INTRODUCTION
Individuals with acquired brain injuries (ABI) often experience a range of neuropsychological and emotional difficulties. Common neuropsychological symptoms experienced by patients with ABI include impaired executive function and cognitive deficits in memory, attention and concentration (Ponsford et al., 1995), and problem solving and planning (Dritschel et al., 1998; Williams et al., 1998). Depression in the general population has been found to affect cognition, with depressed (noninjured) patients experiencing reduced concentration, slowed thinking, and memory difficulties (DSM-IV); for example depression is associated with less efficient recall of autobiographical memory (see Williams, 1996, for a review). Lifetime prevalence rates for depression in the United States have ranged from 15 to 17% (Kessler et al., 2003).
Despite the research within the general population, there are few studies on the impact of depression on individuals with ABI. Indeed, much of the literature relating to depression in ABI has addressed measurement of such disorders rather than the relationships between depression and cognitive function. Many individuals with ABI experience adjustment problems after the acute phases of injury (Ponsford et al., 1995). Within the United Kingdom, hospitalized patients receive 24-hour care and support, but on discharge from hospital, service provision becomes fragmented, leaving individuals with few support mechanisms at a time when the full impact of their “disability” is becoming apparent. This state of affairs is likely to contribute to low mood and anhedonia, common symptoms of depression. Various research projects have been reported which provide evidence of high rates of depression in the TBI population. Overall, it is estimated that the rate is somewhere between 20 and 40% in the first year after injury (Fleminger et al., 2003), with rates increasing to as high as 50% after the first year (Fleminger et al., 2003). This finding provides an indicator that the rates of depression among the ABI population as a whole are much higher than that in the general population (approximately 15–17%; Kessler et al., 2003).
One factor that may contribute to the development and maintenance of depression in individuals with ABI is rumination, which is the tendency to dwell upon negative events, thoughts, and symptoms such as tiredness and lack of motivation (Nolen-Hoeksema, 1991, 2000). Rumination has been found to exacerbate depressed mood and to predict the onset of future episodes of depression (Nolen-Hoeksema, 2000). Furthermore, in patients with depression, rumination has been found to have a detrimental effect on cognitive abilities that are often impaired following ABI, such as memory and executive function (Watkins & Brown, 2002; Watkins & Teasdale, 2001, 2004). Individuals with ABI often spend long periods ruminating over what they have lost in their lives since their brain injury (Garske & Thomas, 1992). This increased tendency to ruminate may be a potential factor in the development and maintenance of depression within this population.
One particular consequence of rumination in patients with depression is to increase overgeneral autobiographical memory recall (Watkins & Teasdale, 2001, 2004). Overgeneral autobiographical recall occurs when individuals produce categoric summaries of repeated events rather than provide a specific episode when asked to recall specific personal memories that occurred at a particular place and time (e.g., to the cue word “sports” responding with “making mistakes” or “watching my team on television every week” rather than “last Saturday I took my kids to their first rugby match, they were so excited by all the singing, and joined in”). Overgeneral autobiographical memory is a marker of impaired cognitive functioning, which is implicated in the development of psychopathology and impaired problem solving. First, overgeneral memory is associated with poor problem-solving (Dritschel et al., 1998; Evans et al., 1992; Goddard et al., 1996, 1997; Pollock & Williams, 2001; Williams et al., 1998, 2005). Second, overgeneral memory predicts poorer long-term outcome for depression and posttraumatic stress disorder (Brittlebank et al., 1993; Dalgleish et al., 2001; Harvey et al., 1998; Mackinger et al., 2000; Peeters et al., 2002).
Williams et al. (1998) identified that depressed individuals with traumatic brain injury (TBI) showed an increased tendency to show overgeneral autobiographical recall. They also showed that autobiographical memory specificity was predicted by working memory capacity. Overgeneral autobiographical memory in ABI groups may, therefore, be due to either neurological impairments and/or as a consequence of rumination (Dritschel et al., 1998; Williams et al., 1998). Williams et al. (1998) noted that those who tended to rate their trauma event as particularly uncontrollable, and due to the actions of others, were more at risk of mood disorder. It was hypothesized that rumination over the cause of the injury may, in part, compromise their capacity for recall of autobiographical memories. The combination of neuropsychologically based impairments and rumination-based deficits could potentially result in severe autobiographical memory impairment within the ABI population. Therefore, the primary aim of the current study was to examine whether an experimental manipulation of rumination (a rumination induction vs. distraction) influenced the extent of overgeneral autobiographical memory among individuals with ABI.
