Introduction
The greatest challenge that health systems globally face in the 21st century concerns the gradual aging of the population, or rather the increasing burden of long-term conditions requiring ongoing management over a period of years or decades, and posing a great variety of health problems (Nolte and McKee, Reference Nolte, McKee, Nolte and McKee2008: 1). A strategic vision is needed, coupled with the ability to mobilize and deliver appropriate resources to patients with long-term conditions in the community, so that healthcare professionals can provide accessible, safe, well-coordinated, cost-effective, high-quality care (Clarke et al., Reference Clarke, Bourn, Skoufalos, Beck and Castillo2017). In particular, case management (CM) is a method designed to provide intensive, personally tailored care to meet the needs of patients with multiple chronic conditions who are at greatest risk of needing hospitalization and responsible for the highest costs (Hutt et al., Reference Hutt, Rosen and McCauley2004). This CM approach was defined by the Case Management Society of America as ‘a collaborative process of assessment, planning, facilitation, care coordination, evaluation, and advocacy for options and services to meet an individualʼs and familyʼs comprehensive health needs through communication and available resources to promote quality, cost-effective outcomes’ (Case Management Society of America, 2007). However, there are multiple components and variations of CM depending on the context and client population, in fact there are complex interdependent and dependent factors influencing what CM interventions are done, when, with whom, and in what context (Lukersmith et al., Reference Lukersmith, Millington and Salvador-Carulla2016).
Numerous systematic reviews and meta-analyses addressing the efficacy/effectiveness of CM have been published in recent years, often with discordant conclusions as regards both health outcomes and healthcare resource consumption (Hallberg and Kristensson, Reference Hallberg and Kristensson2004). For example, Stokes et al. (Reference Stokes, Panagioti, Alam, Checkland, Cheraghi-Sohi and Bower2015) found insignificant differences in total costs, mortality, and service usage when they examined community-based CM for adults with longstanding clinical conditions and ‘at risk’ of hospitalization. In contrast, Hickam et al. (Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013) reported that CM programs can help frail elderly people to avoid or contain functional loss, improve quality of life (QOL), and remain independent, and that CM programs also have the potential to forestall hospitalizations, emergency department (ED) visits, and skilled nursing facility use. Such incongruent evidence on the impact of CM may be a serious issue from the point of view of policy-makers and health system planners. The aim of the present study was to conduct a review of reviews of existing systematic reviews and meta-analyses on CM to pool and examine the abundance of research available on CM-related health outcomes and resource usage.
Methods
Review of reviews methods
Review of reviews systematically seek, organize, and assess existing evidence from multiple systematic reviews and/or meta-analyses on all the health outcomes associated with a given exposure.
We conducted a review of secondary studies (meta-analyses or systematic reviews, excluding reviews that were not systematic) on the efficacy/effectiveness of CM schemes for patients with longstanding conditions on multiple health outcomes and/or health service usage outcomes.
Literature search
PubMed, the Cochrane Database of Systematic Reviews (CDSR), and the Database of Abstracts of Reviews of Effects (DARE) were searched from 2000 up to the end of December 2017. The time window examined is much wider, however, since our search strategy identified reviews that included papers published in earlier years. The detailed search strategy used for PubMed, and also adapted for the CDSR and DARE, was as follows: (case managed[Title] OR case management[Title] OR case management,[Title] OR case manager[Title] OR case managers[Title] OR case managing[Title]) AND (review[ptyp] AND (‘2000/01/01’[PDAT] : ‘2017/12/31’[PDAT]). A manual search was also conducted in the reference lists of relevant articles and in the gray literature to identify additional papers. Studies were selected in two stages. First, the titles and abstracts of the studies identified were screened in full by two authors (AB and GG). Then, the full texts of the selected papers were retrieved and independently reviewed against the inclusion/exclusion criteria by the same two authors (AB and GG), who then discussed any papers on which they disagreed to arrive at a consensus of opinion.
Eligibility criteria and data extraction
Reviews were eligible for inclusion if they were written in English or Italian, were published between 2000 and 2017, and met the following criteria:
– Population: adults (18+) with long-term conditions;
– Intervention: CM. Only reviews in which CM had been analyzed separately from other organizational models were considered. Reviews addressing interventions for a specific disorder (e.g., CM for people with dementia) were excluded to avoid the overall analysis being excessively influenced by those long-term conditions with the highest incidence or most often studied;
– Comparison: usual care or other specific organizational models;
– Outcome: care processes, health measures, and healthcare resource usage.
