Introduction
The rat lungworm, Angiostrongylus cantonensis (Chen, Reference Chen1935) is a metastrongyloid nematode widely known for its zoonotic potential and unusually broad range of paratenic and accidental hosts. Besides humans and domestic animals as its well-described accidental hosts, the parasite has been reported as causing severe neurological disorders in wildlife. In all these accidental hosts, the parasite can lead to paralysis or death (Kuberski and Wallace, Reference Kuberski and Wallace1979; Lindo et al., Reference Lindo, Escoffery, Reid, Codrington, Cunningham-Myrie and Eberhard2004; Monks et al., Reference Monks, Carlisle, Carrigan, Rose, Spratt, Gallagher and Prociv2005; Burns et al., Reference Burns, Bicknese, Qvarnstrom, DeLeon-Carnes, Drew, Gardiner and Rideout2014, Cowie, Reference Cowie2017; Odani et al., Reference Odani, Sox, Coleman, Jha and Malik2021). In most cases, humans get infected with A. cantonensis by eating raw or undercooked intermediate or paratenic hosts that contain infectious L3 larvae (Wang et al., Reference Wang, Wu, Wei, Owen and Lun2012). Angiostrongylus cantonensis originated in Southeast Asia and adjacent regions (Chen, Reference Chen1935; Lv et al., Reference Lv, Guo, Nguyen, Sinuon, Sayasone, Lo, Zhou and Andrews2018), but is now well established in tropical and subtropical regions around the globe (Prociv and Carlisle, Reference Prociv and Carlisle2001; Caldeira et al., Reference Caldeira, Mendonça, Goveia, Lenzi, Graeff-Teixeira, Lima, Mota, Pecora, Medeiros and Carvalho2007; Stockdale Walden et al., Reference Stockdale Walden, Slapcinsky, Roff, Mendieta Calle, Diaz Goodwin, Stern, Corlett, Conway and McIntosh2017). In temperate regions, 6 species of the genus Angiostrongylus and 4 other species of closely related genera (Rodentocaulus spp., Stefanskostrongylus spp.) have been described (Cowie, Reference Cowie2019), and only one of them (A. dujardini) is known to harm animals other than its definitive hosts (Graille et al., Reference Graille, Ferté, Petit, Ollivet Courtois, Gauchot, Nougaillon, Vitaud, Wardzynski and Lemberger2015; Eleni et al., Reference Eleni, Di Cesare, Cavicchio, Tonnicchia, Meoli, di Regalbono, Paoletti, Pietrobelli and De Liberato2016). Angiostrongylus cantonensis cycles between definitive (several rat species mainly of the tribe Rattini) and intermediate (terrestrial and aquatic gastropods) hosts (Alicata, Reference Alicata1965, Yong and Eamsobhana, Reference Yong and Eamsobhana2013). In addition, various poikilotherm vertebrates as well as invertebrates serve as paratenic hosts (Wallace and Rosen, Reference Wallace and Rosen1967; Ash, Reference Ash1968; Radomyos et al., Reference Radomyos, Tungtrongchitr, Praewanich, Khewwatchan, Kantangkul, Junlananto and Ayudhya1994; Wang et al., Reference Wang, Lu, She, Wen, Mo, Li and Li2018; Chaisiri et al., Reference Chaisiri, Dusitsittipon, Panitvong, Ketboonlue, Nuamtanong, Thaenkham, Morand and Dekumyoy2019, Turck et al., Reference Turck, Fox and Cowie2022).
Factors contributing to the emergence of A. cantonensis and its expanding distribution include climate change, global transport and the resulting facilitated movement of hosts (rodents and gastropods) and, finally, changes in population dynamics of hosts and cultural habits in endemic areas (York et al., Reference York, Creecy, Lord and Caire2015; Cowie, Reference Cowie2017). Findings of new A. cantonensis foci in the last 2 decades show not only continuous extension of its distribution, but also an expansion into temperate regions of Europe and USA (Campbell and Little, Reference Campbell and Little1988; Foronda et al., Reference Foronda, López-González, Miquel, Torres, Segovia, Abreu-Acosta, Casanova, Valladares, Mas-Coma, Bargues and Feliu2010; Paredes-Esquivel et al., Reference Paredes-Esquivel, Sola, Delgado-Serra, Riera, Negre, Miranda and Jurado-Rivera2019; Walden et al., Reference Walden, Slapcinsky, Rosenberg and Wellehan2021; Delgado-Serra et al., Reference Delgado-Serra, Sola, Negre and Paredes-Esquivel2022; Galán-Puchades et al., Reference Galán-Puchades, Gómez-Samblás, Osuna, Sáez-Durán, Bueno-Marí and Fuentes2022). York et al. (Reference York, Butler and Lord2014) predicted an increase of suitable habitats for A. cantonensis within Europe.