The second aim of the study was to examine the role of neuropsychological impairments in overgeneral autobiographical memory. By assessing the effects of experimentally manipulating rumination across varying degrees of impairment (those with mild vs. severe cognitive impairments), the study explored how neuropsychological impairment and state rumination each contributed to overgeneral memory recall, and whether they acted independently or interacted in their effects.
We hypothesized that overall, in individuals with ABI, relative to a distraction manipulation, a rumination manipulation would significantly increase overgeneral memory recall. We also explored whether there would be a significant variation on overgeneral memory depending on the severity of ABI, rated on the basis of cognitive performance. We expected that reduction of specificity would be most pronounced, and, possibly, only evident, in those with mild cognitive impairments. This expectation was because those with more severe impairments would be likely to have a generally compromised capacity for memory functioning. Finally, we hypothesized that higher levels of depression and/or rumination preintervention would be associated with less specificity in recall at baseline, or greater response to the rumination manipulation.
METHODS
Participants
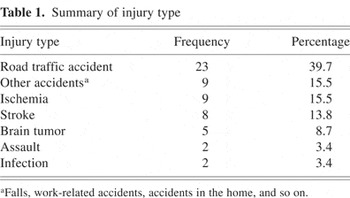
A total of 61 individuals (45 men, 16 women), with mild to severe brain impairments were recruited through the brain injury charity, and support service provider, Headway. All participants had suffered a neurological event severe enough to require hospitalization. Three participants failed to complete both phases of the study. The analysis of the data was based on the remaining 58 participants (42 men, 16 women, 18 to 68 years of age, time in education 11 to 17 years, coma lengths from 0 hr to 7 months, time since injury from 3 months to 40 years). There was no exclusion on the basis of current depression and/or past reported mental health issue. The types of injuries varied considerably, with the most common cause being road traffic accidents (see Table 1). Of the participants, 28 were classified as having mild impairment and 30 as having moderate to severe impairment based on their performance on a neuropsychological assessment. Ethical approval for the study was obtained from the University of Exeter School of Psychology ethics committee. Participants were given an information sheet and were given a verbal explanation of the point of the research, their right to withdraw, and how the data would be used before signing the consent form.
Summary of injury type
Neuropsychological Assessment
Assessment consisted of a structured interview for premorbid, demographic, and injury details and administration of a brief neuropsychological battery. Neuropsychological measures included the Digit Span (forward and backward, Wechsler, 1997, 1999), for immediate recall (working memory assessment task); Trail Making Tests A & B (TMT A & B; Lezak, 1995), for sustained and divided attention (selective attention assessment task); Letter Fluency (FAS) Task (Benton et al., 1976), for executive functions such as initiation and self-monitoring; and Speed of Comprehension and Language Processing Test (SCOLP, Baddeley et al., 1992), for speed, comprehension, and premorbid general cognitive functioning.
Participants were allocated to one of two severity groups based upon their scaled scores on the four neuropsychological measures and coma length. This was because determining severity of injury on the basis of coma length alone was potentially unreliable due to the longevity of time since injury for the majority of participants (Lammi et al., 2005). Participants whose performance fell within the impaired range on more than half of the neuropsychological tests (based on standardized percentile scores for each test, Lezak, 1995) were assigned to the moderate-to-severe impairment group. Participants who scored below borderline on the standardized percentiles for each test were allocated to this impairment group. Those who scored above the impaired range (borderline and above on the standardized percentiles) on more than half of the tests were assigned to the mild impairment group. However, those performing at borderline level (or below) on at least two of the four tests were assigned to the Moderate–Severe group if the coma reported was longer than 6 hr (McMillan & Greenwood, 2003). Subtest data for each of the different neuropsychological tests were analyzed (for example, the Trail Making tests A and B) as well as overall scaled scores to understand the specific functional deficits of individual participants. However, no subtest scores were used to allocate participants to the impairment groups. This allocation was based purely on their overall scaled scores for each of four neuropsychological tests.
