating the doses to organs at risk (OAR) the system can achieve and a lot of the process within the treatment planning system (TPS) is hidden from the user. VMAT prostate planning can be quite simple when a well-developed template is used in clinical practice, although students would be unlikely to learn within the software if they were given a patient with a template for the optimisation structures as there may be little to no necessary interaction with the optimiser, especially with the introduction of RapidPlan.Reference Gysen, O’Toole and Le16
The VMAT planning process varies significantly from the process of 3D-CRT planning, with 3D-CRT planning being a much more manual process. When compared to Bloom’s taxonomy, a framework that allows educators to organise learning activities based on a hierarchy of cognitive skills.Reference Adams17 Most current radiotherapy treatment planning teaching sits within the lower to mid-range, where with an active learning approach, such as gamification, this would focus on the upper terms of ‘analyse, evaluate, create’. This links to the theory of constructivism as stated by Bada et al.,Reference Bada and Olusegun18 ‘An important restriction of education is that teachers cannot simply transmit knowledge to students, but students need to actively construct knowledge in their own minds.’ By allowing the students’ time to interact with objectives for different structures, it may allow for greater understanding of the complexities of VMAT planning. Within the optimiser, there is often a trade-off between gaining the best coverage of the tumour/treatment volume and minimising dose to OARs; this can be seen when the students interact with each structure through the clinical goals section (Figure 1).
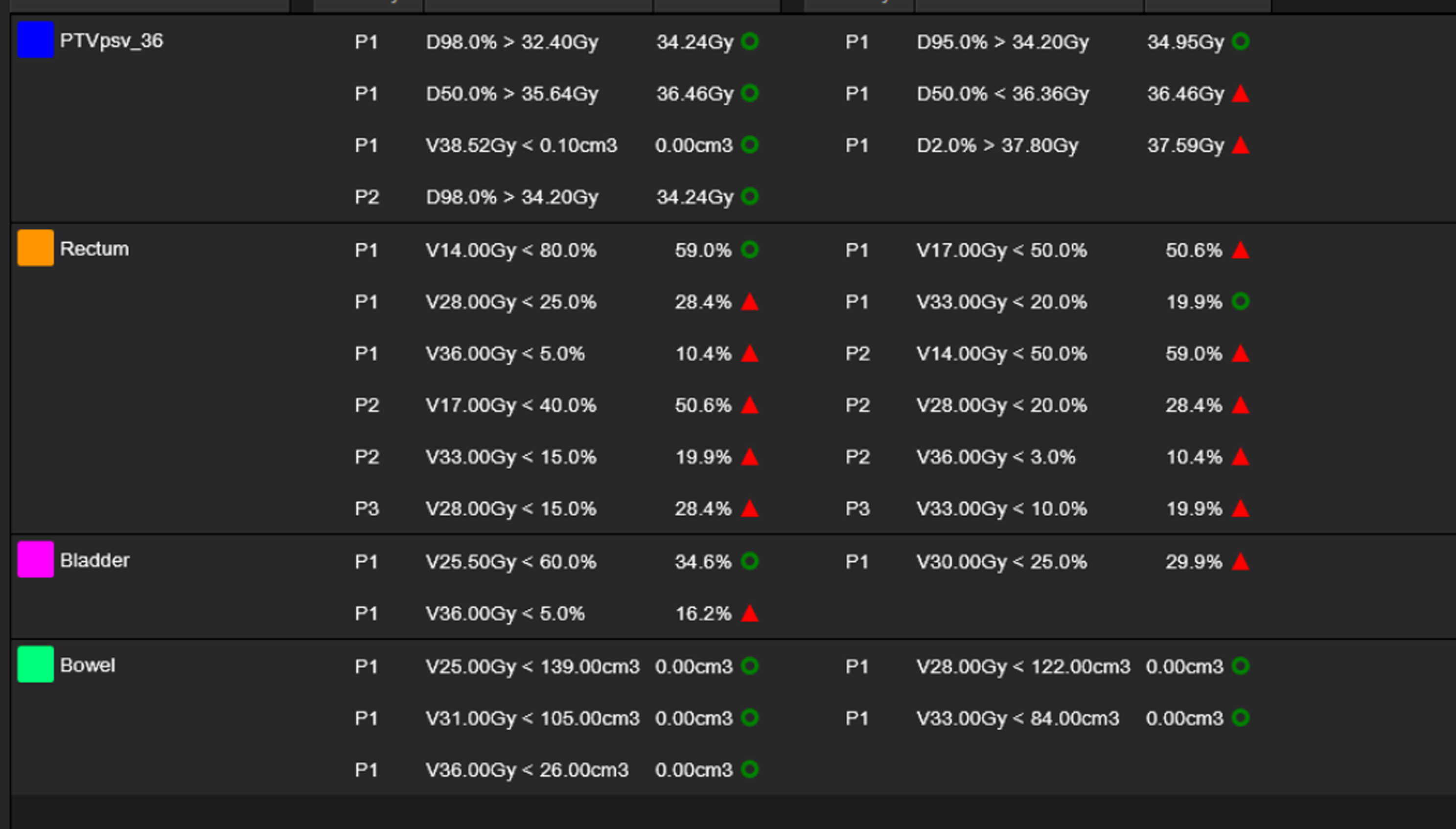
Figure 1. Showing ‘Clinical Goals’ for the given plan within Varian’s Eclipse. The constraints with a green circle show ‘passed’ constraints, whereas the red triangles signify ‘failed’ constraints. PTVpsv_36 was the PTV selected for this patient, which included both the prostate and seminal vesicles. P1, P2, P3 refer to the priority of constraints within the planning protocol; P1 is mandatory constraints, P2 is optimal/recommended and P3 is desirable.