There is an extensive range of metastrongyloid nematode species that thrive in the temperate realm. (Gonzáles et al., Reference Gonzáles, Carbonell, Urios and Rozhnov2007; Ferdushy et al., Reference Ferdushy, Kapel, Webster, Al-Sabi and Grønvold2009; Majoros et al., Reference Majoros, Fukár and Farkas2010; Traversa and Di Cesare, Reference Traversa and Di Cesare2014; Čabanová et al., Reference Čabanová, Miterpáková, Druga, Hurníková and Valentová2018; Morgan et al., Reference Morgan, Modry, Paredes-Esquivel, Foronda and Traversa2021). The ability of their larvae to survive or even continue development in gastropods during the winter months in temperate climate has been experimentally demonstrated in Troglostrongylus brevior (Gerichter, Reference Gerichter1948; Morelli et al., Reference Morelli, Traversa, Colombo, Raue, Strube, Pollmeier and Di Cesare2020) and Aelurostrongylus abstrusus (Morelli et al., Reference Morelli, Colombo, Diakou, Traversa, Grillini, Frangipane di Regalbono and Di Cesare2021). To our knowledge, there have been no studies of A. cantonensis survival in overwintering intermediate hosts. We hypothesized and experimentally tested that A. cantonensis larvae can survive low winter temperatures in gastropods, which may be one of the key factors enabling their future expansion deeper into temperate regions.
Materials and methods
The experimental strain of A. cantonensis was obtained in 2017 in Fatu Hiva, French Polynesia and is maintained in laboratory conditions circulating between Wistar rats and experimental gastropods (Subulina octona and Biomphalaria glabrata). The identity of the isolate was confirmed by the morphology of adult nematodes obtained from infected rats as well as by cox1 sequencing, with the haplotype identified as part of A. cantonensis clade 2 (Červená et al., Reference Červená, Modrý, Fecková, Hrazdilová, Foronda, Alonso, Lee, Walker, Neibuhr, Malik and Šlapeta2019).
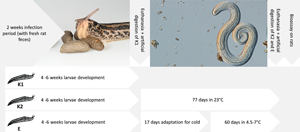
Adult great grey slugs (Limax maximus – LM) were collected from a private garden near Brno, Czech Republic during Autumn 2021. Slugs were kept in plastic boxes containing 8–10 individuals at 20–24°C throughout the experiment except for adaptation to cool temperature and the overwintering period of the experimental group. Boxes containing slugs were equipped with shelters and moss, and coconut soil was used as a bedding. Slugs were checked daily and fed with fresh lettuce and fish flakes every other day. One experimental group (E, 34 individuals) and 2 control groups (K1, 22 individuals and K2; 30 individuals) with a total of 86 LM individuals were infected by offering approximately 1 gram of fresh rat feces (maximum 12 hours old) to slugs in all experimental and control groups for 2 weeks (Fig. 1A). The number of larvae per gram of feces was determined by modified Baermann larvoscopy, such that approximately 40 000 L1 larvae per experimental box were provided during the 2-week period.

Figure 1. Hosts and developmental stages of A. cantonensis in described experiments. A. Slugs Limax maximus feeding on fresh rat feces; B. Angiostrongylus cantonensis L3 larva collected from artificially digested slugs, scale bar = 100 μm.
Experimental group E contained 34 slugs. After the exposure to rat feces containing L1 larvae, all slugs were left for 4 weeks to allow larvae to develop to the third stage. After that period, slugs in group E were gradually adapted to the decreasing temperature by exposing them to 15°C for two 5-day periods with a 7-day break between them at room temperature. After this adaptation period, slugs from group E were deprived of food for 3 days to empty the digestive tract and placed in a laboratory cool room with temperature between 4.5 and 7°C for 60 days. These conditions simulated the natural conditions in which these slugs overwinter, hidden in a shelter or deep underground, where the temperature rarely dip below 0°C (South, Reference South2012). During this period, the slugs were kept undisturbed and without food, except for weekly checks. All the slugs from group E exhibited typical signs of hibernation, i.e. clustered together with no apparent physical activity. After this period, all the slugs from groups E and K2 were weighed, sacrificed by decapitation and individually digested artificially (i.e. 0.3 g pepsin and 100 mL 0.7% HCl on a magnetic stirrer set to 200 RPM and 37°C) (Modrý et al., Reference Modrý, Fecková, Putnová, Manalo and Otranto2021). Motile L3 larvae were isolated, counted and used for the confirmatory bioassay on 2 infection-naive Wistar laboratory rats to assess their infectivity. Each rat was infected with 60 live motile L3 larvae via orogastric tube under general inhalation anaesthesia with diethyl ether. After 45 days post infection, Baermann larvoscopy of rat feces was performed to detect L1 larvae.