Symptom Measures
Symptoms of depression and anxiety were measured using the 21-item Beck Depression Inventory (BDI, Beck et al., 1961) and Beck Anxiety Inventory (BAI, Steer & Beck, 1997).
Rumination Measure
State rumination was assessed using a 25-item version of the Response Style Questionnaire (RSQ, Nolen-Hoeksema & Morrow, 1991), which combined two different 22-item versions of the RSQ. The RSQ measures an individual's natural tendency to ruminate and, therefore, acts as a baseline measure of rumination. A total score on the RSQ was averaged for 22 items to ensure that the scoring was consistent with previous versions. The range of scores fell between 22 and 88. Scores below 40 indicate low levels of rumination. An average score falls between 40 and 50, with scores of 50–60 indicating above normal levels of rumination. Scores above 60 fall within the clinical range. These ranges are based on means obtained by Roberts et al. (1998) from a population of college students.
Autobiographical Memory Test
In the Autobiographical Memory Test (AMT; Williams & Broadbent, 1986), participants are asked to retrieve a specific memory of an event that occurred at a particular place and time, for each of a series of cue words. Two parallel versions of the task, matched for emotionality, were used, each with six positive (e.g., happy), six neutral (e.g., library), and six negative words (e.g., sadness). Data were analyzed for all of the three levels of emotionality combined. Participants had 30 s to retrieve a memory. A memory was coded as specific if it referred to a particular event that lasted less than 24 hr. An overgeneral memory was coded for events that lasted longer than 24 hr and for events that summarized categories of events that had occurred more than once. An omission was coded if the participants failed to produce a memory at all within the 30-s time limit. If the memory recalled reflected a specific occasion that lasted over 24 hr, for example, a specific holiday or trip, the memory was categorized as an extended memory. The proportion of overgeneral memories was calculated by adding the total number of memories recalled (not including the omissions) and then dividing by the number of overgeneral memories given. The principal experimenter first rated the memories, and then an independent judge, unaware of participant groupings, rated all the memories across the whole sample. There was a high level of agreement across the two raters for judgments of categoric and specific memories (inter-rater reliability, k = .980, n = 232).
Rumination and Distraction Manipulations
In both rumination and distraction conditions, participants were asked to work through written lists, concentrating on and imagining each item, at their own pace, for 8 min using the materials developed by Nolen-Hoeksema and Morrow (1991). In the rumination condition, participants were asked to focus upon 28 items that referred to the self, feelings, or symptoms of depression, for example, “think about why you react the way you do,” “think about why things turn out the way they do,” “think about how optimistic or pessimistic you feel about the future.” In the distraction condition, participants were asked to focus upon a series of 28 items that were non–self-related, such as “think about and imagine a boat slowly crossing the Atlantic,” “think about the layout of a typical classroom,” “think about the shape of a black umbrella.” Participants were asked to read each example and contemplate the meaning of the sentence. The focus on self-related examples in the rumination condition was designed to focus participants' attention inwardly to cause them to ruminate. This task tends to lead to negative self-focus, but only in individuals who are already experiencing depressed mood (Nolen-Hoeksema & Morrow, 1991).
Procedure
Participants were first seen for the neuropsychological assessment and completed the BDI, BAI, and RSQ. The experimental phase was carried out at a second testing occasion between 2 and 5 weeks after the assessment (average 4 weeks). During the experimental phase, participants first completed the BDI and BAI, and then completed a baseline AMT. Participants were then randomly allocated to either the distraction or rumination conditions using a random number generator, before completing a second AMT.
RESULTS
Baseline Characteristics
Table 2 displays the baseline measures across group and condition. A series of 2 × 2 mixed design analyses of variance (ANOVAs) were calculated, with Group (levels of impairment: mild vs. moderate-to-severe) and Condition (rumination vs. distraction), as between-subjects factors, and with baseline measures of anxiety, depression, rumination, and neuropsychological functioning as dependent variables. These analyses revealed that there was no effect of Condition on baseline measures, all Fs < 1.5, such that participants in the rumination and distraction conditions were matched for levels of depression, anxiety, rumination, and neuropsychological functioning. There were also no significant differences in depression, anxiety, or rumination across levels of impairment at baseline, all Fs < 1.0 (Table 2). A total of 77.6% of participants were found to have some degree of depressive symptoms (a score of 10 or greater), whereas 58.6% displayed moderate depressive symptoms (scores greater than 17).