Both quantitative and qualitative systematic reviews were considered. Finally, the selected studies were appraised in terms of their adherence to the PRISMA checklist (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009), which consists of 27 items, each scored as being ‘met’ or ‘not met’, or ‘not applicable’. The quality of the reviews was classified as high (for PRISMA scores of 80% or more), intermediate (from 60% to 79%), or low (less than 60%).
Data extraction
A data extraction form was prepared using Microsoft Excel. Descriptive data were extracted by one author (GG) and verified by the other (AB). The data collection included:
– general characteristics of the review: title, first author, journal, year, type (systematic review or meta-analysis; when a study was both a systematic review and a meta-analysis at the same time, it was tagged as a meta-analysis);
– methodological features: databases searched, number, type and data range of studies included, definition of CM, definition of comparison, objective, population, setting, and inclusion/exclusion criteria;
– results: review findings grouped by type of outcome as listed above:
○ process of care: adherence to treatment guidelines (i.e., the degree to which the prescribed therapy complied with the guidelines) and patient compliance;
○ health measures: clinical outcomes, depression and mental health symptoms, QOL, functional status, patient satisfaction, and survival;
○ resource usage: primary care usage, ED visits, hospital admissions, length of stay, and total costs of care.
– conclusions and recommendations for practice.
Summary of evidence
The following criteria were applied to summarize the evidence:
– a high consistency of the evidence was assumed if most of the secondary studies found CM effective or ineffective for a given outcome;
– a low consistency of the evidence was acknowledged if the number of the studies claiming that CM was effective on a given outcome was comparable with the number of studies indicating that this was not.
Results
Figure 1 shows the flow diagram with the number of studies included at each stage of the selection process. The database search generated 241 potentially relevant articles. After screening the titles/abstracts and checking the references and gray literature, 29 articles were selected for full-text analysis and assessed vis-à-vis the eligibility criteria (see Figure 1 for the reasons for exclusion). This led to 22 articles being included in the present study: 4 meta-analyses and 18 systematic reviews. The review quality assessment rated the 4 meta-analysis as high quality, while the 18 systematic reviews were rated as high quality in 6 cases, intermediate-quality in 5, and low quality in 7.

Figure 1. Flow diagram.
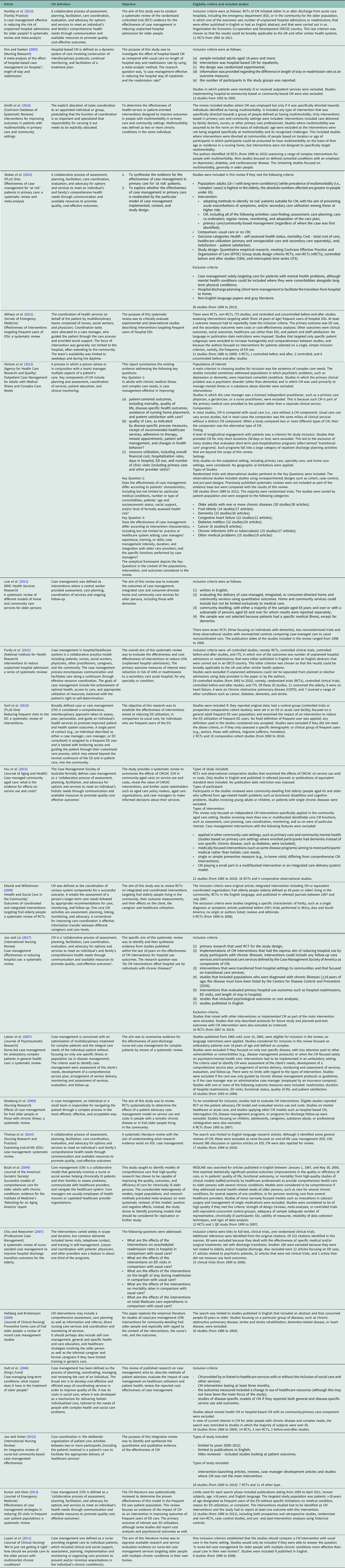
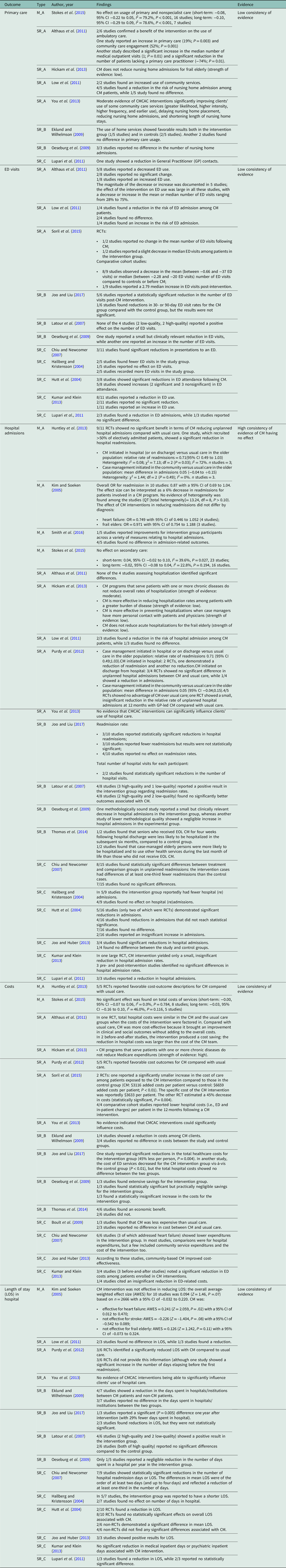
An overall description of the reviews considered is available in Table 1 (while the adherence of the studies to the PRISMA checklist is reported in the Appendix, Table I in Supplementary material).
Table 1. Included studies
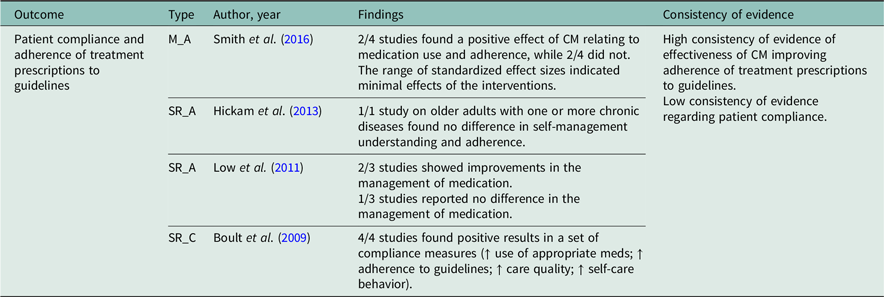
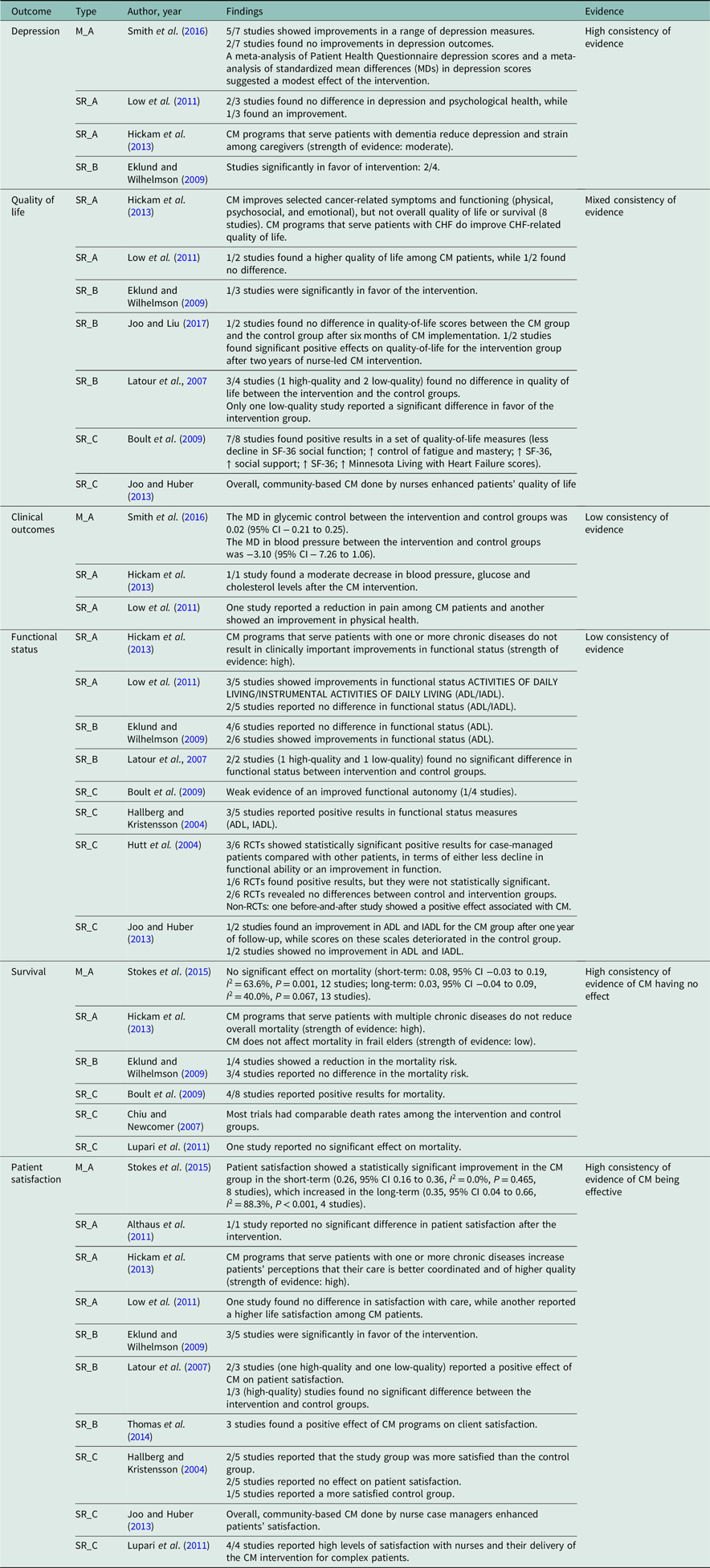
Tables 2, 3, and 4 summarize the main characteristics of all the available reviews and meta-analyses.
Table 2. Processes of care
