Introduction
Conformal radiotherapy for the treatment of prostate cancer allows for the delivery of higher doses of radiation to the prostate gland with little or no increase in normal tissue toxicity.Reference Dearnaley, Khoo, Norman, Meyer, Nahum, Tait, Yarnold and Horwich1, Reference Michalski, Winter and Prudy2 The risks of conformal radiation therapy include the potential for a geographic miss with the associated potential decrease in tumour control and increase in complications.Reference Langen and Jones3–Reference Mackie, Kapatoes and Ruchala5 To reduce the risk of a geographic miss, it is important to immobilize the patient and to minimize pelvic movement. A good immobilization device must maintain the patient's body in a reproducible position while restricting mobility during the treatment session. It should be comfortable for the patient, simple to implement in the simulation process and must not interfere with the delivery of radiation.Reference Saw, Yakoob, Enke, Lau and Ayyangar6 Some centres prefer to primarily immobilize just the legs with a leg cushion device, while others prefer more rigid immobilization of the pelvis, hips and legs.Reference Langen and Jones3
Although there have been many studies evaluating and comparing different immobilization devices,Reference Bayley, Catton and Haycocks7–Reference Song, Washington, Vaida, Hamilton, Spelbring, Wyman, Harrison and Chen12 it is still unclear what device should be used in terms of immobilization and in terms of patient comfort and set-up time. Our institution acquired a Combifix® (Sinmed, Reeuwijk, The Netherlands) treatment immobilization device. It allows positioning of the patient's feet and knees in a reproducible location thereby fixing the pelvic bones. Feet and knees can be immobilized separately for each patient and once locked the device can be used for potentially fast and reproducible set-up. The objective of this study was to assess potential differences between the Combifix® and the conventional double-leg immobilization system through the use of patient and therapist outcomes including ease of set-up, satisfaction, comfort, overall treatment time and an assessment of systematic and random set-up errors related to pelvic bone immobilization.
Materials and Methods
Trial design and patient population
This trial utilized a two-arm crossover design in which patients served as their own controls. Patients were randomized to start with either the Combifix® or leg cushion immobilization device prior to beginning treatment (Figures 1 and 2). Computer-generated block randomization was used and patients were assigned unique identifiers to ensure patient confidentiality. Patients with high-risk prostate cancer (any of the following: prostate-specific antigen ≥20 or Gleason score ≥8 or T3 or T4 lesions) who were being treated with a pelvic phase plus a prostate boost phase were considered eligible. Patients with a hip prosthesis, prostatectomy or previous radiotherapy to the pelvis were excluded. Patients were asked to sign an informed consent document approved by the local university ethics review board.

Figure 1. Combifix® immobilization device. Reproduced with kind permission from CIVCO Medical Solutions.

Figure 2. Double-leg immobilization device.
Endpoints
Primary endpoints for this study included patient comfort and ease of set-up. Secondary endpoints included total treatment time, therapist ease of set-up and mean systematic/random set-up deviations from the isocentre as measured by electronic portal imaging (EPID). No fiducial markers or other prostate localization technologies (such as transabdominal ultrasound) were used in conjunction with our study. The effect of prostate movement was not analyzed as part of this investigation.
Simulation and tumour volumes
Patients underwent computer tomography (CT) simulation using both immobilisation devices on the same day. An urethrogram was used during simulation to delineate the bladder with the bladder comfortably full. The normal tissue volume was contoured according to RTOG p0126 guidelines and included bladder, rectum, femora (to the level of the ischial tuberosity), penile bulb and skin.
Fiducial markers were not used in this study because our endpoints assessed pelvic immobilisation based on bony set-up, not prostate motion.
RTOG 9910 guidelines were used for determination of target volumes for both phases. For the boost phase, the primary tumour target volume was defined as the prostate gland and any clinically or radiologically evident extraprostatic tumour extensions (e.g., seminal vesicle invasion). The boost planning target volume (PTV) conformed to the gross tumour volume (GTV) plus a 1.0 cm margin to account for subclinical extraprostatic tumour extension and variations in treatment set-up and internal organ motion. For the pelvic phase, the regional lymphatic target volume included the external and internal iliac lymph node–bearing areas and was defined with CT-based planning. Multileaf collimator (MLC) shielding was used to block portions of the small intestine and rectum. The boost phase preceded the pelvic phase in this protocol in order to complete all data collection within the first 5 weeks of radiation treatment.