Mean differences across group and condition
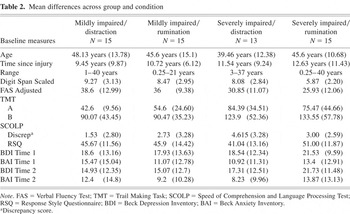
Consistent with the allocation of participants into mild versus moderate-to-severe impairment, the moderate-to-severe impairment group performed significantly worse on the four neuropsychological tests, Digit Span (F1,54 = 6.62; p < .02), TMT A (F1,54 = 14.73; p < .001), TMT B (F1,54 = 8.27; p < .01), FAS (F1,54 = 8.72; p < .01), and the SCOLP discrepancy scores (F1,54 = 4.52; p < .05) than the mild impairment group. There was a significant interaction of Group by Condition for performance on Digit Span, (F1,54 = 4.18; p < .05), which reflected the people in the moderate-to-severe impairment group who ruminated doing significantly worse than the other three cells. No other interactions were significant.
Effect of Rumination on Overgeneral Memory
A 2 × 2 × 2 mixed design ANOVA was calculated, with Time as a within-subjects factor (baseline vs. postmanipulation) and with Group (level of impairment: mild vs. moderate-to-severe) and Condition (rumination vs. distraction) as between-subjects factors. The dependent variable was the proportion of overgeneral memories produced (number of overgeneral memories divided by the total number of memories recalled). Table 3 shows the differences in the proportion of overgeneral memories on the AMT both baseline and postmanipulation. There was a significant main effect of time (F1,54 = 8.65; p < .01; η2 = .14), reflecting a greater proportion of overgeneral memories postmanipulation than baseline. There was also a significant main effect of condition (F1,54 = 4.27; p < .05; η2 = .073), reflecting a greater proportion of overgeneral memories recalled in the rumination condition compared with the distraction condition.
Proportion of overgeneral memories pre- and postmanipulation
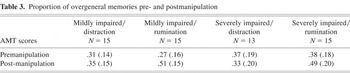
These main effects were secondary to a significant interaction of condition by time (F1,54 = 9.16; p < .005, η2 = .145). As indicated by Figure 1, this interaction reflected a significant increase in the proportion of overgeneral memories recalled from premanipulation (M = .33; SD = .18) to postmanipulation (M = .50, SD = .17) in the rumination condition (t(1,29) = −4.12; p < .001), but no significant change in the proportion of overgeneral memories recalled from premanipulation (M = .34; SD = .16) to postmanipulation (M = .34; SD = .18) in the distraction condition (t(1,27) = .000; p > .05). There were no other significant main effects or interactions: group (F1,54 = .93; p > .05), group by time (F1,54 = 2.62; p > .05), group by condition (F1,54 = .087; p > .05), or group by condition by time (F1,54 = .19; p > .05).
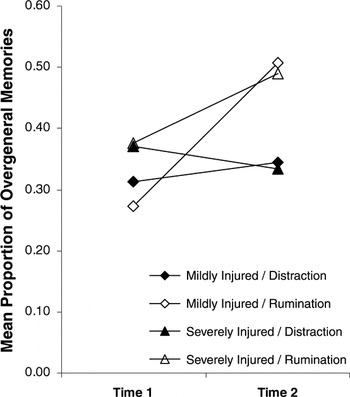
Mean proportion of overgeneral memories.
The proportion of overgeneral memories recalled at Time 1 were analyzed in a series of simple regressions against BDI scores at Time 1 and state rumination scores across the whole data set and within the rumination conditions. There were significant relationships between the proportion of overgeneral memories at Time 1 and both BDI scores at Time 1 (r = .277; p < .05) and state rumination scores (r = .382; p < .005). Depression scores explain 7% of the variance in the proportion of overgeneral memories, whereas state rumination scores explain 15%. When analyzing the relationship between these variables within the rumination conditions, there was no significant relationship between proportion of overgeneral memories and BDI scores (r = .253; p > .05) or state rumination scores (r = .267; p > .05).