Due to the nature of radiotherapy treatment planning, mixing elements of physics, photon interactions and biology as well as a complex computer system (Eclipse TPS V.18, Varian, Palo Alto, CA), it has been noted in module feedback that students can struggle to get to grips with the sessions, as there is a lot to process in quite a limited timeframe. The addition of VMAT adds another layer of complexity, although in many ways, it can be more instinctive as a visual tool; within the optimiser the user works with what is, in essence, an interactive dose volume histogram (DVH) where objectives can be placed along the curves of the graph for each OAR, planning target volume (PTV) or other optimisation structures, to achieve a higher or lower dose at those points.
The aim of this study is to evaluate the use of gamification to teach therapeutic radiography students how to create VMAT plans:
To investigate student perceptions of how gamification influences their understanding of VMAT planning.
To explore students’ engagement and enjoyment of using gamification as a learning tool.
To assess students’ views on the potential for applying gamification to different settings.
Methodology
Ethical approval was given at the University of Liverpool, approval number: 14,008, approved on 03 July 2024. Patient data were anonymised and in conjunction with a data-sharing agreement between both organisations. VMAT training was introduced for 2nd year undergraduate and postgraduate pre-registration radiotherapy students. At this stage of the course, the students have had circa 34 h of taught experience using Eclipse (Varian, Palo Alto, CA) TPS, creating conformal, fixed-field plans in water phantoms, breast, prostate and lung patients, this ensures that students have a strong understanding of treatment planning principles. For this study, participation was on a voluntary basis. About 15 students attended the session. A short presentation was delivered to explain VMAT, how to create a VMAT plan within Eclipse, how this varies from 3D-CRT treatment planning, a background to the Eclipse Optimiser and how each additional VMAT planning structure is made.