Slugs from group K1 (22) were used for confirmation of infection success. These slugs were sacrificed 4 weeks after the infection period, artificially digested as described and the number of larvae per slug was counted. Throughout the experiments, larvae were microscopically confirmed as A. cantonensis based on typical morphology, i.e. tail length, shape of the termination of the tail and oesophagus length (Ash, Reference Ash1970); possible presence of other metastrongylids was excluded using the same criteria (Diakou et al., Reference Diakou, Psalla, Migli, Di Cesare, Youlatos, Marcer and Traversa2016).
Slugs from group K2 (30) did not overwinter and remained at room temperature (20–24°C) throughout the experimental period, to check that A. cantonensis larvae survive in this slug species for this amount of time at room temperature. Slugs were checked daily and fed every other day as before the experiment. The remains of slugs from this group that died spontaneously less than 4 weeks before the end of the experiment were immediately examined for A. cantonensis larvae by artificial digestion. The slugs from K2 that died spontaneously more than 30 days before the end of experiment were excluded. Remaining slugs were sacrificed 4 weeks after the infection period, artificially digested as described above and the number of larvae per individual slug was counted.
Statistical analysis was done using ANOVA and the Tukey HSD test. The average, P value and standard deviation were calculated in R Studio and Microsoft Excel was used to generate a boxplot graph.
Results
All 34 slugs from the experimental (i.e. overwintering) group E survived the entire experiment. In the control group K1 (22 individuals), there were no mortalities either since the slugs were sacrificed just after the larval development to L3. Of 30 slugs in control group K2, 21 survived the entire experiment, 9 of them died during the last month of the experiment and were excluded from the experiment. Six more slugs from K2 group died spontaneously in the last month of the experiment and were processed as those that were sacrificed. The average weight of slugs at the end of the experiment in groups K1, K2 and E was 2.0, 2.2 and 2.3 g, respectively.
In the overwintering group (E), 0–17 motile third-stage metastrongyloid larvae (Fig. 1B) were collected from individual slugs (an average of 4.97 larvae per slug). In control groups K1 and K2, average numbers of larvae retrieved were 17.6 and 18.4, respectively, with a maximum of 61 larvae per slug in K1 and 63 larvae per slug in K2. Detailed information on the number of larvae in each slug are given in Table 1. The difference of L3 survival between the controls and overwintering group is significant (F2,74 = 20.05, P < 0.001) according to the Tukey HSD test and the difference between the 2 control groups is negligible (P = 0.95). Figure 2 is a boxplot graph of numbers of the third-stage larvae collected in each group.
Table 1. Numbers of live motile L3 of A. cantonensis retrieved from each individual slug Limax maximus from control groups K1 and K2 and in overwintering group E. The first six slugs from K2 group died spontaneously during the last month of the experiment.


Figure 2. Boxplot graph of numbers of third-stage larvae collected from each slug. The X marks the average value. The median is indicated by a line across the box. The whiskers on box plots show the ranges of Q1 and Q4 up to the most extreme data points. K1 and K2 are control groups, E is the experimental overwintering group of slugs.
Both Wistar laboratory rats that served as positive controls for the infectivity of larvae retrieved from the overwintering group E had L1 in their feces on day 45 post infection.
Discussion
Our study confirmed the ability of third-stage larvae of A. cantonensis to survive winter conditions in gastropods native to temperate Europe and remain infective for the definitive hosts. This result, together with the relatively long patent period in rats (Mackerras and Sandars, Reference Mackerras and Sandars1955), suggests that the range could further extend in Europe into areas with milder winters and sufficient abundance of definitive hosts.