A further 2 × 2 × 2 mixed-design ANOVA was calculated, with Time as a within-subjects factor (premanipulation vs. postmanipulation) and with Group (level of impairment: mild vs. moderate-to-severe) and Condition (rumination vs. distraction) as between-subjects factors, and number of omissions as the dependent variable. There was a significant main effect of time (F1,54 = 5.49; p < .05; η2 = .92), with more omissions being made postmanipulation (M =3.40; SD = 3.42) than premanipulation (M = 2.76; SD = 3.17). There were no other significant main effects or interactions: group (F1,54 = .52; p > .05), condition (F1,54 = .23; p > .05), group by condition (F1,54 = .92; p > .05), group by time (F1,54 = 2.59; p > .05), condition by time (F1,54 = .39; p > .05), or group by condition by time (F1,54 = 2.56; p > .05). Figure 2 displays the number of omissions.
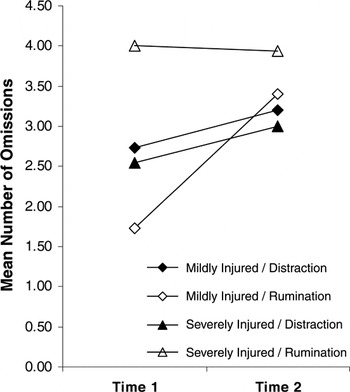
Mean number of omissions.
DISCUSSION
We hypothesized that, relative to a distraction condition, exposing individuals with ABI to rumination would significantly increase overgeneral memory recall. Consistent with this prediction, relative to distraction, rumination significantly increased the proportion of overgeneral memories recalled from premanipulation to postmanipulation in this sample of individuals with ABI. This effect was present for individuals with both mild and moderate-to-severe levels of ABI. The severity of ABI (in relation to cognitive performance) did not influence the effect on overgeneral memory recall of manipulating rumination: there was no interaction between degree of impairment and the experimental manipulation of rumination. Furthermore, we also hypothesized that higher levels of depression and/or state rumination would be associated with overgeneral memory recall in general, or lead to greater effects on recall in response to rumination manipulation. A regression analysis provided support for the hypothesis that depression and state rumination were associated with overgeneral memory. However, we did not find that experimental manipulation produced greater rumination in those with high depression or state rumination. Future research may attempt to account for the links between rumination, background mood, and immediate affect as triggered by intervention. Furthermore, the rumination manipulation was likely to only have induced an increase in overgeneral memory recall among those participants experiencing depression. Although not all participants were classified as depressed, the high overall rates of depressive symptoms (78%) may have resulted in a generalized effect across the data set. Future research to compare depressed and nondepressed ABI patients on these measures would be warranted.
These findings lend support to the hypothesis that rumination may impair aspects of memory in brain-injured patients and that this effect is not dependent upon the level of cognitive impairment. It is as yet unclear whether rumination affects memory directly or whether attention and/or executive functions may contribute to performance and may be affected.
The findings are consistent with previous research, which found that rumination could increase overgeneral memory in patients with depression. Importantly, these findings extend these observed effects of rumination on overgeneral memory into a new population—individuals with ABI. As such, these findings raise the possibility that rumination is a significant contributor to the elevated overgeneral memory observed in individuals with ABI. We note that participants were likely to make omissions, which accounted for some overgenerality, particularly in the mildly impaired rumination group. This group was most likely to shift from providing greatest specificity in recall in response to rumination manipulation. Therefore, it is very possible that autobiographical access is particularly disturbed in people with brain injury at the level of executive control of initiation, search, and monitoring (see Williams et al., 1998). Future research on executive and attentional contributors to autobiographical recall, in context of mood disorder, is warranted.
Furthermore, the general trend for an increase in omissions across the groups from Time 1 to Time 2 may suggest that fatigue may have contributed to decrements in performance. Given that overgeneral memory is associated with poor problem solving and a poorer prognosis for depression, the current findings are also consistent with the hypothesis that rumination may play a role in the development of functional impairments and depression in individuals with ABI. These findings thus suggest that interventions for planning and memory problems in individuals with ABI would benefit from the inclusion of strategies designed to reduce rumination.