The students were asked to create a VMAT radiotherapy plan and given the scenario of the patient they were to plan, the goal of achieving the highest ‘score’ by meeting as many dose constraints as possible and achieving the highest score when compared to their peers by problem-solving as they go. The plan to be created was for a palliative patient having treatment for prostate cancer treated receiving 36Gy/6#/6weeks, this patient was chosen as palliative patients tend to have increased clinical target volume (CTV) to PTV margins than radical patients, therefore create more overlapping of PTV and OARs (Figure 2). This leads to the plan being challenging to create due to the increased overlap and proximity to surrounding OARs. In clinical practice, the plan for this patient had to be dose de-escalated to 30Gy/6#s/6weeks to meet mandatory dose constraints. The level of complexity of this case allowed a wider spread of marks for students to ensure there was a difference across the leaderboard. Dose constraints were input into Eclipse V18 using ‘clinical goals’ (Figure 1), which allowed students to see which constraints were met as they interacted with the optimiser, although there was no leaderboard until it was compiled manually at the end of the session. The constraints used are clinical dose constraints for optimal tumour coverage and minimising dose to OARs.
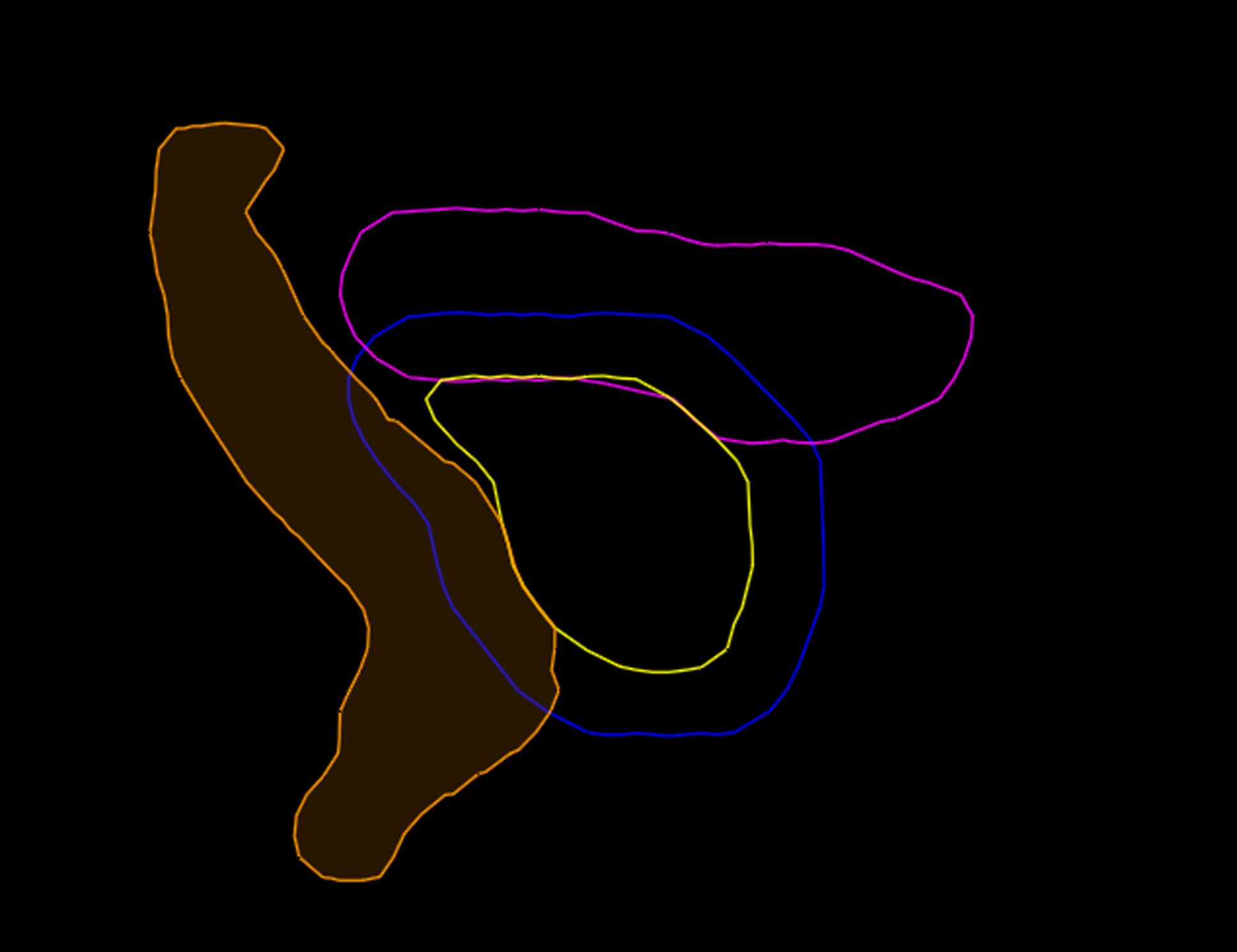
Figure 2. Sagittal view of contours showing large level of overlap of the PTV (Blue) and OARS (Rectum-Orange, Bladder-Pink) along with the CTV (Yellow).