Planning and radiation treatment
Planning was performed on the Theraplan Plus 3.8 (Nucleotron, Kanata, ON, Canada) system and each phase was planned using the CT data set with the appropriate immobilization device. Three-dimensional planning was used. Shielding was through the use of a Varian MLC and plan optimisation was based on dose volume histograms. The field borders were designed to include the PTV within the 95% isodose line. dose–volume histogram (DVH) criteria for an acceptable plan were based on the dose constraints as outlined in the RTOG p0126 protocol.
All patients were treated daily, 5 days per week on an 18 MV Varian 2100 linear accelerator with onboard amorphous silicone portal imager in two phases for a total dose of 73 Gy in 35 fractions to the boost PTV prescribed at the isocentre. The isocentre was routinely placed at or near the centre of the prostate. The pelvis was treated to a dose of 44 Gy in 22 fractions and the prostate and seminal vesicles were then boosted to a total dose of 73 Gy in 35 fractions.
External skin marks corresponding to a common X, Y, Z laser coordinate system were used for daily set-up and verification was by EPID.
Data collection
Weekly questionnaires were filled out individually by each patient as well as by the radiation therapists (group consensus) to assess patient comfort and ease of set-up (Appendix A and B). Patient questionnaires assessed patient comfort, ability to maintain position and ease of getting into and out of the immobilization devices using a 10-point Likert scale adapted from Bayley et al.Reference Bayley, Catton and Haycocks7 Therapist questionnaires assessed various patient positioning issues, patient mobility, and patient comfort also on a 10-point Likert scale. Total treatment unit time was determined from the time the patient entered the room until the time they exited the room. Actual beam on and off time was also recorded.
EPID was used to determine displacement of the treated isocentre to the planned isocentre using external patient skin marks and bony landmarks. Anterior and lateral field imaging by EPID was used for field placement verification on the first day of each phase and twice per week for the first 2 weeks of each phase. Any isocentre deviations of >0.5 cm were corrected by the medical radiation therapist before treatment. Bony landmarks on these EPIDs were compared with simulator films by one investigator (T.S.) in order to measure positioning errors for both devices. Bony landmarks used to determine EPID isocentre shifts included the anterior symphysis pubis and posterior sacrum for anterior/posterior shifts, bilateral pelvic brim for lateral shifts, and the L5-S1 interspace and lower ischial tuberosity for superior/inferior shifts. All shifts were recorded prior to any corrections being made.
Statistical analysis
Sample size was calculated to be 16 patients based on a power of 0.90 and an alpha level of 0.05. This calculation was based on a clinically significant difference of 1.5 points on the Likert scales for self-reported patient comfort scale. Assuming a 10% non-compliance rate with the questionnaires increased our sample size to 18.
Weekly questionnaires from both patients and therapists were analyzed using repeated measures analysis of variance (ANOVA) to compare the two immobilization devices. Two-sided paired Student's t-tests were used to compare treatment time. In order to assess the systematic and random error associated with the two devices, descriptive statistics, the 95% confidence intervals and the mean and standard deviation of both the systematic and random error were calculated for the shifts applied in the anterior–posterior (AP) direction, right–left (RL) direction and superior–inferior (SI) directions. Descriptive statistics for the overall isocentre vector deviation using the formula √AP2 + RL2 + SI2 was also calculated. Repeated measures ANOVA analysis was used to compare devices for the EPID analysis. With a sample size of 18 patients, statistically significant immobilization differences of ∼1mm can be detected at an alpha level of 0.05.
Results
Patient characteristics
Eighteen patients were enrolled in this study between December 2004 and December 2005. There was no loss to follow-up. Baseline patient and tumour characteristics are listed in Table 1. All patients were high-risk and treated with external-beam radiation therapy to a dose of 73 Gy in 35 fractions.
Table 1. Baseline patient and tumour characteristics
cc = cubic centimetres; T = tumour.
Patient and therapist outcomes
There was no statistically significant difference between the Combifix® and the leg cushion in terms of patient comfort (p = 0.596), ability to hold still (p = 0.284) or patient ease-of-use (p = 0.475) (Figure 3). There was no statistical difference between the two devices for the overall composite patient outcome measure (p = 0.640). If we examine data for individual patients, we find that 12 (67%) had no preference for either device, 3 (17%) preferred the Combifix® and 3 (17%) preferred the leg cushion. Data was collected from 32 medical radiation therapists. An average of six different therapists per patient contributed to the questionnaires. Overall, the therapists preferred the leg cushion device in terms of ease-of-use (p = 0.04) and believed that the leg cushion was slightly more comfortable for the patient; however, this did not reach statistical significance (p = 0.083, Figure 4).