M_A = high-quality meta-analyses; SR_A = high-quality systematic reviews; SR_B = intermediate-quality systematic reviews; SR_C = low-quality systematic reviews.
Table 3. Health measures
M_A = high-quality meta-analyses; SR_A = high-quality systematic reviews; SR_B = intermediate-quality systematic reviews; CHF = congestive heart failure; SR_C = low-quality systematic reviews; RCTs = randomized controlled trials.
Table 4. Resource usage
M_A = high-quality meta-analyses; SR_A = high-quality systematic reviews; CMCAC = case management in community-aged care; SR_B = intermediate-quality systematic reviews; SR_C = low-quality systematic reviews; ED = emergency department; RCTs = randomized controlled trials; EOL CM = end-of-life care management.
Concerning the process of care (Table 2), secondary sources assessing the adherence of prescriptions to treatment guidelines agreed that CM was more effective than usual care.
The findings were mixed as regards patient compliance, however, with comparable proportions of the reviews (two on each side) finding or failing to find benefits of CM on this parameter. Cochrane meta-analysis (Smith et al., Reference Smith, Wallace, O’Dowd and Fortin2016) assessed the effectiveness of interventions in patients with multimorbidity in primary care and community settings, including 18 generally well-designed randomized controlled trials (RCTs). Analyzing the only four organizational studies reporting measures relating to the use of medication and patient adherence, it was found higher proportions of patient adherence among participants involved in the intervention, which were in the range of 10% to 40% in absolute terms, but all studies had small effect sizes.