When competitive aspects are introduced into teaching, it is vital to minimise stress levels, allowing students to continue to learn, as high levels of stress, which could be detrimental to their learning.Reference Krishnamurthy, Selvaraj and Gupta13 A positive, relaxed learning environment encourages learning, with the aim of creating a space which was welcoming and can minimise stress as much as possible.Reference Virtanen and Tynjälä19 There can be negative implications of using leaderboards in a learning environment, as shown by Flinton et al.Reference Flinton, Khine and Mannion7 which suggested using a top 5, rather than giving a ‘name and shame’ feeling for students who have not performed well in the task. Completed plans were marked using the clinical goal template. Each passed constraint was given 1 mark with a maximum score of 34. A leaderboard was compiled, and only the top 5 results were shown to the whole class to negate the negative impact of poor results on the leaderboard,Reference Flinton, Khine and Mannion7 although students could share their scores with peers if they wished.
As a debrief, students were told that this was a patient who clinically needed their overall dose to be de-escalated as mandatory dose constraints could not be met. Students were asked to think of what made this plan difficult to achieve mandatory constraints, which were mainly due to the larger CTV-PTV margin. By explaining that this plan could not be achieved in clinical practice gave the students more confidence, rather than feeling like they ‘failed’.
Students were asked to complete a pre- and post-e-questionnaire to evaluate the session, using Microsoft Forms, the pre-questionnaire was used to evaluate their baseline perceived knowledge and understanding, with the post-questionnaire assessing enjoyment and perceived gained knowledge. Both questionnaires utilised Likert scales for quantitative data, as well as a free-text box for qualitative data. Likert scales were utilised as they are a commonly used tool in education-based research; they are easy for participants to complete and give a way of quantifying qualitative data. Although converting ordinal data into numbers can cause issues with assessing results, such as mean and standard deviation, there is not an even spread of results.Reference Sullivan and Artino20 Respondents were asked to use a ‘memorable phrase/word’ to allow their questionnaires to be anonymous but also allow for individual comparison between each student’s pre- and post-results. Thematic analysis was carried out on the free-text area of both pre- and post-questionnaires to ascertain themes that came up throughout and to summarise qualitative findings.
Unfortunately, during the session, students were only able to spend ∼10 min optimising their time as the system would only allow 2–4 students to optimise at any given time, despite having 20 licenses for this piece of software. This has been raised to the manufacturer. This meant students had much less time to adjust aspects of their plan and to experiment with different solutions than was originally planned.
Results
In the pre-questionnaire, students (P1–15) were asked what they would like to gain from the session; answers included:
P1—‘Better understanding of VMAT plans and the tools used in the treatment planning process’,
P2—‘Feeling more at ease with VMAT’,
P14—‘To understand how VMAT plans are created and the different components used. Also to see how a real-life situation requires problem solving to create the best plan possible for a patient to maximise tumour control and minimise normal tissue complications’,
And:
P15—‘Better understanding of the type of plan we will see more commonly in practice’.
This showed that the students were keen to take on this additional session and that there was a desire to have a greater understanding of VMAT, as it is what they see mostly when they are on clinical placement.