Even though the collected larvae were infective for rats as definitive hosts, we observed a decrease in numbers of live motile larvae in slugs during the overwintering period (average 4.97 larvae per slug in group E compared to 18.19 in group K2). We chose L. maximus as a model species since it is a synanthropic slug with a lifespan of 2–3 years, naturally overwintering in shelters where the temperature almost never falls below 0°C (South, Reference South2012). The highest mortality observed in group K2, which was kept at room temperature, may be attributable to their maladaptation to captive conditions, since overwintering is natural for these slugs. LM has been described as an intermediate host suitable for other metastrongyloid nematodes (Conboy et al., Reference Conboy, Guselle and Schaper2017), although it usually carries relatively low numbers of L3 larvae (Ferdushy et al., Reference Ferdushy, Kapel, Webster, Al-Sabi and Grønvold2009). Other slug species in temperate Europe reported to host metastrongyloids also showed low abundance of larvae, barely reaching 100 larvae per individual (Lange et al., Reference Lange, Penagos-Tabares, Hirzmann, Failing, Schaper, Van Bourgonie, Backeljau, Hermosilla and Taubert2018). For comparison, the numbers of A. cantonensis L3 recovered from tropical slugs may reach hundreds to thousands (or even millions) of larvae, depending on the species (Heyneman and Lim, Reference Heyneman and Lim1967; Hollingsworth et al., Reference Hollingsworth, Howe and Jarvi2013; Kim et al., Reference Kim, Hayes, Yeung and Cowie2014; Rollins et al., Reference Rollins, Cowie, Echaluse and Medeiros2021). Environmental temperature has an impact on activity of L1 larvae and their ability to develop in intermediate hosts (Ishii, Reference Ishii1984; Lv et al., Reference Lv, Zhou, Zhang, Liu, Zhu, Yin, Steinmann, Wang and Jia2006). However, the massive load of A. cantonensis larvae in some tropical snails and slugs could also be related to differences in behaviour, food preferences and overall ecology of intermediate and definitive hosts.
Previous studies have shown that A. cantonensis larvae cannot develop to the third stage at less than 15°C (Ishii, Reference Ishii1984; Lv et al., Reference Lv, Zhou, Zhang, Liu, Zhu, Yin, Steinmann, Wang and Jia2006), which is very similar to the case of A. vasorum (Ferdushy et al., Reference Ferdushy, Kapel, Webster, Al-Sabi and Grønvold2010). However, our results confirmed that already developed L3 larvae survive and maintain their infectivity like the latter species, which is widely distributed in carnivores in temperate Europe (Fuehrer et al., Reference Fuehrer, Morelli, Unterköfler, Bajer, Bakran-Lebl, Dwużnik-Szarek, Farkas, Grandi, Heddergott, Jokelainen, Knific, Leschnik, Miterpáková, Modrý, Petersen, Skírnisson, Vergles Rataj, Schnyder and Strube2021; Tieri et al., Reference Tieri, Saletti, D'Angelo, Parisciani, Pelini, Cocco, Teodoro, Censo, D́Alterio, Latrofa, Otranto and Pascucci2021).
Our experiments indicate that once an infected mollusc as an intermediate host survives cold winter temperature, larvae of A. cantonensis most likely will stay infective within it for several months. This result, together with the relatively long patent period in rats (Mackerras and Sandars, Reference Mackerras and Sandars1955) suggests further possible range expansion to higher latitudes or altitudes in areas with sufficient abundance of the definitive hosts as the low winter temperatures are not necessarily an obstacle to the spread of the parasite (until reaching certain very high latitude or altitude points).
Data availability
All data generated and analysed during this study are included in this published article.
Acknowledgements
We thank Kateřina Kintrová for her help with the statistical analysis. We also thank the Veterinary University, Brno for providing the facilities for the experiment.
Authors’ contributions
Conceptualization was done by D.M. and L.A.; methodology by L.A. and D.M.; investigation was carried out by L.A, A.Š., E.I.R., V.V.; writing was by L.A, D.M.; visualization by L.A.; supervision by D.M. and project administration by D.M. All authors have read and agreed to the published version of the manuscript.
Financial support
The study was supported by SEAEUROPEJFS19IN-053 and Czech Science Foundation grant no. 22-26136S. Work of Lucia Anettova and Anna Šipkova was also supported by Specific research – support of student projects, n. MUNI/A/1488/2021. E. Izquierdo-Rodriguez was funded by the scholarship M-ULL (becas M-ULL, convocatoria 2019).
Competing interest
None.
Ethical standards
The authors declare that all ethical standards and requirements were fulfilled.