As for service responsiveness to patients’ expectations (Table 3), there was a strong concordance among the studies (7 out of 10) regarding the effectiveness of CM in improving patient satisfaction. In particular, Stokes et al. (Reference Stokes, Panagioti, Alam, Checkland, Cheraghi-Sohi and Bower2015) found a statistically significant beneficial effect on patient satisfaction in the CM group in the short term, which increased in the longer term. Hickam et al. (Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013) reported that CM interventions were generally associated with improved patient (and caregiver) satisfaction, although satisfaction with the CM itself varied across interventions. Studies measuring patient satisfaction typically reported overall satisfaction with care, rather than satisfaction in specific domains. Some studies found that CM improved patients’ perceptions of coordination among healthcare providers.
Regarding health outcomes, none of the secondary studies found any effect of CM on either short- or long-term survival.
On the issue of depression, the secondary studies identified highly consistent results. In a meta-analysis of 18 RCTs examining a range of complex interventions for people with multimorbidity, Smith et al. (Reference Smith, Wallace, O’Dowd and Fortin2016) found that mental health outcomes improved, with modest reductions in mean depression scores for the comorbidity studies targeting participants with depression. Hickam et al. (Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013) found moderate evidence of CM programs for patients with dementia reducing their depression and the strain on caregivers.
Hickam et al. (Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013) also found that CM interventions produced mixed results in terms of improving patients’ QOL. On the whole, CM sometimes succeeded in improving aspects of QOL targeted directly by the interventions. For instance, CM improved caregiver stress among individuals caring for patients with dementia and also raised congestive heart failure (CHF)-related QOL among patients with this chronic heart condition. The measures used to assess QOL varied across studies, and any improvements in QOL achieved by CM were either small or of unclear clinical significance. CM was less successful in improving overall QOL, as indicated by global measures not specific to a particular condition. When Joo et al. (2013) investigated the effectiveness of nurse-led, community-based CM, they found that it generally enhanced patients’ QOL. Boult et al. (Reference Boult, Green, Boult, Pacala, Snyder and Leff2009) likewise found that 7/8 studies produced positive results for a set of QOL measures (less decline in SF-36 social function; greater control of fatigue and improved mastery; an increase in social support).
A low consistency among studies emerged regarding the effectiveness of CM on patients’ functional status. Hickam et al. (Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013) found that CM programs serving patients with one or more chronic diseases do not result in clinically important improvements in their functional status (three studies). Boult et al. (Reference Boult, Green, Boult, Pacala, Snyder and Leff2009) also said that CM studies produced weak evidence of patients achieving a greater functional autonomy. When Hutt et al. (Reference Hutt, Rosen and McCauley2004) analyzed the effectiveness of CM on long-term conditions, they found 6 RCTs that had considered functional ability as an outcome: 3 of them reported better results for patients who were involved in CM schemes than for those who were not, in terms of either a more limited decline in functional ability or an improvement in function.
Based on the available literature, contrasting data emerged regarding clinical outcomes. In particular, Hickam et al. (Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013) found only one observational study with a pre-post design that had examined changes in physiological measures after three months of CM. Blood pressure and glucose and cholesterol levels showed a moderate decrease compared with pre-CM values. Smith et al. (Reference Smith, Wallace, O’Dowd and Fortin2016) wrote that five studies had reported on six measures of glycemic control with a mean difference (MD) equal to 0.02 (95% CI − 0.21 to 0.25), and four studies reported on systolic blood pressure (SBP), describing a MD of −3.10 (95% CI − 7.26 to 1.06).
As for resource usage (Table 4), secondary studies (4 meta-analyses and 5 systematic reviews) consistently returned a lack of evidence of CM producing any reduction in hospital admissions. For example, Huntley et al. (Reference Huntley, Thomas, Mann, Huws, Elwyn, Paranjothy and Purdy2013) found that 9 of 11 studies (including RCTs) had found no decline in unplanned hospital admissions with CM compared with usual care. Stokes et al. (Reference Stokes, Panagioti, Alam, Checkland, Cheraghi-Sohi and Bower2015) also reported no effect on secondary care in either the short term (0.04, 95% CI −0.02 to 0.10, I 2 = 39.6%, P = 0.027) or the longer term (−0.02, 95% CI −0.08 to 0.04, I 2 = 22.8%, P = 0.194, 16 studies).