Understanding
About 60% of participants rated their understanding of VMAT planning processes as ‘poor’ in the pre-questionnaire, with 86·7% answering no or unsure if they knew what specific VMAT planning structures were. While in the post-questionnaire, all respondents said they agreed or strongly agreed to having a greater understanding of VMAT planning (Figure 3) and 96·7% stating they knew what the specific VMAT planning structures were, with only one student answering ‘unsure’ to knowing what a cold/optimisation structure was.
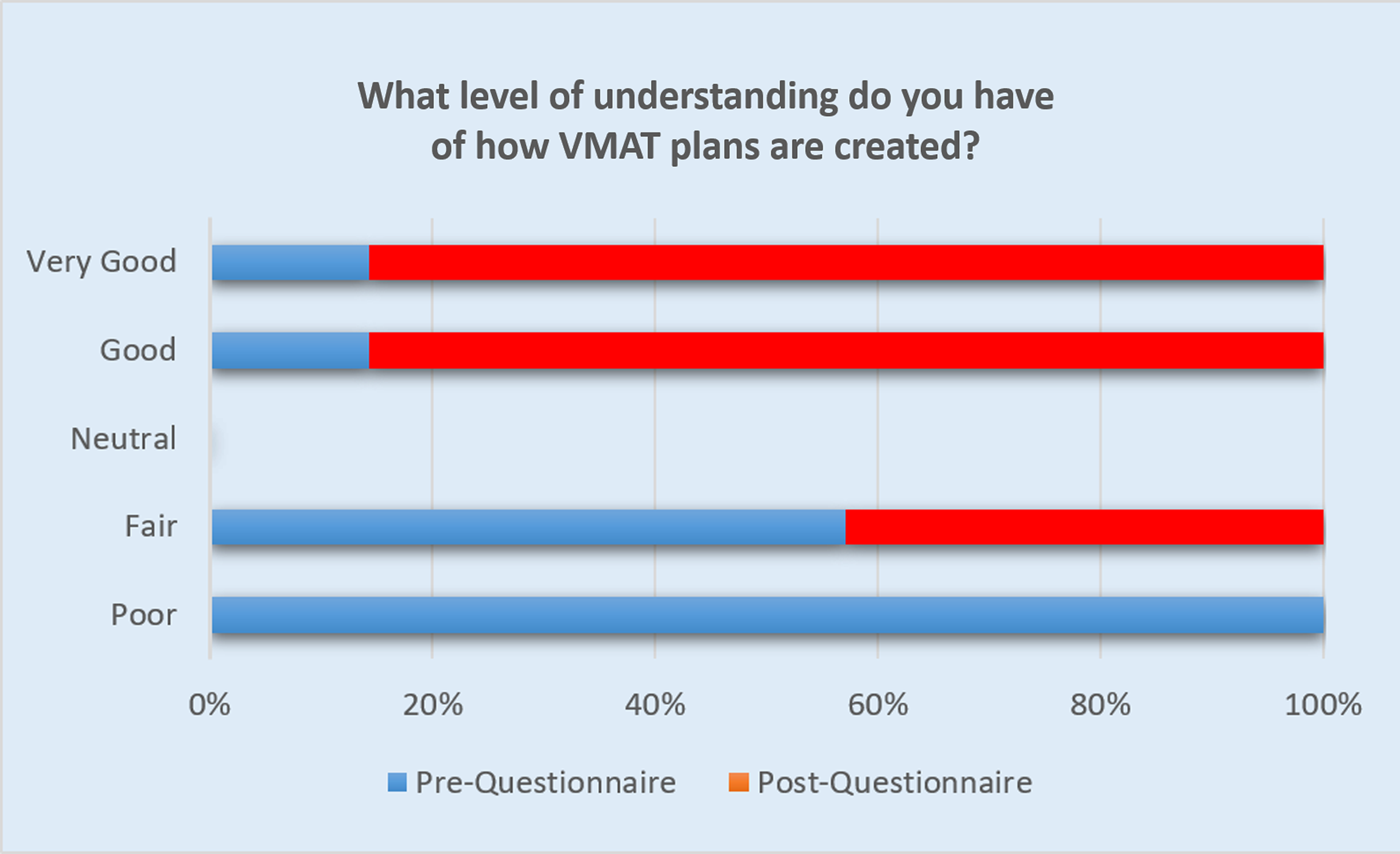
Figure 3. Stacked bar chart showing understanding self-assessment from both pre- and post-questionnaires.