Figure 3. Mean (±SD) for patient outcomes on patient reported 10-point Likert scale. Comparison of the leg cushion and Combifix immobilization devices in terms of patient comfort using weekly questionnaires and a 10-point Likert scale.

Figure 4. Mean (±SD) for therapists questionnaire on a 10-point Likert scale. Comparison of the leg cushion and Combifix immobilization devices in terms of therapists ease of set-up and patient comfort using weekly questionnaires and a 10-point Likert scale.
Treatment time
There was no statistically significant difference in the average total treatment time when using the Combifix® device compared to the leg cushion device (18.9 min vs. 18.4 min).
EPID isocentre deviations
Descriptive statistics for systematic (Table 2) and random (Table 3) errors were determined for both immobilisation devices with statistically significant differences found in the superior/inferior shifts (random error only), absolute value of superior/inferior shift (systematic and random errors) and overall vector (systematic error only). All other immobilisation device differences in systematic and random errors were not statistically significant. The overall mean difference in isocentre vector displacement between immobilisation devices was in the order of 1.0 mm with a small advantage related to use of the double-leg immobilisation system (mean systematic error Combifix® 3.9 mm versus double leg 2.9 mm, p = 0.03). No overall mean difference in vector random error was seen between the immobilization devices (p = 0.92).
Table 2. EPID systematic error
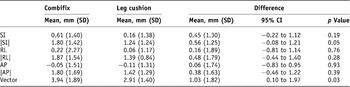
AP = anterior–posterior; RL = right–left (lateral); SI = superior–inferior.
Note: Table showing the systematic error measurements for all deviations from the isocentre as measured by EPID for the Leg cushion and Combifix. Measurements include mean, standard deviation (SD), the 95% Confidence Intervals (CI) and the p value.
Table 3. EPID systematic error

AP = anterior–posterior; RL = right–left (lateral); SI = superior–inferior.
Note: Table showing the random error measurements for all deviations from the isocentre as measured by electronic portal imaging (EPID) for the Leg cushion and Combifix. Measurements include mean, standard deviation (SD), the 95% Confidence Intervals (CIs) and the p value.
Discussion
Daily reproducible patient set-up is a necessary pre-requisite for successful implementation of three-dimensional conformal external-beam radiation therapy. Good immobilisation during treatment allows for optimisation of treatment portals by minimising necessary set-up margins. This in turn allows for target dose escalation and potentially better treatment outcomes both in terms of tumour control and reduction in normal tissue toxicity. The ideal immobilisation device should be comfortable, reproducible, easy to use, and should achieve adequate immobilisation without interfering with radiation delivery.Reference Pollack, Zagars, Smith, Lee, von Eschenbach, Antolak, Starkschall and Rosen13 There have been numerous studies comparing immobilization devices and immobilization techniques for prostate cancer patients. Prospective and retrospective trials have compared different devices such as the leg cushion, alpha cradle, Aquaplast® cast and HipFix®, as well as prone versus supine positioning.Reference Catton, Lebar, Warde, Hao, Catton, Gospodarowicz, McLean and Milosevic8–Reference Malone, Szanto, Perry, Gerig, Manion, Dahrouge and Crook10, Reference Baumert, Zagralioglu, Davis, Reiner, Luetolf and Ciernik14–Reference Pouliot, Bani-Hashemi and Chen15 However, no clear evidence of a preferred immobilisation device has yet been presented in the medical literature.
There have been very few randomised trials looking at the issue of external immobilisation in prostate cancer radiation. Kneebone et al. reported on a randomized trial looking at set-up accuracy with no immobilisation versus rigid immobilisation in the prone position.Reference Kneebone, Gebski, Hogendoorn and Turner16 Weekly port films were used to look at bony deviations from the isocentre in both groups. Thirty percent of the control films showed deviations >10 mm compared to 10% of the films in the experimental arm. They concluded that rigid immobilisation resulted in significantly less deviation with the same comfort and treatment times compared to no immobilization. In 2004, Bayley et al. utilised a randomised crossover design to compare set-up accuracy, prostate movement and patient comfort for supine versus prone positioning.Reference Bayley, Catton and Haycocks7 A Vac-Loc® device was used for the supine position and the HipFix® for the prone position. Prostate motion was assessed using fiducial markers and isocentre positioning errors were assessed with EPID. Supine position was found to be superior in terms of patient comfort, decreased dose to critical organs, decreased prostate motion, and fewer pre-treatment corrections. Two different immobilisation devices were used in the setting of two different patient positions; therefore, it is unclear whether observed differences were strictly due to treatment position or may have also been influenced by the choice of device.