When overall expenditure was considered, the consistency was low once again. Hickam et al. (Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013) found that studies examining the impact of CM for adults with chronic medical illnesses and complex care needs on the overall cost of care had identified no significant differences between patients receiving CM and controls. Although the cost of CM programs was often modest relative to the overall costs of patients with high levels of health service usage, the effect of CM in reducing said usage was minimal. On the other hand, when Soril et al. (Reference Soril, Leggett, Lorenzetti, Noseworthy and Clement2015) looked at CM interventions to reduce frequent visits to the ED, they found two RCTs that had specifically assessed the costs of CM programs from a health system perspective. One identified an increase in the cost of care for all participants over a 12-month follow-up, but this cost increase was significantly smaller for the patients exposed to the CM intervention than for those in the control group. The other study estimated a (statistically significant) 45% reduction in the cost of care for the CM intervention group.
Discussion
This review of reviews not only provides strong evidence of CM improving adherence to treatment guidelines and patient satisfaction but also shows that CM has no impact on patient survival or hospitalization rates. Inconsistent evidence emerged on whether or not the other outcomes addressed are improved by CM.
Going into more detail, our review of reviews seems to show that CM ameliorates care processes. In particular, all the secondary studies considered consistently demonstrated that CM improved the adherence of prescriptions to the guidelines. In fact, CM interventions often employed clinical pathways to arrange personalized treatment plans (Kim and Soeken, 2015), making it easier for prescriptions to reflect evidence-based care (Chawla et al., Reference Chawla, Westrich, Matter, Kaltenboeck and Dubois2016). As for patients’ compliance to their drug prescriptions, people with multimorbidity frequently have specific difficulties relating to polypharmacy and the management of complex medical treatment regimes, so CM interventions to adjust their medication may facilitate their compliance (Brown and Bussell, Reference Brown and Bussell2011). Our review of reviews found inconsistent evidence of CM succeeding in improving this outcome, however.
Concerning health measures, all the secondary studies confirmed the effectiveness of CM in enhancing patient satisfaction. This is in line with other reports that CM implemented by nurses improves patient-centered care, empowering patients to manage their own health, control their symptoms, and improve their QOL and helping them to stay independent for longer (Dorr et al., Reference Dorr, Wilcox, Burns, Brunker, Narus and Clayton2006). Developing patients’ self-management skills could also help to reinforce their satisfaction with their care.
On the other hand, all the secondary studies that we analyzed were unable to demonstrate the effectiveness of CM in improving overall survival. Several authors tried to explain the reasons for the limited impact of CM on this parameter, most of them arguing that the intervention period may have been too short to make a difference, or that the follow-up time was too short to detect a difference (Eklund and Wilhelmson, Reference Eklund and Wilhelmson2009). Starfield suggested instead that the limited influence of CM may be due to excellent usual care. In other words, CM may simply be replacing some of the functions of a well-coordinated, person-centered primary care (Starfield et al., Reference Starfield, Shi and Macinko2005). Stokes et al. (Reference Stokes, Panagioti, Alam, Checkland, Cheraghi-Sohi and Bower2015) tested this hypothesis, confirming that the effects of CM on overall survival are greater when it is delivered in contexts where routine primary care services are less well developed, whereas the capacity of CM to improve overall survival is minimal in settings with strong primary care services. Other subgroup analyses performed on the same studies indicated that CM by a multidisciplinary team (as opposed to a single case manager) that included a social worker improved short-term (but not long-term) mortality. These findings are consistent with the wider literature advocating the use of a multidisciplinary team to manage patients with long-term conditions successfully (Wagner, Reference Wagner2000) and promote a stronger integration of health and social care (Valentjin et al., Reference Valentijn, Schepman, Opheij and Bruijnzeels2013).
As for the impact of CM on healthcare expenditures, our review of reviews cannot sustain the efficacy of CM in containing acute hospitalizations, especially in the light of the findings of the high-quality systemic reviews and meta-analyses we considered. Here again, Stokes conducted subgroup analyses to see if certain characteristics of CM can improve this outcome, confirming that CM performed significantly better vis-à-vis the usage of secondary care in countries less oriented toward primary care delivery by multidisciplinary teams, and with the involvement of a social worker (Stokes et al., Reference Stokes, Panagioti, Alam, Checkland, Cheraghi-Sohi and Bower2015). Both Huntley and Hickam also suggested that the effectiveness of an intervention relates to the profile of the population recruited, and they both concluded that CM is more effective in reducing hospitalization rates among patients with a greater burden of disease (Hickam et al., Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013; Huntley et al., Reference Huntley, Thomas, Mann, Huws, Elwyn, Paranjothy and Purdy2013). This last issue appears to be strongly influenced by the type of risk tool used to target patients most likely to benefit from CM. In fact, Stokes et al. (Reference Stokes, Panagioti, Alam, Checkland, Cheraghi-Sohi and Bower2015) demonstrated a greater efficacy of CM in reducing secondary care service usage in the short term for programs that adopted a risk modeling approach rather than relying on clinical judgment, although the difference was not statistically significant.