Enjoyment
About 80% of students said they enjoyed the session, with the other 20% responding ‘neutral’. 66·6% enjoyed the use of gamification, with the other 33·3% replying ‘neutral’ to this question. 93·3% of students said the session was beneficial, and 93·3% would recommend the use of similar sessions to be integrated into the therapeutic radiography degree programme (Figure 4).
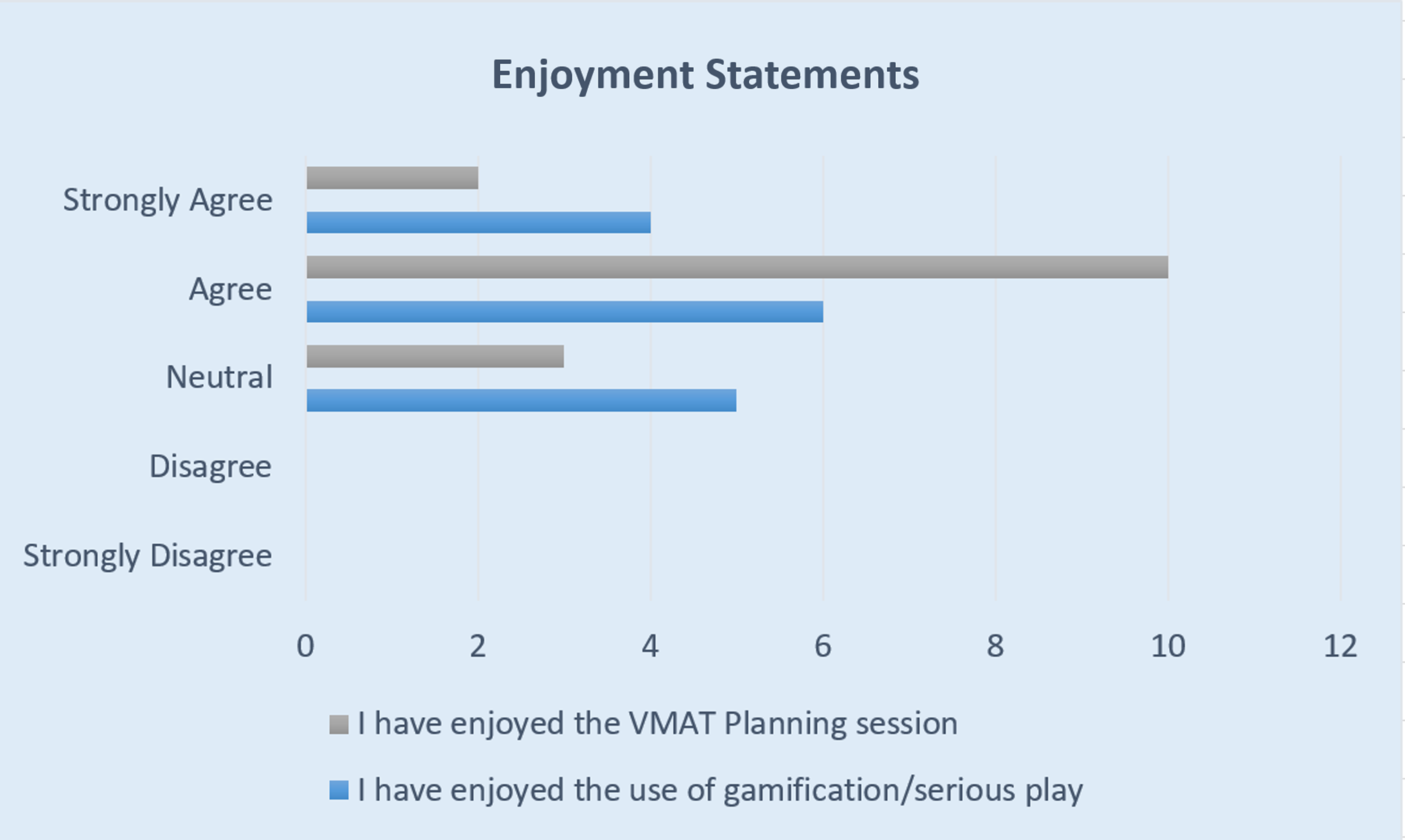
Figure 4. Bar chart showing results from 2 enjoyment statement questions from post-questionnaire.