Baseline measures indicated that the severe impairment rumination group performed significantly worse on the digit span test. This result indicated that baseline performance in this group on memory tasks such as the AMT was likely to be impaired. This conclusion is supported by the results (Table 3). This did not affect the overall findings. By assessing the differences in the proportion of overgeneral memories from Time 1 to Time 2, any differences in baseline performance were controlled for.
Although the rumination manipulation has been widely used in rumination research, we note that the stimuli used in the rumination condition may have differed from those in the distraction condition in terms of their level of abstraction and/or imageability. This could, in the context of brain-injured groups, contribute to biased response style. Future research may benefit from further analyses of relative resource demands of the stimuli for brain-injured groups.
Further limitations of this study relate to the measurement of mood disturbance and the assessment of functioning. The study identified higher rates of depressive symptoms (BDI, Beck et al., 1961, premanipulation, M = 19.17; SD = 12.04) than found by previous studies of individuals with ABI (Fleminger et al., 2003). These relatively high BDI scores raise the possibility that there was an elevated rate of clinical depression in this sample; however, there were no diagnostic interviews to determine diagnostic status. This study used the BDI and BAI to measure mood disturbance, as these measures are commonly used in rumination studies carried out with non–brain-injured populations. However, these scales may be less appropriate for use with the ABI population and may overestimate the extent of depression, as they tend to assess physical and motivational symptoms (Kreutzer et al., 2001) that are commonly associated with brain injury as well as depression. More accurate measurements may have been obtained by using scales such as the Hospital Anxiety and Depression Scales (HADS, Zigmond & Snaith, 1983), which, although still containing physical measures, relies less heavily on items that may be related to brain injury as opposed to mood disturbance.
The assignment of some participants to one of the two impairment groups based on coma length was problematic. Assessment of coma length across levels of injury found that there were no significant differences between those with mild and severe impairments. This finding indicates that coma length was not an accurate measure of impairment, although greater coma length is usually associated with increased dysfunction (McMillan & Greenwood, 2003). In this study, many of the participants were several years after injury, suggesting that improvements may have occurred over time that made the use of coma length invalid as an index of severity. Future studies will need to consider time postinjury when relying on coma length as an assessment criterion.
This study has indicated that manipulating rumination can influence autobiographical memory deficits found in ABI individuals. This finding suggests that, in addition to the neuropsychologically based deficits on memory functioning already faced by individuals with ABI, ruminative thinking could further exacerbate memory impairments in ABI. These findings, therefore, raise the possibility that deficits in autobiographical memory, and possibly other deficits in cognitive functioning found in ABI, could be a consequence of the thinking adopted in response to the ABI, as much as the direct effects of the injury, particularly as elevated rumination is a common response after ABI.
Current approaches to reducing neuropsychological impairments focus on neurorehabilitation methods, such as the use of memory techniques and aids. If cognitive processes, like rumination, do play a causal role in impaired functioning in ABI, then psychological interventions such as cognitive–behavioral therapy (CBT), which are designed to reduce such negative thinking, may further augment the impact of neurorehabilitation in reducing cognitive impairments. CBT is well structured and focuses on concrete behavioral problems and thought processes. CBT also lends itself to the inclusion of close friends or relatives to aid the patient with homework tasks and problem-solving techniques (Williams et al., 2003). By providing ABI patients with this form of therapy, it would be possible to teach them coping strategies and stress management (Ownsworth & Oei, 1998), as well as reduce their tendency to ruminate on their past lives (Ponsford et al., 1995). Further research needs to be conducted into the use of integrated, transdiagnostic treatment approaches for treating both neuropsychological- and cognitive-based memory deficits together.
ACKNOWLEDGMENTS
This research was facilitated by Headway (brain injury charity) in the United Kingdom. We note that Dr. Huw Williams is a (honorary) Trustee of Headway Devon, and Headway UK Medical Expert panel. There are no conflicts of interests, and we thank the clients and staff at the Headway centres in Devon, Somerset, and Dorset who participated in this study and allowed us to use their facilities.