This review of reviews has some limitations to bear in mind. The most significant concerns the lack of any indication of the overlap between the primary studies included in each of the secondary analyses. For example, some studies may have been included in multiple analyses, making their findings more influential because they were counted more than once (Aromataris et al., Reference Aromataris, Fernandez, Godfrey, Holly, Khalil and Tungpunkom2015). Theoretically, this means that the less recent studies acquire more weight as they are more likely to have been included in earlier and later analyses, whereas the most recent studies can clearly have only been the object of one secondary analysis since their publication.
Another important limitation of our review of reviews concerns the marked differences between the characteristics of the primary studies on CM. Most of the systematic reviews and meta-analyses had already highlighted this issue, but a review of reviews pooling secondary analyses together naturally makes this issue even more prominent, complicating the comparison between the studies and hampering the opportunity to make conclusive statements. The main variations concerned sample size, population characteristics, patient identification and assessment, measurements of outcome, content and duration of the CM intervention, context-related barriers and facilitators within organizations, length of follow-up, and outcomes. Information on the content of the intervention was often rather scarce, as was the information provided on the care given to the control groups.
Implications for research
Our review of reviews found a low consistency of the evidence of the impact of CM for most of the outcomes considered. It is hard to say whether this stems from the intrinsic variability of the outcome measures or, more plausibly, from the heterogeneity of the CM programs considered (in terms of what the intervention involved), the target populations, and the tools used to measure the outcomes. This important drawback suggests that future clinical research needs a more detailed and clearly classified description of such interventions. At the same time, future secondary studies should clearly state their eligibility criteria in order to facilitate the interpretation of sources of variability. CM programs often differ in setting, case manager figure, elements of the program, and possibly also the components of single interventions. For example, the components of self-care support interventions can vary widely (Challis et al., Reference Challis, Hughes, Berzins, Reilly, Abell and Stewart2010). As concerns the target population, a description of the tools used to enroll participants in CM schemes is essential to enable considerations on their external validity and generalizability (Smith et al., Reference Smith, Wallace, O’Dowd and Fortin2016). On this point, the main issues probably lie in the great variety of risk assessment tools used to assess the degree of a patientʼs multimorbidity (O’Caoimh et al., Reference O’Caoimh, Cornally, Weathers, O’Sullivan, Fitzgerald, Orfila, Clarnette, Paùl and Molloy2015), and the setting where this assessment is conducted will have an influence too. Finally, another problem concerns the different scales generally used to measure the same outcome in different studies, and the different periods of time considered: a longer-term relationship between patients and their case managers is likely to improve the success of a CM program (Hickam et al., Reference Hickam, Weiss, Guise, Buckley, Motu’apuaka, Graham, Wasson and Saha2013).
Studies should also provide details on the barriers to and facilitators of CM implementation across various primary care settings. For instance, one previous review (Kadu and Paul, Reference Kadu and Paul2015) found that the inner setting of the organization, the process of implementation, and characteristics of the individual healthcare providers could mediate the effectiveness of the primary care model.
Further investigations could focus on whether CM can be considered cost-effective or cost-saving from a societal and healthcare payment perspective by comparison with traditional fragmented practice. This could support healthcare decision-makers to conduct Health Technology Assessments that would also be applicable in the assessment of organizational models.
Acknowledgments
This article is based on a research program titled ‘Chronic diseases: support and comparative evaluation of interventions for the proactive identification and treatment of complex patients aimed at preventing repeated hospitalizations’, project carried out with the financial support of the Ministry of Health.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1463423620000080