In the ‘any other comments?’ section of the post-questionnaire, students (P1–15) wrote:
P13—‘This was a very useful session to see how VMAT plans are made, as these are the most common technique on set. It was interesting to see how the planning software generates the plan and all the constraints that have to be fulfilled… it would benefit future students to give an understanding of how VMAT plans are made’.
P11—‘Thank you for taking the time to run the session, it has been beneficial to see some basic VMAT planning principles in the palliative prostate setting’.
P10—‘I think the session would have been better if everyone was working at the same time but I understand the issues that occurred were unforeseeable and no ones fault. I think had everything gone to plan the session would have been very beneficial’.
P14—‘I really enjoyed being able to play around and use the optimisation tool to see if the clinical goals could be achieved. Using gamification is a great, interactive way of learning that would help students gain a better understanding of how this technique is used in a clinical setting’.
And:
P15—‘This is really beneficial as it is similar to the computer plans that we will see whilst on placement. It is so interesting to be able to see they have been generated. It also gives us the chance to try planning for ourselves which may help to broaden our career prospects’.
When answers were thematically analysed, the main themes were enjoyment and understanding, although these are very similar to the Likert scale questions, this may have guided these responses, as the free-text box was for any feedback. If this was repeated, more specific questions would be added for free-text options.
Prior experience in clinical placement
Participants were asked if they had seen VMAT planning in clinical placement, this was compared to their questionnaire results mainly their understanding of how VMAT plans are created; out of the five students who had seen VMAT planning in clinical placement, one student rated their understanding as very good, two rated their understanding as fair and two rated their understanding as poor. This shows that some standardisation on clinical placement would be beneficial to ensure all students have a fair chance of learning.
Discussion
Throughout the feedback, it was evident that participants had a positive experience and were engaged with and enjoyed the session, as per findings from other studies, such as van Gaalen,Reference Flinton, Khine and Mannion7 despite the technical issues. Although having 20 VMAT licences, the current servers could not cope with the demand of 15 people using the optimiser at the same time. Since the session took place the linac models, beam data and algorithms have been updated, which should allow for a larger cohort to use the system at one time. The updates have also allowed the graphics processing unit (GPU) function to be activated within the optimiser, GPUs are specialised processors designed to perform calculations quickly and efficiently, particularly for tasks involving parallel processing, like dose calculations in the radiation therapy function to operate within the optimiser.Reference Spalding, Walsh and Aland21 There is also the option of improving the software’s performance by increasing the number of servers, which could include cloud-based servers. There may be the possibility of running the session in smaller groups, which would minimise the chance of issues with the software. This would also allow for a more in-depth analysis of the plans, but if the capacity was limited, the session would need to be repeated as many times depending on cohort size to ensure all students were given a chance, which is not practical or possible in the current timetable. However, if the users optimising at one time could be increased to 20, then it would be an ideal size of class. A time limit could be set, but this would minimise the time students will get to interact with the optimiser and could take away from the gamification aspect. It could also be run as part of a breakout session from another workshop, although this would also require another lecturer to participate.