Our trial was designed as a randomized crossover trial. We chose a crossover design because it is ideal for analysing new techniques in small single-institution studies. Because patients serve as their own controls smaller patient numbers can be used to answer clinically relevant questions in a relatively short time frame. We wished to assess patient comfort, ease of set-up and accuracy of set-up for two different immobilisation devices, the double-leg cushion and the Combifix®. Our standard immobilisation device is a foam cushion designed to hold the lower legs horizontal with the knees locked. It can be moved easily in all directions, making daily set-up quick and simple. The Combifix® was designed to immobilise both the knees and ankles with the legs flexed. In order to accommodate different body shapes, the knee cushion portion of the Combifix® device has three different heights and the ankle holder can be moved superiorly, inferiorly, and at different angles. Individualising patient set-up in this manner should theoretically provide superior immobilisation; however, set-up procedures may be more complex. When we analysed the questionnaires from our study, the therapists preferred the double-leg cushion to the Combifix® and specifically cited the challenges of daily set-up as the main reason for their preference between devices.
From the patient's point of view, there was no significant difference between the two in terms of comfort or ease-of-use scores. If we look at individual patient data, two-thirds of patients had no preference for either device and of the remaining one-third, half preferred the Combifix® and half the leg cushion. Those with lower back problems tended to prefer the Combifix® because the flexed leg position was easier on the back. The downside appeared to be the fact that the Combifix® was harder to get into becuause it was physically bolted to the table and alignment of the lasers was more challenging and time consuming. Although set-up with the Combifix® appeared to take slightly longer (18.9 min versus 18.4 min), there was no statistical difference in total treatment unit time.
When EPID was used to determine isocentre deviations, there was greater vector mean systematic error with the Combifix® as compared to the leg cushion (p = 0.03). Because the legs are flexed, the Combifix® causes the pelvis to tilt slightly inferiorly, which may explain this systematic error. Furthermore, if we assess deviations in the superior/inferior direction, we noted that there was greater systematic (p = 0.05) and random error (p = 0.03) with the Combifix® as compared to the leg cushion. The leg cushion maintains the legs in a horizontal position; therefore, error in the superior/inferior direction should be minimised. With the Combifix®, the legs are flexed and the height of the cushions as well as the tilt of the ankles can be adjusted, potentially leading to slight changes in body position and more random error. Furthermore, the therapists noted that when patients were using the Combifix® they had to be reminded not to push against the ankle support, which can raise the pelvis and create additional random error in the superior/inferior direction.
Conclusions
This research project confirmed the feasibility of mounting a small single-institution randomized crossover technology assessment related to a practical radiotherapy issue. No clinically important advantage was seen with the Combifix® device versus our standard double-leg cushion in terms of patient preference, patient comfort and bony pelvic immobilization. The therapists, however, did prefer the standard device for ease-of-use. In addition, this work can serve as a baseline for future immobilisation studies assessing both patient/therapist outcomes as well as quantitative set-up error. In fact, the statistical data (mean, standard deviations, and clinically important differences) presented in this study can be used in future randomised clinical trials for sample size calculations.
Acknowledgements
We acknowledge Mr. Larry Stitt for his statistical expertise. In addition, we thank Dr. Andrew Bayley for the use of the patient and therapist immobilisation questionnaires.
Appendix A: Patient questionnaire*
On the scale below please circle the number that best corresponds to your feelings over the last week
How comfortable was the treatment position during the last week? 1 2 3 4 5 6 7 8 9 10 very uncomfortable very comfortable
How easy was it to stay still during your treatment during the last week? 1 2 3 4 5 6 7 8 9 10 very hard very easy
How easy was it to get into your (Leg cushion/Combifix) device last week? 1 2 3 4 5 6 7 8 9 10 very hard very easy
*Adapted with permission from Bayley, 2004.
Appendix B: Therapist questionnaire*
On the scale below please circle the number that best corresponds to your feelings over the last week
Was the patient difficult to position? 1 2 3 4 5 6 7 8 9 10 very hard very easy
Did the patient have the mobility to position himself? YESNO
Did the patient find the treatment comfortable? 1 2 3 4 5 6 7 8 9 10 very uncomfortable very comfortable
Did the patient line up in their immobilization device? YESNO
*Adapted with permission from Bayley, 2004.