As the patient who was used in the study was unable to have an acceptable plan created, there was a chance that students could become disillusioned that they were wasting their time creating a plan as an unachievable goal. Although this was used as a learning tool, and multiple patients were tested, it was difficult to get a spread of results from other patients. This was primarily due to the centre where data was obtained from use small margins which minimises the overlap of PTV and OARs, along with utilising a drinking protocol.Reference Burns, Rosbottom and Mitchell22 This also shows the students a real-world example of what happens in practice when dose de-escalation is required as this patient was then treated with 30Gy/6#/6weeks instead of 36Gy/6#/6weeks.
Across the cohort, there were three males and 12 females, previous studies into gamificationReference Flinton, Khine and Mannion7 have found a correlation between gender and enjoyment/positive feedback from the implementation of gamification, although no correlation was found. The age range was 19–58 years, although 14/15 participants were between 19 and 30 years old, with a mean age of 24·7 years and a standard deviation of 9·3 years. Similar studies have had a greater range of ages and have compared the outcomes/evaluations based on age, but with a small spread of ranges, this will not be useful in this case.
Despite the positive feedback from students, it has been stated in publications that the enjoyment and usefulness of gamification decline with use, and initial feedback might be positive because of the novelty of the use of gamification.Reference Kovisto and Hamari23 Although this is not an overused pedagogic approach throughout therapeutic radiography training, therefore this should not be a concern.
Although students were asked within the pre-questionnaire if they had seen VMAT planning in clinical placement, there was a positive correlation between seeing the planning process for creating a VMAT plan in clinical placement and perceived understanding. Within the questionnaire, the question ‘Have you been shown VMAT planning in the treatment planning department in your clinical placement sites?’ was only a yes/no; so, there is no metric of how much planning experience these students were given within their clinical blocks as this could vary significantly, in the future a free-text box for greater detail would be beneficial, it could also lead to follow-up studies relating to fair learning opportunities in practice placements across multiple placement sites. Moreover, the correlation between having previous experience from clinical placement and their final mark from the task would have been a useful metric but was not able to be analysed due to the anonymisation of questionnaires.
The use of a dynamic leaderboard would have been a constructive addition to the gamification aspect as the students could compare how their current plan is fairing against the rest of the cohort, fuelling engagement, although this was not possible to create in the timeframe and to create this would require further discussions with the manufacturers to add such a function to the software.
The cohort for this study volunteered to participate which could mean the students who were present were keen to engage and learn about VMAT, therefore there may be more resistance from the overall year group, although over half of both postgraduate and undergraduate year two students volunteered and several more stated they would like to be part of the session but could not attend on that day. Therefore, a positive attitude and desire to learn more about VMAT were shown by a large proportion of the year-groups. As radiotherapy is a relatively small course of ∼40 students, staff tend to have a good rapport with students; therefore, it must be considered that although the questionnaires were anonymous, students may have been kind with their responses. This teaching would fit well within the curriculum and is a true representation of planning practices. The ideal time to fit this into the curriculum is in the second year of both Therapeutic Radiography programmes, as students will have had several sessions of 3D-CRT planning, therefore understanding the basic principles of beam placement and manipulation.
Conclusion
Overall, the results were positive, despite technical difficulties throughout the session. Student perceived understanding improved throughout, a large proportion of the students enjoyed the session, and the use of gamification and engagement was better in the room than in other treatment planning sessions, which highlights the positive impact of the use of gamification. The sessions will be repeated, after technical issues have been rectified, allowing feedback to be analysed based on a longer session, giving participants more time to interact with their treatment plans and the planning software. Although based on the current feedback from the student participants, gamification appears to be a valid tool for VMAT radiotherapy treatment planning sessions but should not be overused as its usefulness can wear off. Further work will compare gamification versus more traditional treatment planning sessions. Once completed, it could also be useful to create a follow-up questionnaire to gain feedback from the student participants on whether they found learning about VMAT in this matter beneficial in the rest of their studies. Gamification will be further utilised across cohorts for radiotherapy treatment planning sessions.
Competing interests
The authors declare none.






